Abstract
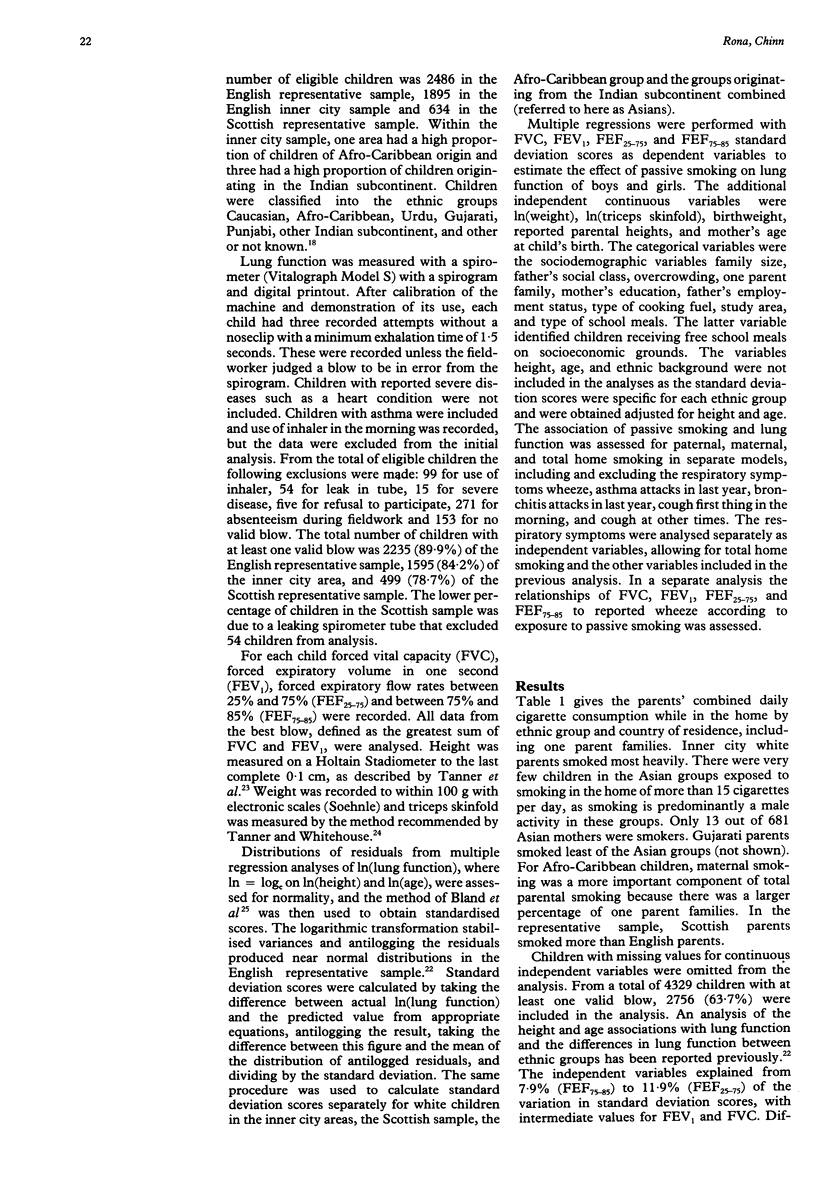
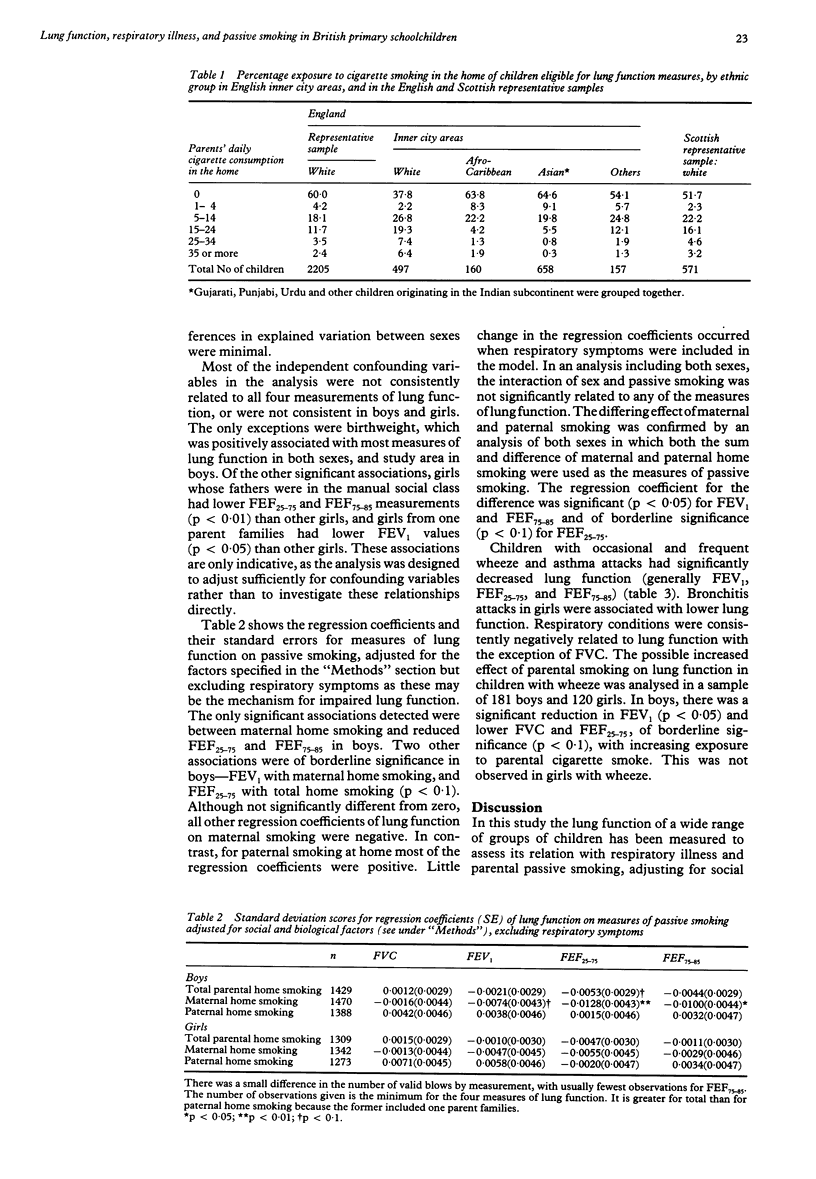
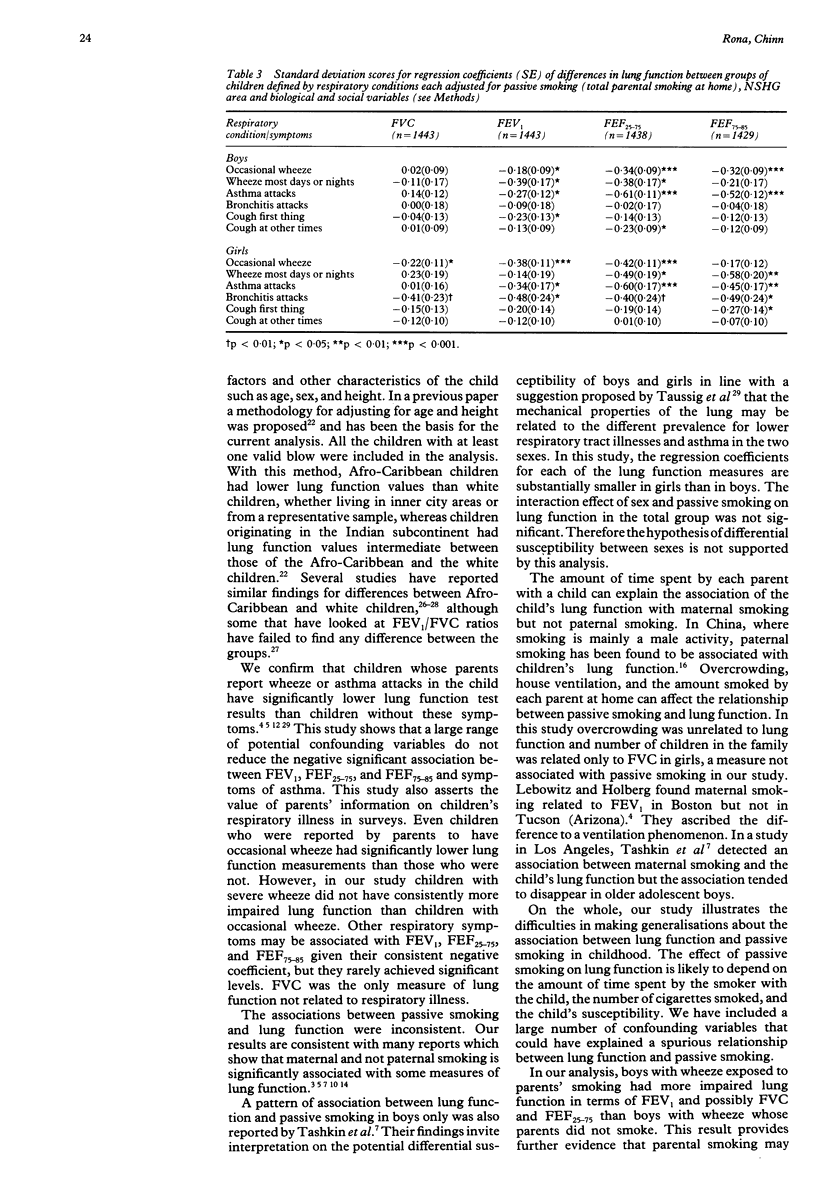
BACKGROUND: Many studies have reported a significant association between parents' smoking and reduced lung function in their children, but often the association has been found to be significant only in relation to maternal smoking. There have been few epidemiological studies on this topic in Britain. METHODS: Spirometry, in 2756 children aged 6.50-11.99 years, was carried out in a representative sample of English children, an inner city and ethnic minority sample, and a Scottish sample. Forced vital capacity (FVC), forced expiratory volume in one second (FEV1), and forced expiratory flow rates of 25-75% and 75-85% (FEF25-75 and FEF75-85) were measured and standardised scores obtained separately for the English representative sample, the Scottish sample and subgroups in the inner city sample, white and Afro-Caribbean children and those originating from the Indian subcontinent. Multiple regression analyses were used to assess associations of FVC, FEV1, FEF25-75 and FEF75-85 with the passive smoking and respiratory illness, with adjustment for a large number of potential confounders. Passive smoking was defined in terms of reported number of cigarettes smoked at home by each parent. The respiratory symptoms and illnesses assessed were wheeze, asthma and bronchitis attacks, cough in the morning, and cough at any other time as reported by parents. RESULTS: Maternal smoking, but not paternal smoking, was associated with reduced FEF25-75 and FEF75-85 in boys. No association was found between passive smoking and lung function in girls, but in an analysis including both sexes the interaction of sex and parental smoking on lung function was not significant. With few exceptions, FEV1, FEF25-75 and FEF75-85 were reduced in children with wheeze and asthma attacks. CONCLUSIONS: The effect of passive smoking may depend on the close contact of a parent with a susceptible child as only maternal smoking in boys was significantly associated with impaired lung function. However, this explanation remains unsubstantiated. A parent's report of wheeze and asthma attacks in the child is reflected in reduced lung function.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brunekreef B., Dockery D. W., Speizer F. E., Ware J. H., Spengler J. D., Ferris B. G. Home dampness and respiratory morbidity in children. Am Rev Respir Dis. 1989 Nov;140(5):1363–1367. doi: 10.1164/ajrccm/140.5.1363. [DOI] [PubMed] [Google Scholar]
- Burchfiel C. M., Higgins M. W., Keller J. B., Howatt W. F., Butler W. J., Higgins I. T. Passive smoking in childhood. Respiratory conditions and pulmonary function in Tecumseh, Michigan. Am Rev Respir Dis. 1986 Jun;133(6):966–973. doi: 10.1164/arrd.1986.133.6.966. [DOI] [PubMed] [Google Scholar]
- Chen Y., Li W. X. The effect of passive smoking on children's pulmonary function in Shanghai. Am J Public Health. 1986 May;76(5):515–518. doi: 10.2105/ajph.76.5.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinn S., Rona R. J. Height and age adjustment for cross sectional studies of lung function in children aged 6-11 years. Thorax. 1992 Sep;47(9):707–714. doi: 10.1136/thx.47.9.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinn S., Rona R. J. Quantifying health aspects of passive smoking in British children aged 5-11 years. J Epidemiol Community Health. 1991 Sep;45(3):188–194. doi: 10.1136/jech.45.3.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dockery D. W., Berkey C. S., Ware J. H., Speizer F. E., Ferris B. G., Jr Distribution of forced vital capacity and forced expiratory volume in one second in children 6 to 11 years of age. Am Rev Respir Dis. 1983 Sep;128(3):405–412. doi: 10.1164/arrd.1983.128.3.405. [DOI] [PubMed] [Google Scholar]
- Hasselblad V., Humble C. G., Graham M. G., Anderson H. S. Indoor environmental determinants of lung function in children. Am Rev Respir Dis. 1981 May;123(5):479–485. doi: 10.1164/arrd.1981.123.5.479. [DOI] [PubMed] [Google Scholar]
- Holland W. W., Halil T., Bennett A. E., Elliott A. Factors influencing the onset of chronic respiratory disease. Br Med J. 1969 Apr 26;2(5651):205–208. doi: 10.1136/bmj.2.5651.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauffmann F., Tager I. B., Muñoz A., Speizer F. E. Familial factors related to lung function in children aged 6-10 years. Results from the PAARC epidemiologic study. Am J Epidemiol. 1989 Jun;129(6):1289–1299. doi: 10.1093/oxfordjournals.aje.a115248. [DOI] [PubMed] [Google Scholar]
- Lebowitz M. D., Holberg C. J. Effects of parental smoking and other risk factors on the development of pulmonary function in children and adolescents. Analysis of two longitudinal population studies. Am J Epidemiol. 1988 Sep;128(3):589–597. doi: 10.1093/oxfordjournals.aje.a115006. [DOI] [PubMed] [Google Scholar]
- Lebowitz M. D., Holberg C. J., Knudson R. J., Burrows B. Longitudinal study of pulmonary function development in childhood, adolescence, and early adulthood. Development of pulmonary function. Am Rev Respir Dis. 1987 Jul;136(1):69–75. doi: 10.1164/ajrccm/136.1.69. [DOI] [PubMed] [Google Scholar]
- Leeder S. R., Corkhill R. T., Wysocki M. J., Holland W. W. Influence of personal and family factors on ventilatory function of children. Br J Prev Soc Med. 1976 Dec;30(4):219–224. doi: 10.1136/jech.30.4.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melia R. J., Chinn S., Rona R. J. Respiratory illness and home environment of ethnic groups. Br Med J (Clin Res Ed) 1988 May 21;296(6634):1438–1441. doi: 10.1136/bmj.296.6634.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick J. M., Patel A. Ethnic differences in the growth of lung function in children: a cross-sectional study in inner-city Nottingham. Ann Hum Biol. 1986 Jul-Aug;13(4):307–315. doi: 10.1080/03014468600008491. [DOI] [PubMed] [Google Scholar]
- Rona R. J., Chinn S. National Study of Health and Growth: social and biological factors associated with height of children from ethnic groups living in England. Ann Hum Biol. 1986 Sep-Oct;13(5):453–471. doi: 10.1080/03014468600008631. [DOI] [PubMed] [Google Scholar]
- Rona R. J., du V Florey C. National study of health and growth: respiratory symptoms and height in primary schoolchildren. Int J Epidemiol. 1980 Mar;9(1):35–43. doi: 10.1093/ije/9.1.35. [DOI] [PubMed] [Google Scholar]
- Schilling R. S., Letai A. D., Hui S. L., Beck G. J., Schoenberg J. B., Bouhuys A. Lung function, respiratory disease, and smoking in families. Am J Epidemiol. 1977 Oct;106(4):274–283. doi: 10.1093/oxfordjournals.aje.a112463. [DOI] [PubMed] [Google Scholar]
- Schwartz J., Katz S. A., Fegley R. W., Tockman M. S. Sex and race differences in the development of lung function. Am Rev Respir Dis. 1988 Dec;138(6):1415–1421. doi: 10.1164/ajrccm/138.6.1415. [DOI] [PubMed] [Google Scholar]
- Strachan D. P., Jarvis M. J., Feyerabend C. The relationship of salivary cotinine to respiratory symptoms, spirometry, and exercise-induced bronchospasm in seven-year-old children. Am Rev Respir Dis. 1990 Jul;142(1):147–151. doi: 10.1164/ajrccm/142.1.147. [DOI] [PubMed] [Google Scholar]
- Strachan D. P., Sanders C. H. Damp housing and childhood asthma; respiratory effects of indoor air temperature and relative humidity. J Epidemiol Community Health. 1989 Mar;43(1):7–14. doi: 10.1136/jech.43.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tager I. B., Weiss S. T., Muñoz A., Rosner B., Speizer F. E. Longitudinal study of the effects of maternal smoking on pulmonary function in children. N Engl J Med. 1983 Sep 22;309(12):699–703. doi: 10.1056/NEJM198309223091204. [DOI] [PubMed] [Google Scholar]
- Tager I. B., Weiss S. T., Rosner B., Speizer F. E. Effect of parental cigarette smoking on the pulmonary function of children. Am J Epidemiol. 1979 Jul;110(1):15–26. doi: 10.1093/oxfordjournals.aje.a112783. [DOI] [PubMed] [Google Scholar]
- Tanner J. M., Whitehouse R. H. Revised standards for triceps and subscapular skinfolds in British children. Arch Dis Child. 1975 Feb;50(2):142–145. doi: 10.1136/adc.50.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner J. M., Whitehouse R. H., Takaishi M. Standards from birth to maturity for height, weight, height velocity, and weight velocity: British children, 1965. I. Arch Dis Child. 1966 Oct;41(219):454–471. doi: 10.1136/adc.41.219.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tashkin D. P., Clark V. A., Simmons M., Reems C., Coulson A. H., Bourque L. B., Sayre J. W., Detels R., Rokaw S. The UCLA population studies of chronic obstructive respiratory disease. VII. Relationship between parental smoking and children's lung function. Am Rev Respir Dis. 1984 Jun;129(6):891–897. doi: 10.1164/arrd.1984.129.6.891. [DOI] [PubMed] [Google Scholar]
- Taussig L. M., Cota K., Kaltenborn W. Different mechanical properties of the lung in boys and girls. Am Rev Respir Dis. 1981 Jun;123(6):640–643. doi: 10.1164/arrd.1981.123.6.640. [DOI] [PubMed] [Google Scholar]
- Ware J. H., Dockery D. W., Spiro A., 3rd, Speizer F. E., Ferris B. G., Jr Passive smoking, gas cooking, and respiratory health of children living in six cities. Am Rev Respir Dis. 1984 Mar;129(3):366–374. doi: 10.1164/arrd.1984.129.3.366. [DOI] [PubMed] [Google Scholar]
- Ware J. H., Ferris B. G., Jr, Dockery D. W., Spengler J. D., Stram D. O., Speizer F. E. Effects of ambient sulfur oxides and suspended particles on respiratory health of preadolescent children. Am Rev Respir Dis. 1986 May;133(5):834–842. [PubMed] [Google Scholar]
- Yarnell J. W., St Leger A. S. Respiratory infections and their influence on lung function in children: a multiple regression analysis. Thorax. 1981 Nov;36(11):847–851. doi: 10.1136/thx.36.11.847. [DOI] [PMC free article] [PubMed] [Google Scholar]


