Abstract
Nonalcoholic fatty liver disease (NAFLD) has increased in parallel with central obesity, and its prevalence is anticipated to increase as the obesity epidemic remains unabated. NAFLD is now the most common cause of chronic liver disease in developed countries and is defined as excessive lipid accumulation in the liver, that is, hepatosteatosis. NAFLD ranges in severity from benign fatty liver to nonalcoholic steatohepatitis (NASH), and NASH is characterized by hepatic injury, inflammation, oxidative stress, and fibrosis. NASH can progress to cirrhosis, and cirrhosis is a risk factor for primary hepatocellular carcinoma (HCC). The prevention of NASH will lower the risk of cirrhosis and NASH-associated HCC. Our studies have focused on NASH prevention. We developed a model of NASH by using mice with the LDL cholesterol receptor gene ablated fed the Western diet (WD). The WD induces a NASH phenotype in these mice that is similar to that seen in humans and includes robust induction of hepatic steatosis, inflammation, oxidative stress, and fibrosis. With the use of transcriptomic, lipidomic, and metabolomic approaches, we examined the capacity of 2 dietary ω-3 (n–3) polyunsaturated fatty acids, eicosapentaenoic acid (20:5ω-3; EPA) and docosahexaenoic acid (22:6ω-3; DHA), to prevent WD-induced NASH. Dietary DHA was superior to EPA at attenuating WD-induced changes in plasma lipids and hepatic injury and at reversing WD effects on hepatic metabolism, oxidative stress, and fibrosis. The outcome of these studies suggests that DHA may be useful in preventing NASH and reducing the risk of HCC.
Keywords: fatty liver disease, liver cancer, inflammation, oxidative stress, fibrosis, metabolomics, ω-3 PUFAs
Introduction
Primary hepatocellular carcinoma (HCC)4 is the fifth most common human cancer in men and the seventh most common cancer in women in the Western societies, and HCC represents the third most frequent cause of cancer deaths worldwide (1–3). High rates of HCC are seen in Eastern and Southeastern Africa and Asia and lower levels in Western countries. Risk factors for HCC include age and sex (male), hepatitis virus infection (hepatitis B and C viruses), exposure to toxins (aflatoxin), chronic alcohol abuse, cirrhosis, tobacco use, and genetic disorders (hereditary hemochromatosis, α1-antitrypsin deficiency, and primary biliary cirrhosis) (1, 2).
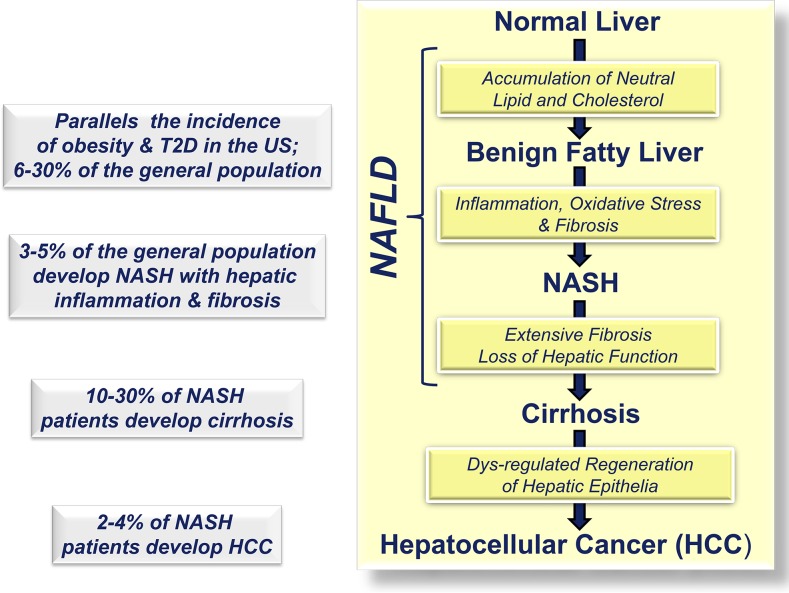
The unabated increase in the incidence of obesity, type 2 diabetes (T2D), and nonalcoholic fatty liver disease (NAFLD) is driving the concern for an increased HCC incidence in Western societies (4) (Figure 1). This is because NAFLD can progress to nonalcoholic steatohepatitis (NASH) and cirrhosis; cirrhosis is a risk factor for HCC. Chronic fatty liver disease sets the stage for poorly regulated regeneration of hepatic parenchymal cells resulting from hepatic inflammation, parenchymal cell death, and fibrosis, thus, increasing HCC risk. Current treatment options for HCC are limited to surgery and drugs such as the multi-kinase inhibitor, sorafenib. Because diet is a main driver of NAFLD and NASH progression, our focus was on developing nutritional strategies to prevent NASH. This report focuses on the use of dietary 20–22-carbon ω-3 PUFAs to prevent NASH.
FIGURE 1.
Transition from normal liver to primary HCC. HCC, hepatocellular carcinoma; NAFLD, nonalcoholic fatty liver disease; NASH, nonalcoholic steatohepatitis; T2D, type 2 diabetes.
NAFLD and NASH
Current data from the CDC estimate that nearly 78.6 million obese adults and 12.7 million obese children (aged 2–19 y) are in the United States (5, 6). Obesity is a risk factor for developing NAFLD and NASH. As such, the prevalence of NAFLD and NASH has increased in parallel with the incidence of central obesity in Western societies (7, 8). NAFLD is the most common fatty liver disease in developed countries (9) and is defined as excessive lipid accumulation in the liver, that is, hepatosteatosis (10, 11). NAFLD is the hepatic manifestation of metabolic syndrome (MetS) (12), and MetS risk factors include obesity, elevated plasma TGs and LDL cholesterol, reduced HDL cholesterol, high blood pressure, and fasting hyperglycemia (13). The prevalence of NAFLD in the general population is estimated to range from 6% to 30%, depending on the method of analysis and population studied (14) (Figure 1).
NAFLD ranges from benign hepatosteatosis to NASH (15), which is defined as hepatosteatosis with inflammation and hepatic injury (16). Approximately 30–40% of patients with steatosis develop NASH (17), representing ∼3–5% in the general population (14). NAFLD and NASH have high prevalence (≥60%) in the population with T2D (18). Patients undergoing bariatric surgery have NAFLD (93%) or NASH (26%) (19). Patients with NASH have higher mortality rates than patients with NAFLD, and both are higher than in the general population (20–22). Over a 10-y period, cirrhosis and liver-related death occurs in 20% and 12% of patients with NASH, respectively (23). Given the increasing prevalence of NASH and its adverse clinical outcome, NASH is rapidly becoming an important public health burden. NASH can progress to cirrhosis and HCC (8, 17). By the year 2020, cirrhosis resulting from NASH is projected to be the leading cause of liver transplantation in the United States (24).
Multi-Hit Hypotheses for NASH Development
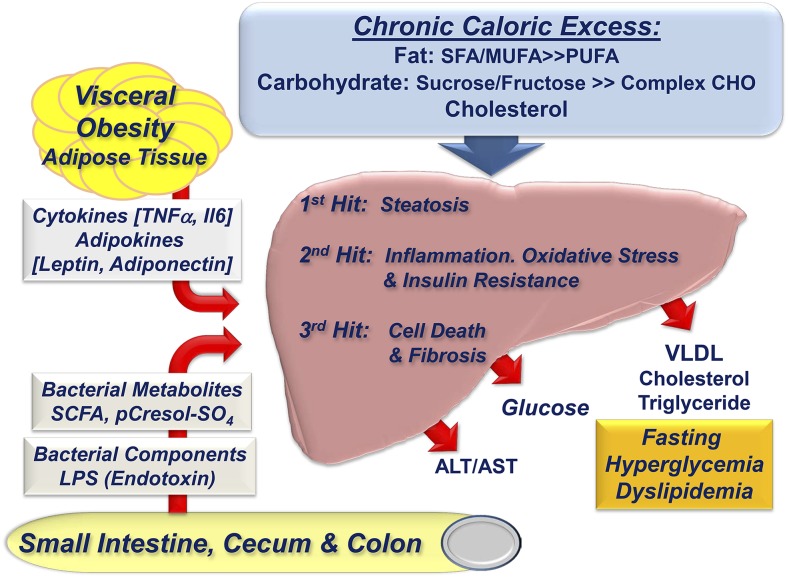
The development of NASH was proposed to follow a multi-hit model (25–27). The first hit involves excessive neutral lipid accumulation in the liver which sensitizes the liver to the second hit (26) (Figure 2). The second hit is characterized by hepatic inflammation, oxidative stress, and hepatic insulin resistance. These events promote hepatic damage that is associated with increased blood concentrations of hepatic enzymes/proteins (alanine aminotransferase, aspartate aminotransferase, C-reactive protein, serum amyloid A1, and plasminogen activator inhibitor-1) (7, 8, 28). This proinflammatory state leads to hepatocellular death and necrosis (necroinflammation), and cell death promotes fibrosis, that is, the third hit. Fibrosis is mediated by activation of hepatic stellate cells and myofibrillar cells; these cells produce extracellular matrix proteins, such as collagen [collagen 1A1 gene, (Col1A1)] and smooth muscle α2 actin (29). Dietary (excess fat, cholesterol, glucose, and fructose), metabolic (plasma and hepatic FA profiles, hepatic ceramide, oxidized LDL), endocrine/paracrine (insulin, leptin, adiponectin, and TGF-β), gut (endotoxin, microbial metabolites), and genetic (e.g., patatin-like phospholipase domain containing 3 polymorphisms) factors contribute to NASH progression (30–38).
FIGURE 2.
Factors contributing to the onset and progression of NASH. ALT, alanine aminotransferase; AST, aspartate aminotransferase; CHO, carbohydrate; NASH, nonalcoholic steatohepatitis.
Hepatosteatosis develops because of an imbalance of hepatic lipid metabolism that leads to the accumulation of hepatic neutral lipids as TGs and diacylglycerols and cholesterol esters. FA sources of hepatic TGs and cholesterol esters include nonesterified FAs mobilized from adipose tissue, de novo lipogenesis (DNL), and the diet via the portal circulation. Hepatic FA oxidation and VLDL assembly and secretion represent 2 pathways for removal of fat from the liver. Hepatosteatosis develops when lipid storage exceeds lipid export and oxidation (39). In humans with NAFLD, ∼60% of the FAs appearing in the liver are derived from circulating nonesterified FAs mobilized from adipose tissue; 26% are from DNL and 15% from diet (40). Both hepatic and peripheral insulin resistance also contribute to the disruption of these pathways and to the development of hepatosteatosis (39).
Patients with NASH consume a lower ratio of PUFAs to SFAs than the general population (41, 42). Consumption of a low ratio of ω-3 PUFAs to ω-6 PUFAs is also associated with NAFLD development, whereas increased dietary long-chain ω-3 PUFAs decrease hepatic steatosis (43–45). Mice fed a ω-3 PUFA-deficient diet developed hepatosteatosis and insulin resistance (46). Livers of these mice showed a major decline in α-linolenic acid (18:3ω-3), EPA (20:5ω-3), and DHA (22:6ω-3), but no change in hepatic ω-6 PUFAs, such as linoleic acid (18:2ω-6) or arachidonic acid (20:4ω-6). Depletion of hepatic ω-3 PUFAs lowered FA oxidation, a PPARα-regulated mechanism, and increased DNL and TG accumulation, which are sterol regulatory element binding protein 1, carbohydrate regulatory element binding protein, and max-like factor X-regulated pathways. PPARα, sterol regulatory element binding protein 1, and the carbohydrate regulatory element binding protein/max-like factor X heterodimer are well-established targets of 20–22-carbon ω-3 PUFA control (47). Although trans-FA (TFA) consumption is associated with insulin resistance and cardiovascular disease, the impact of TFA consumption on NAFLD in humans is less clear (48). Studies that used mice suggest that TFA consumption is associated with hepatic steatosis and injury (49, 50). Thus, reduced hepatic ω-3 PUFAs and increased concentrations of TFAs may account for changes in hepatic lipid metabolism that promote NAFLD.
Excess dietary cholesterol contributes to NASH (51) by promoting hepatic inflammation (32, 52–54). In the global ablation of the LDL receptor gene (Ldlr−/−) mouse model, high-fat/high-cholesterol diets promote NASH (55). Kupffer cells, that is, resident hepatic macrophage, become engorged with oxidized-LDL which induces inflammatory cytokine secretion. These locally secreted cytokines act on neighboring hepatic cells to promote a proinflammatory state, leading to cell injury. Kupffer cells also secrete chemokines [monocyte chemoattractant protein-1 gene, (MCP1)] that recruit monocytes to the liver, further amplifying hepatic inflammation. Controlling hepatic inflammation is an attractive target for NASH management and therapy.
Excessive consumption of simple sugar was implicated in hepatosteatosis and NASH progression. Over the past 30 y there was a dramatic increase in obesity and NAFLD in the United States. Although total fat consumption has remained steady, carbohydrate and total caloric intake have increased (56–60). As such, elevated carbohydrate and specifically fructose consumption were linked to NAFLD and NASH progression (61–63). The liver expresses the fructose-specific transporter (glucose transporter 5 gene). Moreover, the liver metabolizes up to 70% of dietary fructose (62, 63), and fructose metabolism is independent of insulin regulation. Compared with glucose, fructose more readily enters the pathways for DNL and TG synthesis. Fructose promotes all aspects of MetS, including hepatosteatosis, insulin resistance, dyslipidemia, hyperglycemia, obesity, and hypertension. In contrast to fructose, hepatic glucose metabolism is well regulated by insulin in healthy individuals, and glucose is converted to glycogen for storage. Excess glucose consumption does not promote hepatosteatosis as aggressively as excess fructose consumption. Fructose also affects several biochemical events that exacerbate NASH development, including formation of advanced glycation end-products and reactive oxygen species (64–67).
Development of Mouse Models of NASH
Several mouse models of NAFLD and NASH were developed. Four such models include the genetic models (ob/ob and db/db mice), a dietary model (methionine-choline–deficient diets), and chemically induced model (intraperitoneal carbon tetrachloride) (68, 69). These models recapitulate some aspects of human NAFLD/NASH but not other aspects of the disease. Ldlr−/− mice develop hypercholesteremia because of elevated plasma VLDL and LDL when fed a high-cholesterol diet (70). Although Ldlr−/− mice were used to study atherosclerosis, we and others observed that when Ldlr−/− mice are fed a high-fat/high-cholesterol diet, such as the Western diet (WD), mice develop a NASH phenotype similar to that seen in humans (32, 36, 54, 71–74). Because humans and Ldlr−/− mice develop NAFLD and NASH in a context of obesity and insulin resistance, these mice appear to be a useful preclinical model to investigate the development, progression, and remission of NASH.
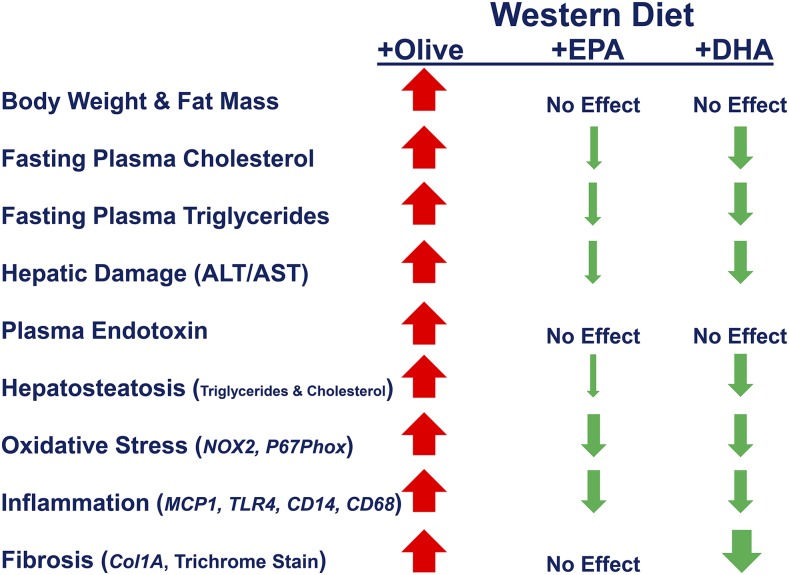
The WD (Research Diets; D12079B) used in our studies is moderately high in saturated and trans-fat (41% total calories), sucrose (30% total calories), and cholesterol (0.15 g%, wt:wt) and is similar to the fast-food diet (75) and human diets linked to obesity in the United States (76, 77). Both the WD and fast-food mouse models induced a NASH phenotype that recapitulates many of the clinical features of human NASH with MetS, including dyslipidemia, hyperglycemia, hepatosteatosis, hepatic damage (plasma alanine aminotransferase and aspartate aminotransferase), hepatocyte ballooning, induction of hepatic markers of inflammation (MCP1), oxidative stress [NADPH oxidase 2 gene (NOX2) and other NOX components], and fibrosis (TGF-β1 gene, proCol1A1, tissue inhibitor of metalloprotease-1 gene) (54, 73, 75, 78–80) (Figure 3). Moreover, NASH is associated with a major enrichment of both plasma and liver with SFAs and MUFAs and depletion of hepatic ω-3 PUFAs (54, 73, 78). The development of this phenotype was attributed to a diet high in saturated and trans-fat, sucrose, and cholesterol (32, 52–55, 62, 71–74, 81, 82).
FIGURE 3.
Effects of the Western diet and 20–22-carbon ω-3 PUFAs on the prevention of NASH Ldlr−/− mice. The size of the arrow indicates effect size. No effect indicates no changes from WD + olive oil-fed mice. Olive oil was added to the WD to keep all diets isocaloric. ALT, alanine aminotransferase; AST, aspartate aminotransferase; CD14, CD14 molecule gene; CD68, CD68 molecule gene; Col1A, collagen 1A1 gene; Ldlr−/−, global ablation of the LDL receptor gene; MCP1, monocyte chemoattractant protein-1; NASH, nonalcoholic steatohepatitis; NOX2, NADPH oxidase 2 gene; P67Phox, 67 kDa neutrophil cytosolic factor 2; TLR4, toll-like receptor 4 gene; WD, Western diet.
Potential for Dietary 20–22-Carbon ω-3 PUFAs to Prevent NASH
20–22-Carbon ω-3 PUFAs are pleiotropic regulators of cell function; they have well-established effects on membrane structure, cell signaling, gene expression, lipid and carbohydrate metabolism, and inflammation (47). As such, these FAs appear to be an ideal bioactive nutrient to combat NASH. A meta-analysis of 9 clinical studies indicated that dietary supplementation with 20–22-carbon ω-3 PUFAs decreased liver fat (83), and clinical trials suggest 20–22-carbon ω-3 PUFAs may lower liver fat in children and adults with NAFLD (84–89). Of 235 clinical trials that assessed NASH and NASH therapies (90), 23 trials used 20–22-carbon ω-3 PUFAs as a treatment strategy. In most trials, diets were supplemented with fish oil or a combination of EPA + DHA; few studies used EPA or DHA alone.
Preclinical assessment of the efficacy of ω-3 PUFA supplementation to prevent NASH in Ldlr−/− mice.
Diets supplemented with fish oil, EPA, or DHA prevent high-fat diet-induced NASH to varying degrees (47, 54, 73, 78). The amount of EPA and DHA in these high-fat diets was at ∼2% of total calories. This dose of 20–22-carbon ω-3 PUFAs is comparable with the dose consumed by patients taking Lovaza (GlaxoSmithKline) for the treatment of dyslipidemia (91). Humans who consumed EPA + DHA ethyl esters (4 g/d for 12 wk) showed increased plasma EPA + DHA from 5.5 mol% before treatment to 16.2 mol% after treatment (92). Supplementing human diets with a DHA-enriched fish oil (6 g/d for 8 wk) increased plasma DHA from 4 mol% before treatment to 8 mol% after treatment (93, 94). Plasma concentrations of DHA and total 20–22-carbon ω-3 PUFAs [EPA, docosapentaenoic acid (22:5ω-3), and DHA] in Ldlr−/− mice fed a WD for 16 wk was 4.3 and 6.7 mol%, respectively. Feeding Ldlr−/− mice a WD that contained DHA (at 2% total calories) for 16 wk increased plasma DHA and total 20–22-carbon ω-3 PUFAs to 9 and 15.2 mol%, respectively. Our protocol for 20–22-carbon ω-3 PUFA supplementation of diets yields a change in blood 20–22-carbon ω-3 PUFAs that is comparable with that seen in humans who consumed 4–6 g 20–22-carbon ω-3 PUFAs/d.
Dietary ω-3 PUFAs do not prevent WD-induced systemic inflammation.
Systemic inflammation is a main driver of NASH. Inflammatory signals that affect NASH progression include gut-derived microbial products (e.g., endotoxin/LPS, oxidized LDL (34, 55, 80, 95), adipokines (leptin and adiponectin) and cytokines (TNFα) (96), and products from hepatocellular death (27, 97) (Figure 2). Supplementation of the WD with either EPA or DHA does not attenuate WD-induced endotoxinemia (78). The appearance of endotoxin in the plasma of WD-fed Ldlr−/− mice (98) may represent a problem with gut physiology such as microbial overgrowth, increased gut permeability (leaky gut), or cotransport of microbial lipids with chylomicron (34, 98–100). A link between the gut microbiome and NAFLD was established (34, 101, 102).
ω-3 PUFAs attenuate hepatic inflammation.
Despite the absence of an effect of 20–22-carbon ω-3 PUFAs on systemic inflammation markers, such as endotoxin, gene expression analyses showed that DHA was more effective than EPA at attenuating WD-induced expression of hepatic toll-like receptor gene (TLR) subtypes (TLR2, TLR4, TLR9), CD14 molecule gene (CD14; binds endotoxin), downstream targets of TLRs, such as NF-κB (p50 subunit) nuclear abundance and downstream targets of NF-κB such as chemokines (MCP1), cytokines (IL-1β gene), inflammasome components (nucleotide-binding domain, leucine-rich containing family, pyrin domain containing protein 3 gene), and oxidative stress (NOX2, and its subunits) markers (73, 78). These studies suggest that EPA and DHA attenuate the hepatic (cellular) response to plasma inflammatory factors by downregulating key cellular mediators of inflammation, such as TLRs, CD14 (binds LPS, effect on CD14 mRNA and protein), NF-κB-p50 nuclear abundance.
ω-3 PUFAs have selective effects on hepatic oxidative stress.
Hepatic oxidative stress increases with NASH and is reflected by a substantial increase in gene expression and metabolite markers of oxidative stress that appear in liver and urine (54, 73). A response to increased oxidative stress is the induction of nuclear factor (erythroid-derived 2)-like 2 (Nrf2), a key transcription factor involved in the antioxidant response (78). Nrf2 regulates the expression of multiple transcripts linked to the antioxidant stress response, such as hemeoxygenase 1 and glutathione S-transferase α 1 genes and several NOX subunits. Adding EPA or DHA to the WD did not prevent the WD-mediated increase in hepatic nuclear content of Nrf2 or expression of hemeoxygenase 1 or glutathione S-transferase α 1 gene. The EPA- and DHA-containing diets, however, significantly lowered WD-mediated induction of multiple NOX subunits (Nox2, P22phox, P40phox, and P67phox) (73). NOX subtypes are a main source of superoxide and hydrogen peroxide. As such, the NOX pathway is a main target of WD and 20–22-carbon ω-3 PUFAs.
ω-3 PUFAs attenuate hepatic fibrosis.
Hepatic fibrosis (scarring) develops as a result of cell death and activation of hepatic stellate cells and myofibrillar cells to produce extracellular matrix proteins. Key regulators of fibrosis include TGF-β, connective tissue growth factor, platelet-derived growth factor, NOX, inflammatory mediators (endotoxin, TLR agonist), and leptin (38, 80, 103). A fibrotic liver can progress to a cirrhotic liver (Figure 1), and 90% of HCCs arise from cirrhotic livers (104).
Addition of DHA to the WD attenuated the WD-mediated fibrosis as quantified by suppression of expression of Col1A1, tissue inhibitor of metalloprotease 1 gene, TGF-β1 gene, plasminogen activated inhibitor-1 gene, and staining of liver for fibrosis with the use of trichrome, a collagen stain (54, 73). Interestingly, EPA did not prevent WD-induced fibrosis. On the basis of these studies, DHA is the preferred ω-3 PUFA to prevent NASH-associated fibrosis.
WD and 20–22-Carbon ω-3 PUFAs affect all major hepatic metabolic pathways.
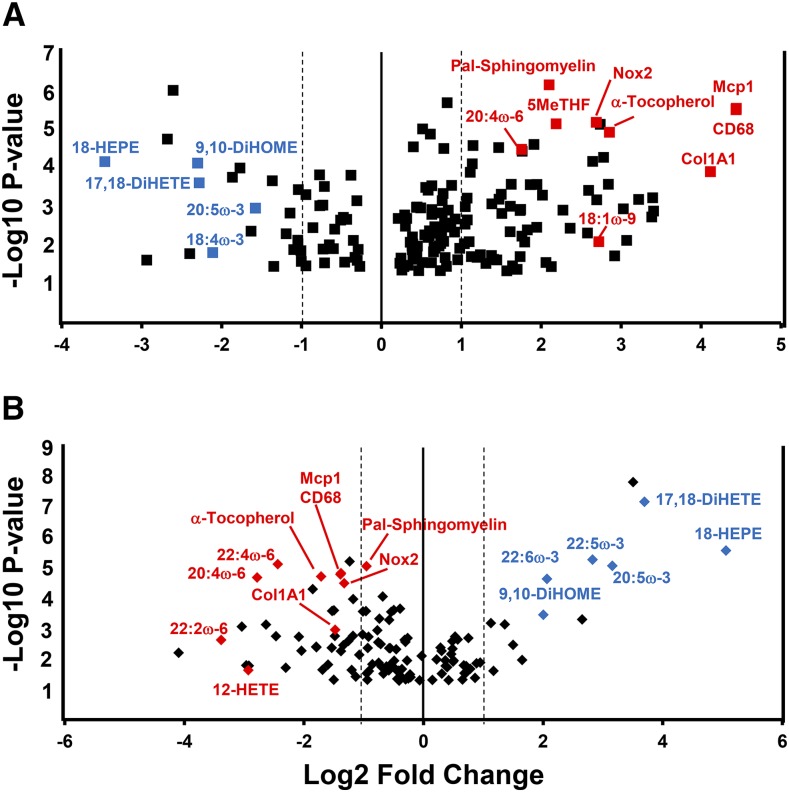
The impact of the WD and 20–22-carbon ω-3 PUFAs on liver metabolism was studied by using a global nontargeted metabolomic approach. The analysis identified 320 known biochemicals (78). Compared with mice fed an unpurified diet, both the WD + olive oil- and WD + DHA-containing diets significantly affected the abundance of metabolites in all major hepatic metabolic pathways, including amino acids and peptides, carbohydrate and energy, lipid, nucleotide, and vitamins and cofactors. Our studies have identified gene expression and metabolite signatures for NASH (73, 78). The gene expression signature for NASH includes increased expression of chemokines (MCP1), Kupffer cell surface marker (CD68 molecule gene), TLRs and their components (TLR4, CD14), enzymes involved in oxidative stress (NOX2), stearoyl CoA desaturase 1 gene, and collagen (Col1A1). The metabolomic signature for NASH includes increased hepatic content of palmitoyl-sphingomyelin, MUFAs (16:1ω-7, 18:1ω-7, and 18:1ω-9), α-tocopherol (vitamin E), 5-methyl tetrahydrofolate and decreased hepatic content of EPA, DHA, and oxidized lipids derived from EPA, specifically 18-hydroxyeicosapentaenoic acid (18-HEPE) and 17,18-dihydroxyeicosatetraenoic acid (17,18-DiHETE). A volcano plot of the metabolomic and gene expression data illustrates the impact of diet on the hepatic amount of these molecules (Figure 4). The metabolites and mRNAs that comprise the metabolomic and gene expression signature were changed dramatically by the WD + olive oil diet, compared with mice fed the unpurified diet. These changes were reversed in mice fed the WD + DHA diet.
FIGURE 4.
Volcano plots of WD effects on hepatic metabolites. A metabolomic and transcriptomic analysis was performed as described (78). More than 300 hepatic metabolites and 6 mRNA markers of NASH were examined with the use of MetaboAnalyst 3.0 (http://www.metaboanalyst.ca/MetaboAnalyst/) (105). The outcome of this analysis provided a volcano plot. Results are plotted as log2 fold change vs. log10 P value. Several metabolites and RNA transcripts are labeled to illustrate the impact of diet on hepatic abundance of these molecules. (A) The comparison of hepatic molecules from unpurified diet-fed compared with WD + olive oil-fed Ldlr−/− mice. (B) The comparison of hepatic molecules from WD + olive oil-fed mice compared with WD + DHA-fed Ldlr−/− mice. CD68, CD68 molecule; Col1A1, collagen 1A1; Ldlr−/−, global ablation of the LDL receptor gene; Mcp1, monocyte chemoattractant protein 1; NASH, nonalcoholic steatohepatitis; Nox2, NADPH oxidase 2; WD, Western diet; 5-MeTHF, 5-methyl tetrahydrofolate; 9,10-DiHOME, 9,10-dihydroxy-12Z-octadecenoic acid; 17,18-DiHETE, 17,18-dihydroxy-eicosatetraenoic acid; 18-HEPE, 18-hydroxy-eicosapentaenoic acid.
The oxidized lipids identified in these studies are generated by enzymatic and nonenzymatic processes. 18-HEPE is a resolvin E1 precursor, and resolvins are anti-inflammatory oxidation products of EPA (106). 17,18-DiHETE is an oxidized lipid generated first by cytochrome P450 2C-catalyzed formation of 17,18-epoxy-eicosatetraenoic acid from EPA; this epoxy FA is converted to the di-hydroxy FA by a epoxide hydrolase to form 17,18-DiHETE. The metabolomic analysis did not detect the 17,18- epoxy-eicosatetraenoic acid, suggesting that this lipid does not accumulate as a nonesterified lipid. Compared with mice fed the unpurified diet, WD + olive oil-fed mice have >60% reduction in hepatic content of 18-HEPE and 17,18-DiHETE. Compared with WD + olive oil-fed mice hepatic amounts of 18-HEPE and 17,18-DiHETE increased ≥40-fold in mice fed the WD that contained EPA or DHA. These dramatic changes in oxidized derivatives of EPA are inversely associated with the severity of NASH. A recent report suggest the Cyp450 epoxygenase pathway may play a key role in regulating hepatic inflammation in fatty liver disease (107). As such, the generation of these oxidized ω-3 PUFAs may be hepatoprotective.
Can ω-3 PUFAs Be Used to Treat Human NASH?
Therapeutic strategies for human NASH start with lifestyle management (diet and exercise) and treating the comorbidities associated with NASH, that is, obesity, T2D, and dyslipidemia. The best strategy for managing NASH, however, has not been established (108). Some clinical approaches to manage NASH included 1) reduce overall body weight through diet management, exercise, or bariatric surgery; 2) pharmaceutical and dietary supplements, that is, metformin, fibrates, thiazolidinediones, statins, ω-3 PUFAs; 3) suppress inflammation with the use of TLR modifiers or ω-3 PUFAs; and 4) suppress oxidative stress with the use of vitamin E, silybin, and other antioxidants (84, 109–114). Therapeutic regulators of fibrosis, however, are less well defined (80, 115).
Several clinical trials have reported that ω-3 PUFAs lower hepatic fat in obese children and adults with NAFLD (84–89, 116, 117), whereas others report that fish oil (116) and EPA-ethyl esters (117) do not attenuate the histologic features of the disease, such as fibrosis. As such, human studies with the use of ω-3 PUFAs to treat NAFLD/NASH have yielded mixed results.
The Ldlr−/− mouse studies described in the sections above suggest that ω-3 PUFAs may be an attractive dietary supplement to combat NAFLD and NASH, with the added benefit of preventing NASH-associated HCC. These FAs have well-defined effects on hepatic lipid metabolism and inflammation (47, 118) and more recently hepatic fibrosis (54, 73, 90). Although several human studies have provided evidence in support of using supplemental ω-3 PUFAs to treat NAFLD (84–89, 116, 117), some studies suggest there may be limitations to the use of ω-3 PUFAs to treat NASH (116, 117). For example, in a recent double-blind, placebo-controlled trial (89), NAFLD patients received placebo or Lovaza (GlaxoSmithKline) at 4 g/d (∼50:50 mix of EPA- and DHA-ethyl esters) for 15–18 mo. Compared with the placebo-treated group, the Lovaza-treated group showed a substantial reduction in liver fat without a substantial reduction in fibrosis scores.
Because DHA attenuates fibrosis in 2 separate rodent models of liver injury, that is, WD-induced fibrosis in mice and bile duct ligation-induced fibrosis in rats (54, 73, 119), we speculate that failure of 20–22-carbon ω-3 PUFAs to decrease hepatic fibrosis in humans may be explained by study design. Likely explanations include the type and amount of ω-3 PUFAs used in the trial. Our studies established that DHA is more effective than EPA at attenuating the onset and progression of NASH (73). Human studies, however, have examined the impact of ω-3 PUFAs on patients with preexisting disease (84–89, 116, 117). We are unaware of preclinical rodent studies that have assessed the impact of ω-3 PUFAs to promote remission or regression of NASH or hepatic fibrosis. As such, more preclinical studies are required to establish the capacity of ω-3 PUFAs to attenuate NASH at various stages in the disease process.
Conclusions and Key Unanswered Questions
To date, several human studies have indicated that ω-3 PUFAs may be useful in reducing liver fat in obese patients with NAFLD. Moreover, preclinical studies in mice have established that DHA can prevent NASH and NASH-associated fibrosis. It remains unclear whether dietary ω-3 PUFAs have the capacity to reverse the NASH, cirrhosis, or HCC phenotypes once these diseases are established. Equally important is defining the molecular mechanisms for DHA control of hepatic fibrosis. Finally, changes in hepatic EPA and DHA content significantly affect oxidized lipids derived from ω-3 and ω-6 PUFAs. These oxidized lipids likely play a role in inflammation and will affect the onset and progression of NASH. Whether these oxidized lipids affect the development of NASH, cirrhosis, or HCC remains to be determined.
Acknowledgments
All authors read and approved the final manuscript.
Footnotes
Abbreviations used: CD14, CD14 molecule gene; Col1A1, collagen 1A1 gene; DNL, de novo lipogenesis; HCC, hepatocellular carcinoma; MCP1, monocyte chemoattractant protein 1 gene; MetS, metabolic syndrome; NAFLD, nonalcoholic fatty liver disease; NASH, nonalcoholic steatohepatitis; NOX2, NADPH oxidase 2 gene; Nrf2, nuclear factor (erythroid-derived 2)-like 2; TLR, toll-like receptor; T2D, type 2 diabetes; WD, Western diet; 17,18-DiHETE, 17,18-dihydroxy-eicosatetraenoic acid; 18-HEPE, 18-hydroxy-eicosapentaenoic acid.
References
- 1.Bosetti C, Turati F, Vecchia CL. Hepatocellular carcinoma epidemiology. Best Pract Res Clin Gastroenterol 2014;28:753–70. [DOI] [PubMed] [Google Scholar]
- 2.Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet 2012;379:1245–55. [DOI] [PubMed] [Google Scholar]
- 3.Sanyal AJ, Yoon SK, Lencioni R. The etiology of hepatocellular carcinoma and consequences for treatment. Oncologist 2010;15(Suppl 4):14–22. [DOI] [PubMed] [Google Scholar]
- 4.Freedman ND, Marrero JA. Can dietary fish intake prevent liver cancer? Gastroenterology 2012;142:1411–3. [DOI] [PubMed] [Google Scholar]
- 5.Adult Obesity Facts [Internet]. Atlanta: CDC, Division of Nutrition, Physical Activity, and Obesity [updated 2015 Jun 16; cited 2015 Aug 5]. Available from: http://www.cdc.gov/obesity/data/adult.html.
- 6.Childhood Obesity Facts [Internet]. Atlanta: CDC, Division of Nutrition, Physical Activity, and Obesity [updated 2015 Jun 19; cited 2015 Aug 5]. Available from: http://www.cdc.gov/obesity/data/childhood.html.
- 7.Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology 2006;43:S99–112. [DOI] [PubMed] [Google Scholar]
- 8.Cohen JC, Horton JD, Hobbs HH. Human fatty liver disease: old questions and new insights. Science 2011;332:1519–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bellentani S, Scaglioni F, Marino M, Bedogni G. Epidemiology of non-alcoholic fatty liver disease. Dig Dis 2010;28:155–61. [DOI] [PubMed] [Google Scholar]
- 10.Angulo P, Lindor KD. Non-alcoholic fatty liver disease. J Gastroenterol Hepatol 2002;17(Suppl):S186–90. [DOI] [PubMed] [Google Scholar]
- 11.Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology 2003;37:1202–19. [DOI] [PubMed] [Google Scholar]
- 12.Kim CH, Younossi ZM. Nonalcoholic fatty liver disease: a manifestation of the metabolic syndrome. Cleve Clin J Med 2008;75:721–8. [DOI] [PubMed] [Google Scholar]
- 13.Alberti KG, Zimmet P, Shaw J. The metabolic syndrome–a new worldwide definition. Lancet 2005;366:1059–62. [DOI] [PubMed] [Google Scholar]
- 14.Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther 2011;34:274–85. [DOI] [PubMed] [Google Scholar]
- 15.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med 2002;346:1221–31. [DOI] [PubMed] [Google Scholar]
- 16.Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ; American Gastroenterological Association; American Association for the Study of Liver Diseases; American College of Gastroenterology. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology 2012;142:1592–609. [DOI] [PubMed] [Google Scholar]
- 17.McCullough AJ. Pathophysiology of nonalcoholic steatohepatitis. J Clin Gastroenterol 2006;40(Suppl 1):S17–29. [DOI] [PubMed] [Google Scholar]
- 18.Prashanth M, Ganesh HK, Vima MV, John M, Bandgar T, Joshi SR, Shah SR, Rathi PM, Joshi AS, Thakkar H, et al. . Prevalence of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus. J Assoc Physicians India 2009;57:205–10. [PubMed] [Google Scholar]
- 19.Ong JP, Elariny H, Collantes R, Younoszai A, Chandhoke V, Reines HD, Goodman Z, Younossi ZM. Predictors of nonalcoholic steatohepatitis and advanced fibrosis in morbidly obese patients. Obes Surg 2005;15:310–5. [DOI] [PubMed] [Google Scholar]
- 20.Söderberg C, Stål P, Askling J, Glaumann H, Lindberg G, Marmur J, Hultcrantz R. Decreased survival of subjects with elevated liver function tests during a 28-year follow-up. Hepatology 2010;51:595–602. [DOI] [PubMed] [Google Scholar]
- 21.Ekstedt M, Franzen LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, Kechagias S. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology 2006;44:865–73. [DOI] [PubMed] [Google Scholar]
- 22.Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology 2005;129:113–21. [DOI] [PubMed] [Google Scholar]
- 23.McCullough AJ. The clinical features, diagnosis and natural history of nonalcoholic fatty liver disease. Clin Liver Dis 2004;8:521–33. [DOI] [PubMed] [Google Scholar]
- 24.McCullough AJ. Epidemiology of the metabolic syndrome in the USA. J Dig Dis 2011;12:333–40. [DOI] [PubMed] [Google Scholar]
- 25.Day CP, James OF. Steatohepatitis: a tale of two “hits”? Gastroenterology 1998;114:842–5. [DOI] [PubMed] [Google Scholar]
- 26.LaBrecque D, Abbas Z, Anania F, Ferenci P, Gahafoor Kahn A, Goh K-L, Hamid SS, Isakov V, Lizarzabal M, Mojica Pernaranda M, et al. . Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. World Gastroenterology Organisation Global Guidelines. Milwaukee (WI): The Organisation; 2012. [DOI] [PubMed] [Google Scholar]
- 27.Tilg H, Moschen AR. Evolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology 2010;52:1836–46. [DOI] [PubMed] [Google Scholar]
- 28.Hashimoto E, Tokushige K, Farrell GC. Histological features of non-alcoholic fatty liver disease: what is important? J Gastroenterol Hepatol 2012;27:5–7. [DOI] [PubMed] [Google Scholar]
- 29.Friedman SL. Mechanisms of hepatic fibrogenesis. Gastroenterology 2008;134:1655–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abdelmalek MF, Suzuki A, Guy C, Unalp-Arida A, Colvin R, Johnson RJ, Diehl AM. Increased fructose consumption is associated with fibrosis severity in patients with nonalcoholic fatty liver disease. Hepatology 2010;51:1961–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guturu P, Duchini A. Etiopathogenesis of nonalcoholic steatohepatitis: role of obesity, insulin resistance and mechanisms of hepatotoxicity. Int J Hepatol. 2012;2012:212865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wouters K, van Gorp PJ, Bieghs V, Gijbels MJ, Duimel H, Lutjohann D, Kerksiek A, van Kruchten R, Maeda N, Staels B, et al. . Dietary cholesterol, rather than liver steatosis, leads to hepatic inflammation in hyperlipidemic mouse models of nonalcoholic steatohepatitis. Hepatology 2008;48:474–86. [DOI] [PubMed] [Google Scholar]
- 33.Pagadala M, Kasumov T, McCullough AJ, Zein NN, Kirwan JP. Role of ceramides in nonalcoholic fatty liver disease. Trends Endocrinol Metab 2012;23:365–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harte AL, da Silva NF, Creely SJ, McGee KC, Billyard T, Youssef-Elabd EM, Tripathi G, Ashour E, Abdalla MS, Sharada HM, et al. . Elevated endotoxin levels in non-alcoholic fatty liver disease. J Inflamm (Lond) 2010;7:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hooper AJ, Adams LA, Burnett JR. Genetic determinants of hepatic steatosis in man. J Lipid Res 2011;52:593–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bieghs V, Van Gorp PJ, Wouters K, Hendrikx T, Gijbels MJ, van Bilsen M, Bakker J, Binder CJ, Lutjohann D, Staels B, et al. . LDL receptor knock-out mice are a physiological model particularly vulnerable to study the onset of inflammation in non-alcoholic fatty liver disease. PLoS One 2012;7:e30668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Joyce SA, MacSharry J, Casey PG, Kinsella M, Murphy EF, Shanahan F, Hill C, Gahan CGM. Regulation of host weight gain and lipid metabolism by bacterial bile acid modification in the gut. Proc Natl Acad Sci USA 2014;111:7421–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elinav E, Ali M, Bruck R, Brazowski E, Phillips A, Shapira Y, Katz M, Solomon G, Halpern Z, Gertler A. Competitive inhibition of leptin signaling results in amelioration of liver fibrosis through modulation of stellate cell function. Hepatology 2009;49:278–86. [DOI] [PubMed] [Google Scholar]
- 39.Matherly SC, Puri P. Mechanisms of simple hepatic steatosis: not so simple after all. Clin Liver Dis 2012;16:505–24. [DOI] [PubMed] [Google Scholar]
- 40.Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest 2005;115:1343–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Toshimitsu K, Matsuura B, Ohkubo I, Niiya T, Furukawa S, Hiasa Y, Kawamura M, Ebihara K, Onji M. Dietary habits and nutrient intake in non-alcoholic steatohepatitis. Nutrition 2007;23:46–52. [DOI] [PubMed] [Google Scholar]
- 42.Musso G, Gambino R, De Michieli F, Cassader M, Rizzetto M, Durazzo M, Faga E, Silli B, Pagano G. Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis. Hepatology 2003;37:909–16. [DOI] [PubMed] [Google Scholar]
- 43.Capanni M, Calella F, Biagini MR, Genise S, Raimondi L, Bedogni G, Svegliati-Baroni G, Sofi F, Milani S, Aggate R, et al. . Prolonged n-3 polyunsaturated fatty acid supplementation ameliorates hepatic steatosis in patients with non-alcoholic fatty liver disease: a pilot study. Aliment Pharmacol Ther 2006;23:1143–51. [DOI] [PubMed] [Google Scholar]
- 44.Cortez-Pinto H, Jesus L, Barros H, Lopes C, Moura MC, Camilo ME. How different is the dietary pattern in non-alcoholic steatohepatitis patients? Clin Nutr 2006;25:816–23. [DOI] [PubMed] [Google Scholar]
- 45.Levy JR, Clore JN, Stevens W. Dietary n-3 polyunsaturated fatty acids decrease hepatic triglycerides in Fischer 344 rats. Hepatology 2004;39:608–16. [DOI] [PubMed] [Google Scholar]
- 46.Pachikian BD, Essaghir A, Demoulin JB, Neyrinck AM, Catry E, De Backer FC, Dejeans N, Dewulf EM, Sohet FM, Portois L, et al. . Hepatic n-3 polyunsaturated fatty acid depletion promotes steatosis and insulin resistance in mice: genomic analysis of cellular targets. PLoS One 2011;6:e23365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jump DB, Tripathy S, Depner CM. Fatty acid-regulated transcription factors in the liver. Annu Rev Nutr 2013;33:249–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zelber-Sagi S, Ratziu V, Oren R. Nutrition and physical activity in NAFLD: an overview of the epidemiological evidence. World J Gastroenterol 2011;17:3377–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tetri LH, Basaranoglu M, Brunt EM, Yerian LM, Neuschwander-Tetri BA. Severe NAFLD with hepatic necroinflammatory changes in mice fed trans fats and a high-fructose corn syrup equivalent. Am J Physiol Gastrointest Liver Physiol 2008;295:G987–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lottenberg AM, Afonso Mda S, Lavrador MS, Machado RM, Nakandakare ER. The role of dietary fatty acids in the pathology of metabolic syndrome. J Nutr Biochem 2012;23:1027–40. [DOI] [PubMed] [Google Scholar]
- 51.Yasutake K, Nakamuta M, Shima Y, Ohyama A, Masuda K, Haruta N, Fujino T, Aoyagi Y, Fukuizumi K, Yoshimoto T, et al. . Nutritional investigation of non-obese patients with non-alcoholic fatty liver disease: the significance of dietary cholesterol. Scand J Gastroenterol 2009;44:471–7. [DOI] [PubMed] [Google Scholar]
- 52.Wouters K, van Bilsen M, van Gorp PJ, Bieghs V, Lutjohann D, Kerksiek A, Staels B, Hofker MH, Shiri-Sverdlov R. Intrahepatic cholesterol influences progression, inhibition and reversal of non-alcoholic steatohepatitis in hyperlipidemic mice. FEBS Lett 2010;584:1001–5. [DOI] [PubMed] [Google Scholar]
- 53.Teratani T, Tomita K, Suzuki T, Oshikawa T, Yokoyama H, Shimamura K, Tominaga S, Hiroi S, Irie R, Okada Y, et al. A high-cholesterol diet exacerbates liver fibrosis in mice via accumulation of free cholesterol in hepatic stellate cells. Gastroenterology 2012;142:152–64.e10. [DOI] [PubMed] [Google Scholar]
- 54.Depner CM, Torres-Gonzalez M, Tripathy S, Milne G, Jump DB. Menhaden oil decreases high-fat diet-induced markers of hepatic damage, steatosis, inflammation, and fibrosis in obese Ldlr−/− mice. J Nutr 2012;142:1495–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Walenbergh SMA, Koek GH, Bieghs V, Shiri-Sverdlov R. Non-alcoholic steatohepatitis: the role of oxidized low-density lipoproteins. J Hepatol 2013;58:801–10. [DOI] [PubMed] [Google Scholar]
- 56.Marriott BP, Olsho L, Hadden L, Connor P. Intake of added sugars in the United States: what is the measure? Am J Clin Nutr 2011;94:1652–3; author reply 3. [DOI] [PubMed] [Google Scholar]
- 57.Chun OK, Chung CE, Wang Y, Padgitt A, Song WO. Changes in intakes of total and added sugar and their contribution to energy intake in the U.S. Nutrients 2010;2:834–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chanmugam P, Guthrie JF, Cecilio S, Morton JF, Basiotis PP, Anand R. Did fat intake in the United States really decline between 1989–1991 and 1994–1996? J Am Diet Assoc 2003;103:867–72. [DOI] [PubMed] [Google Scholar]
- 59.Lee S, Harnack L, Jacobs DR Jr, Steffen LM, Luepker RV, Arnett DK. Trends in diet quality for coronary heart disease prevention between 1980–1982 and 2000–2002: the Minnesota Heart Survey. J Am Diet Assoc 2007;107:213–22. [DOI] [PubMed] [Google Scholar]
- 60.Marriott BP, Olsho L, Hadden L, Connor P. Intake of added sugars and selected nutrients in the United States, National Health and Nutrition Examination Survey (NHANES) 2003–2006. Crit Rev Food Sci Nutr 2010;50:228–58. [DOI] [PubMed] [Google Scholar]
- 61.Vos MB, Kimmons JE, Gillespie C, Welsh J, Blanck HM. Dietary fructose consumption among US children and adults: the Third National Health and Nutrition Examination Survey. Medscape J Med 2008;10:160. [PMC free article] [PubMed] [Google Scholar]
- 62.Lim JS, Mietus-Snyder M, Valente A, Schwarz JM, Lustig RH. The role of fructose in the pathogenesis of NAFLD and the metabolic syndrome. Nat Rev Gastroenterol Hepatol 2010;7:251–64. [DOI] [PubMed] [Google Scholar]
- 63.Bizeau ME, Pagliassotti MJ. Hepatic adaptations to sucrose and fructose. Metabolism 2005;54:1189–201. [DOI] [PubMed] [Google Scholar]
- 64.Schalkwijk CG, Stehouwer CD, van Hinsbergh VW. Fructose-mediated non-enzymatic glycation: sweet coupling or bad modification. Diabetes Metab Res Rev 2004;20:369–82. [DOI] [PubMed] [Google Scholar]
- 65.Bunn HF, Higgins PJ. Reaction of monosaccharides with proteins: possible evolutionary significance. Science 1981;213:222–4. [DOI] [PubMed] [Google Scholar]
- 66.Bose T, Chakraborti AS. Fructose-induced structural and functional modifications of hemoglobin: implication for oxidative stress in diabetes mellitus. Biochim Biophys Acta 2008; 1780:800–8. [DOI] [PubMed] [Google Scholar]
- 67.Wei Y, Wang D, Moran G, Estrada A, Pagliassotti MJ. Fructose-induced stress signaling in the liver involves methylglyoxal. Nutr Metab (Lond) 2013;10:32–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kucera O, Cervinkova Z. Experimental models of non-alcoholic fatty liver disease in rats. World J Gastroenterol 2014;20:8364–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Takahashi Y, Soejima Y, Fukusato T.. Animal models of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J Gastroenterol. 2012;18:2300–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ishibashi S, Brown MS, Goldstein JL, Gerard RD, Hammer RE, Herz J. Hypercholesterolemia in low density lipoprotein receptor knockout mice and its reversal by adenovirus-mediated gene delivery. J Clin Invest 1993;92:883–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Saraswathi V, Gao L, Morrow JD, Chait A, Niswender KD, Hasty AH. Fish oil increases cholesterol storage in white adipose tissue with concomitant decreases in inflammation, hepatic steatosis, and atherosclerosis in mice. J Nutr 2007;137:1776–82. [DOI] [PubMed] [Google Scholar]
- 72.Saraswathi V, Morrow JD, Hasty AH. Dietary fish oil exerts hypolipidemic effects in lean and insulin sensitizing effect in obese LDLR−/− mice. J Nutr 2009;139:2380–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Depner CM, Philbrick KA, Jump DB. Docosahexaenoic acid attenuates hepatic inflammation, oxidative stress, and fibrosis without decreasing hepatosteatosis in a Ldlr(−/−) mouse model of western diet-induced nonalcoholic steatohepatitis. J Nutr 2013;143:315–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Subramanian S, Goodspeed L, Wang S, Kim J, Zeng L, Ioannou GN, Haigh WG, Yeh MM, Kowdley KV, O'Brien KD, et al. . Dietary cholesterol exacerbates hepatic steatosis and inflammation in obese LDL receptor-deficient mice. J Lipid Res 2011;52:1626–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Charlton M, Krishnan A, Viker K, Sanderson S, Cazanave S, McConico A, Masuoko H, Gores G. Fast food diet mouse: novel small animal model of NASH with ballooning, progressive fibrosis and high physiological facility to the human condition. Am J Physiol Gastrointest Liver Physiol 2011;301:G825–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cordain L, Eaton SB, Sebastian A, Mann N, Lindeberg S, Watkins BA, O’Keefe JH, Brand-Miller J. Origins and evolution of the western diet: health implications for the 21st century. Am J Clin Nutr 2005;81:341–54. [DOI] [PubMed] [Google Scholar]
- 77.Ishimoto T, Lanaspa MA, Rivard CJ, Roncal-Jimenez CA, Orlicky DJ, Cicerchi C, McMahan RH, Abdelmalek MF, Rosen HR, Jackman MR, et al. . High-fat and high-sucrose (western) diet induces steatohepatitis that is dependent on fructokinase. Hepatology 2013;58:1632–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Depner CM, Traber MG, Bobe G, Bohren KM, Morin-Kensicki E, Milne G, Jump DB. A metabolomic analysis of omega-3 fatty acid mediated attenuation of western diet-induced non-alcoholic steatohepatitis in LDLR−/− mice. PLoS One 2013;8:e83756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Depner CM, Lytle K, Tripathy S, Jump DB. Omega-3 fatty acids and nonalcoholic fatty liver disease. In: Tirosh O, editor. Fatty liver diseases and consequences. Boca Raton (FL): CRC Press; 2014. p. 247–80. [Google Scholar]
- 80.Schuppan D, Kim YO. Evolving therapies for liver fibrosis. J Clin Invest 2013;123:1887–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nomura K, Yamanouchi T. The role of fructose-enriched diets in mechanisms of nonalcoholic fatty liver disease. J Nutr Biochem 2012;23:203–8. [DOI] [PubMed] [Google Scholar]
- 82.Nomura K, Yamanouchi T. The role of fructose-enriched diets in mechanisms of nonalcoholic fatty liver disease. J Nutr Biochem 2012;23:203–8. [DOI] [PubMed] [Google Scholar]
- 83.Parker HM, Johnson NA, Burdon CA, Cohn JS, O'Connor HT, George J. Omega-3 supplementation and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Hepatol 2012;56:944–51. [DOI] [PubMed] [Google Scholar]
- 84.Nobili V, Bedogni G, Alisi A, Pietrobattista A, Rise P, Galli C, Agostoni C. Docosahexaenoic acid supplementation decreases liver fat content in children with non-alcoholic fatty liver disease: double-blind randomised controlled clinical trial. Arch Dis Child 2011;96:350–3. [DOI] [PubMed] [Google Scholar]
- 85.Sofi F, Giangrandi I, Cesari F, Corsani I, Abbate R, Gensini GF, Casini A. Effects of a 1-year dietary intervention with n-3 polyunsaturated fatty acid-enriched olive oil on non-alcoholic fatty liver disease patients: a preliminary study. Int J Food Sci Nutr 2010;61:792–802. [DOI] [PubMed] [Google Scholar]
- 86.Bulchandani DG, Nachnani JS, Nookala A, Naumovitch C, Herndon B, Molteni A, Quinn T, Alba LM. Treatment with omega-3 fatty acids but not exendin-4 improves hepatic steatosis. Eur J Gastroenterol Hepatol 2010;22:1245–52. [DOI] [PubMed] [Google Scholar]
- 87.Ishikawa Y, Yokoyama M, Saito Y, Matsuzaki M, Origasa H, Oikawa S, Sasaki J, Hishida H, Itakura H, Kita T, et al. . Preventive effects of eicosapentaenoic acid on coronary artery disease in patients with peripheral artery disease. Circ J 2010;74:1451–7. [DOI] [PubMed] [Google Scholar]
- 88.Kishino T, Ohnishi H, Ohtsuka K, Matsushima S, Urata T, Watanebe K, Honda Y, Mine Y, Matsumoto M, Nishikawa K, et al. . Low concentrations of serum n-3 polyunsaturated fatty acids in non-alcoholic fatty liver disease patients with liver injury. Clin Chem Lab Med 2011;49:159–62. [DOI] [PubMed] [Google Scholar]
- 89.Scorletti E, Bhatia L, McCormick KG, Clough GF, Nash K, Hodson L, Moyses HE, Calder PC, Byrne CD; WELCOME Study. Effects of purified eicosapentaenoic and docosahexaenoic acids in non-alcoholic fatty liver disease: Results from the WELCOME* study. Hepatology 2014;60:1211–21. [DOI] [PubMed] [Google Scholar]
- 90.NASH [Internet]. Bethesda (MD): US NIH. [cited 2015 May 1]. Available from: https://www.clinicaltrials.gov/ct2/results?term=NASH+&Search=Search.
- 91.Barter P, Ginsberg HN. Effectiveness of combined statin plus omega-3 fatty acid therapy for mixed dyslipidemia. Am J Cardiol 2008;102:1040–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Di Stasi D, Bernasconi R, Marchioli R, Marfisi RM, Rossi G, Tognoni G, Tacconi MT. Early modification of fatty acid composition in plasma phospholipids, platelets and mononucleates of healthy volunteers after low doses of n-3 PUFA. Eur J Clin Pharmacol 2004;60:183–90. [DOI] [PubMed] [Google Scholar]
- 93.Superko HR, Superko SM, Nasir K, Agatston A, Garrett BC. Omega-3 fatty acid blood levels. Clinical significance and controversy. Circulation 2013;128:2154–61. [DOI] [PubMed] [Google Scholar]
- 94.Lockyer S, Tzanetou M, Carvalho-Wells AL, Jackson JG, Minihane AM, Lovegrove JA. STAT gene dietary model to implement diets of differing fat composition in prospectively genotyped groups (apoE) using commercially available foods. Br J Nutr 2012;108:1705–13. [DOI] [PubMed] [Google Scholar]
- 95.Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, Neyrinck AM, Fava F, Tuohy KM, Chabo C, et al. . Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 2007;56:1761–72. [DOI] [PubMed] [Google Scholar]
- 96.Leclercq IA, Farrell GC, Schriemer R, Robertson GR. Leptin is essential for the hepatic fibrogenic response to chronic liver injury. J Hepatol 2002;37:206–13. [DOI] [PubMed] [Google Scholar]
- 97.Marra F, Gastaldelli A, Baroni GS, Tell G, Tiribelli C. Molecular basis and mechanisms of progression of non-alcoholic steatohepatitis. Trends Mol Med 2008;14:72–81. [DOI] [PubMed] [Google Scholar]
- 98.Akira S, Takeda K. Toll-like receptor signalling. Nat Rev Immunol 2004;4:499–511. [DOI] [PubMed] [Google Scholar]
- 99.Erridge C, Attina T, Spickett CM, Webb DJ. A high-fat meal induces low-grade endotoxemia: evidence of a novel mechanism of postprandial inflammation. Am J Clin Nutr 2007;86:1286–92. [DOI] [PubMed] [Google Scholar]
- 100.Laugerette F, Vors C, Geloen A, Chauvin MA, Soulage C, Lambert-Porcheron S, Peretti N, Alligier M, Burcelin R, Laville M, et al. . Emulsified lipids increase endotoxemia: possible role in early postprandial low-grade inflammation. J Nutr Biochem 2011;22:53–9. [DOI] [PubMed] [Google Scholar]
- 101.Goel A, Gupta M, Aggarwal R. Gut microbiota and liver disease. J Gastroenterol Hepatol 2014;29:1139–48. [DOI] [PubMed] [Google Scholar]
- 102.Henao-Mejia J, Elinav E, Jin C, Hao L, Mehal WZ, Strowig T, Thaiss CA, Kau AL, Eisenbarth SC, Jurczak MJ, et al. . Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity. Nature 2012;482:179–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Brenner DA, Seki E, Taura K, Kisseleva T, Deminicis S, Iwaisako K, Inokuchi S, Schnabl B, Oesterreicher CH, Paik YH, et al. . Non-alcoholic steatohepatitis-induced fibrosis: Toll-like receptors, reactive oxygen species and Jun N-terminal kinase. Hepatol Res 2011;41:683–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Thompson AI, Conroy KP, Henderson NC. Hepatic stellate cells: central modulator of hepatic carcinogenesis. BMC Gastroenterol 2015; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Xia J, Sinelnikov I, Han B, Wishart DS. MetaboAnalyst 3.0-making metabolomics more meaningful. Nucleic Acids Res 2015;43:W251–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tjonahen E, Oh SF, Siegelman J, Elangovan S, Percarpio KB, Hong S, Arita M, Serhan CN. Resolvin E2: identification and anti-inflammatory actions: pivotal role of human 5-lipoxygenase in resolvin E series biosynthesis. Chem Biol 2006;13:1193–202. [DOI] [PubMed] [Google Scholar]
- 107.Schuck RN, Zha W, Edin ML, Gruzdev A, Vendrov KC, Miller TM, Xu A, Lih FB, DeGraff LM, Tomer KB, et al. . The cytochrome P450 epoxygenase pathway regulates the hepatic inflammatory response in fatty liver disease. PLoS One 2014;9:e110162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Chan HL, de Silva HJ, Leung NW, Lim SG, Farrell GC. How should we manage patients with non-alcoholic fatty liver disease in 2007? J Gastroenterol Hepatol 2007;22:801–8. [DOI] [PubMed] [Google Scholar]
- 109.Musso G, Cassader M, Rosina F, Gambino R. Impact of current treatments on liver disease, glucose metabolism and cardiovascular risk in non-alcoholic fatty liver disease (NAFLD): a systematic review and meta-analysis of randomised trials. Diabetologia 2012;55:885–904. [DOI] [PubMed] [Google Scholar]
- 110.Petit JM, Guiu B, Duvillard L, Jooste V, Brindisi MC, Athias A, Bouillet B, Habchi M, Cottet V, et al. . Increased erythrocytes n-3 and n-6 polyunsaturated fatty acids is significantly associated with a lower prevalence of steatosis in patients with type 2 diabetes. Clin Nutr 2012;31:520–5. [DOI] [PubMed] [Google Scholar]
- 111.Zheng JS, Xu A, Huang T, Yu X, Li D. Low docosahexaenoic acid content in plasma phospholipids is associated with increased non-alcoholic fatty liver disease in China. Lipids 2012;47:549–56. [DOI] [PubMed] [Google Scholar]
- 112.Parker HM, Johnson NA, Burdon CA, Cohn JS, O’Connor HT, George J. Omega-3 supplementation and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Hepatol 2012;56:944–51. [DOI] [PubMed] [Google Scholar]
- 113.Di Minno MN, Russolillo A, Lupoli R, Ambrosino P, Di Minno A, Tarantino G. Omega-3 fatty acids for the treatment of non-alcoholic fatty liver disease. World J Gastroenterol 2012;18:5839–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Shapiro H, Tehilla M, Attal-Singer J, Bruck R, Luzzatti R, Singer P. The therapeutic potential of long-chain omega-3 fatty acids in nonalcoholic fatty liver disease. Clin Nutr 2011;30:6–19. [DOI] [PubMed] [Google Scholar]
- 115.Cohen-Naftaly M, Friedman SL. Current status of novel antifibrotic therapies in patients with chronic liver disease. Therap Adv Gastroenterol 2011;4:391–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Argo CK, Patrie JT, Lackner C, Henry TD, de Lang EE, Weltman AL, Shah NL, Al-Osaimi AM, Pramoonjago P, Jayakumar S, et al. . Effects of n-3 fish oil on metabolic and histological parameters in NASH: a double-blind, randomized, placebo-controlled trial. J Hepatol 2015;62:190–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Sanyal AJ, Abdelmalek MF, Suzuki A, Cummings OW, Chojkier M. No significant effects of ethyl-eicosapentaenoic acid on histologic features of nonalcoholic steatohepatitis in a phase 2 trial. Gastroenterology 2014;147:377–84.e1. [DOI] [PubMed] [Google Scholar]
- 118.Calder PC. Mechanisms of action of (n-3) fatty acids. J Nutr 2012;142:592S–9S. [DOI] [PubMed] [Google Scholar]
- 119.Chen WY, Lin SY, Pan HC, Liao SL, Chuang YH, Yen YJ, Lin SY, Chen EJ. Beneficial effect of docosahexaenoic acid on cholestatic liver injury in rats. J Nutr Biochem 202:252–64. [DOI] [PubMed] [Google Scholar]