Abstract
Objective: To evaluate the effect of pharyngeal musculature and genioglossus exercising on obstructive sleep apnea and hypopnea syndrome (OSAHS). Methods: We conducted a non-randomized retrospective clinical trial of 75 patients with OSAHS. Fifty-four patients were managed by exercising of the pharyngeal musculature and genioglossus (exercising group). Twenty-one patients, who refused to undertake any treatment, were defined as the control group. We took the Epworth Sleepiness Scale (ESS), checked patients’ polysomnography, and took 320 detector computed tomography (CT) before treatment. Six and twelve months later, we made records of apnea hypopnea index (AHI), lowest arterial oxygen saturation (LSaO2), body mass index (BMI), the shortest sagittal diameter, and transverse diameter, and the effective rates of exercising were calculated and compared with the 21 patients without any treatment (control group) at the same time. SPSS 10.0 was used to analyze the data. Results: Before treatment, the ESS value was 7.67; 6 and 12 months later, the values were 3.54 and 3.25, respectively in the exercising group. AHI was decreased to 15.36 after 6 months and 13.79 after 12 months from 22.84 at the beginning. LSaO2 values were up to 81.18% after 6 months and 81.93% after 12 months from 74.05% at the beginning. There were significant differences in ESS scores, AHI, and LSaO2 between pre-treatment and post-treatment in the exercising group (P<0.05). However, there was no statistical difference in all the parameters between 6 and 12 months of exercising. The effective rates were 70.37% and 74.07% after 6- and 12-month exercising, respectively. There were significant differences between the exercising and control groups (P<0.0001). There was no statistical difference in the effective rate of the exercising group between 6 and 12 months of exercising (P>0.05). At 12 months of exercising, the compliance of the anteroposterior pharyngeal wall of the retropalatal area was lower (P<0.01) than that before treatment. There was no significant change of BMI in either group. Conclusions: Exercising pharyngeal musculature and genioglossus is a kind of non-invasive and cost-effective method to treat some OSAHS patients, especially those who are old, without surgical complications, and especially mild and moderate OSAHS patients who do not want to take surgery and continuous positive airway pressure (CPAP) treatment. In addition, exercising pharyngeal musculature and genioglossus can be considered as remedial treatment of OSAHS to surgery and other therapies.
Keywords: Obstructive sleep apnea and hypopnea syndrome, Non-surgical management, Exercise, Genioglossus, Valsalva maneuver, Pharyngeal musculature
1. Introduction
Obstructive sleep apnea and hypopnea syndrome (OSAHS) is a common clinical condition defined by excessive daytime sleepiness, loud snoring, and witnessed breathing pauses (at least five events of apnea/hypopnea per hour of sleep). It has been associated with a number of chronic diseases such as cardiovascular disease (Chouchou et al., 2014), hypertension (Wang et al., 2014), and metabolic disease (Zhang et al., 2014). Because of daytime hyper somnolence, there is an increased likelihood of vehicle accidents associated with OSAHS. The relationship between OSAHS and obesity in women after the menopause has been published (Kirkness et al., 2008). It has been shown that OSAHS is caused by partial or total obstruction of the upper airway, which is due to the upper airway obstruction or laryngeal soft tissue collapse during sleep. The obstruction was detected by methods such as flexible rhinolaryngoscopy, computed tomography (CT), magnetic resonance imaging (MRI), and acoustic rhinometry (Schwartz et al., 1998).
The reduction in tension and strength of the upper airway muscles is the key factor in the etiology of OSAHS (Mezzanotte et al., 1992; Kuna, 2001; Mateika and Syed, 2013; Shortt et al., 2013). These muscles include the genioglossus, petrostaphylinustensor veli palatini and palatosalpingeuslevator veli palatini, staphylinus externus, and levator veli palatine. Therefore exercises to enhance the tension and strength of these muscles might be helpful to OSAHS. Consequently, the purpose of this study is to evaluate the effect of exercising pharyngeal musculature and genioglossus on OSAHS.
2. Patients and methods
2.1. Patients
Data were collected prospectively on 105 patients who were definitely diagnosed as having OSAHS by polysomnography (PSG) overnight in the ENT (ear nose throat) Department of the First Hospital of Ningbo City (Ningbo, China) from January 2010 to April 2012. Some presented with the symptoms including feeling tired, sleepy and fatigued during the day, frequent snoring, and witnessed apnea; some were referred by other physicians while being treated for hypertension. Thirty patients with tonsillar hypertrophy, adenoidal hypertrophy, any maxillofacial deformity, the presence of laryngopharyngeal and neck tumors, clinical and biochemical evidence of hypothyroidism, any neuromuscular disorder and other sleep-related diseases were excluded. Fifty-four patients treated by the pharyngeal musculature exercising were defined as the exercising group. Twenty-one patients refused any treatment in a 12-month period and were defined as the control group. Their age, height, and weight were matched. A standard history was taken and physical examination was performed. Parameters including patient age, gender, weight, height, and body mass index (BMI), the apnea hypopnea index (AHI) and the lowest arterial oxygen saturation (LSaO2) were recorded. Polysomnography (PSG) was employed to ensure that AHI and LSaO2 met the American Academy of Sleep Medicine Criteria (1999). The effective rate was calculated according to guidelines for the diagnosis and surgical treatment of OSAHS, which was made by the Chinese Medicine Association (Editorial Board of Chinese Journal of Otorhinolaryngology Head and Neck Surgery, 2009).
All patients were instructed in lifestyle changes such as reducing weight, quitting smoking, reducing or ceasing the use of alcohol, and trying to sleep in a lateral position only. They were supported by both their family members and their doctors by telephone.
This study was approved by the Ethics Review Committee of the Ningbo First Hospital (Ningbo, China).
2.2. Testing methods
All the patients were scored by the Epworth Sleepiness Scale (ESS). The scores for subjective symptoms were designed and counted by the questionnaire below, which relates to the most common symptoms mentioned by patients and their families:
(1) Do you snore loudly (louder than talking or loud enough to be heard through closed doors)
(2) Do you often feel tired, fatigued, or sleepy during the day
(3) Has anyone observed you to stop breathing during your sleep
(4) Do you suffer from poor or lack of concentration
(5) Do you suffer from memory impairment
(6) Has anyone observed you moving significantly during your sleep
(7) Do you feel thirsty and have bad breath in the morning when you wake up
(8) Has anyone observed you salivating significantly at night
As to the score system, 0 represents none, 1 represents occasional somnolence, 2 represents sometimes, and 3 represents frequent somnolence.
The overnight PSG provided the records of AHI, LSaO2, and BMI.
Since MRI produces poor images of the craniofacial skeleton, costs more, and cannot be completed in the duration of the holding of a single breath or obtain dynamic images, our study chose 320-detector CT scanning instead. A 320-detector CT scan was used for continuous scanning of the upper airway and reconstructed in two planes including the sagittal position and horizontal position stages. Scanning images were also made in two phases: first, the end of a normal deep inspiration; second, at the deepest inspiration against a closed glottis as performed in the Valsalva maneuver. Scanning was performed in a conscious patient in the supine position, with the head and neck in the neutral position. The patient was instructed not to swallow or speak during the scanning imaging process. The scan covered the airway from the roof of the nasopharynx inferiorly to the subglottis. The images were used to calculate the minimum sagittal diameter and transverse diameter of the retropalatal region and retroglossal region during the quiet breathing phase and the Valsalva maneuver phase. The slice thickness was 0.5 mm, and the scan speed was 0.35 s per rotation. The compliances of the lateral pharyngeal wall, anteroposterior pharyngeal wall, and total pharyngeal wall of the retropalatal and retroglossal regions were calculated as follows.
The compliance of the lateral pharyngeal wall=(the minimal lateral diameter at expiration during quiet breathing−the minimal lateral diameter at expiration during the Valsalva maneuver)/the minimal lateral diameter at expiration during quiet breathing.
The compliance of the anteroposterior pharyngeal wall=(the minimal anteroposterior diameter at expiration during quiet breathing−the minimal anteroposterior diameter at expiration during the Valsalva maneuver)/the minimal anteroposterior diameter at expiration during quiet breathing.
The compliance of the total lateral pharyngeal wall of the retropalatal or retroglossal area=(the minimal volume of the pharyngeal wall at inspiration during quiet breathing−the minimal volume of the pharyngeal wall at inspiration during the Valsalva maneuver)/the minimal volume of the pharyngeal wall at inspiration during quiet breathing.
Each patient in both the treated exercising group and control group was followed up for one year, with investigations of ESS, PSG, and BMI at the end of 6 and 12 months. Thirty-five of 54 patients in the exercising group underwent 320-detector CT scanning after 12 months of treatment. The investigations were performed by the same investigators as at the initial point of the study.
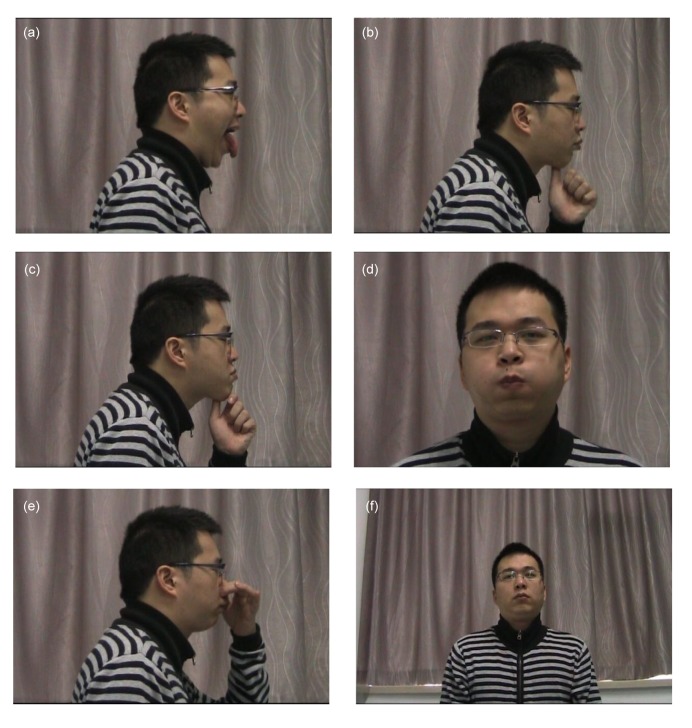
2.3. Exercising methods
Those patients in the exercising group were instructed to perform the following exercises: (1) Open mouth and stretch tongue ten times every day and night (Fig. 1a); (2) Use the thumb pad to massage the submental area for one minute every day (Fig. 1b); (3) Use thumb to push the chin forward and upward ten times every day (Fig. 1c); (4) Blow out the cheeks ten times a day for at least five seconds each time (Fig. 1d); (5) Hold the nose, close the mouth, and blow (Valsalva maneuver) ten times a day for at least five seconds each time (Fig. 1e); (6) Close the mouth, inhale and exhale slowly and deeply through the nose 20 times every night (Fig. 1f).
Fig. 1.
Patients’ exercising method
(a) Open mouth and stretch tongue ten times every day and night; (b) Use the thumb pad to massage the submental area for one minute every day; (c) Use thumb to push the chin forward and upward ten times every day; (d) Blow out the cheeks ten times a day for at least five seconds each time; (e) Hold the nose, close the mouth, and blow (Valsalva maneuver) ten times a day for at least five seconds each time; (f) Close the mouth, inhale and exhale slowly and deeply through the nose 20 times every night
The frequency and time were designed and adjusted according to the compliance of patients. Before the exercises, patients of the exercising group were asked to do as many as possible of the moves within seven days. Our doctors recorded the frequency and time in which patients could insist on exercising, then the minimum frequency and time were sorted out as mentioned above. All the patients were under medical supervision by telephone.
Patients who suffered illnesses such as upper respiratory tract infections were told to cease the exercises until they recovered. Six patients experienced flu and all recovered in one week.
2.4. Statistical analysis
The Wilcoxon signed-rank test was used to compare the questionnaire scores. The paired-samples t-test was used to compare the AHI, LSaO2, and BMI scores of 54 patients in the exercising group between pre-treatment and post-treatment at 6 and 12 months. The Pearson’s chi-squared test was used for the comparison of effective rates between the exercising and control groups and within the exercising group after 6 and 12 months of exercising. The independent samples t-test was used for comparison of the total resilience of the postpalate area and the postlingual area, and the resilience of the lateral pharyngeal wall and anteroposterior wall between exercising and control groups before treatment and 12 months later by SPSS 10.0. A P-value less than 0.05 was considered to be statistically significant.
3. Results
The characteristics of the patients are shown in Table 1. According to the Chinese OSAHS criteria (Editorial Board of Chinese Journal of Otorhinolaryngology Head and Neck Surgery, 2009), all patients were graded as follows: mild (AHI ranging from 5 to 20), moderate (AHI ranging from 21 to 40), severe (AHI is more than 40).
Table 1.
Subject characteristics
| Group | Total number (male:female) | Age (year) | BMI | AHI | LSaO2 (%) | Grade |
||
| Mild | Moderate | Severe | ||||||
| Exercising | 54 (30:24) | 41 (20–68) | 26.60 (18.80–45.60) | 22.84 (5.20–69.30) | 74.05 (34.00–87.00) | 23 (42.60%) | 15 (27.78%) | 16 (29.63%) |
| Control | 21 (14:7) | 39 (31–54) | 26.10 (22.50–39.60) | 20.90 (18.00–64.20) | 71.60 (51.00–85.00) | 10 (47.62%) | 5 (23.81%) | 6 (28.57%) |
Data are expressed as median (range) or n (%). BMI: body mass index; AHI: apnea hypopnea index; LSaO2: lowest arterial oxygen saturation
After 6 and 12 months of exercising, the AHI was reduced in all patients of the exercising group, the daytime tiredness improved and the volume of snoring diminished, as indicated by their family members. The values of ESS, AHI, LSaO2, and BMI pre-treatment and at 6 and 12 months are shown in Table 2.
Table 2.
Comparisons of ESS, questionnaire scores, BMI, AHI, and LSaO2 of the exercising group between pre- and post-treatment
| Time | BMI | ESS | Questionnaire scores | AHI | LSaO2 |
| Pre-treatment (n=54) | 26.4±10.6 | 7.67±3.58* # | 17.08±5.84* # | 22.84±19.65* # | 74.05±13.86* # |
| Post-treatment (n=54) | |||||
| 6 months | 25.7±12.3 | 3.54±2.23 | 14.47±4.97 | 15.36±16.76 | 81.18±6.89 |
| 12 months | 27.5±15.8 | 3.25±1.45 | 14.35±4.82 | 13.79±17.51 | 81.93±13.69 |
Data are expressed as mean±standard deviation (SD).
P<0.05 compared with 6-month exercising;
P<0.05 compared with 12-month exercising
The mean ESS score decreased from 7.67 at pre-treatment to 3.54 and 3.25 after 6 and 12 months of exercise, respectively. The mean AHI score reduced from 22.84 pre-treatment to 15.36 and 13.79 after 6 and 12 months, respectively. The mean LSaO2 score increased from 74.05% pre-exercise to 81.18% and 81.93% after 6 and 12 months, respectively.
There was statistical significance (P<0.05) between pre-treatment and after 6 or 12 months of treatment in all parameters except BMI. There was no statistical difference in the scores of the ESS, questionnaire, AHI, or LSaO2 (P>0.05) between 6- and 12-month intervals.
Table 3 shows that the effective rates of the exercising group were 70.37% and 74.07% after 6 and 12 months of exercising, respectively. There was no significant difference between them. However, the differences were significant between the exercising and control groups after both 6 and 12 months of exercising.
Table 3.
Comparisons of the effective rates of the exercising and control groups after 6- and 12-month intervals
| Group | Number of patients |
Effective rate (%) | |||
| Recovery | Marked improvement | Slight improvement | No improvement | ||
| 6 months | |||||
| Exercising (n=54) | 6 | 11 | 21 | 16 | 70.37* |
| Control (n=21) | 0 | 0 | 0 | 21 | 0 |
| 12 months | |||||
| Exercising (n=54) | 8 | 15 | 17 | 14 | 74.07# |
| Control (n=21) | 0 | 0 | 0 | 21 | 0 |
P<0.05 compared with 6-month control group;
P<0.05 compared with 12-month control group
Table 4 shows the compliance of the different parts of the pharyngeal wall. There was a significant difference between the compliance of the retropalatal anteroposterior pharyngeal wall before and after the 12-month treatment period in the exercising group (P<0.05). No significant differences were found in the compliance of other areas of the pharyngeal wall between pre-treatment and post-treatment in the exercising group and the control group. An example (Fig. 2) is given here. Fig. 2a shows one patient’s minimal pharyngeal wall volume (retropalatal area) to be 10.6 mm×6.6 mm×0.5 mm during quiet breathing. Fig. 2b shows the patient’s minimal transverse diameters of retropalatal and retroglossal areas to be 4.5 mm and 8.0 mm, respectively. After 12 months of exercise, the data changed to 11.8 mm×7.8 mm×0.5 mm, 6.1 mm, and 8.8 mm, as shown in Figs. 2c and 2d.
Table 4.
Comparison of the compliance of the pharyngeal wall in different layers between pre- and post-treatment
| Group | Retropalatal (pharyngeal wall) | Retroglossal (pharyngeal wall) | ||||
| Anteroposterior | Lateral | Total | Anteroposterior | Lateral | Total | |
| Exercising (n=54) | ||||||
| Pre-treatment | 0.57±0.32* | 0.58±0.26 | 0.81±0.30 | 0.39±0.15 | 0.39±0.10 | 0.67±0.14 |
| 12 months | 0.39±0.22 | 0.48±0.16 | 0.65±0.23 | 0.37±0.13 | 0.34±0.14 | 0.62±0.11 |
| Control (n=21) | ||||||
| Pre-treatment | 0.55±0.43 | 0.66±0.35 | 0.88±0.17 | 0.35±0.20 | 0.39±0.06 | 0.68±0.11 |
| 12 months | 0.54±0.36 | 0.66±0.28 | 0.87±0.45 | 0.47±0.27 | 0.30±0.20 | 0.64±0.21 |
Data are expressed as mean±SD.
P<0.05 compared with 12-month exercising
Fig. 2.

320-detector CT scan of the patient before and after the 12-month treatment period in the exercising group
Retropalatal area volume and minimal transverse diameters of retropalatal and retroglossal areas are indicated with white arrows
4. Discussion
Therapies for the management of OSAHS include continuous positive airway pressure (CPAP), mandibular advancement devices (MAD) (Quinnell et al., 2014), changes of lifestyle such as weight loss, and surgery. Surgery includes uvulopalatopharyngoplasty, mandibular advancement, suprahyoid tensing, nasal surgery, and tracheostomy. Surgery may benefit some patients in the short term; however, the effect of surgery in the long term is not defined. Additionally, potential complications are associated with surgery, including airway obstruction, apnea, hemorrhage, velopharyngeal insufficiency, and cerebral vascular accident peri-operatively. New therapies for obstructive sleep apnea (OSA) exist (White, 2014). Hypoglossal nerve stimulation was designed to activate the upper airway muscles, and it has worked well in a selective group of OSA patients. The Winx device works by establishing a vacuum in the oral cavity, which pulls the uvula and soft palate forward and stabilizes the tongue position. It worked in approximately 40% of patients and the early data suggest that adherence may be effective. The Provent device has been available for several years and is disposable. It is attached to the nares nightly and establishes substantial expiratory resistance. It could successfully treat OSA in about 35%–50% of patients. However, cost, acceptance, and adherence of CPAP, MAD, hypoglossal nerve stimulation device, and Winx and Provent devices may be a problematic.
Some studies of muscle function have shown little difference in fatigability, muscle strength (Mortimore et al., 2000), twitch tension (Sériès et al., 1995), or force-frequency relationships (Carrera et al., 1999) in OSA patients compared with snorers or non-snorers. Also, the degree of dilatation of the upper airway muscles correlates closely with OSAHS. There are over twenty muscles that contribute to the upper airway, among which the genioglossus, levator veli palati muscle, and tensor veli palatini are the most important dilators (White, 2005).
In OSAHS patients, airway dilation appears less coordinated compared with that in healthy subjects. Failure to continuously recruit and coordinate dilator muscles to counterbalance the forces that act to close the airway results in hypopneas or apneas. Repeated failures lead to OSA (Bilston and Gandevia, 2014).
Inspiratory movement of the tongue varies between and within subjects, likely as a result of local and neural factors. However, in severe OSA, inspiratory movement is minimal (Brown et al., 2013). An animal experiment found that a negative pressure reflex activated the tongue or other pharyngeal muscles. Stimulation of tongue protrudor muscles alone or coactivation of protrudor and retractor muscles caused anterior-posterior pharyngeal expansion to be greater than lateral. Stimulation of rodent tongue muscles could adjust pharyngeal shape, which can be applied to the treatment of OSA (Fregosi, 2011).
Philip et al. (2005) reported that chronic increase of tissue volume around the upper airway can lead to pathologic changes of pharyngeal myofibrils and functional disorders of the upper airway dilators, which are the two most important causes of OSAHS. Chen et al. (2005) found that the variation of genioglossus myoelectric activity during sleep apnea had specific features. From prophase to early stage of sleep apnea, the myoelectricity of the genioglossus decreased slowly and resulted in airway obstruction. In the advanced stage of apnea, with the increase in negative airway pressure, oxygen tension reduced and carbon dioxide tension increased. Through the regulation of the central and regional baroreceptors and chemoreceptors, the myoelectrical activity of genioglossus was noted to increase gradually and peaked at the end of this apneic phase. This caused contraction of the genioglossus muscle, pushing forward the tongue and enlarging the retroglossal airway space. The myoelectrical activity of the genioglossus started to diminish after the apneic phase ceased and returned to the pre-apneic phase.
When the dilators of the upper airway were activated, the airway was kept open by the muscle tension. Any weakness of these muscles partially or completely resulted in a reduction of the cross sectional area or a total collapse of the airway (White, 2005).
Most OSAHS patients could breathe normally and maintained normal oxygen saturation in the awake state. This is a consequence of the high myogenic activity of the dilator muscles of the upper airway, which prevents the total collapse of the airways that were already narrow (Mezzanotte et al., 1992). The contractility of the dilator muscles of the upper airway is the key factor in maintaining a patent resilience. Mezzanotte et al. (1996) found that there was a reduction in electrical activity of the genioglossus in OSAHS patients of 50% or more when compared with normal people. Carrera et al. (1999) reported that the fatigue resistance ability of OSAHS patients was lower than that of normal people in an in vitro study. As OSAHS progresses, changes have been noted in the myofibers of the genioglossus, which included irreversible damage and deterioration of muscle function, and decrease in myofibers with an increase of fibrous tissue.
The incidence of adult OSAHS is positively related to increasing age. Aging has a negative effect on the ability to maintain a patent upper airway. Thus, even if surgery removes any potential obstructive factors, OSAHS may recur as the AHI deteriorates over time. Therefore, there would be a possibility to improve OSAHS with physical exercises designed to recover or enhance muscle activity of the upper airway, resulting in potential relief of OSAHS.
As previously mentioned, OSAHS correlates with age, and even after surgical removal of any obstructive factor, the incidence of OSAHS remains stubbornly high with increase in AHI. Physical and functional muscular activity may enhance the dilators of the upper airway and assist in relief of OSAHS. Such physical activity focusing on muscular rehabilitation is already well-recognized and employed in patient management in various orthopedic and neurological disorders. Such functional training is considered to promote metabolism and circulation in order to avoid myotrophy (Carrera et al., 1999).
Therefore, we designed a series of exercises of the pharyngeal musculature and genioglossus as an option in the treatment of OSAHS. The functional muscle training requires a certain period of time to be effective. It can be easily taught and is of minimal cost. All patients should be counseled on the risks of OSAHS and fully investigated before any treatment is undertaken. In general, we recommend that the exercises of the pharyngeal musculature and genioglossus are for patients with moderate OSAHS. Severe OSAHS patients need to be managed with CPAP or surgery, because benefit is obtained only after several months of exercising.
After 6 to 12 months of exercising, all patients in the exercising group had a reduction in their AHI score, improvements in LSaO2, decreases in ESS and questionnaire scores, reflecting the improvement of clinical symptoms. The effective rates were about 70.37% and 74.07%, respectively. The mechanisms employed in exercising the pharyngeal musculature and genioglossus to treat OSAHS might be a combination of promoting circulation, improving muscular tension, and reducing the compliance of the pharynx. After a period of exercising, strength and tension of the genioglossus and pharyngeal musculature were improved. Because of the improvement, the airway patency was maintained, and then clinical symptoms of OSAHS patients improved. The only significant change was found in the compliance of the retropalatal anteroposterior pharyngeal wall, which was consistent with the study of Brown et al. (2013).
It has not been demonstrated how the frequency and duration of the exercises may influence OSAHS, as there were no significant differences in AHI and LSaO2 between 6 and 12 months of exercising. However, the patients’ symptoms alleviated with the extension of duration. This implies that other factors than simply a patent upper airway may result in persistent abnormal findings. Further studied are needed.
We conclude that exercising the pharyngeal musculature and genioglossus is a kind of non-invasive and effective method involving minimal cost to treat some OSAHS patients, especially for the old patients, without surgical conditions, and especially mild and moderate OSAHS patients who do not want surgery or CPAP treatment. Further, exercising the pharynx and genioglossus can be considered as an alternative treatment for OSAHS to surgery and other therapies.
Footnotes
Project supported by the Social Development of Science and Technology Program of Ningbo City (No. 2010C50031) and the Ningbo Natural Science Foundation (No. 2013A610261), China
Compliance with ethics guidelines: Shi-xiong TANG, Jing QING, Yao-wen WANG, Liang CHAI, Wei-min ZHANG, Xian-wang YE, Jie ZHANG, Yi-qin HUANG, and Peng CHENG declare that they have no conflict of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study.
References
- 1.Bilston LE, Gandevia SC. Biomechanical properties of the human upper airway and their effect on its behavior during breathing and in obstructive sleep apnea. J Appl Physiol (1985) 2014;116(3):314–324. doi: 10.1152/japplphysiol.00539.2013. [DOI] [PubMed] [Google Scholar]
- 2.Brown EC, Cheng S, McKenzie DK, et al. Respiratory movement of upper airway tissue in obstructive sleep apnea. Sleep. 2013;36(7):1069–1076. doi: 10.5665/sleep.2812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carrera M, Barbe F, Sauleda J, et al. Patients with obstructive sleep apnea exhibit genioglossus dysfunction that is normalized after treatment with continuous positive airway pressure. Am J Respir Crit Care Med. 1999;159(6):1960–1966. doi: 10.1164/ajrccm.159.6.9809052. [DOI] [PubMed] [Google Scholar]
- 4.Chen LY, Ye JY, Cui JH. The study of genioglossus muscle activity on patients with obstructive sleep apnea hypopnea syndrome. Chin Arch Otolaryngol Head Neck Surg. 2005;12(7):453–457. (in Chinese) [Google Scholar]
- 5.Chouchou F, Pichot V, Barthélémy JC, et al. Cardiac sympathetic modulation in response to apneas/hypopneas through heart rate variability analysis. PLoS ONE. 2014;9(1):e86434. doi: 10.1371/journal.pone.0086434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Editorial Board of Chinese Journal of Otorhinolaryngology Head and Neck Surgery. Guidelines for the diagnosis and surgical treatment of obstructive sleep apnea hypopnea syndrome. Chin J Otorhinolaryngol Head Neck Surg. 2009;44(2):95–96. doi: 10.3760/cma.j.issn.1673-0860.2009.02.003. (in Chinese) [DOI] [PubMed] [Google Scholar]
- 7.Fregosi RF. Influence of tongue muscle contraction and transmural pressure on nasopharyngeal geometry in the rat. J Appl Physiol (1985) 2011;111(3):766–774. doi: 10.1152/japplphysiol.01501.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kirkness JP, Schwartz AR, Schneider H, et al. Contribution of maleXII, age, and obesity to mechanical instability of the upper airway during sleep. J Appl Physiol (1985) 2008;104(6):1618–1624. doi: 10.1152/japplphysiol.00045.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuna ST. Effects of pharyngeal muscle activation on airway size and configuration. Am J Respir Crit Care Med. 2001;164(7):1236–1241. doi: 10.1164/ajrccm.164.7.2011030. [DOI] [PubMed] [Google Scholar]
- 10.Mateika JH, Syed Z. Intermittent hypoxia, respiratory plasticity and sleep apnea in humans: present knowledge and future investigations. Respir Physiol Neurobiol. 2013;188(3):289–300. doi: 10.1016/j.resp.2013.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mezzanotte WS, Tangel DJ, White DP. Waking genioglossal electromyogram in sleep apnea patients versus normal controls (a neuromuscular compensatory mechanism) J Clin Invest. 1992;89(5):1571–1579. doi: 10.1172/JCI115751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mezzanotte WS, Tangel DJ, White DP. Influence of sleep onset on upper-airway muscle activity in apnea patients versus normal controls. Am J Respir Crit Care Med. 1996;153(6):1880–1887. doi: 10.1164/ajrccm.153.6.8665050. [DOI] [PubMed] [Google Scholar]
- 13.Mortimore I, Bennett S, Douglas N. Tongue protrusion strength and fatiguability: relationship to apnoea/hypopnoea index and age. J Sleep Res. 2000;9(4):389–393. doi: 10.1046/j.1365-2869.2000.00222.x. [DOI] [PubMed] [Google Scholar]
- 14.Philip P, Gross CE, Taillard J, et al. An animal model of a spontaneously reversible obstructive sleep apnea syndrome in the monkey. Neurobiol Dis. 2005;20(2):428–431. doi: 10.1016/j.nbd.2005.03.024. [DOI] [PubMed] [Google Scholar]
- 15.Quinnell TG, Bennett M, Jordan J, et al. A crossover randomized controlled trial of oral mandibular advancement devices for obstructive sleep apnoea-hypopnoea (TOMADO) Thorax. 2014;69(10):938–945. doi: 10.1136/thoraxjnl-2014-205464. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz AR, O'Donnell CP, Baron J, et al. The hypotonic upper airway in obstructive sleep apnea: role of structures and neuromuscular activity. Am J Respir Crit Care Med. 1998;157(4):1051–1057. doi: 10.1164/ajrccm.157.4.9706067. [DOI] [PubMed] [Google Scholar]
- 17.Sériès F, Côté C, Simoneau J, et al. Physiologic, metabolic, and muscle fiber type characteristics of musculus uvulae in sleep apnea hypopnea syndrome and in snorers. J Clin Invest. 1995;95(1):20–25. doi: 10.1172/JCI117640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shortt CM, Fredsted A, Bradford A, et al. Diaphragm muscle remodeling in a rat model of chronic intermittent hypoxia. J Histochem Cytochem. 2013;61(7):487–499. doi: 10.1369/0022155413490947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang Q, Zhang C, Jia P, et al. The association between the phenotype of excessive daytime sleepiness and blood pressure in patients with obstructive sleep apnea-hypopnea syndrome. Int J Med Sci. 2014;11(7):713–720. doi: 10.7150/ijms.7487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White DP. Pathogenesis of obstructive and central sleep apnea. Am J Respir Crit Care Med. 2005;172(11):1363–1370. doi: 10.1164/rccm.200412-1631SO. [DOI] [PubMed] [Google Scholar]
- 21.White DP. New therapies for obstructive sleep apnea. Semin Respir Crit Care Med. 2014;35(5):621–628. doi: 10.1055/s-0034-1390074. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Q, Zhang X, Zhao M, et al. Correlation of obstructive sleep apnea hypopnea syndrome with metabolic syndrome in snorers. J Biomed Res. 2014;28(3):222–227. doi: 10.7555/JBR.28.20120120. [DOI] [PMC free article] [PubMed] [Google Scholar]