Abstract
Alzheimer disease is a multifactorial pathology and the development of new multitarget neuroprotective drugs is promising and attractive. We synthesized a group of original compounds, which combine in one molecule γ-carboline fragment of dimebon and phenothiazine core of methylene blue (MB) linked by 1-oxo- and 2-hydroxypropylene spacers. Inhibitory activity of the conjugates toward acetylcholinesterase (AChE), butyrylcholinesterase (BChE) and structurally close to them carboxylesterase (CaE), as well their binding to NMDA-receptors were evaluated in vitro and in silico. These newly synthesized compounds showed significantly higher inhibitory activity toward BChE with IC50 values in submicromolar and micromolar range and exhibited selective inhibitory action against BChE over AChE and CaE. Kinetic studies for the 9 most active compounds indicated that majority of them were mixed-type BChE inhibitors. The main specific protein-ligand interaction is π-π stacking of phenothiazine ring with indole group of Trp82. These compounds emerge as promising safe multitarget ligands for the further development of a therapeutic approach against aging-related neurodegenerative disorders such as Alzheimer and/or other pathological conditions.
The development of novel compounds that are able to modify the pathogenesis of neurodegenerative diseases appears to be as a promising approach among different drug discovery strategies in this emerging area1,2. Taking into account the multifactorial nature of neurodegenerative diseases3,4, focusing on the design of multitarget drugs that are capable to act simultaneously on different main biotargets, which are involved in the disease pathogenesis, seems to be very attractive and promising5,6,7,8. During the past decade, previous studies have indicated that the progression of Alzheimer disease (AD), amyotrophic lateral sclerosis (ALS) and some other neuropathological disorders is closely connected to dysfunctions in cholinergic and glutamatergic neuronal systems9,10,11,12. Nowadays, the main scheme for AD treatment is the use of three inhibitors of cholinesterase’s (donepezil, rivastigmine and galantamine) and low-affinity antagonist of NMDA-receptors—memantine13. The current standard of AD treatment recommends combination of AChE inhibitors with memantine13,14,15,16,17,18. Recently, it was shown that combining glutamatergic and cholinergic approaches in the symptomatic treatment of AD could be much more efficient17 compared to the single treatment option. In this regard, the design of new compounds that can interact with both of these neuromediator systems is more likely to confer better protection against neurodegeneration and therefore compensating the deficit of cholinergic and glutamatergic functions that appeared to be key features of these diseases19.
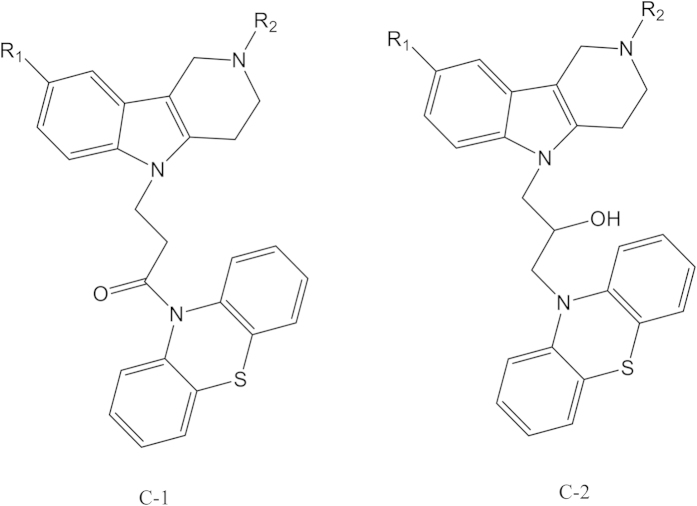
Recent studies showed that Dimebon (latreperdine) and methylene blue (MB) are able to protect neurons in different models of neurodegeneration20,21,22,23,24. Moreover, significant protective effects were observed in a vitro model of ALS when both compounds are administered simultaneously25. In this context, we previously synthesized a group of original compounds that combine γ-carboline fragment of dimebon and phenothiazine core of MB in the same structure26,27, as a novel approach to the development of multitarget disease-modifying agents (Fig. 1).
Figure 1. Structures of the studied conjugates of γ-carbolines and phenothiazine.
R1, R2 = Alkyl, F.
In the present work, we assessed the biological action of such compounds on the key targets of cholinergic and glutamatergic systems, in particular, acetylcholinesterase (EC 3.1.1.7, AChE), butyrylcholinesterase (EC 3.1.1.8, BChE) and structurally close to them, carboxylesterase (EC 3.1.1.1, CaE), as well on binding to NMDA-receptors. The background for selection of these biological targets were the results of the previous observations that phenothiazine derivatives including MB can effectively inhibit the enzymes of cholinesterase family28,29,30,31 and one of the target of dimebon neuronal action is the NMDA-receptor32.
Results
Inhibiting activity of conjugates of γ-carboline and phenothiazine against human erythrocyte AChE, equine serum BChE and porcine liver CaE
All γ-carboline-phenothiazine conjugates have been assessed as inhibitors of AChE and BChE, which are important for AD and/or AD-like dementia development and structurally close enzyme—CaE. CaE is responsible for hydrolysis of numerous ester-containing drugs33,34. Inhibition of CaE by anticholinesterase compounds leads to adverse drug-drug interactions35. AChE from human erythrocytes was used along with two enzymes of non-human origin, namely BuChE from horse serum and CaE from porcine liver because of their lower cost, high degree of identity with human enzymes and the exploratory character of this work. The inhibitory potency was described as IC50—an inhibitor concentration, which reduces the enzyme activity by half. In our study, dimebon, phenothiazine and methylene blue were used as reference compounds. Bis-4-nitrophenyl phosphate (BNPP), a selective inhibitor of CaE36 was used as a positive control in CaE inhibition study.
The results, which are summarized in Table 1, show that the conjugates with both types of spacers: 1-oxopropylene one (C-1 series) and 2-hydroxypropylene one (C-2 series) (Fig. 1) very weakly inhibited AChE and CaE and had rather high inhibitory activity against BChE. All of the compounds showed submicromolar and micromolar activity and very high selectivity against BChE; they were more active (10–15 times for the most active compounds) and much more selective inhibitors of BChE than that compared to dimebon.
Table 1. Inhibitory activity (IC50) of conjugates of γ-carbolines and phenothiazine (Fig. 1) towards AChE, BChE and CaE.
| Compounds |
IC50 (μM) ± SEM |
||||
|---|---|---|---|---|---|
| No | R1 | R2 | AChE | BChE | CaE |
| C-1a | CH3 | CH3 | >200 | 62.6 ± 4.3 | >200 |
| C-1b | CH3 | С2H5 | >200 | 2.04 ± 0.55 | >200 |
| C-1c | F | CH3 | >200 | 1.79 ± 0.28 | >200 |
| C-1d | H | CH3 | >200 | 1.07 ± 0.12 | >200 |
| C-1e | H | С2H5 | >200 | 0.52 ± 0.01 | >200 |
| C-1f | F | С2H5 | >200 | 0.58 ± 0.06 | >200 |
| C-1g | С2H5 | CH3 | >100 | 1.36 ± 0.06 | >200 |
| C-1h | i-С3H7 | CH3 | >100 | 2.79 ± 0.09 | 120 ± 13 |
| C-2a | CH3 | CH3 | n.a. | 11.7 ± 0.4 | >200 |
| C-2b | F | С2H5 | n.a. | 2.01 ± 0.04 | >200 |
| C-2c | CH3O | CH3 | n.a. | 0.39 ± 0.02 | >200 |
| dimebon | 36.3 ± 5.8 | 5.76 ± 0.51 | n.a. | ||
| phenothiazine | n.a. | 137 ± 31 | n.a. | ||
| МB | 1.21 ± 0.09 | 11.1 ± 0.1 | >200 | ||
| BNPP | n.a. | n.a. | 1.80 ± 0.11 | ||
Among the studied conjugates, the maximum inhibitory activity was showed by 1-oxopropylene spacer connected compounds (C-1e) and (C-1f) containing ethyl substituent in carboline cycle (R2 = C2H5): IC50 = 0.52 ± 0.01 and 0.58 ± 0.06 μM, respectively. For compounds with 2-hydroxypropylene spacer, the most active was compound (C-2c) with R1 = CH3O, R2 = CH3: IC50 = 0.39 ± 0.02 μM. Compound (C-1h) with bulky iso-propyl substituent R1 was twice less active (IC50 = 2.79 ± 0.09 μM) than compound (C-1g) with R1 = C2H5 (IC50 = 1.36 ± 0.06 μM). The least active as BChE inhibitors were compounds (C-1a) and (C-2a) with R1 = R2 = CH3.
Comparison of IC50 values for the conjugates (C-1f) and (C-2b), which have 1-oxo- and 2-hydroxypropylene spacers and identical substituents R1 and R2 (R1 = F, R2 = C2H5), showed 3.5 times higher inhibitory activity for the compound with 1-oxopropylene spacer. However, as indicated in the Table 1, for the studies with conjugates with different substituents R1 and R2, anti-BChE activity varies moderately, with maximal activity IC50 = 0.39 ± 0.02 μM for compound (C-2c) and minimal one IC50 = 2.79 ± 0.09 μM for compound (C-1h).
The mechanisms of action of the 9 most active compounds (C-1b)—(C-h) and (C-2b)—(C-2c) towards BChE are presented in Table 2. The linear Lineweaver—Burk equation, which is a double reciprocal form of the Michaelis—Menten one, was used to evaluate the selective characteristics and type of inhibition. As an example, the graphical analysis of steady-state inhibition data for compounds (C-1f) and (C-2b) towards BChE is shown in Fig. 2. The compounds have identical substituents R1 and R2 and different spacers.
Table 2. Inhibition constants of the active conjugates of γ-carbolines and phenothiazine (Fig. 1) towards BChEa.
| Compounds |
Ki (μM) | αKi (μM) | ||
|---|---|---|---|---|
| No | R1 | R2 | ||
| C-1b | CH3 | С2H5 | 0.43 ± 0.05 | 1.46 ± 0.40 |
| C-1c | F | CH3 | 0.48 ± 0.06 | 1.27 ± 0.41 |
| C-1d | H | CH3 | 0.37 ± 0.01 | 1.64 ± 0.20 |
| C-1e | H | С2H5 | 0.26 ± 0.02 | 0.65 ± 0.07 |
| C-1f | F | С2H5 | 0.17 ± 0.02 | 0.52 ± 0.04 |
| C-1g | С2H5 | CH3 | 0.46 ± 0.02 | 0.99 ± 0.04 |
| C-1h | i-С3H7 | CH3 | 1.94 ± 0.01 | |
| C-2b | F | С2H5 | 0.82 ± 0.02 | 2.98 ± 0.19 |
| C-2c | CH3O | CH3 | 0.25 ± 0.04 | 0.89 ± 0.18 |
| MB | 0.35 ± 0.01 | 0.64 ± 0.02 | ||
aValues for Ki (competitive inhibition constant) and αKi (non-competitive inhibition constant) were determined from analysis of slopes of 1/V versus 1/S at various inhibitor concentrations. Values (means ± SEM) are from at least three experiments.
Figure 2. Steady state inhibition of BChE by compounds (C-1f),
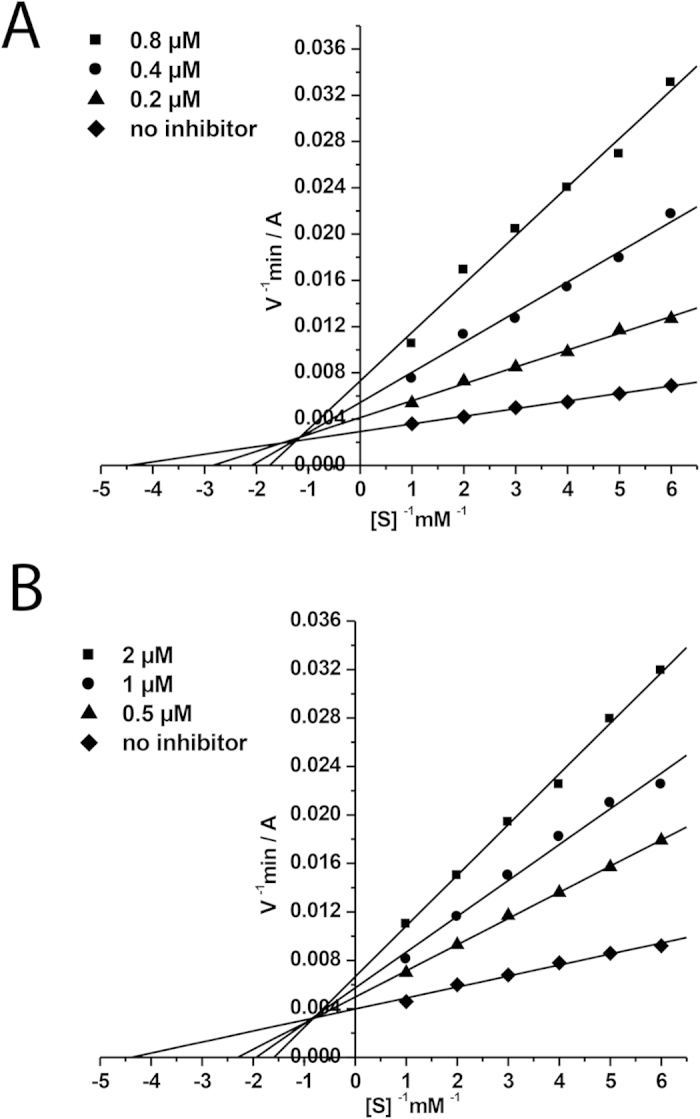
(A) and (C-2b) (B). Lineweaver-Burk reciprocal plots of initial velocity and substrate concentrations in the presence of inhibitors (C-1f), (C-2b) (three concentrations) and their absence are presented. The plots A and B show mixed-type inhibition.
Both compounds are mixed-type reversible inhibitors. As shown in Figs 2A,B, binding of compounds (C-1f) and (C-2b) to BChE changed both Vmax and Km values, a trend that is generally ascribed to mixed-type inhibition. In particular, a decreased Vmax at increasing inhibitor concentrations and increasing intercepts (higher Km) with higher inhibitor concentration were observed. Thus, a structure of the spacer does not affect the mechanism of BChE inhibition by the studied conjugates. The value of inhibition constant for compound (C-1f) was Ki = 0.17 ± 0.02 μM (competitive component) and αKi = 0.52 ± 0.04 μM (noncompetitive component). For compound (C-2b) Ki = 0.82 ± 0.02 μM (competitive component) and αKi = 2.98 ± 0.19 μM (noncompetitive component). The values of obtained BChE inhibition constants (Ki—component competitive and αKi—non-competitive component) are shown in Table 2. Most of the conjugates of γ-carboline and phenothiazine are mixed-type reversible inhibitors of BChE were seen. Only one compound (C-1h) with bulky iso-propyl substituent inhibits BChE by non-competitive mechanism (Table 2).
Molecular modeling
The nature of high inhibitory activity and selectivity of γ-carboline-phenothiazine conjugates to BChE was assessed by molecular docking of the compounds to BChE active site. In the results below, we show the docking of the most active compounds (C-1f) (R1 = F, R2 = C2H5) and (C-2c) (R1 = CH3O, R2 = CH3) containing 1-oxo- and 2-hydroxypropylene spacers.
Quantum mechanical optimization of the ligand structures
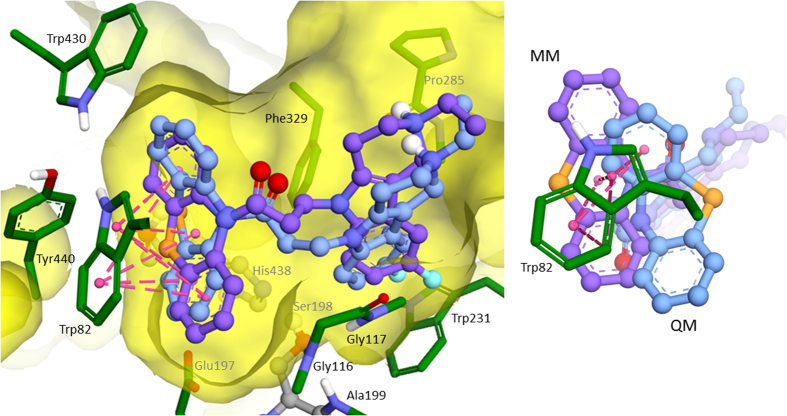
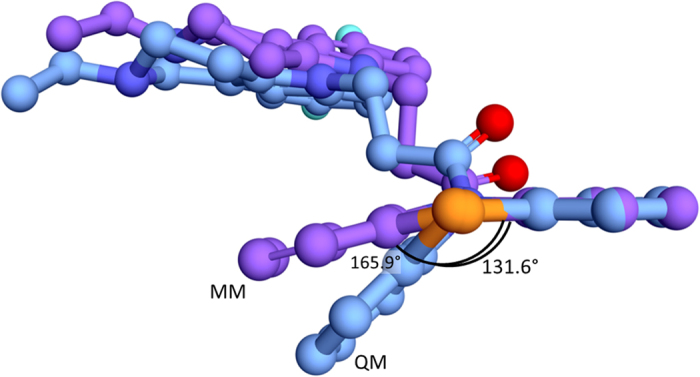
Geometries of the ligands under consideration were optimized quantum mechanically. Comparing to the initial molecular mechanical (MM) optimization, the geometries changed significantly. Phenothiazine fragment after MM optimization has almost planar shape, while after QM optimization it has geometry of two planes intersect at the angle (Fig. 3). This observation similar to the earlier report was already described in28,37, and such a shape was called “butterfly”.
Figure 3. Overlay of structures of phenothiazine fragment of compound (C-1f) after MM (carbon atoms are colored violet) and QM (carbon atoms are colored blue) optimizations.
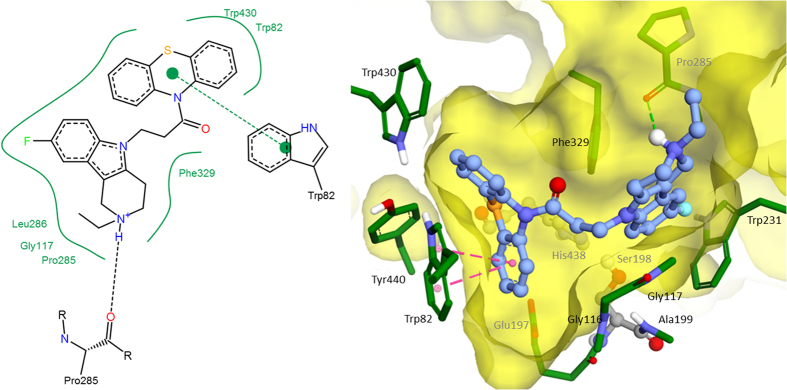
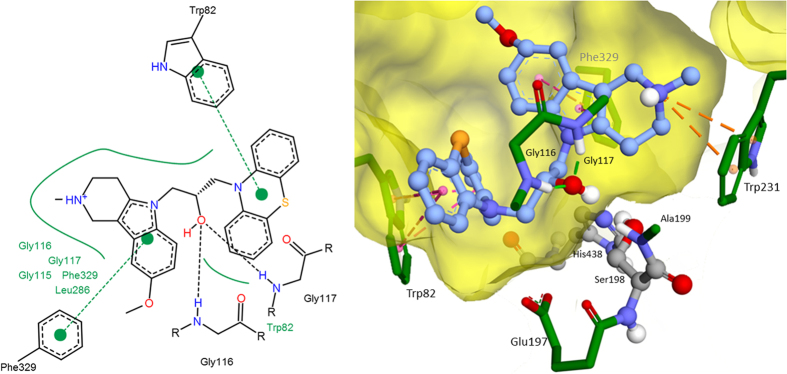
Molecular docking
Molecular docking was performed for MM and QM optimized structures of compound (C-1f). The calculated binding free energy for MM-optimized geometry −11.89 kcal/mol (the corresponding theoretical Ki = 1.94 nM) was significantly overestimated comparing to the experimental data of Ki = 0.17 ± 0.02 μM, αKi = 0.52 ± 0.04 μM. For the QM-optimized structure, the estimated binding affinity reduced due to weaker interaction of non-planar phenothiazine fragment with Trp82 comparing to the planar one as a result of decrease of π-systems overlap (Fig. 4). Estimated binding free energy of compound (C-1f) was −8.89 kcal/mol (the theoretical Ki = 0.3 μM) and linearly positively correlated with the experimental data. Consequently, for all compounds QM-optimized structures were used for molecular docking. As a result, estimated binding energies were in −7.5–−9.5 kcal/mol range, which correspond to the experimental inhibitory activity range of 3–0.1 μМ. There were few specific interactions of conjugates of γ-carboline and phenothiazine with active site and gorge of BChE, while it had perfect geometry fitness. The major interaction was π-π stacking between indole ring of Trp82 and phenothiazine fragment, though slightly weakened by non-planarity of the latter (Figs 5, 6). Besides, hydroxyl group of (C-2c) forms hydrogen bonds with the BChE oxyanion center (Fig. 6). Additionally, weak π-π interaction exists between γ-carboline fragment and Phe329. In protonated forms of the ligands, positively charged group might form additional interactions: π-cation in the case of (C-2c) with Trp231 (Fig. 6) and hydrogen bond with Pro285 in the case of (C-1f) (Fig. 5). However, these interactions contribution is not significant, since for the charged form the estimated binding free energy differences was less than 1 kcal/mol.
Figure 4. Overlay of the best docked positions of compound (C-1f) into active site of BChE.
Carbon atoms of MM optimized structure are shown violet and QM-optimized are colored blue. Views from two different points are shown.
Figure 5. The best docked position of compound (C-1f) inside BChE (2D and 3D images).
Figure 6. The best docked position of compound (C-2c) inside BChE (2D and 3D images).
Radioligand study of compounds interaction with NMDA-receptor binding sites
We have assessed the interaction of synthesized compounds with two main binding sites of NMDA-receptor, namely with [3H] МК-801-binding site and with [3H] ifenprodil-binding site (Table 3). For series of compounds with 1-oxopropylene spacer (C-1) the connection of phenothiazine fragment to γ-carboline cycle leads to significant increase (in 10 times) of their affinity towards МК-801 site compared to dimebon. Binding to ifenprodil site increases in some cases. In particular, compounds (C-1e), (C-1f) and (C-1g) containing ethyl substituent in the carboline cycle have the strongest binding characteristics towards both NMDA-receptor sites. When a 2-hydroxypropylene spacer was used (C-2 series), the reduction of the conjugates affinity towards both sites was detected. At the same time, none of compounds showed any selectivity in relation to ifenprodil-binding site typical for MB (Table 3).
Table 3. The binding of γ-carboline-phenothiazine conjugates (Fig. 1) to МК-801 and ifenprodil binding sites of NMDA receptor.
| Compounds |
Binding characteristics of compounds |
|||||
|---|---|---|---|---|---|---|
| No | R1 | R2 | % of [3H]МК-801 blockadeat 100 μM ofcompound | [3H]МК-801, IC50, μM | % of [3H]ifenprodilblockade at100 μM ofcompound | [3H]ifenprodil,(IC50, μM) |
| C-1a | CH3 | CH3 | 80.4 ± 6.6 | 13.5 ± 3.6 | 42.6 ± 7.2 | 88.4 ± 8.3 |
| C-1b | CH3 | С2H5 | 95.7 ± 1.0 | 8.5 ± 0.8 | 48.1 ± 5.9 | 74.4 ± 4.0 |
| C-1c | F | CH3 | 78.7 ± 1.4 | 17.7 ± 2.6 | 50.2 ± 5.2 | 55.1 ± 5.8 |
| C-1d | H | CH3 | 74.9 ± 1.1 | 18.5 ± 0.9 | 60.1 ± 1.4 | 23.4 ± 0.7 |
| C-1e | H | С2H5 | 76.1 ± 1.2 | 14.6 ± 1.9 | 69.4 ± 3.3 | 13.4 ± 2.6 |
| C-1f | F | С2H5 | 82.4 ± 7.3 | 15.8 ± 1.8 | 78.2 ± 6.8 | 8.8 ± 1.8 |
| C-1g | С2H5 | CH3 | 89.4 ± 4.6 | 13.2 ± 2.2 | 64.6 ± 5.2 | 15.4 ± 3.9 |
| C-1h | i-С3H7 | CH3 | 80.3 ± 6.9 | 17.8 ± 2.0 | 88.7 ± 5.6 | 85.8 ± 7.2 |
| C-2a | CH3 | CH3 | 87.1 ± 7.7 | 84.8 ± 9.2 | 69.7 ± 8.3 | 57.2 ± 6.7 |
| C-2b | F | С2H5 | 24.1 ± 1.9 | 106.3 ± 9.2 | 25.7 ± 4.6 | 81.2 ± 6.7 |
| C-2c | CH3O | CH3 | 19.1 ± 2.2 | 113.4 ± 11.1 | 47.4 ± 6.6 | 115.4 ± 9.3 |
| dimebon | 27.8 ± 3.9 | 91.5 ± 7.7 | 34.1 ± 4.9 | 82.4 ± 4.1 | ||
| МB | 2.0 ± 4.0 | n/d | 70.4 ± 10.1 | 9.3 ± 4.5 | ||
Discussion
In the present study, we provide a throughout evaluation of the inhibitory activity on AChE, BChE and CaE of the γ-carboline-phenothiazine conjugates by kinetics and computational tools as well radioligand assessment of conjugates interaction with two binding sites of NMDA receptor. AChE and BChE are important for AD and/or AD-like dementia development and structurally close enzyme – CaE is responsible for the hydrolysis of numerous ester-containing drugs33,34. Inhibition of CaE by anticholinesterase compounds leads to adverse drug-drug interactions35. In our study, dimebon, phenothiazine and methylene blue were used as reference compounds. The results in Table 1 demonstrate, regardless the type of spacer, the γ-carboline-phenothiazine conjugates had rather high inhibitory activity toward BChE and very low activity against two other studied esterases, AChE and CaE. Thus, the compounds possess a high inhibitory selectivity to BChE. The conjugates were more active (10–15 times for the most active compounds) and much more selective inhibitors of BChE compared to dimebon. That is, substitution of 2-pyridoethyl fragment in a dimebon molecule on phenothiazine group connected to gamma-carboline by 1-oxopropylene or 2-hydroxypropylene spacer changes the esterase profile38,39 of the dimebon. As for other reference compounds, MB is more specific to AChE than to BChE, while it is well known that its phenothiazine core has been the basis of many selective inhibitors of BChE28,29,31,37,40. Very low activity of γ-carboline-phenothiazine conjugates against AChE indicates that these compounds will not cause unwanted side effects inherent AChE inhibitors; lacking inhibitor activity against CaE suggests they will not cause adverse drug-drug interactions.
The molecular docking results suggest that interaction between γ-carboline-phenothiazine conjugates and BChE active site and gorge are characterized rather by good geometrical complementarity than those specific interactions. This geometrical fitness seems to be the main reason for high inhibitory activity and selectivity of the compounds under consideration. Since the main specific protein-ligand interaction is π-π stacking between indole group of Trp82 and phenothiazine fragment of conjugates, this explains moderate effect of alterations of structure of γ-carboline fragment and the spacer nature on inhibitory activity of the conjugate compounds.
In healthy brains, acetylcholine is mainly hydrolysed by AChE, while BChE plays a secondary role. However, in AD brains, the activity of AChE decreases while that of BChE gradually rises41,42. Therefore, BChE appears as an increasingly important therapeutic target to reduce AD cholinergic deficit41,43,44. The remarkable activity and selectivity towards BChE showed by the conjugates (C-1e), (C-1f) and (C-2c) could be of great importance in the development of selective new and more specific anti-AD therapies, since it has been described that selective BChE inhibition increases brain acetylcholine and improves learning in rodents44,45. Moreover, the proven efficacy of inhibitors affecting both cholinesterases46,47,48 and the clinical failure of AChE-specific inhibition suggest that BuChE inhibition could be important for more effective treatment of AD. Therefore, BuChE-selective inhibitors provide promise for improved clinical benefit49.
By our previous observations, the NMDA-receptor is one of the targets of dimebon neuronal action32. The radioligand binding study of γ-carboline-phenothiazine conjugates with two main binding sites of non-competitive negative modulators of NMDA-receptor, namely intra-channel blocker МК-801 and allosteric modulator ifenprodil, was performed. It was observed that the ligand properties of conjugates radically differed from dimebon and MB—the basic structures for designed compounds (Table 3). The substitution of 2-pyridoethyl fragment in a dimebon molecule on phenothiazine group connected to γ-carboline by 1-oxopropylene spacer increases (in 10 times) compounds binding to both NMDA-receptor binding sites; whereas using 2-hydroxypropylene spacer impairs binding properties. None of compounds showed any selectivity in relation to ifenprodil-binding site typical for MB. The compounds (C-1e), (C-1f) and (C-1g) containing ethyl substituent in the carboline cycle demonstrated the strongest binding characteristics towards both NMDA-receptor sites. It can be assumed that compounds that compete for them would also act as non-competitive negative modulators of NMDA-receptor. Two of the compounds (C-1e) and (C-1f) also were the best inhibitors of BChE.
Conclusions
To discover multifunctional agents for treatment of neurodegenerative diseases, a series of original compounds, which combine γ-carboline fragment of dimebon and phenothiazine core of MB in one molecule was studied as inhibitors of AChE, BChE and CaE. It was found that the conjugates had a high inhibitory activity toward BChE with IC50 values in submicromolar and micromolar range and exhibited strong inhibitory activities and selectivity against BChE over AChE and CaE. Studies of the compounds binding to МК-801 and ifenprodil-binding sites of NMDA-receptors showed that conjugates with 1-oxopropylene spacer had increased affinity towards both NMDA-receptor binding sites compared to the dimebon. Compounds (C-1e) and (C-1f), which showed the highest affinity to both NMDA-receptor sites, also were significant inhibitors of BChE. It is important to point that these compounds did not inhibit AChE, therefore will not cause unwanted side effects; they also did not inhibit the structurally related enzyme CaE, i.e. and will not cause adverse drug-drug interactions. Finally, these compounds emerge as promising safe multitarget ligands for drugs development against age-related neurodegenerative disorders such as Alzheimer, Parkinson or other related conditions.
Materials and Methods
Chemistry
The studied conjugates of γ-carbolines and phenothiazine (Fig. 1) have been synthesized as described previously26,27.
Biological assay
In vitro AChE, BChE and CaE inhibition
Acetylcholinesterase (AChE, EC 3.1.1.7, from human erythrocyte), butyrylcholinesterase (BChE, EC 3.1.1.8, from equine serum), carboxylesterase (CaE, EC 3.1.1.1, from porcine liver), acetylthiocholine iodide (ATCh), butylthiocholine iodide (BTCh), 5,5´-dithiobis-(2-nitrobenzoic acid) (DTNB), 4-nitrophenyl acetate (4-NPA), were purchased from Sigma-Aldrich (Germany).
AChE and BChE activities were measured by the method of Ellman and coworkers as described earlier50. The assay solution consisted of 0.1 M K/Na phosphate buffer pH 7.5, 25 °C with the addition of 0.33 mM DTNB, 0.02 unit/mL of AChE or BChE and 1 mM of substrate (ATCh or BTCh, respectively). Assays were carried out with a blank containing all components except ATCh and BTCh in order to account for non-enzymatic reaction.
The activity of CaE was determined spectrophotometrically by the release of 4-nitrophenol at 405 nm51. The assay solution consisted of 0.1 M K/Na phosphate buffer pH 8.0, 25 °C with the addition of 1 mM 4-nitrophenyl acetate and 0.02 unit/mL of CaE. Assays were carried out with a blank containing all components except CaE.
The tested compounds were dissolved in DMSO; the incubation mixture contained 2% of the solvent. Eight different concentrations of the test compounds in the range of 10−11–10−4 M were selected in order to obtain inhibition of AChE and BChE activity comprised between 20% and 80%. The test compounds were added to the assay solution and preincubated at 25 °C with the enzymes for 10 min followed by the addition of substrate. A parallel control was made for the assay solution with no inhibitor. Measurements were performed in a BioRad Benchmark Plus microplate spectrophotometer (France). Each experiment was performed in triplicate. The results were expressed as the mean ± SEM. The reaction rates in the presence and absence of inhibitor were compared, and the percent of residual enzyme activity due to the presence of test compounds was calculated. IC50 (the concentration of inhibitor required to decrease the enzyme activity by 50%) values were determined graphically from inhibition curves (log inhibitor concentration vs percent residual enzyme activity) using the Origin 6.1 software.
Kinetic analysis of BChE inhibition. Determination of steady-state inhibition constants
To elucidate the inhibition mechanisms for the most active compounds, the BChE residual activity were determined in the presence of 3 increased concentrations of the test compounds and 6 decreasing concentrations of the substrates. The test compounds were preincubated with the enzymes at 25 °C for 10 min, followed by the addition of the substrates. Parallel controls were made for an assay of the rate of hydrolysis of the same concentrations of substrates in the solutions with no inhibitor. The kinetic parameters of substrate hydrolysis were determined. Measurements were performed in a BioRad Benchmark Plus microplate spectrophotometer (France). Each experiment was performed in triplicate. Results were fitted into Lineweaver-Burk double-reciprocal kinetic plots of 1/V versus 1/[S] and values of inhibition constants Ki (competitive component) and αKi (noncompetitive component) were calculated using the program Origin 6.1.
Radioligand study of compounds interaction with NMDA-receptor binding sites
Effect of test compounds on the radioligand binding to NMDA receptors was determined by using a modified method as reported earlier by Zhou L-M and coworkers52. Two radioactive ligands were used: [3H] MK-801 (dizocilpine) with a specific activity of 210 Ci/mmol binding to all isolated NMDA receptors, and [3H] ifenprodil with a specific activity of 79 Ci/mmol binding only to NMDA receptors containing the NR2B subunit53,54.
A membrane preparation of hippocampus for radioligand analysis was prepared by the techniques described previously55. The obtained membrane pellet was resuspended in a work buffer (5 mM HEPES/4.5 mM Tris buffer, pH 7.6) in a ratio of 1:5, and stored in liquid nitrogen. The reaction mixture (the final volume of 0.5 ml) contained 200 μl of the working buffer, 50 μl of 50 nM radioligand solution and 250 μl of the membrane suspension. Nonspecific binding was determined in the presence of 50 μl of 1 M of unlabeled ligand.
For binding study, the reaction mixture was incubated at room temperature for 2 hours. After incubation, the samples were filtered through the glass-fiber filters GF/B (Whatman), washed with the work buffer, dried and transferred to scintillation vials to which 5 ml of scintillation fluid was added containing 4g diphenyl oxazole (PPO), 0.2g diphenyloxazoil benzene (POPOP) and 1 liter of toluene. Radioactivity was determined in the scintillation counter TriCarb2800 TR (PerkinElmer, Packard, USA) with counting efficiency of about 65%.
Investigation of the effect of the tested compounds on the binding of [3H] MK-801 and [3H] ifenprodil to rat hippocampal membranes was carried out by adding to the incubation medium 50 μl of the test compounds in the concentration range of 10−8–10−3 M. By the results of inhibition, IC50 values were calculated for the tested compounds using GraphPadPrism 4 Demo. In the cases where inhibition by the test compound in the concentration of 100 mM did not exceed 50%, the value of IC50 was not determined (n/d).
Molecular modelling
To determine protonation state of piperidine nitrogen atom of γ-carboline fragment of the compounds, Marvin 6.3.0 (ChemAxon, http://www.chemaxon.com) was used to estimate pKa values. Since they were found to be close to 7.4, forms, protonated and neutral were used for molecular docking.
Geometries of the ligands were quantum-mechanically (QM) optimized in Gamess-US package56 using DFT method B3LYP and basis 6-31G*. Partial atomic charges were taken from QM results according to Mulliken scheme57. The PDB58 structure of human BChE 1P0I59 was used. Previously the importance of saturation of BuChE gorge with water molecules was demonstrated60. Protein structure was prepared, saturated with water molecules and optimized using QM/MM method as reported previously60,61.
Molecular docking with a Lamarckian Genetic Algorithm62 was performed with Autodock 4.2.6 software63. Grid box for docking included the whole BChE active site and the gorge with dimensions 15 Å × 20.25 Å × 18 Å with grid spacing 0.375 Å. The main of selected Lamarckian Genetic Algorithm parameters were 256 runs, 25 × 106 evaluations, 27 × 104 generations and population size 300. For the best docked positions, additional 256 runs of local search were performed. Docking positions with the lowest binding energies were used for analysis. Structural images were prepared with Accelrys Discovery Studio Visualiser 4.0 (http://www.accelrys.com), 2D images of protein-ligand are prepared with PoseView software (http://poseview.zbh.uni-hamburg.de/).
Additional Information
How to cite this article: Makhaeva, G. F. et al. Conjugates of γ-Carbolines and Phenothiazine as new selective inhibitors of butyrylcholinesterase and blockers of NMDA receptors for Alzheimer Disease. Sci. Rep. 5, 13164; doi: 10.1038/srep13164 (2015).
Acknowledgments
The study was supported by the grant of the Russian Science Foundation (project number 14-23-00160). S.V. Lushchekina is grateful to the “Dynasty” foundation for the scholarship (a support of the computer-modeling part of this study).
Footnotes
Author Contributions G.F.M., S.V.L, N.P.B., V.B.S., V.V.G., O.G.S., E.A.V. and A.Y.A. designed and performed experiments; G.E.B., G.A. and S.O.B. analyzed the data; G.F.M., S.V.L, N.P.B., G.E.B., G.A. and S.O.B. discussed and wrote the manuscript.
References
- Salomone S., Caraci F., Leggio G. M., Fedotova J. & Drago F. New pharmacological strategies for treatment of Alzheimer’s disease: focus on disease modifying drugs. British journal of clinical pharmacology 73, 504–517, 10.1111/j.1365-2125.2011.04134.x (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youdim M. B. Why do we need multifunctional neuroprotective and neurorestorative drugs for Parkinson’s and Alzheimer’s diseases as disease modifying agents. Experimental neurobiology 19, 1–14, 10.5607/en.2010.19.1.1 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carreiras M. C., Mendes E., Perry M. J., Francisco A. P. & Marco-Contelles J. The multifactorial nature of Alzheimer’s disease for developing potential therapeutics. Current topics in medicinal chemistry 13, 1745–1770 (2013). [DOI] [PubMed] [Google Scholar]
- Eisen A. Amyotrophic lateral sclerosis: A 40-year personal perspective. Journal of clinical neuroscience: official journal of the Neurosurgical Society of Australasia 16, 505–512, 10.1016/j.jocn.2008.07.072 (2009). [DOI] [PubMed] [Google Scholar]
- Bachurin S. O. [Medicinal and chemical approaches to focused search of agents for treatment and therapy of Alzheimer disease]. Voprosy meditsinskoi khimii 47, 155–197 (2001). [PubMed] [Google Scholar]
- Calza L. et al. From the multifactorial nature of Alzheimer’s disease to multitarget therapy: the contribution of the translational approach. Current topics in medicinal chemistry 13, 1843–1852 (2013). [DOI] [PubMed] [Google Scholar]
- Geldenhuys W. J. & Van der Schyf C. J. Rationally designed multi-targeted agents against neurodegenerative diseases. Current medicinal chemistry 20, 1662–1672 (2013). [DOI] [PubMed] [Google Scholar]
- Guzior N., Wieckowska A., Panek D. & Malawska B. Recent development of multifunctional agents as potential drug candidates for the treatment of Alzheimer’s disease. Current medicinal chemistry 22, 373–404 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blasco H., Mavel S., Corcia P. & Gordon P. H. The glutamate hypothesis in ALS: pathophysiology and drug development. Current medicinal chemistry 21, 3551–3575 (2014). [DOI] [PubMed] [Google Scholar]
- Cacabelos R., Takeda M. & Winblad B. The glutamatergic system and neurodegeneration in dementia: preventive strategies in Alzheimer’s disease. International journal of geriatric psychiatry 14, 3–47 (1999). [DOI] [PubMed] [Google Scholar]
- Mufson E. J., Counts S. E., Perez S. E. & Ginsberg S. D. Cholinergic system during the progression of Alzheimer’s disease: therapeutic implications. Expert review of neurotherapeutics 8, 1703–1718, 10.1586/14737175.8.11.1703 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canas P. M., Simoes A. P., Rodrigues R. J. & Cunha R. A. Predominant loss of glutamatergic terminal markers in a beta-amyloid peptide model of Alzheimer’s disease. Neuropharmacology 76 Pt A, 51–56, 10.1016/j.neuropharm.2013.08.026 (2014). [DOI] [PubMed] [Google Scholar]
- Parsons C. G., Danysz W., Dekundy A. & Pulte I. Memantine and cholinesterase inhibitors: complementary mechanisms in the treatment of Alzheimer’s disease. Neurotoxicity research 24, 358–369, 10.1007/s12640-013-9398-z (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez A. & Castro A. Novel cholinesterase inhibitors as future effective drugs for the treatment of Alzheimer’s disease. Expert opinion on investigational drugs 15, 1–12, 10.1517/13543784.15.1.1 (2006). [DOI] [PubMed] [Google Scholar]
- Rodda J. & Carter J. Cholinesterase inhibitors and memantine for symptomatic treatment of dementia. Bmj 344, e2986, 10.1136/bmj.e2986 (2012). [DOI] [PubMed] [Google Scholar]
- Wilkinson D. G., Francis P. T., Schwam E. & Payne-Parrish J. Cholinesterase inhibitors used in the treatment of Alzheimer’s disease: the relationship between pharmacological effects and clinical efficacy. Drugs & aging 21, 453–478 (2004). [DOI] [PubMed] [Google Scholar]
- Francis P. T., Parsons C. G. & Jones R. W. Rationale for combining glutamatergic and cholinergic approaches in the symptomatic treatment of Alzheimer’s disease. Expert review of neurotherapeutics 12, 1351–1365, 10.1586/ern.12.124 (2012). [DOI] [PubMed] [Google Scholar]
- Grossberg G. T., Edwards K. R. & Zhao Q. Rationale for combination therapy with galantamine and memantine in Alzheimer’s disease. Journal of clinical pharmacology 46, 17S–26S, 10.1177/0091270006288735 (2006). [DOI] [PubMed] [Google Scholar]
- Rosini M., Simoni E., Minarini A. & Melchiorre C. Multi-target design strategies in the context of Alzheimer’s disease: acetylcholinesterase inhibition and NMDA receptor antagonism as the driving forces. Neurochemical research 39, 1914–1923, 10.1007/s11064-014-1250-1 (2014). [DOI] [PubMed] [Google Scholar]
- Oz M., Lorke D. E. & Petroianu G. A. Methylene blue and Alzheimer’s disease. Biochemical pharmacology 78, 927–932, 10.1016/j.bcp.2009.04.034 (2009). [DOI] [PubMed] [Google Scholar]
- Atamna H. & Kumar R. Protective role of methylene blue in Alzheimer’s disease via mitochondria and cytochrome c oxidase. Journal of Alzheimer’s disease: JAD 20 Suppl 2, S439–452, 10.3233/JAD-2010-100414 (2010). [DOI] [PubMed] [Google Scholar]
- Bharadwaj P. R. et al. Latrepirdine: molecular mechanisms underlying potential therapeutic roles in Alzheimer’s and other neurodegenerative diseases. Translational psychiatry 3, e332, 10.1038/tp.2013.97 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano-Cuenca N., Solis-Garcia del Pozo J. E. & Jordan J. Evidence for the efficacy of latrepirdine (Dimebon) treatment for improvement of cognitive function: a meta-analysis. Journal of Alzheimer’s disease: JAD 38, 155–164, 10.3233/JAD-130872 (2014). [DOI] [PubMed] [Google Scholar]
- Steele J. W. & Gandy S. Latrepirdine (Dimebon(R), a potential Alzheimer therapeutic, regulates autophagy and neuropathology in an Alzheimer mouse model. Autophagy 9, 617–618, 10.4161/auto.23487 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamashita M. et al. Methylene blue and dimebon inhibit aggregation of TDP-43 in cellular models. FEBS letters 583, 2419–2424, 10.1016/j.febslet.2009.06.042 (2009). [DOI] [PubMed] [Google Scholar]
- Bachurin S. O. et al.Derivatives of 1, 2, 3, 4-tetrahydropyrido [4, 3-b]indole containing phenothiazines as inhibitors of cholinesterases and blockers of serotonin 5-HT6 receptors, methods for their synthesis and pharmacological agent on their base. Russia patent #2530881(2014). [Google Scholar]
- Bachurin S. O. et al. Derivatives of phenothiazine containing 1, 2, 3, 4-tetrahydropyrido [4, 3-b]indoles as agents for reducing uncontrolled protein aggregation in nervous system, methods for their synthesis, pharmacological agent on this base and method for reducing uncontrolled protein aggregation in nervous system. Russia patent #2529899(2014). [Google Scholar]
- Darvesh S. et al. Carbamates with differential mechanism of inhibition toward acetylcholinesterase and butyrylcholinesterase. Journal of medicinal chemistry 51, 4200–4212, 10.1021/jm8002075 (2008). [DOI] [PubMed] [Google Scholar]
- Darvesh S. et al. Differential binding of phenothiazine urea derivatives to wild-type human cholinesterases and butyrylcholinesterase mutants. Bioorganic & medicinal chemistry 18, 2232–2244, 10.1016/j.bmc.2010.01.066 (2010). [DOI] [PubMed] [Google Scholar]
- Sezgin Z., Biberoglu K., Chupakhin V., Makhaeva G. F. & Tacal O. Determination of binding points of methylene blue and cationic phenoxazine dyes on human butyrylcholinesterase. Archives of biochemistry and biophysics 532, 32–38, 10.1016/j.abb.2013.01.003 (2013). [DOI] [PubMed] [Google Scholar]
- Simeon-Rudolf V., Sinko G., Stuglin A. & Reiner E. Inhibition of human blood acetylcholinesterase and butyrylcholinesterase by ethopropazine. Croat Chem Acta 74, 173–182 (2001). [Google Scholar]
- Grigoriev V. V., Dranyi O. A. & Bachurin S. O. Comparative study of action mechanisms of dimebon and memantine on AMPA- and NMDA-subtypes glutamate receptors in rat cerebral neurons. Bulletin of experimental biology and medicine 136, 474–477 (2003). [DOI] [PubMed] [Google Scholar]
- Imai T. Human carboxylesterase isozymes: catalytic properties and rational drug design. Drug metabolism and pharmacokinetics 21, 173–185 (2006). [DOI] [PubMed] [Google Scholar]
- Laizure S. C., Herring V., Hu Z., Witbrodt K. & Parker R. B. The role of human carboxylesterases in drug metabolism: have we overlooked their importance? Pharmacotherapy 33, 210–222, 10.1002/phar.1194 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsurkan L. G., Hatfield M. J., Edwards C. C., Hyatt J. L. & Potter P. M. Inhibition of human carboxylesterases hCE1 and hiCE by cholinesterase inhibitors. Chemico-biological interactions 203, 226–230, 10.1016/j.cbi.2012.10.018 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heymann E. & Krisch K. [Phosphoric acid-bis-(p-nitro-phenylester), a new inhibitor of microsomal carboxylesterases]. Hoppe-Seyler’s Zeitschrift fur physiologische Chemie 348, 609–619 (1967). [PubMed] [Google Scholar]
- Darvesh S. et al. Structure-activity relationships for inhibition of human cholinesterases by alkyl amide phenothiazine derivatives. Bioorganic & medicinal chemistry 13, 211–222, 10.1016/j.bmc.2004.09.059 (2005). [DOI] [PubMed] [Google Scholar]
- Makhaeva G. F. et al. Combined QSAR studies of inhibitor properties of O-phosphorylated oximes toward serine esterases involved in neurotoxicity, drug metabolism and Alzheimer’s disease. SAR and QSAR in environmental research 23, 627–647, 10.1080/1062936X.2012.679690 (2012). [DOI] [PubMed] [Google Scholar]
- Makhaeva G. F. et al. Organophosphorus compound esterase profiles as predictors of therapeutic and toxic effects. Chemico-biological interactions 203, 231–237, 10.1016/j.cbi.2012.10.012 (2013). [DOI] [PubMed] [Google Scholar]
- Darvesh S. et al. Selective reversible inhibition of human butyrylcholinesterase by aryl amide derivatives of phenothiazine. Bioorganic & medicinal chemistry 15, 6367–6378, 10.1016/j.bmc.2007.06.060 (2007). [DOI] [PubMed] [Google Scholar]
- Greig N. H. et al. A new therapeutic target in Alzheimer’s disease treatment: attention to butyrylcholinesterase. Current medical research and opinion 17, 159–165, 10.1185/0300799039117057 (2001). [DOI] [PubMed] [Google Scholar]
- Lane R. M., Potkin S. G. & Enz A. Targeting acetylcholinesterase and butyrylcholinesterase in dementia. The international journal of neuropsychopharmacology/official scientific journal of the Collegium Internationale Neuropsychopharmacologicum 9, 101–124, 10.1017/S1461145705005833 (2006). [DOI] [PubMed] [Google Scholar]
- Wang L. et al. Donepezil + propargylamine + 8-hydroxyquinoline hybrids as new multifunctional metal-chelators, ChE and MAO inhibitors for the potential treatment of Alzheimer’s disease. European journal of medicinal chemistry 80, 543–561, 10.1016/j.ejmech.2014.04.078 (2014). [DOI] [PubMed] [Google Scholar]
- Kamal M. A. et al. Kinetics of human serum butyrylcholinesterase inhibition by a novel experimental Alzheimer therapeutic, dihydrobenzodioxepine cymserine. Neurochemical research 33, 745–753, 10.1007/s11064-007-9490-y (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greig N. H. et al. Selective butyrylcholinesterase inhibition elevates brain acetylcholine, augments learning and lowers Alzheimer beta-amyloid peptide in rodent. Proceedings of the National Academy of Sciences of the United States of America 102, 17213–17218, 10.1073/pnas.0508575102 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordberg A. et al. Different cholinesterase inhibitor effects on CSF cholinesterases in Alzheimer patients. Current Alzheimer research 6, 4–14 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samadi A. et al. Synthesis, pharmacological assessment, and molecular modeling of 6-chloro-pyridonepezils: new dual AChE inhibitors as potential drugs for the treatment of Alzheimer’s disease. European journal of medicinal chemistry 67, 64–74, 10.1016/j.ejmech.2013.06.021 (2013). [DOI] [PubMed] [Google Scholar]
- Weinstock M. & Groner E. Rational design of a drug for Alzheimer’s disease with cholinesterase inhibitory and neuroprotective activity. Chemico-biological interactions 175, 216–221, 10.1016/j.cbi.2008.03.014 (2008). [DOI] [PubMed] [Google Scholar]
- Macdonald I. R., Rockwood K., Martin E. & Darvesh S. Cholinesterase inhibition in Alzheimer’s disease: is specificity the answer? Journal of Alzheimer’s disease: JAD 42, 379–384, 10.3233/JAD-140219 (2014). [DOI] [PubMed] [Google Scholar]
- Ellman G. L., Courtney K. D., Andres V. Jr. & Feather-Stone R. M. A new and rapid colorimetric determination of acetylcholinesterase activity. Biochemical pharmacology 7, 88–95 (1961). [DOI] [PubMed] [Google Scholar]
- Sterri S. H., Johnsen B. A. & Fonnum F. A radiochemical assay method for carboxylesterase, and comparison of enzyme activity towards the substrates methyl [1-14C] butyrate and 4-nitrophenyl butyrate. Biochemical pharmacology 34, 2779–2785 (1985). [DOI] [PubMed] [Google Scholar]
- Zhou L. M. et al. (2S, 4R)-4-methylglutamic acid (SYM 2081): a selective, high-affinity ligand for kainate receptors. The Journal of pharmacology and experimental therapeutics 280, 422–427 (1997). [PubMed] [Google Scholar]
- Coughenour L. L. & Barr B. M. Use of trifluoroperazine isolates a [(3)H]Ifenprodil binding site in rat brain membranes with the pharmacology of the voltage-independent ifenprodil site on N-methyl-D-aspartate receptors containing NR2B subunits. The Journal of pharmacology and experimental therapeutics 296, 150–159 (2001). [PubMed] [Google Scholar]
- Dana C., Benavides J., Schoemaker H. & Scatton B. Pharmacological characterisation and autoradiographic distribution of polyamine-sensitive [3H]ifenprodil binding sites in the rat brain. Neuroscience letters 125, 45–48 (1991). [DOI] [PubMed] [Google Scholar]
- Nowak G., Trullas R., Layer R. T., Skolnick P. & Paul I. A. Adaptive changes in the N-methyl-D-aspartate receptor complex after chronic treatment with imipramine and 1-aminocyclopropanecarboxylic acid. The Journal of pharmacology and experimental therapeutics 265, 1380–1386 (1993). [PubMed] [Google Scholar]
- Schmidt M. W. et al. General atomic and molecular electronic structure system. Journal of Computational Chemistry 14, 1347–1363 (2004). [Google Scholar]
- Mulliken R. S. Electronic population analysis on LCAO-MO molecular wave functions. Journal of Chemical Physics 23, 1841–1846 (1955). [Google Scholar]
- Berman H. M. et al. The Protein Data Bank. Nucleic acids research 28, 235–242 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolet Y., Lockridge O., Masson P., Fontecilla-Camps J. C. & Nachon F. Crystal structure of human butyrylcholinesterase and of its complexes with substrate and products. The Journal of biological chemistry 278, 41141–41147, 10.1074/jbc.M210241200 (2003). [DOI] [PubMed] [Google Scholar]
- Masson P., Lushchekina S., Schopfer L. M. & Lockridge O. Effects of viscosity and osmotic stress on the reaction of human butyrylcholinesterase with cresyl saligenin phosphate, a toxicant related to aerotoxic syndrome: kinetic and molecular dynamics studies. The Biochemical journal 454, 387–399, 10.1042/BJ20130389 (2013). [DOI] [PubMed] [Google Scholar]
- Lushchekina S. V., Polomskikh V. S., Varfolomeev S. D. & Masson P. Molecular modeling of butyrylcholinesterase inhibition by cresyl saligenin phosphate. Russian Chemical Bulletin 62, 2527–2537 10.1007/s11172-013-0366-9 (2013). [DOI] [Google Scholar]
- Morris G. M. et al. Automated docking using a Lamarckian genetic algorithm and an empirical binding free energy function. Journal of Computational Chemistry 19, 1639–1662 (1999). [Google Scholar]
- Morris G. M. et al. AutoDock4 and AutoDockTools4: Automated docking with selective receptor flexibility. J Comput Chem 30, 2785–2791, 10.1002/jcc.21256 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]