Abstract
Objective
Diabetes is highly prevalent in individuals with acute coronary syndrome (ACS). Current NICE guidelines recommend diabetes screening of hyperglycaemic patients using a fasting plasma glucose after 4 days from admission. In 2012 the World Health Organisation (WHO) approved the use of HbA1c in the diagnosis and targeted screening for type 2 diabetes. We introduced a service improvement project using HbA1c for diabetes screening in patients with no previous diagnosis of diabetes admitted with ACS regardless of glycaemic state.
Method
An initial retrospective audit utilised 21 months of data from the MINAP database to identify patients meeting current NICE criteria for diabetes screening. A prospective service improvement project was undertaken over a 4 month period using HbA1c as a universal screening test to categorise ACS patients based on WHO criteria.
Results
The retrospective audit identified 93 of 420 (22%) patients with pre-existing diabetes and 8 of the remaining 327 (2.4%) were hyperglycaemic, thus meeting NICE criteria for diabetes screening. In the service improvement project 2/49 patients (4%) met NICE criteria for diabetes screening. Twenty six of these 49 patients had a HbA1c test on admission and 17/26 (65.4%) were classified as probable diabetes or high risk.
Conclusion
A significant proportion of ACS patients have diabetes, which may be undetected by current NICE criteria. Universal HbA1c testing offers utility as a simple and effective screening test for diabetes in the ACS population.
Keywords: Diabetes Screening, HbA1c, Acute Coronary Syndrome
INTRODUCTION
Diabetes mellitus is a significant public health challenge associated with cardiovascular morbidity and mortality.1 The prevalence of diabetes in Northern Ireland is currently around 5.3%, with new diagnoses increasing by around 33% in the past 5 years.2 It is estimated that up to 12,000 individuals within the region with diabetes remain undiagnosed.2 A targeted programme of diabetes screening, particularly for those with established cardiovascular disease is recommended to identify and treat individuals at high risk.
Coronary heart disease is a leading cause of morbidity and mortality in diabetes, and around 22-27% of patients admitted with acute coronary syndrome (ACS), have established diabetes.3, 4, 5, 6 As in the general population, unrecognised diabetes is an unmet need for up to 22-31% of others presenting with ACS.3, 4, 5, 6 NICE (National Institute for Health and Care Excellence) guidelines for diabetes screening recommend that all patients with admission blood glucose concentrations above 11.0 mmol/l should have a fasting plasma glucose no earlier than day 4 after ACS onset or have an HbA1c test before discharge.1
The WHO have recommended HbA1c as the preferred screening test for the diagnosis of type 2 diabetes mellitus.6 Others have highlighted the potential role for HbA1c as a universal screening test in the ACS setting.7 More recently the ESC/EASD (European Society of Cardiology/European Association for the Study of Diabetes) have recommended all ACS patients be screened for diabetes.8
We undertook a retrospective audit of NICE diabetes screening guidelines followed by a service improvement project assessing the utility of universal HbA1c screening in the ACS population.
METHODS
Audit
The Myocardial Ischaemia National Audit Project (MINAP) is a clinical database, for collection of clinical data on all patients admitted with ACS. 420 patients who presented to the Mater Hospital were identified using the MINAP database over a 21 month period. 93 had previously diagnosed diabetes and 8 met NICE criteria to be screened for diabetes.
Service Improvement Project
HbA1c testing was recommended for screening in ACS regardless of glycaemic status during a service improvement project.
No patients tested were known to have medical conditions that could influence HbA1c measurement. This included factors that affect erythropoiesis such as iron or B12 deficiency or supplementation, haemoglobinopathies and conditions that affect erythocyte life span such as splenectomy or splenomegaly.6 Patients were not screened for chronic aspirin use which may cause a falsely low HbA1c in certain assays.6
We categorised patients according to WHO criteria as “probable diabetes” (HbA1c≥48 mmol/mol), “high risk” (HbA1c 42-47 mmol/mol) and “not diabetes” (HbA1c<42 mmol/mol).6, 7
RESULTS
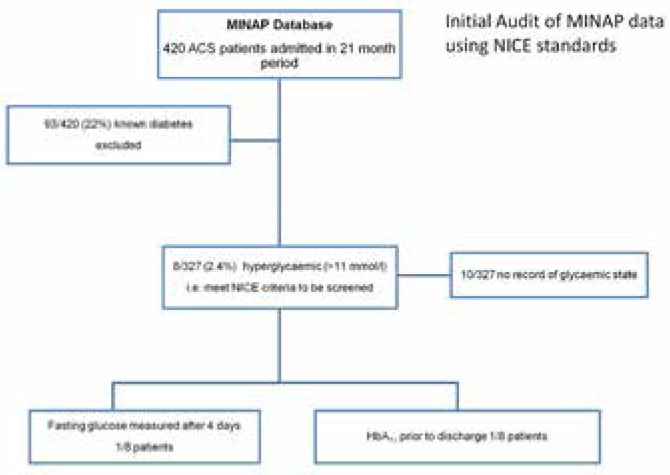
Over the previous 21 month period 93 of 420 (22%) ACS patients were identified with established diabetes. Of the remaining 327 patients, only 8 (2.4%) met NICE criteria for diabetes screening and only one patient was tested (Figure 1).
Fig 1.
Initial Audit of NICE Guidelines
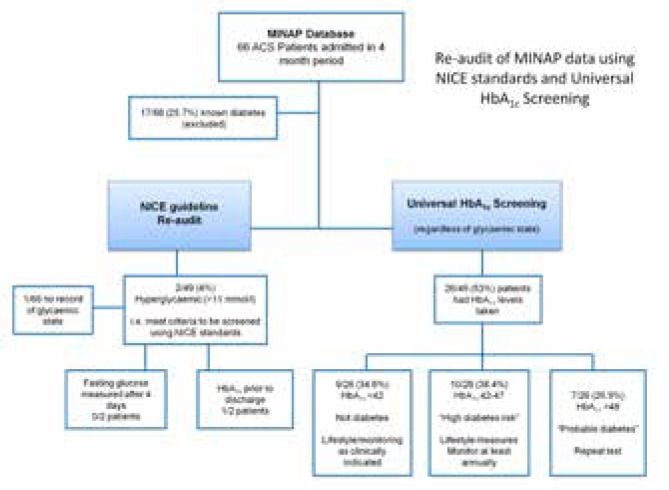
During the service improvement phase, 17 of 66 ACS patients had established diabetes. Of the remaining 49 patients only 2 met criteria for screening and neither had fasting glucose tested. 26 of 49 patients (52%) were tested with a mean HbA1c level of 45.1 mmol/mol (range 31.1-65.0 mmol/mol).
7/26 (26.9%) of these were categorised as “probable diabetes”, 10/26 (38.4%) were at high risk of developing diabetes and 9/26 (34.6%) had diabetes excluded (Figure 2).
Fig 2.
Re-audit of MINAP using NICE standards and Universal HbA1c Screening Project
DISCUSSION
Diabetes mellitus is increasingly prevalent and is a significant public health challenge.2, 6 Diabetes is associated with increased cardiovascular risk, and in patients presenting with acute coronary syndrome; it is an independent predictor of mortality and is associated complications including heart failure and bleeding.8 For these reasons, the European Society of Cardiology (ESC) recommend that all patients admitted with ACS are screened for diabetes and have recently recommended the adoption of HbA1c as a screening tool in line with the World Health Organisation.8
Targeted diabetes screening as advocated by NICE using hyperglycaemia as an inclusion criterion appeared to lack sensitivity and was not readily implemented in clinical practice during our recent audit. Use of universal HbA1c screening on admission appeared to be more practical and effective with improved detection rates in this setting. In our service improvement project we identified a higher prevalence of probable diabetes and pre-diabetes cases (65.4%) compared with earlier published series.3, 4, 5, 6 We detected a prevalence rate of established diabetes of around 22%, which is similar to earlier published reports.3, 4, 5
Poor utilisation of current NICE screening may reflect the guidelines complexity, limited awareness and the small numbers of qualifying patients. In addition, patients may not be screened with day four fasting glucose measurement due to increasingly shorter length of stays.
There are a number of potential benefits in using HbA1c as a screening tool for diabetes. Firstly, it is less likely to be impacted by short term fluctuations in glycaemic control, including stress hyperglycaemia. While HbA1c testing is more expensive (£6.81) than fasting plasma glucose (£2.05) it compares favourably to the cost of an oral glucose tolerance test at £7.48.9 HbA1c testing is not recommended for screening in type 1 diabetes, secondary diabetes or pregnancy. In these scenarios, established fasting plasma glucose and/or glucose tolerance testing criteria remain valid and are recommended for use. Other confounders include alcoholism, chronic renal failure and conditions affecting erythropoesis.6
This study has a number of limitations. As this was an audit and service improvement project it was not designed to determine sensitivity and specificity against a gold standard test. Despite staff education a significant proportion of patients (47%) were not tested using HbA1c. Had we achieved screening of consecutive ACS patients, we would have anticipated a higher proportion of patients testing positive for diabetes. Nevertheless, introduction of HbA1c as a screening test for diabetes during this service improvement project was considered to be of clinical value as a practical, widely accessible, and reproducible method for the purpose for ACS patients who have been hospitalised. Indeed, this approach has utility, including for patients attending other cardiac services such as rapid access chest pain clinics.10
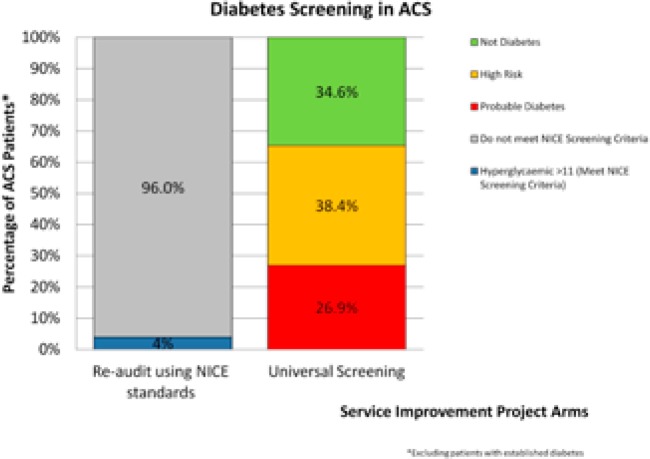
This service improvement project revealed a missed population of patients with “probable diabetes” (26.9%) and at “high risk” (38.4%) of diabetes who were largely previously unscreened when NICE guidance was followed (Figure 3). We believe that introduction of HbA1c as part of an ACS admission profile offers a simplified and accessible screening test for the early diagnosis and management of patients with diabetes. Perhaps it is time for a reappraisal of UK guidelines?
Fig 3.
Comparison of NICE Guidelines to Universal Screening strategy
The Authors have no conflict of interest.
REFERENCES
- 1.NICE Clinical Guideline; CG130. Hyperglycaemia in acute coronary syndromes: management of hyperglycaemia in acute coronary syndromes. London: National Institute for Health and Care Excellence; 2013. Available from: http://guidance.nice.org.uk/CG130. Last accessed May 2015. [PubMed] [Google Scholar]
- 2.Diabetes UK. Diabetes prevalence 2013 (February 2014). Quality and outcomes framework; State of the Nation; Available from: https://www.diabetes.org.uk/About_us/What-we-say/Statistics/Diabetesprevalence-2013/ Last accessed May 2015. [Google Scholar]
- 3.Okosieme OE, Peter R, Usman M, Bolusani H, Suruliram P, George L, et al. Can admission and fasting glucose reliably identify undiagnosed diabetes in patients with acute coronary syndrome? Diabetes Care. 2008;31(10):1955–9. doi: 10.2337/dc08-0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norhammar A, Tenerz A, Nilsson G, Hamsten A, Efendic S, Ryden L, et al. Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus; a prospective study. Lancet. 2002;359(9324):2140–4. doi: 10.1016/S0140-6736(02)09089-X. [DOI] [PubMed] [Google Scholar]
- 5.Bartnik M, Ryden L, Ferrari R, Malmberg K, Pyorala K, Simoons M, et al. The prevalence of abnormal glucose regulation in patients with coronary artery disease across Europe. The EuroHeart Survey on diabetes and the heart. Eur Heart J. 2004;25(21):1880–90. doi: 10.1016/j.ehj.2004.07.027. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organisation. Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: abbreviated report of a WHO consultation. Geneva: World Health Organisation; 2011. Available from: http://www.who.int/diabetes/publications/diagnosis_diabetes2011/en/. Last accessed May 2015. [PubMed] [Google Scholar]
- 7.Gholap N, Davies MJ, Mostafa SA, Squire I, Khunti K. A simple strategy for screening for glucose intolerance, using glycated haemoglobin, in individuals admitted with acute coronary syndrome. Diabet Med. 2012;29(7):838–43. doi: 10.1111/j.1464-5491.2012.03643.x. [DOI] [PubMed] [Google Scholar]
- 8.ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD) Eur Heart J. 2013;34(39):3035–87. doi: 10.1093/eurheartj/eht108. [DOI] [PubMed] [Google Scholar]
- 9.NICE Clinical Guideline: CG130. London: National Institute for Health and Care Excellence; 2011. Hyperglycaemia in acute coronary syndromes. Costing statement. Implementing NICE guideline. Available from: http://www.nice.org.uk/guidance/cg130/resources/cg130-hyperglycaemia-in-acute-coronary-syndromes-costing-statement2. Last accessed May 2015. [PubMed] [Google Scholar]
- 10.Wallace HJ, Ferguson S, Bernatowicz D, Dougan J, Hunter SJ. Targeted Screening Using HbA1c Identifies a High Yield of Patients with Impaired Glucose Metabolism (IGM) Ir J Med Sci. 2013;182(9 Suppl):S415–6. [Google Scholar]