Abstract
Beta-blockers can help reduce mortality following acute myocardial infarction (MI); however, whether beta-blockers exert a class effect remains controversial. This study identified all patients with first ST-elevation MI for the period of 2003 to 2010 from the National Health Insurance claims database, Taiwan. We compared patients prescribed carvedilol, bisoprolol, and propranolol. Study outcomes included all-cause death, cardiovascular death, and recurrence of MI. The propensity scores were constructed using multinomial logistic regression to model the receipt of different beta-blockers. Treating carvedilol group as a reference, we employed a simultaneous three-group comparison approach using the Cox regression model with adjustment for the propensity scores to compare the relative risks of various outcomes. Among the 16836 patients, 7591 were prescribed carvedilol, 5934 bisoprolol, and 3311 propranolol. Mean follow-up time was one year. After accounting for baseline differences, patients treated with bisoprolol (HR 0.87, 95% CI 0.72–1.05, p = 0.14) or propranolol (HR 1.07, 95% CI 0.84–1.36, p = 0.58) had a similar risk of all-cause death in comparison with carvedilol. No significant differences were observed among three beta-blocker groups with regard to the risks of cardiovascular death and recurrence of MI. Our results suggest that beta-blockers exert a possible class effect in the treatment of acute MI.
Beta-blocker therapy is the standard treatment for ST-elevation myocardial infarction (STEMI). The 2013 American College of Cardiology Foundation/American Heart Association Guidelines for the Management of STEMI state that STEMI should be treated with oral beta-blockers in patients without contraindications (Class I indication)1. Benefits of beta-blockers for patients with acute myocardial infarction (MI) include anti-ischemic, antihypertensive, antiarrhythmic, and antithrombotic effects2. Most evidence supporting the benefits of beta-blockers has been obtained from randomized trials pre-dating the advent of modern reperfusion therapy and pharmacotherapy3,4,5,6. In the era of percutaneous coronary intervention (PCI), several prospective cohort studies have also indicated that treatment with beta-blockers is associated with reduced mortality in patients suffering from acute MI7,8,9,10
Most physicians assume that all beta-blockers exert a class effect; therefore, there is considerable variation in the type of beta-blocker prescribed to treat acute MI11. However, given the differences in pharmacologic properties among available beta-blockers, this assumption is questionable12. The current study investigated long-term outcomes of STEMI patients treated with different beta-blockers (carvedilol, bisoprolol, and propranolol). Subjects were identified from the National Health Insurance (NHI) claims database in Taiwan.
Results
Characteristics of study subjects
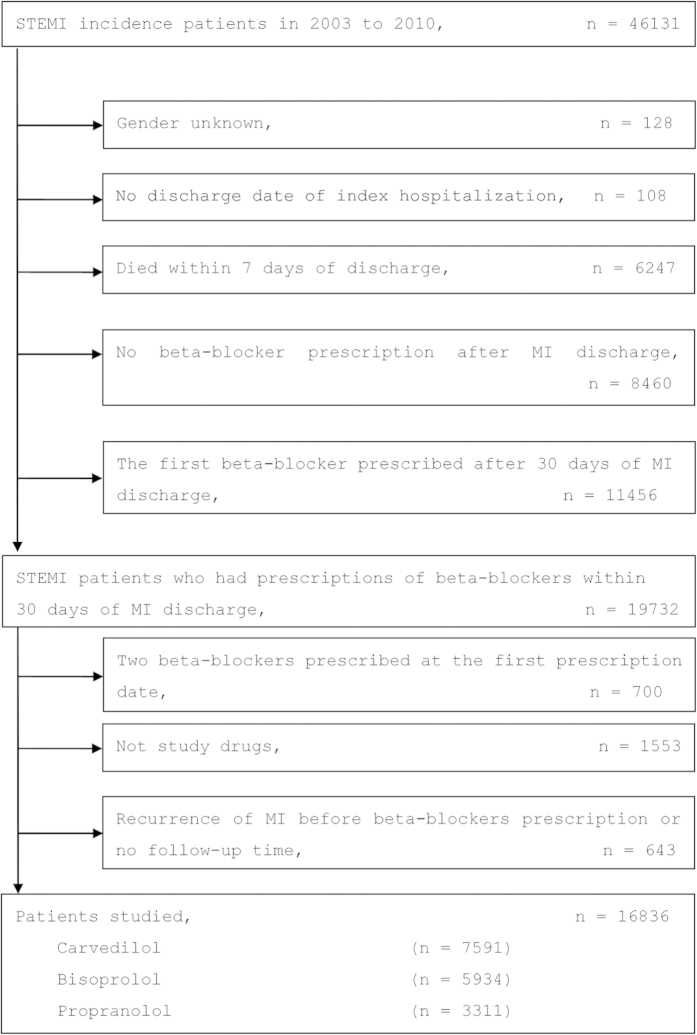
We identified a total of 16836 patients that met selection criteria in the NHI claims database for the period covering January 2003 to December 2010. Among them, 7591 (45%) patients were prescribed carvedilol, 5934 (35%) were prescribed bisoprolol, and 3311 (20%) were prescribed propranolol (Fig. 1).
Figure 1.
A flowchart illustrating the process of patient identification. Abbreviations: MI, myocardial infarction; STEMI, ST-elevation myocardial infarction .
The majority of the study population was considered to be at intermediate risk (i.e. 10%–20% 10-year risk of coronary heart disease according to the Framingham Risk Score)13. In addition, most patients were male, and the median age of subjects was 61 years. Patients prescribed bisoprolol were more likely to also have a prescription for clopidogrel or statin than patients belonging to the carvedilol group, but less likely to have prescriptions for loop diuretics, spironolactone, or amiodarone. Compared with the carvedilol group, patients prescribed propranolol were younger, less likely to suffer from congestive heart failure (CHF) or diabetes with chronic complications, and less likely to have a prescription for clopidogrel, ARBs, loop diuretics, spironolactone, statins, amiodarone, or insulin. Totally, 62.2% patients received coronary angiography during the index hospitalization; 1.9% received CABG; and 7.0% received t-PA. Comparing treatment groups, patients prescribed bisoprolol were more likely to receive coronary angiography. Conversely, patients treated with propranolol were less likely than the carvedilol group to receive coronary angiography but more likely to receive t-PA (Table 1).
Table 1. Demographic and clinical characteristics of study subjects.
|
Bisoprolol |
Propranolol |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Total | Carvedilol | p* | SD* | p† | SD† | ||
| Patients (n) | 16836 | 7591 | 5934 | 3311 | ||||
| Female (%) | 20.8 | 21.7 | 19.7 | 0.005 | 0.05 | 20.8 | 0.29 | 0.02 |
| Age (years, Mean) | 61.3 | 62.1 | 60.7 | <0.001 | 0.10 | 60.6 | <0.001 | 0.11 |
| Comorbidities (%) | ||||||||
| Congestive Heart failure | 5.8 | 6.9 | 5.2 | <0.001 | 0.07 | 4.3 | <0.001 | 0.12 |
| Cerebrovascular disease | 9.1 | 9.7 | 8.8 | 0.06 | 0.03 | 8.2 | 0.010 | 0.06 |
| Chronic pulmonary disease | 8.1 | 8.6 | 7.7 | 0.07 | 0.03 | 7.7 | 0.12 | 0.03 |
| Dementia | 1.3 | 1.4 | 1.1 | 0.15 | 0.03 | 1.3 | 0.91 | <0.01 |
| Diabetes without chronic complication | 23.6 | 24.7 | 23.8 | 0.26 | 0.02 | 20.9 | <0.001 | 0.09 |
| Diabetes with chronic complication | 7.1 | 8.4 | 6.1 | <0.001 | 0.09 | 5.5 | <0.001 | 0.12 |
| Liver disease | 5.2 | 5.2 | 5.0 | 0.58 | 0.01 | 5.5 | 0.55 | 0.01 |
| Peptic ulcer disease | 9.7 | 9.6 | 9.6 | 0.97 | <0.01 | 10.2 | 0.31 | 0.02 |
| Renal disease | 4.9 | 5.6 | 4.4 | 0.002 | 0.06 | 4.1 | 0.001 | 0.07 |
| Prescriptions at discharge (%) | ||||||||
| Aspirin | 96.9 | 96.7 | 97.5 | 0.009 | 0.05 | 96.3 | 0.34 | 0.02 |
| Clopidogrel | 88.0 | 88.7 | 92.7 | <0.001 | 0.14 | 78.1 | <0.001 | 0.29 |
| Warfarin | 3.0 | 3.6 | 2.3 | <0.001 | 0.08 | 2.7 | 0.028 | 0.05 |
| CCBs | 23.8 | 23.1 | 24.3 | 0.12 | 0.03 | 24.6 | 0.08 | 0.04 |
| ACEIs | 73.9 | 75.6 | 72.6 | <0.001 | 0.07 | 72.4 | <0.001 | 0.07 |
| ARBs | 19.8 | 20.1 | 23.3 | <0.001 | 0.08 | 13.1 | <0.001 | 0.19 |
| Loop diuretics | 37.0 | 44.5 | 33.0 | <0.001 | 0.24 | 26.9 | <0.001 | 0.37 |
| Spironolactone | 10.6 | 13.6 | 9.6 | <0.001 | 0.13 | 5.5 | <0.001 | 0.28 |
| Statins | 55.7 | 53.9 | 63.4 | <0.001 | 0.19 | 46.0 | <0.001 | 0.16 |
| Amiodarone | 13.6 | 16.2 | 12.4 | <0.001 | 0.11 | 10.0 | <0.001 | 0.18 |
| OADs | 27.0 | 28.2 | 27.2 | 0.22 | 0.02 | 23.8 | <0.001 | 0.10 |
| Insulin | 20.1 | 22.4 | 18.7 | <0.001 | 0.09 | 17.1 | <0.001 | 0.13 |
| Medical utilizations (median) | ||||||||
| Number of OPD visits | 16 | 16 | 16 | 0.95 | <0.01 | 16 | 0.69 | 0.03 |
| Number of hospitalizations | 0 | 0 | 0 | 0.93 | 0.05 | 0 | 0.10 | 0.03 |
| Cardiac procedures during index hospitalization (%) | ||||||||
| Coronary angiography | 62.2 | 60.5 | 72.1 | <0.001 | 0.25 | 48.6 | <0.001 | 0.25 |
| CABG | 1.9 | 2.2 | 1.9 | 0.34 | 0.02 | 1.4 | 0.004 | 0.06 |
| t-PA | 7.0 | 6.2 | 5.4 | 0.06 | 0.03 | 11.8 | <0.001 | 0.20 |
Abbreviations: ACEI, angiotensin-converting-enzyme inhibitor; ARB, angiotensin receptor blocker; CABG, coronary artery bypass graft; CCB, calcium channel blocker; OAD, oral anti-diabetic drug; OPD, out-patient department; SD, standardized difference; t-PA, tissue plasminogen activator.
*Bisoprolol vs. Carvedilol.
†Propranolol vs. Carvedilol.
Main results
The mean follow-up time was 1.0 year, ending on Dec. 31, 2011. Overall, the accumulated incidence of all-cause death was 3.7%; for cardiovascular death, it was 1.8%; and the recurrence of MI was 7.3% (Table 2). In the unadjusted Cox model, treatment with bisopolol was associated with a lower risk of all-cause death (unadjusted hazard ratio [HR] 0.62, 95% confidence interval [CI] 0.52–0.74, p < 0.001) and cardiovascular death (unadjusted HR 0.64, 95% CI 0.50–0.82, P < 0.001) than treatment with carvedilol. Treatment with propranolol also presented a lower risk of cardiovascular death (unadjusted HR 0.66, 95% CI 0.46–0.95, p = 0.024) than the carvedilol group (Table 3).
Table 2. Clinical outcomes associated with the three beta-blocker groups.
| Total | Carvedilol | Bisoprolol | Propranolol | |
|---|---|---|---|---|
| n | 16836 | 7591 | 5934 | 3311 |
| Follow-up time (years) | ||||
| Mean (SD) | 1.0 (1.3) | 1.0 (1.3) | 1.3 (1.4) | 0.6 (1.0) |
| All-cause death, n (%) | 624 (3.7%) | 345 (4.5%) | 193 (33%) | 86 (2.6%) |
| CV death, n (%) | 309 (1.8%) | 174 (2.3%) | 99 (1.7%) | 36 (1.1%) |
| Recurrence of MI, n (%) | 1229 (7.3%) | 564 (7.4%) | 442 (7.5%) | 223 (6.7%) |
Abbreviations: CV, cardiovascular; MI, myocardial infarction; SD, standard deviation.
Table 3. Relative risks of various clinical outcomes associated with the three beta-blocker groups.
| All-cause death | CV death | Recurrence of MI | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Crude results | |||||||||
| Drug | HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p |
| Carvedilol | 1 | 1 | 1 | ||||||
| Bisoprolol | 0.62 | (0.52–0.74) | <0.001 | 0.64 | (0.50–0.82) | <0.001 | 0.92 | (0.81–1.04) | 0.18 |
| Propranolol | 0.81 | (0.64–1.03) | 0.08 | 0.66 | (0.46–0.95) | 0.024 | 1.12 | (0.96–1.31) | 0.16 |
| Simultaneous three-group comparison with adjustment for the propensity scores* | |||||||||
| Carvedilol | 1 | 1 | 1 | ||||||
| Bisoprolol | 0.87 | (0.72–1.05) | 0.14 | 0.87 | (0.68–1.13) | 0.30 | 0.97 | (0.85–1.10) | 0.63 |
| Propranolol | 1.07 | (0.84–1.36) | 0.58 | 0.92 | (0.64–1.32) | 0.64 | 1.14 | (0.97–1.33) | 0.12 |
| Pairwise contrast with adjustment for the propensity scores† | |||||||||
| Carvedilol | 1 | 1 | 1 | ||||||
| Bisoprolol | 0.88 | (0.73–1.06) | 0.17 | 0.88 | (0.68–1.13) | 0.31 | 0.98 | (0.86–1.12) | 0.76 |
| Propranolol | 1.06 | (0.83–1.36) | 0.62 | 0.90 | (0.62–1.31) | 0.58 | 1.12 | (0.95–1.31) | 0.18 |
| Pairwise contrast with stratification on quintiles of the propensity scores‡ | |||||||||
| Carvedilol | 1 | 1 | 1 | ||||||
| Bisoprolol | 0.86 | (0.72–1.04) | 0.11 | 0.87 | (0.67–1.13) | 0.29 | 0.98 | (0.86–1.12) | 0.77 |
| Propranolol | 1.04 | (0.81–1.33) | 0.77 | 0.89 | (0.61–1.29) | 0.53 | 1.13 | (0.96–1.33) | 0.14 |
*Simultaneous three-group comparison using the Cox proportional hazards model with adjustment for age, sex, and the propensity scores in which carvedilol is treated as the reference group.
†Repeated pairwise comparison using the Cox proportional hazards model with adjustment for age, sex, and the propensity scores in which carvedilol is treated as the reference group.
‡Repeated pairwise comparison using the Cox proportional hazards model with adjustment for age, sex, and stratified on quintiles of the propensity scores in which carvedilol is treated as the reference group.
However, using a simultaneous three-group comparison approach and adjusting for age, sex, and the propensity scores, we found no difference between the bisoprolol group and the carvedilol group with regard to risks of all-cause death (adjusted HR 0.87, 95% CI 0.72–1.05, p = 0.14), cardiovascular death (adjusted HR 0.87, 95% CI 0.68–1.13, p = 0.30), and recurrence of MI (adjusted HR 0.97, 95% CI 0.85–1.10, p = 0.63). Similarly, patients treated with propranolol and patients treated with carvedilol presented similar risk levels with regard to all-cause death (adjusted HR 1.07, 95% CI 0.84–1.36, p = 0.58), cardiovascular death (adjusted HR 0.92, 95% CI 0.64–1.32, p = 0.64) and recurrence of MI (adjusted HR 1.14, 95% CI 0.97–1.33, p = 0.12). The analyses using the pairwise contrast approach (either with adjustment for the propensity scores or stratification on the propensity score quintiles) yielded similar results (Table 3).
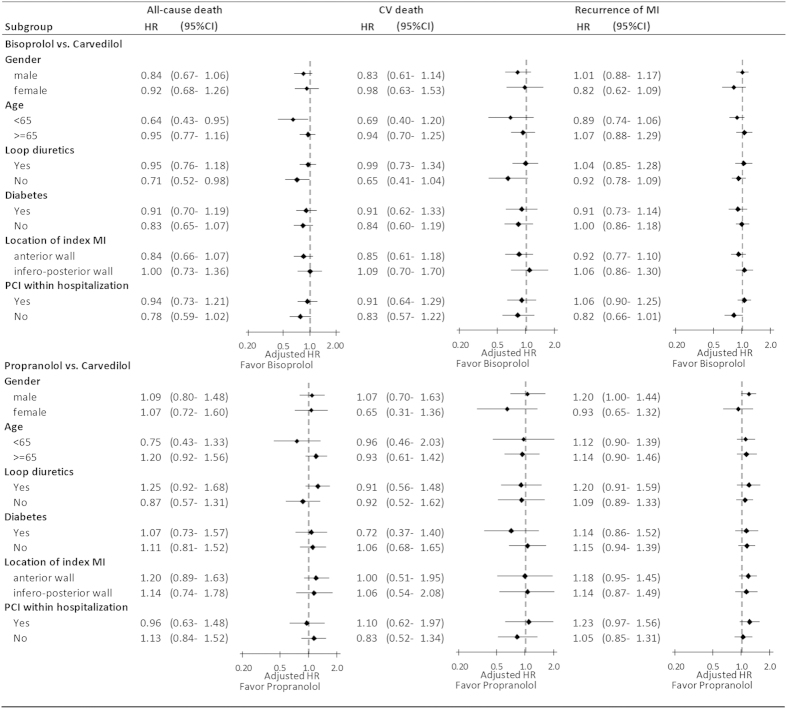
Subgroup analyses
The lack of difference in risks of clinical outcomes between the three beta-blockers was consisted in most of the prespecified subgroups including gender, age, use/non-use of loop diuretics, diabetes status, location of the index MI and receiving PCI or not during the index hospitalization. However, we found an association between bisoprolol and a reduced risk of all-cause death among younger (<65 years old) patients (adjusted HR 0.64, 95% CI 0.43–0.95) and patients not receiving loop diuretics (adjusted HR 0.71, 95% CI 0.52–0.98) in comparison with carvedilol group (Fig. 2).
Figure 2. Relative risks of various clinical outcomes associated with the three beta-blockers, stratified according to subgroups.
Abbreviations: CI, confidence interval; CV, cardiovascular; HR, hazard ratio; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Sensitivity analyses
In the two sensitivity analyses, the exclusion criterion of beta-blockers prescribed more than 30 days after discharge was replaced with 14 days and 42 days, respectively. All the results remained unchanged in both sensitivity analyses (supplementary Table 1 and Table 2).
Discussion
For this study, we investigated three beta-blockers that are most commonly prescribed in Taiwan (Supplementary Table 3). Carvedilol, a non-selective beta-blocker with alpha-blocker activity, has pleiotropic effects including anti-oxidation and vasodilation14. Bisoprolol is a selective beta-1 receptor blocker without intrinsic sympathomimetic activity (ISA). In contrast, propranolol is a non-selective beta-blocker with a shorter half-life. The primary purpose of this study was to examine whether beta-blockers exert a class effect in terms of reducing mortality in post-MI patients. Our unadjusted results indicate that bisoprolol and propranolol may be more effective in this regard. Nevertheless, following adjustment for baseline characteristics, no differences related to risk of all-cause death, cardiovascular death, or recurrence of MI were observed between carvedilol, bisoprolol, and propranolol groups.
Prior to the era of reperfusion and thrombolytics, a meta-regression analysis had found that treating post-MI patients with beta-blockers at the time of discharge improved survival by approximately 25%15. Furthermore, in the Carvedilol Post-Infarct Survival Control in LV Dysfunction (CAPRICORN) study and other studies on acute MI patients, carvedilol was also shown to reduce overall mortality16,17. Similar reductions in mortality were reported in trials investigating the effect of propranolol among post-MI patients5,18,19. Bisoprolol was shown to reduce all-cause mortality in patients with heart failure. However, no trial has been conducted to evaluate treatment efficacy of bisoprolol in patients with acute MI20. Although current guidelines support the use of beta-blockers in all eligible MI survivors1,6, a number of head-to-head comparisons between various types of beta-blockers have yielded conflicting conclusions. For example, one open-label study comparing carvedilol with atenolol showed no significant differences in primary endpoints after a median follow-up time of 1.6 years21. Another study of 313 patients that compared metoprolol with carvedilol over a mean duration of 13.4 months also found no differences with regard to different clinical endpoints22. However, one meta-analysis indicated that the efficacy of carvedilol in reducing all-cause mortality significantly exceeded that of selective beta-1 blockers (atenolol, bisoprolol, metoprolol, and nebivolol) in MI patients23. Higher mortality rates were observed in patients received metoprolol compared with those that received atenolol or acebutolol24. Furthermore, patients prescribed propranolol at the time of discharge presented a slightly higher mortality rate than patients prescribed metoprolol or atenolol25. These conflicting findings suggest that the assumption that beta-blockers exert a class effect for secondary prevention after acute MI is questionable. Besides, a few researchers proposed that the ancillary properties (i.e., ISA, beta 1-selectivity, membrane stabilizing activity, and lipophilicity) of different beta-blockers might have influence on their clinical efficacy26.
The all-cause death rate in our study was 3.7%, which is similar to the results obtained from other studies conducted among post-MI patients treated with beta-blockers in the contemporary PCI era (approximately 3–4% over a one-year follow-up)9,10,27. The crude results of our study seem to indicate that the use of bisoprolol or propranolol is associated with a reduction in all-cause death and cardiovascular death compared with use of carvedilol. However, significant differences were observed in baseline demographics and clinical characteristics of patients treated with different beta-blockers. Overall, patients prescribed carvedilol were more likely to have CHF and used more medications (such as loop diuretics, spironolactone, and amiodarone) compared with patients in the bisorpolol and propranolol groups. After adjusting for baseline characteristics, no significant differences were observed between the three beta-blockers with regard to effectiveness in reducing mortality. All the three different methods of statistical analysis yielded the same results, demonstrating the robustness of our findings. Our results imply a class effect of beta-blockers in the treatment of patients suffering from STEMI and support the concept that specific beta-blockers have little influence on mortality21,22,25
CHF is a common complication of acute MI and presents in 20–30% of MI survivors28,29,30,31. In the literature, carvedilol, bisoprolol, and metoprolol succinate are the preferred drugs for patients with a reduced left ventricle ejection fraction (LVEF)32,33. Although there was no individual LVEF in our database, we chose the use of loop diuretics at discharge as a surrogate for presence of CHF after the index MI. In our study, the proportion of patients prescribed loop diuretics at discharge was 37%, which was similar to the prevalence rate of CHF in several registries and clinical trials concerning acute MI patients28,29,30,31. In our subgroup analysis, we still noted no differences between the three study drugs with regard to the risks of different clinical outcomes among patients prescribed loop diuretics at discharge.
Study limitations
A number of limitations in the present study must be acknowledged. Firstly, in most previous studies, metoprolol was examined with regard to its effects in the secondary prevention in post-MI patients. However, the patient population using metorpolol in Taiwan was too small to be included in our analysis (Supplementary Table 3). Secondly, we were unable to conduct a randomized, controlled trial; therefore, our results may have been affected by defects inherent to non-randomized comparisons. These include selection bias and an uneven distribution of risk factors. To address these issues, we conducted several statistical methods with utilization of propensity scores to control for detected differences between groups. Thirdly, although we attempted to control for the majority of known risk factors, it is possible that some factors were not properly accounted for. For example, we were unable to access data related to LVEF or drug adherence, as this information is not available in the NHI database. We tried to control for left ventricular dysfunction using prescriptions of loop diuretics as a proxy for left ventricular systolic dysfunction. However, the results may vary according to different LVEF. Besides, the inability to evaluate patient compliance in taking the prescribed beta-blockers means that their true effects may have been under-represented. Fourthly, our follow-up duration (one-year) was shorter than that of many large trials and registries (i.e. a median follow-up time of between two and four years10,27,34). The similar outcomes associated with the three drugs investigated may therefore be due to a lack of power and a follow-up of insufficient duration. Finally, we did not adjust for in-hospital administration of beta-blockers; therefore, we are unable to evaluate the benefits of early beta-blocker usage after acute MI, as reported in the Effect of Metoprolol in Cardioprotection During an Acute Myocardial Infarction (METOCARD-CNIC) trial35.
Conclusions
In the real-world population-based setting of Taiwan, carvedilol, bisoprolol and propranolol possessed similar clinical effectiveness in STEMI survivors. In spite of the exclusion of metoprolol, one of the most commonly used cardioselective beta-blockers in other countries, our results are still suggestive of a possible class effect of beta-blockers.
Materials and Methods
Sources of data
The NHI program has provided compulsory universal health insurance in Taiwan since 1995. More than 98% of the entire Taiwanese population of 23 million is covered by the program. All medical institutions contracted with the NHI must submit standard computerized claims in order to obtain reimbursement. As a result, the NHI claims database contains a nearly complete history of diagnoses (classified according to the International Classification of Diseases Ninth Revision Clinical Modification [ICD-9-CM] codes) as well as records for medical procedures and drugs dispensed. In this study, we extracted all of the records of the study subjects from the NHI claims database and linked to the National Death Registry (NDR) for mortality outcomes using the identification number of each patient. To comply with data privacy regulations, personal identities were encrypted and all data were analyzed in a de-identified manner. The protocol for this study was approved by the Institutional Review Board of National Taiwan University Hospital.
Study population
The NHI claims database was investigated for the period covering 1998 to 2011. We identified all patients who were above 18 years old and had their first hospitalization for STEMI (ICD-9-CM codes, 410.1–410.6 and 410.8) between January 2003 and December 2010. Several exclusion criteria were applied to increase the reliability and validity of our results. Specifically, patients were excluded if: (1) they had previously been hospitalized for acute MI between 1998 and 2002, (2) their gender was unknown, (3) the discharge date was missed in the index hospitalization, (4) death occurred within 7 days of discharge, (5) MI recurred prior to the initial prescription of beta-blockers, (6) they were prescribed two beta-blockers at the same time, (7) they were prescribed beta-blockers other than the drugs specified in the study, (8) beta-blockers were not prescribed following discharge throughout the study period or were prescribed 30 days after discharge. A flowchart of the process used to identify study subjects is presented in Fig. 1.
Drug use, covariates, and outcomes
Three most commonly prescribed beta-blockers, carvedilol, bisoprolol, and propranolol, in post-MI population in Taiwan were included in the current study (Supplementary Table 3). Patients were classified as users of carvedilol, bisoprolol, or propranolol based on the first prescription filled for a beta-blocker within 30 days post discharge. The date of the first beta-blocker prescription was operationally defined as the index date. In addition to recording gender and age on index date, we evaluated comorbidities based on NHI claims data filed within the twelve-month baseline period prior to the index date. Specifically, we obtained information for several comorbidities, including CHF, cerebrovascular disease, chronic pulmonary disease, dementia, diabetes, liver disease, peptic ulcer disease, and renal disease, in accordance with Charlson comorbidity measurements36. The presence of a comorbid condition was defined as the specific diagnosis codes recorded in claims data for at least two times on different days within the twelve-month baseline period. Individual comorbid conditions were evaluated and coded as binary variables. Medications that were prescribed at discharge during the index hospitalization, including aspirin, clopidogrel, warfarin, calcium channel blockers (CCBs), angiotensin-converting-enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), loop diuretics, spironolactone, statins, amiodarone, oral anti-diabetic drugs (OADs), and insulin were identified. For health care utilizations, we recorded the numbers of out-patient and in-patient services each patient used within the twelve-month baseline period prior to the index date. During the index hospitalization, cardiac procedures including coronary angiography, coronary artery bypass graft (CABG), and the use of tissue plasminogen activator (t-PA) were also evaluated.
Due to the availability of NHI and NDR data, the mortality of study subjects and other clinical outcomes were assessed through to December 31, 2011. Subjects were censored if they switched to another beta-blocker, in cases where study drugs were discontinued for more than 30 days, or at the end of the follow-up period. Study outcomes included all-cause death, cardiovascular death (ICD-9-CM codes, 401–449 as the cause of death), and recurrence of MI (ICD-9-CM codes, 401.0–410.9 in discharge diagnoses).
Statistical analyses
To enable a comparison of baseline characteristics between the three beta-blockers groups, the χ2 test, the two sample t-test and the Mann-Whitney U test were used with the carvedilol group as the reference. We used standardized difference to measure covariate balance, whereby an absolute standardized difference of greater than 10% represented meaningful imbalance.
Because of the heterogeneity of three groups, the propensity scores were constructed using multinomial logistic regression to model the receipt of different beta-blockers as a function of baseline patient characteristics37,38. All the background characteristics listed in Table 1, such as age, gender, comorbidities, medications, medical utilizations and procedures received during the index hospitalization, were included in the multinomial logistic regression model during construction of the propensity scores. As propensity score – matching usually results in marked reduction in sample size39,40, a simultaneous three-group comparison approach using the Cox regression model with adjustment for age, sex, and the propensity scores was used to compare the relative risks of various outcomes associated with the three beta-blockers37,41. Carvedilol, the beta-blocker most frequently used by MI patients in Taiwan, was selected a priori as the reference category. We also applied the pairwise contrast methods using the Cox regression model with adjustment for the propensity scores and the Cox regression model stratified on quintiles of the propensity scores. Subgroup analysis was also performed using the simultaneous three-group comparison approach, and the subgroups included gender, age, use/non-use of loop diuretics, diabetes status, location of the index MI and receiving PCI or not during the index hospitalization.
In the primary analysis, patients who were prescribed beta-blockers after 30 days of discharge were excluded. Since the 30-day criterion was arbitrary, we also performed two sensitivity analysis with 14-day and 42-day exclusion criteria to test the robustness of our study design and results.
All analyses were performed using SAS 9.2 software (SAS Institute Inc., Cary, North Carolina). A p-value of <0.05 was considered statistically significant.
Additional Information
How to cite this article: Lin, T.-T. et al. Class effect of beta-blockers in survivors of ST-elevation myocardial infarction: A nationwide cohort study using an insurance claims database. Sci. Rep. 5, 13692; doi: 10.1038/srep13692 (2015).
Supplementary Material
Acknowledgments
All the data used in this study was released and approved by the Collaboration Center of Health Information Application (CCHIA), Ministry of Health and Welfare, Executive Yuan, Taiwan. Source of funding: This study was supported by grants from the Science and Technology Unit, Ministry of Health and Welfare, Executive Yuan, Taiwan (DOH 101-TD-B-111-001 and DOH 102-TD-B-111-001).
Footnotes
Author Contributions The specific contributions made to this article by the listed authors are as follows: Ting-Tse Lin drafted the manuscript. Ho-Min Chen performed data analysis. K. Arnold Chan, Mei-Shu Lai, and Chao-Lun Lai designed the study. Chao-Lun Lai revised the manuscript and took responsibility for the interpretation of the results. All authors have reviewed the manuscript.
References
- O’Gara P. T. et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 82, E1–27. (2013). [DOI] [PubMed] [Google Scholar]
- Lopez-Sendon J. et al. Expert consensus document on beta-adrenergic receptor blockers. Eur Heart J. 25, 1341–1362 (2004). [DOI] [PubMed] [Google Scholar]
- Roberts R. et al. Immediate versus deferred beta-blockade following thrombolytic therapy in patients with acute myocardial infarction. Results of the Thrombolysis in Myocardial Infarction (TIMI) II-B Study. Circulation . 83, 422–437 (1991). [DOI] [PubMed] [Google Scholar]
- Randomised trial of intravenous atenolol among 16 027 cases of suspected acute myocardial infarction: ISIS-1. First International Study of Infarct Survival Collaborative Group. Lancet . 2, 57–66 (1986). [PubMed] [Google Scholar]
- A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality results. JAMA . 247, 1707–1714 (1982). [DOI] [PubMed] [Google Scholar]
- Steg P. G. et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 33, 2569–2619 (2012). [DOI] [PubMed] [Google Scholar]
- Harjai K. J. et al. Effects of prior beta-blocker therapy on clinical outcomes after primary coronary angioplasty for acute myocardial infarction. Am J Cardiol. 91, 655–660 (2003). [DOI] [PubMed] [Google Scholar]
- Kernis S. J. et al. Does beta-blocker therapy improve clinical outcomes of acute myocardial infarction after successful primary angioplasty? J Am Coll Cardiol. 43, 1773–1779 (2004). [DOI] [PubMed] [Google Scholar]
- Choo E. H. et al. Benefit of beta-blocker treatment for patients with acute myocardial infarction and preserved systolic function after percutaneous coronary intervention. Heart. 100, 492–499 (2014). [DOI] [PubMed] [Google Scholar]
- Nakatani D. et al. Impact of beta blockade therapy on long-term mortality after ST-segment elevation acute myocardial infarction in the percutaneous coronary intervention era. Am J Cardiol. 111, 457–464. (2013). [DOI] [PubMed] [Google Scholar]
- Furberg C. D., Herrington D. M. & Psaty B. M. Are drugs within a class interchangeable? Lancet. 354, 1202–1204 (1999). [DOI] [PubMed] [Google Scholar]
- Frishman W. H. & Alwarshetty M. Beta-adrenergic blockers in systemic hypertension: pharmacokinetic considerations related to the current guidelines. Clin Pharmacokinet 41, 505–516 (2002). [DOI] [PubMed] [Google Scholar]
- D’Agostino R. B. Sr. et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 117, 743–753 (2008). [DOI] [PubMed] [Google Scholar]
- Wang R. et al. Pleiotropic effects of the beta-adrenoceptor blocker carvedilol on calcium regulation during oxidative stress-induced apoptosis in cardiomyocytes. J Pharmacol Exp Ther. 318, 45–52 (2006). [DOI] [PubMed] [Google Scholar]
- Freemantle N., Cleland J., Young P., Mason J. & Harrison J. beta Blockade after myocardial infarction: systematic review and meta regression analysis. BMJ . 318, 1730–1737 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dargie H. J. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet. 357, 1385–1390 (2001). [DOI] [PubMed] [Google Scholar]
- Basu S. et al. Beneficial effects of intravenous and oral carvedilol treatment in acute myocardial infarction. A placebo-controlled, randomized trial. Circulation. 96, 183–191 (1997). [DOI] [PubMed] [Google Scholar]
- Barber J. M., Boyle D. M., Chaturvedi N. C., Singh N. & Walsh M. J. Practolol in acute myocardial infarction. Acta Med Scand Suppl 587, 213–219 (1976). [DOI] [PubMed] [Google Scholar]
- Aronow W. S., Ahn C. & Kronzon I. Effect of propranolol versus no propranolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction > or = 40% treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol. 80, 207–209 (1997). [DOI] [PubMed] [Google Scholar]
- The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet . 353, 9–13 (1999). [PubMed] [Google Scholar]
- Jonsson G. et al. A comparison of the two beta-blockers carvedilol and atenolol on left ventricular ejection fraction and clinical endpoints after myocardial infarction. a single-centre, randomized study of 232 patients. Cardiology 103, 148–155 (2005). [DOI] [PubMed] [Google Scholar]
- Mrdovic I. B. et al. Randomized active-controlled study comparing effects of treatment with carvedilol versus metoprolol in patients with left ventricular dysfunction after acute myocardial infarction. Am Heart J. 154, 116–122 (2007). [DOI] [PubMed] [Google Scholar]
- DiNicolantonio J. J., Lavie C. J., Fares H., Menezes A. R. & O’Keefe J. H. Meta-analysis of carvedilol versus beta 1 selective beta-blockers (atenolol, bisoprolol, metoprolol, and nebivolol). Am J Cardiol. 111, 765–769. (2013). [DOI] [PubMed] [Google Scholar]
- Rinfret S. et al. A population-based analysis of the class effect of beta-blockers after myocardial infarction. Am Heart J. 153, 224–230 (2007). [DOI] [PubMed] [Google Scholar]
- Gottlieb S. S. & McCarter R. J. Comparative effects of three beta blockers (atenolol, metoprolol, and propranolol) on survival after acute myocardial infarction. Am J Cardiol. 87, 823–826 (2001). [DOI] [PubMed] [Google Scholar]
- Soriano J. B., Hoes A. W., Meems L. & Grobbee D. E. Increased survival with beta-blockers: importance of ancillary properties. Prog Cardiovasc Dis. 39, 445–456 (1997). [DOI] [PubMed] [Google Scholar]
- Ozasa N. et al. Lack of effect of oral beta-blocker therapy at discharge on long-term clinical outcomes of ST-segment elevation acute myocardial infarction after primary percutaneous coronary intervention. Am J Cardiol. 106, 1225–1233 (2010). [DOI] [PubMed] [Google Scholar]
- Jhund P. S. & McMurray J. J. Heart failure after acute myocardial infarction: a lost battle in the war on heart failure? Circulation. 118, 2019–2021 (2008). [DOI] [PubMed] [Google Scholar]
- Hasdai D. et al. Frequency, patient characteristics, and outcomes of mild-to-moderate heart failure complicating ST-segment elevation acute myocardial infarction: lessons from 4 international fibrinolytic therapy trials. Am Heart J. 145, 73–79 (2003). [DOI] [PubMed] [Google Scholar]
- Kashani A. et al. Severity of heart failure, treatments, and outcomes after fibrinolysis in patients with ST-elevation myocardial infarction. Eur Heart J. 25, 1702–1710 (2004). [DOI] [PubMed] [Google Scholar]
- Velazquez E. J. et al. An international perspective on heart failure and left ventricular systolic dysfunction complicating myocardial infarction: the VALIANT registry. Eur Heart J. 25, 1911–1919 (2004). [DOI] [PubMed] [Google Scholar]
- Yancy C. W. et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 62, e147–239 (2013). [DOI] [PubMed] [Google Scholar]
- McMurray J. J. et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 33, 1787–1847 (2012). [DOI] [PubMed] [Google Scholar]
- Bangalore S. et al. beta-Blocker use and clinical outcomes in stable outpatients with and without coronary artery disease. JAMA. 308, 1340–1349, 1310.1001/jama.2012.12559 (2012). [DOI] [PubMed] [Google Scholar]
- Pizarro G. et al. Long-term benefit of early pre-reperfusion metoprolol administration in patients with acute myocardial infarction: results from the METOCARD-CNIC trial (Effect of Metoprolol in Cardioprotection During an Acute Myocardial Infarction). J Am Coll Cardiol. 63, 2356–2362 (2014). [DOI] [PubMed] [Google Scholar]
- Quan H. et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 43, 1130–1139 (2005). [DOI] [PubMed] [Google Scholar]
- Chou H. W. et al. Risks of cardiac arrhythmia and mortality among patients using new-generation macrolides, fluoroquinolones, and beta-lactam/beta-lactamase inhibitors: a Taiwanese nationwide study. Clin Infect Dis. 60, 566–577 (2015). [DOI] [PubMed] [Google Scholar]
- Imbens G. W. The Role of the Propensity Score in Estimating Dose-Response Functions. Biometrika 87, 706–710 (2000). [Google Scholar]
- D’Agostino R. B. Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 17, 2265–2281 (1998). [DOI] [PubMed] [Google Scholar]
- Brookhart M. A., Wyss R., Layton J. B. & Sturmer T. Propensity score methods for confounding control in nonexperimental research. Circ Cardiovasc Qual Outcomes . 6, 604–611 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharya S., Abebe K., Simon M., Saba S. & Adelstein E. Role of cardiac resynchronization in end-stage heart failure patients requiring inotrope therapy. J Card Fail. 16, 931–937 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.