Abstract
Background
N-Methyl-d-aspartate receptor antagonists reverse hyperalgesia during morphine infusion in male mice only. Because the melanocortin-1 receptor can act as a female-specific counterpart to N-methyl-d-aspartate receptors in κ-opioid analgesic mechanisms, the authors assessed the contribution of melanocortin-1 receptors to the sex-specific mechanisms underlying morphine hyperalgesia.
Methods
The tail-withdrawal test was used to compare the nociceptive responses of male and female C57BL/6J (B6) mice with those of C57BL/6J-Mc1re/e (e/e) mice, spontaneous mutants of the B6 background lacking functional melanocortin-1 receptors, during continuous morphine infusion (1.6 and 40.0 mg kg−1 · 24 h−1). Separate groups of hyperalgesic B6 and outbred CD-1 mice were injected with MK-801 or MSG606, selective N-methyl-d-aspartate and melanocortin-1 receptor antagonists, respectively.
Results
Morphine infusion (40.0 mg · kg−1 · 24 h−1) reduced baseline withdrawal latencies by 45–55% in B6 mice of both sexes, indicating hyperalgesia; this increased nociception was manifest in male e/e mice only. Although MK-801 reversed hyperalgesia in male mice only, increasing latencies by 72%, MSG606 increased latencies by approximately 60% exclusively in females. A lower morphine infusion dose (1.6 mg · kg−1 · 24 h−1) reduced baseline withdrawal latencies by 45–52% in B6 and e/e mice of both sexes, which was reversed by MK-801, but not MSG606, in both male and female B6 mice.
Conclusions
The data indicate the sex-specific mediation of highdose morphine-induced hyperalgesia by N-methyl-d-aspartate and melanocortin-1 receptors in male and female mice, respectively, suggesting a broader relevance of this known sexual dimorphism. The data further indicate that the neural substrates contributing to hyperalgesia are morphine dose-dependent.
Sustained morphine delivery can paradoxically enhance pain sensitivity in humans1,2 and nociceptive behavior in rodents.3,4 This opioid-induced hyperalgesia is obviously a major challenge to the clinical treatment of pain, for which μ-opioid agonists such as morphine are a mainstay. Interestingly, morphine enhances nociception in mice even when opioid receptors are effectively blocked by concurrent treatment with high doses of the broad-spectrum opioid receptor antagonist, naltrexone,5,6 or absent entirely in mice lacking all three opioid receptor genes,7 indicating that morphine hyperalgesia is independent of previous or concurrent opioid receptor activation.
We have recently reported a qualitative sex difference in morphine hyperalgesia.6 Specifically, male and female mice manifest hyperalgesia of equal magnitude and duration during 12 days of continuous morphine (40.0 mg · kg−1 · 24 h−1) infusion, but blockade of N-methyl-d-aspartate (NMDA) receptors with LY235959 or MK-801 markedly reversed hyperalgesia in male mice only. This sex-specific response does not seem to be related to any putative sex-dependent potentiation of morphine analgesia by NMDA receptor antagonists8,9 because mice were concurrently treated with naltrexone during morphine infusion. This sex difference was not attributable to antagonist dosing as well because MK-801 did reverse hyperalgesia in males and ovariectomized females but not in ovariectomized females treated with estrogen. These data collectively indicate that female mice possess functional male-typical NMDA receptor-mediated hyperalgesic mechanisms, but they are diverted from their use by ovarian sex steroids. But what neurochemical system mediates morphine hyperalgesia in intact female mice?
There are previous reports that NMDA receptor antagonists effectively reduce κ-opioid analgesia10,11 and nonopioid swim stress-induced analgesia12 in male but not in female mice. In the latter study, MK-801 was an effective antagonist in ovariectomized females but not in ovariectomized females treated with estrogen, which parallels exactly our findings with morphine hyperalgesia. By using genetic and pharmacological tools, Mogil et al.11 subsequently demonstrated the critical contribution of melanocortin-1 receptors to the sex-specific mediation of κ-opioid analgesic mechanisms in intact female mice. Accordingly, we assessed the contribution of this receptor to sex differences in morphine hyperalgesia using MSG606, a selective melanocortin-1 receptor antagonist, and by assaying nociception during morphine infusion in melanocortin-1 receptor-deficient C57BL/6J-Mc1re/e (e/e) mice. The sensitivity of these mutants was compared with that of their genetic background, C57BL/6J (B6) mice.
Materials and Methods
Subjects
All procedures were approved by the College of Staten Island/City University of New York Institutional Animal Care and Use Committee and conform to guidelines of the International Association for the Study of Pain. Naïve, adult CD-1 and B6 (both obtained from Charles River Labs, Kingston, NY) and mutant e/e mice originally obtained from Roger D. Cone, Ph.D. (Professor, Vollum Institute, Oregon Health and Science University, Portland, Oregon) were maintained on a 12:12-h light– dark cycle in a climate-controlled room with free access to food and tap water. The e/e mice possess a spontaneously occurring frameshift mutation in the second extracellular loop of the murine melanocortin-1 receptor gene, and thus they are effectively null mutants having completely nonfunctional melanocortin-1 receptors.13 Each mouse was used only once, and for all groups, n = 8–10. All surgical procedures were performed under sterile conditions and during oxygen/isoflurane anesthesia.
Nociceptive Assay
A modified version of the tail-withdrawal test14 was chosen for its stability in the context of repeated testing for more than 2 weeks.5–7,15,16 In this assay, the distal portion of the tail is immersed in water thermostatically maintained at 47.3° ± 0.2°C using an immersion circulator pump (Isotemp Model 71; Fisher, Pittsburgh, PA). In previous studies with females and males,5,6 this temperature consistently yielded premorphine baseline latencies of 8–10 s, thereby minimizing possible floor effects during the hyperalgesia phase of morphine infusion. Latency to respond with a vigorous flexion of the tail was recorded twice at 30-s intervals and averaged. A cutoff latency of 18 s (i.e., roughly twice the baseline) for analgesic responses was used throughout. Nociception was always tested near mid-photophase to reduce possible circadian effects on nociception.10
Drug Doses and Delivery
Osmotic pumps (Alzet Model 2001; Alza, Mountain View, CA) containing morphine or saline vehicle were implanted subcutaneously via a small dorsal midline incision made during anesthesia. Osmotic pumps provide continuous infusion for 7 days, thereby preventing hyperalgesia associated with withdrawal in morphine-dependent subjects that can potentially confound experiments in which chronic morphine treatment is accomplished via repeated acute injections.17 When testing exceeded 7 days, pumps were replaced on Day 6 as in previous studies.5,6 Pellets containing 30 mg of the general opioid receptor antagonist, naltrexone, or a placebo formulation were wrapped in nylon mesh and implanted subcutaneously in the nape of the neck. Pellets were implanted 24 h before the start of morphine infusion. In rats, identical naltrexone pellets substantially increase naltrexone plasma levels 1 h after implant and sustain pharmacologically active levels of naltrexone such that there is a greater than 50-fold rightward shift in the morphine analgesia dose–response curve 8 days later.18 In mice, these pellets completely abolished the analgesic effect of an acute 10-mg/kg morphine injection starting 24 h after implant, coinciding with the start of morphine infusion, and for a minimum of 7 days thereafter.5 Accordingly, we restricted our testing of naltrexone-pelleted mice to the first seven morphine infusion days. Both morphine and pellets containing naltrexone or a placebo formulation were generously provided by NIDA Drug Supply Program (Bethesda, MD). Acute bolus doses of the noncompetitive NMDA receptor antagonist, MK-801, (Sigma-Aldrich, St. Louis, MO) and selective melanocortin-1 receptor antagonist, MSG606, were dissolved in 0.9% physiologic saline and a saline, 10% dimethyl sulfoxide vehicle, respectively. MSG606 (Cyclo-[(CH2)3CO-Gly-His-D-Phe-Arg-D-Trp-Cys(S-)]-Asp-Arg-Phe-Gly-NH2), a potent and novel cyclic thioether peptide, was synthesized in the laboratory of Victor J. Hruby, Ph.D. (Regents Professor, Department of Chemistry, University of Arizona, Tucson, Arizona) as follows. Rink amide resin (100 mg, 0.065 mmol/g; Polymer Laboratories [Amherst, MA]) was placed into a 5-ml polypropylene syringe with the frit on the bottom and swollen in dichloromethane (2 ml) for 30 min and in N,N-dimethylformamide (DMF; 2 ml) for 30 min. The 9H-(f)luoren-9-yl(m)eth(o)xy(c)arbonyl protecting group on the Rink linker was removed by 50% piperidine in DMF. After 20 min, the solution of piperidine was removed, and the resin was washed with DMF (2 ml, 10 times). 9H-(f)luoren-9-yl(m)eth(o)xy(c)arbonyl amino acid (3 equivalents, 0.195 mmol) and 1-hydroxybenzotriazole (3 equivalents, 0.195 mmol) were dissolved in 700 µl of DMF, and then, 1,3-diisopropylcarbodiimide (3 equivalents, 0.195 mmol) was added. The coupling mixture was sucked into the syringe with the resin and shaken for 1–3 h. The coupling completion was monitored with bromophenol blue and ninhydrin tests. The coupling mixture was removed, and the resin was washed with DMF (2 ml, 5 times). The N2 9H-(f)luoren-9-yl(m)eth(o)xy(c)arbonyl group was cleaved with 50% piperidine in DMF. Each coupling and deprotection step was repeated until a linear peptide was assembled. Bromoacetic acid (3 equivalents, 0.195 mmol) was dissolved in 700 µl of DMF and 1,3-diisopropylcarbodiimide (3 equivalents, 0.195 mmol) was added. The acylation reaction was usually complete after 20 min. The reaction mixture was removed, and the resin was washed with DMF (2 ml, 5 times) and dichloromethane (2 ml, 5 times). The monomethoxytrityl group was cleaved by treatment with 2% trifluoroacetic acid/ 5% triisopropylsilane/dichloromethane (2 ml, 5 times, 5 min each treatment). The resin was washed with dichloromethane (2 ml, 10 times) and DMF (2 ml, 5 times). Peptide cyclization was performed in a solution of 5% N,N-diisopropylethylamine in DMF during 10–12 h at room temperature. The final wash of the resin was done with DMF (2 ml, 5 times) and dichloromethane (2 ml, 5 times). The product was cleaved from the resin with a mixture of 95% trifluoroacetic acid, 2.5% triisopropylsilane, and 2.5% water in 1.5 h. Side chain-protecting groups were removed during the cleavage step as well. The cleavage mixture was evaporated on a rotary evaporator. The crude cyclic peptide was dissolved in acetic acid and purified using high-pressure liquid chromatography. The resulting peptide was tested for binding affinities (IC50: concentration at which 50% of the competing ligand [125I-NDP-α-MSH] is displaced) and cyclic adenosine monophosphate production (EC50: concentration of ligand at which 50% of maximum cyclic adenosine monophosphate production is obtained using HEK 293 cell stabling transfected with human melanocortin [hMC] receptor types hMC1, hMC3, hMC4, or hMC5) using a range of concentrations (10−10–10−5 m) and displayed a 70-fold or greater affinity for the melanocortin-1 receptor subtype relative to other melanocortin receptor types (hMC1— IC50: 17 nm, EC50: no cAMP produced at 10−5 m; hMC3—IC50: 3900 nm, EC50: 103 nm; hMC4—IC50: no binding at 10−5 m, EC50: NA; hMC5—IC50: 1300 nm, EC50: 1300 nm). MK-801 (0.05 mg/kg) was injected subcutaneously in a volume of 10 ml/kg, and MSG606 (7.5 µg) was injected into the lateral ventricles in a 5-µl volume according to the method of Haley and McCormick.19 As adapted here, a small midline incision was made in the scalp of mice during oxygen/isoflurane inhalant anesthesia, and lambda was located. Drug was then injected directly through the skull at a point 2 mm rostral and lateral to lambda at a depth of 3 mm using a 10-ml Hamilton microsyringe fitted with a 27-gauge needle. A stainless steel wound clip was then used to close the incision. Motor function (i.e., “step test” and performance on a 90° inclined grid) and righting reflexes were assayed in small (n = 6) separate groups of morphine-infused male and female CD-1 mice injected with MSG606 at postinjection intervals corresponding to the maximal effect of this drug on nociception. The dose of MK-801 used has already been reported to have no effect on motoric functioning5,6,9 and was thus not assayed.
Data Analysis
Tail-withdrawal latencies in all experiments were analyzed using two-way repeated-measures analysis of variances (Systat v.11; SPSS Inc., Chicago, IL), with sex and drug (agonist or antagonist, as appropriate) as between-subject factors and morphine infusion day or postinjection time as the repeated measure. When appropriate, repeated measures were then run separately on each sex/drug combination, followed by a post hoc test for repeated measures (two tailed) using Bonferroni correction for multiple comparisons. For all analyses, α = 0.05.
Results
Nociception during Morphine Infusion in B6 and e/e Mice
Hyperalgesia during continuous morphine infusion has only been previously reported in CD-1 mice.5,6 To facilitate comparisons with e/e mice, we also tested B6 mice, the genetic background of the mutant. To control for possible uneven analgesia between males and females during morphine infusion that could confound their comparison, both placebo-and naltrexone-pelleted mice were tested.
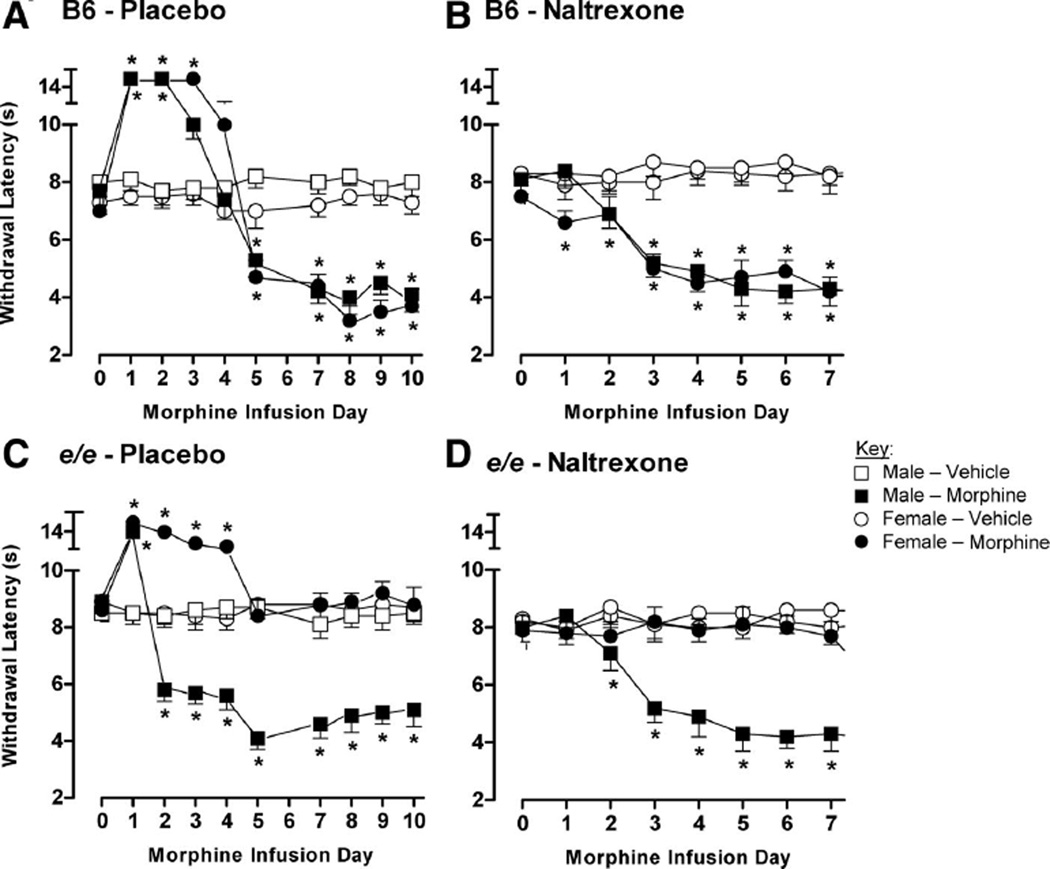
Infusing a cumulative daily morphine dose of 40.0 mg/kg in placebo-pelleted male and female B6 mice increased withdrawal latencies relative to premorphine infusion baseline values (Day 0) for 3 and 4 days, respectively (fig. 1A; sex × drug × repeated measure: F9,243 = 9.5, P < 0.001; repeated measures in male/morphine and female/morphine groups, both P < 0.001). This analgesia dissipated as latencies in both sexes were significantly reduced as morphine infusion continued, with significant hyperalgesia (i.e., reductions from Day 0) evident on days 5–10 in both sexes. The magnitude of hyperalgesia between sexes on days 5–10 was largely similar. However, when testing male and female B6 mice implanted with naltrexone pellets before the start of morphine infusion, there was no initial analgesic response (fig. 1B). Although transient hyperalgesia was evident in females on infusion Day 1, persistent hyperalgesia was evident in both sexes starting from Day 3 (sex × drug × repeated measure: F7,196 = 5.5, P < 0.001; repeated measures in male/morphine and female/morphine groups, both P < 0.001). As observed for placebo-pelleted mice, there was no significant sex difference in hyperalgesic magnitude, and latency values were highly similar throughout the testing time course.
Fig. 1.
Hyperalgesia in B6 and e/e mice during continuous morphine infusion. Male and female B6 (A, B) and e/e (C, D) mice were implanted with placebo (A, C) or naltrexone (B, D) pellets and assayed for nociception on the tail-withdrawal test 24 h later (Day 0). Mice were then immediately implanted with osmotic pumps providing continuous infusion of a cumulative daily morphine dose of 40.0 mg/kg or vehicle. Nociception was reassessed daily on the subsequent infusion days. Symbols are mean ± SEM withdrawal latencies, with n = 8–10 mice in every group. *Indicates significant difference (in either direction) relative to own baseline (Day 0) latency (Bonferroni corrected P < 0.05).
In placebo-pelleted e/e male mice (fig. 1C), the identical morphine treatment protocol first significantly increased then, starting from Day 2, caused a persistent decrease in withdrawal latencies relative to premorphine infusion baseline values (Day 0) (sex × drug × repeated measure: F9,279 = 53.2, P < 0.001; repeated measures in male/morphine and female/morphine groups, both P < 0.001). This pattern of significant short-lived analgesia followed by several days of unremitting hyperalgesia was not observed in female e/e mice, which displayed significant analgesia of 4 days duration followed by a return to premorphine infusion baseline values as infusion continued on days 5–10. Again, naltrexone abolished analgesia in both sexes (fig. 1D). Although the withdrawal latencies of male mice were significantly reduced starting from Day 1, there were no significant alterations in the latencies of female mice during morphine infusion (fig. 1D; sex × drug × repeated measure: F7,203 = 37.3, P < 0.001; repeated measures in male/morphine group only significant at P < 0.001). Vehicle infusion in placebo- or naltrexone-pelleted mice had no effect on tail-withdrawal latencies in males or females of either strain (all repeated measures P > 0.05).
Effect of MK-801 and MSG606 on Morphine Hyperalgesia
NMDA and melanocortin-1 receptors can sex-dependently modulate the analgesic effect of opioids,8,9,11 which could confound the between-sex comparison of concurrent hyperalgesia during morphine infusion. Thus, the ability of MK-801 and MSG606 to reverse morphine hyperalgesia was assayed in naltrexone-pelleted male and female mice.
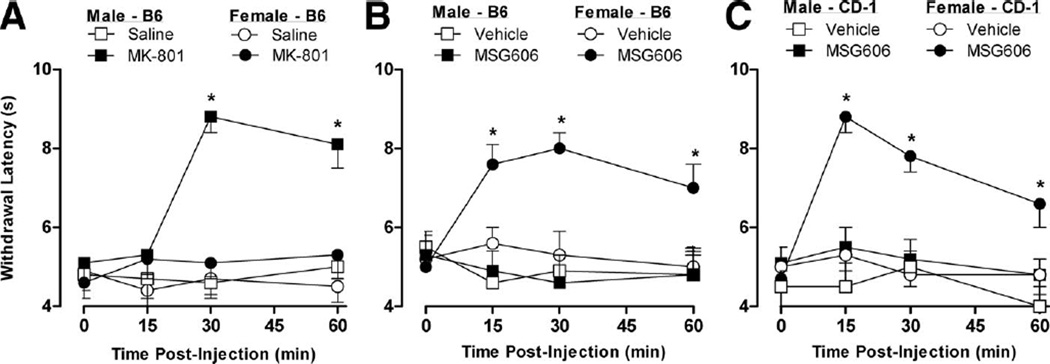
Baseline latencies were obtained on Day 0 in male (9.7 ± 0.4) and female (9.4 ± 0.5) B6 mice, which were then subject to cumulative daily morphine infusion doses of 40.0 mg/kg. Consistent with data shown in figure 1, withdrawal latencies were significantly reduced by approximately 4 s on infusion Day 5 (time 0, fig. 2A). Mice of each sex were then randomly assigned to groups injected with MK-801, MSG606, or their corresponding vehicles. Although MK-801 injection increased withdrawal latencies (back to baseline levels) relative to immediate preantagonist injection (i.e., time 0) values 30–60 min later in male B6 mice, the latencies of females remained unchanged throughout the testing period (fig. 2A; sex × drug × repeated measure: F3,90 = 42.8, P < 0.001; repeated measures in male/MK-801 group alone significant at P < 0.001). These data are in complete contrast with latencies obtained after MSG606 injection, which were significantly increased within 15 min in female B6 mice—and remained increased for the entire 60-min testing period—but not in males (fig. 2B; sex × drug × repeated measure: F3,90 = 19.8, P < 0.001; repeated measures in female/MK-801 group alone significant at P < 0.001). Vehicle injections did not alter withdrawal latencies in mice of either sex.
Fig. 2.
Effect of the N-methyl-d-aspartate receptor antagonist, MK-801, and the melanocortin-1 receptor antagonist, MSG606, on morphine hyperalgesia in male and female mice. Naltrexone-pelleted B6 and CD-1 mice of both sexes were assayed for nociception on the tail-withdrawal test on Day 0 and began receiving continuous morphine infusion at cumulative daily doses of 40.0 mg/kg. Withdrawal latencies were again obtained on infusion Day 5 and, consistent with the earlier data, confirmed that the mice were hyperalgesic. Mice were then immediately injected with MK-801 (A), MSG606 (B, C), or their corresponding vehicle and retested for the next 60 min. Symbols are mean ± SEM withdrawal latencies obtained immediately before (time 0) and after injection using 8–10 mice in every group. *Indicates significant increase in latency relative to own baseline (time 0) value (Bonferroni corrected P < 0.05).
To determine whether these findings with MSG606 in inbred B6 mice are relevant to the sex-specific mediation of morphine hyperalgesia initially described in outbred CD-1 mice,6 we also obtained baseline withdrawal latencies in CD-1 mice (males: 9.7 ± 0.3; females: 9.6 ± 0.3) and subjected them to cumulative daily morphine infusion doses of 40.0 mg/kg. Consistent with previous studies using this strain,5,6 latencies were significantly reduced on infusion Day 5 (time 0, fig. 2C). Subjects of each sex were then randomly divided into two groups and immediately injected with MSG606 or vehicle. As with B6 mice, only the latencies of female CD-1 mice increased between 15 and 60 min after MSG606 injection (fig. 2C; sex × drug × repeated measure: F3,87 = 29.9, P < 0.001; repeated measures in female/MK-801 group alone significant at P < 0.001). Vehicle injections were again without effect at any testing interval. Furthermore, MSG606 injection had no effect on the motoric functioning of male or female morphine-infused CD-1 mice 15 min later (data not shown).
NMDA Receptors but not Melanocortin-1 Receptors Mediate Hyperalgesia Evoked by a Low Morphine Infusion Dose in Both Sexes
Morphine can activate distinct dose-dependent hyperalgesic systems,5,6,20 and our previous data indicate that a cumulative daily morphine infusion dose of 1.6 mg/kg evokes hyperalgesia that, in contrast to the 40.0 mg · kg−1 · 24 h−1 infusion dose tested in the above studies, is mediated by NMDA receptors in both male and female CD-1 mice.6 We studied whether this finding can be generalized to B6 mice and whether there is any contribution of melanocortin-1 receptors to hyperalgesia during infusion of this lower morphine dose.
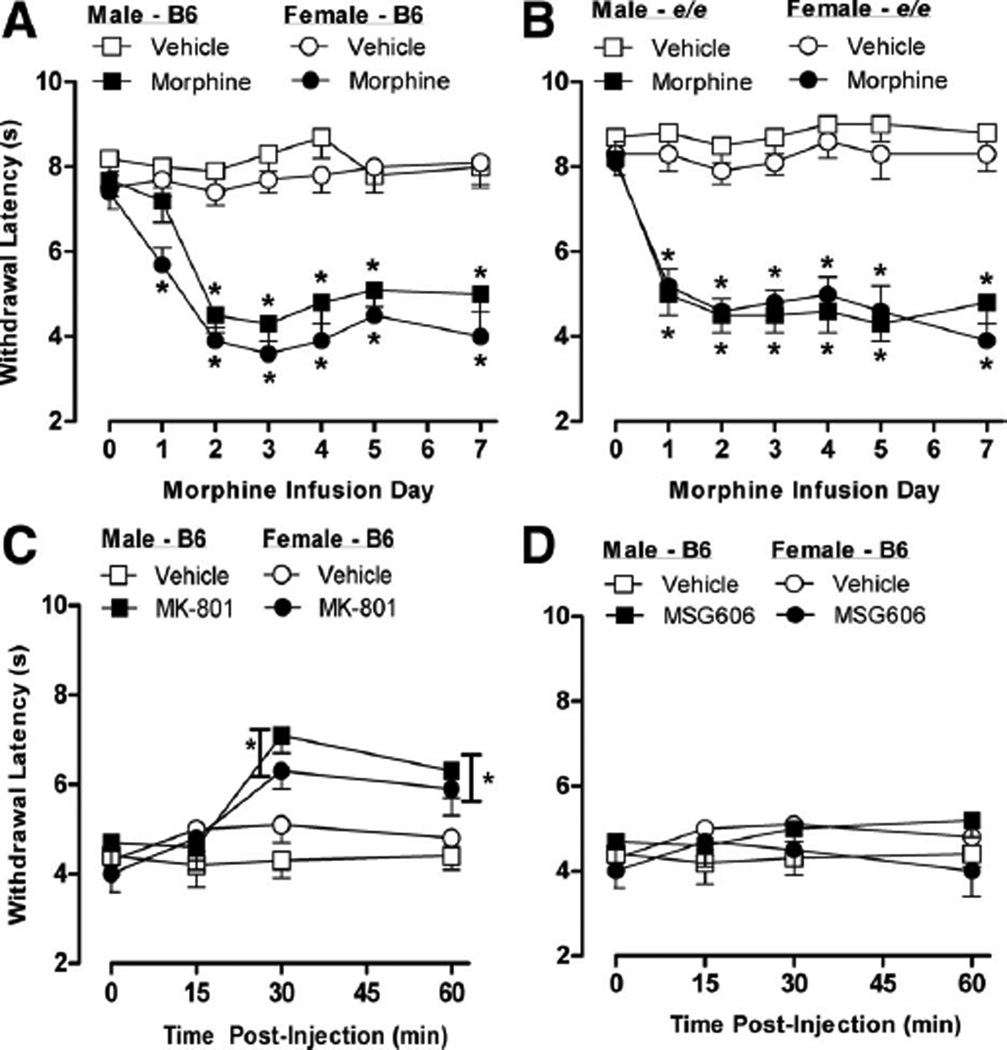
Naltrexone-pelleted B6 and e/e mice of both sexes were implanted with pumps infusing a cumulative daily morphine dose of 1.6 mg/kg. As illustrated in figure 3A and B, significant latency reductions indicative of hyperalgesia were evident on almost all of the seven morphine infusion days in both sexes and strains, including e/e female mice lacking functional melanocortin-1 receptors (sex × drug × repeated measures interactions significant in both strains at P < 0.05; repeated measures in all morphine-treated groups significant at P < 0.001). The contribution of NMDA receptors to hyperalgesia at this lower morphine infusion dose was assayed in a separate group of naltrexone-pelleted B6 male and female mice. When the baseline values of these male (8.9 ± 0.4) and female mice (8.5 ± 0.5) were significantly reduced on Day 5 (time 0, fig. 3C), confirming their hyperalgesia, they were randomly assigned to two groups and each immediately injected with MK-801 or vehicle. Relative to preantagonist injection (time 0) values, MK-801 injection increased the latencies of B6 male and female mice from 30 to 60 min (fig. 3C). In this data set, the main effect of sex and the sex × drug × repeated measures interaction was not significant; all other factors and interactions were significant at P < 0.001. Thus, a repeated-measures analysis of variance was performed on male and female data combined (fig. 3C). In contrast, vehicle injections did not reverse hyperalgesia in either sex. The contribution of menaocortin-1 receptors to hyperalgesia at this lower morphine infusion dose was also assayed this way using a separate group of naltrexone-pelleted B6 mice. When the baseline values of B6 male (8.6 ± 0.5) and female (8.8 ± 0.4) mice were significantly reduced on Day 5 (time 0, fig. 3D), confirming their hyperalgesia, they were randomly assigned to two groups and each immediately injected with MSG606 or vehicle. Neither MSG606 nor vehicle altered the latencies of either B6 male or female mice relative to preantagonist injection (time 0) values during the 60-min testing period (fig. 3D; all main effects and interactions P > 0.05).
Fig. 3.
N-methyl-d-aspartate receptors mediate hyperalgesia during infusion of a low morphine dose. B6 (A) and e/e mice (B) of both sexes were implanted with naltrexone pellets and 24 h later (Day 0) assayed for nociception on the tail-withdrawal test. Mice were then immediately implanted with osmotic pumps providing continuous infusion of a cumulative daily morphine dose of 1.6 mg/kg or vehicle. Nociception was retested daily on subsequent infusion days. Separate groups of naltrexone-pelleted male and female B6 mice were assayed for nociception on Day 0 and began receiving continuous morphine infusion at cumulative daily doses of 1.6 mg/kg. Consistent with the earlier data, withdrawal latencies obtained on infusion Day 5 confirmed that the mice were hyperalgesic. Mice were then immediately injected with MK-801 (C) or MSG606 (D) or their corresponding vehicles and retested for the next 60 min. Symbols are mean ± SEM withdrawal latencies, with n = 8–10 mice in every group. *Indicates significant difference in tail-withdrawal latencies relative to own baseline (Day 0) value (Bonferroni corrected P < 0.05). In (C), asterisk refers to data from both sexes combined (MK-801 compared with vehicle), because no significant sex × drug × repeated measures interaction was obtained.
Discussion
NMDA receptors are widely recognized as contributing to opioid hyperalgesia.3,4,20 However, we previously reported that hyperalgesia during morphine infusion at a daily cumulative dose of 40.0 mg/kg is reversed by the NMDA receptor antagonist, MK-801, in male but not in female CD-1 mice.6 We confirm and extend this finding by reporting the identical sex-dependent reversal of morphine hyperalgesia by MK-801 in B6 mice, indicating that the sex-dependent mediation of morphine hyperalgesia by NMDA receptors is not artifactual or obviously strain dependent. Although NMDA receptor antagonists can potentiate morphine analgesia in a sex-dependent manner,8,9 the current demonstration of a sex-dependent reversal of hyperalgesia by MK-801 in naltrexone-pelleted B6 mice discounts this possibility and is consistent with findings obtained in naltrexone-pelleted CD-1 mice.6 More relevant to the current study, the manifestation of hyperalgesia during morphine infusion in both placebo- and naltrexone-pelleted male B6 mice contrasts with the nociceptive sensitivity of identically treated female e/e mice, whose nociceptive sensitivity never increased relative to baseline. Because B6 and e/e mice are genetically identical except for an inactivating frameshift mutation in the second extracellular loop of the melanocortin-1 receptor gene in the e/e mice, the data indicate that melanocortin-1 receptors make a critical contribution to morphine hyperalgesia in female mice only. The manifestation of morphine hyperalgesia in male e/e mice indicate that, like B6 males, their hyperalgesia is not mediated by melanocortin-1 receptors. These conclusions are fully supported by the data obtained here in hyperalgesic male and female male B6 mice injected with the melanocortin-1 receptor antagonist, MSG606. Although an acute MSG606 bolus injection reversed hyperalgesia in females, it was without any effect in males. Identical results were obtained in CD-1 mice. We conclude that NMDA and melanocortin-1 receptors contribute to morphine hyperalgesia in male and female B6 mice, respectively, and that this sex-dependent mediation of morphine hyperalgesia underlies the qualitative sex difference in hyperalgesia during morphine infusion initially described in CD-1 mice as well.6
We previously reported that MK-801 is not effective in reversing hyperalgesia in intact CD-1 female mice during infusion of a daily cumulative morphine dose of 40.0 mg/kg.6 In that study, however, MK-801 was effective when females were subject to morphine infusion after ovariectomy but not when ovariectomy was followed by estrogen treatment before the start of morphine infusion. Therefore, we concluded that female mice possess the male-typical NMDA receptor-mediated hyperalgesic circuitry, but that they are precluded from its use by ovarian hormones. We report that MSG606 reverses hyperalgesia in intact female CD-1 mice subject to the identical morphine infusion protocol used in that study. Collectively, these data indicate that both NMDA and meanocortin-1 receptors contribute to morphine hyperalgesia in intact female CD-1 mice, but they are restricted to doing so in a mutually exclusive manner under the regulation of ovarian hormones.
We are impressed by the striking parallel between our findings and those of Mogil et al.,11 who showed that κ-opioid analgesia is mediated by NMDA receptors in males and by melanocortin-1 receptors in females. The relevant NMDA and melanocortin-1 receptors are likely (although not proven to be) in the midbrain periaqueductal gray matter21,22; we have also confirmed using quantitative real-time polymerase chain reaction a sex-dependent (females > males) expression of the mouse Mc1r gene in this region (J-S Austin, B.Sc., Research Associate, Department of Psychology, McGill University, Montreal, Quebec, Canada, and JS Mogil, unpublished data, August 2009). We believe that this very unusual pattern of sex-dependent neurochemistry, which to our knowledge has only been described for κ-opioid analgesia and morphine hyperalgesia, is not simply coincidental but instead represents the activity of a single neuronal organization, which acts to modulate nociception. It is not currently known to which other nociceptive testing and/or opioid delivery conditions, if any, these sex-dependent systems may contribute. However, in addition to their demonstration in mice, Mogil et al.11 also demonstrated the female-dependent melanocortin-1 receptor mediation of κ-opioid analgesia in individuals with variants of the human MC1R gene. Accordingly, the current data predict that women with inactivating variants of the melanocortin-1 receptor—that is, redheaded women—would likely be refractory to morphine hyperalgesia. This is an intriguing possibility worthy of study.
Although this study demonstrates that melanocortin-1 receptors contribute to hyperalgesia evoked by the continuous infusion of a cumulative daily morphine dose of 40.0 mg/kg, similar findings were not obtained when mice were tested for nociception when infused with accumulative daily morphine dose of 1.6 mg/kg. Specifically, both male and female e/e mice manifest hyperalgesia largely identical to that observed in male and female B6 mice. Furthermore, although MK-801 was effective in reversing hyperalgesia in both sexes during infusion of this lower morphine dose, MSG606 was not. Collectively, these data are consistent with our previous findings that only NMDA receptors mediate hyperalgesia during this lower morphine infusion dose in CD-1 mice of both sexes.6 The demonstration in B6 mice indicates that our previous findings are not restricted to CD-1 mice. That there is a qualitative sex difference in the mediation of hyperalgesia during infusion of the larger 40.0 mg/kg but not the lower 1.6 mg/kg infusion dose is consistent with our previous findings that these two doses activate distinct neural substrates to cause hyperalgesia. For example, the lower infusion dose causes an estrogen-mediated sex difference in the duration of morphine hyperalgesia not observed in mice infused with the larger morphine dose.6 In male mice, the onset of hyperalgesia caused by infusion of the lower dose actually precedes that of the 25-fold higher dose by several infusion days.5 This difference cannot be attributed to putative differences in concurrent analgesia during the initial infusion days because this onset difference was also observed in naltrexone-pelleted mice. Finally, only the hyperalgesia manifested during infusion of the lower morphine dose displays cross-adaptation with the pronociceptive nonopioid morphine metabolite morphine-3-β-glucuronide (M3G).5 The physiologic basis by which these morphine infusion doses activate distinct hyperalgesic mechanisms is not known. Whether they are related to any of the diverse hyperalgesic mechanisms already described elsewhere3,4,20 remains to be determined.
Hyperalgesia has been previously demonstrated during continuous morphine infusion in naltrexone-pelleted male and female CD-1 mice5,6 and in opioid receptor triple knockout mice devoid of μ-, δ-, and κ-opioid receptors.7 The ability of morphine infusion to induce hyperalgesia despite opioid receptor blockade is replicated and extended to include B6 and e/e mice of both sexes. The efficacy of naltrexone pellets to cause prolonged blockade of opioid receptors and morphine analgesia has been previously established5,18 and, as evidence of their effectiveness here, they abolished the analgesia expressed during the first few days of 40.0 mg/kg morphine infusion under placebo pellet conditions in male and female B6 and e/e mice. These findings support previous conclusions that morphine can activate mechanisms facilitating pain completely independently of those inhibiting pain or opioid receptor activity.5–7,23–25 Although the mechanisms by which morphine causes hyperalgesia independently of opioid receptor activity are not yet known, we have previously speculated on the possible contribution of M3G. M3G has no detectable opioid receptor affinity,26,27 is pronociceptive in rats and mice,5,28 and is believed to underlie hyperalgesia in humans during chronic morphine treatment.1,2 However, there are inconsistencies. In this study in B6 mice, and in a previous study of CD-1 mice,6 for example, the NMDA receptor antagonist MK-801 did not reverse hyperalgesia in females infused with the 40.0 mg/kg morphine infusion dose, although NMDA antagonists are also functional M3G antagonists.29 We tested larger antagonist doses in pilot studies but, consistent with previous reports,9,12 these caused adverse side effects that precluded their use. Nevertheless, this lack of MK-801 efficacy is evidently not dose related because the MK-801 dose used in both studies was sufficiently large to markedly reverse hyperalgesia in males and ovariectomized females.6 A similar line of questioning is related to the current demonstration that melanocortin-1 receptors contribute to morphine hyperalgesia in female mice. Specifically, there is no current data indicating that M3G (or any other morphine metabolite) can directly activate melanocortin-1 receptors. Thus, the basis by which this receptor contributes to morphine hyperalgesia that is independent of opioid receptor activity is unknown. However, in the absence of a direct interaction between M3G and melanocortin-1 receptors, we speculate that M3G activates pronociceptive circuitry that includes melanocortin-1 receptors downstream. This is similar to the proposed contribution of NMDA receptors to the current model of nonopioid morphine hyperalgesia where, as noted earlier, NMDA receptors are not directly activated by M3G, but NMDA antagonists are functional M3G antagonists.29 We are currently performing studies to more cogently characterize the contribution of M3G as well as NMDA and melanocortin-1 receptors to nonopioid morphine hyperalgesia.
What We Already Know about This Topic
-
❖
Continued opioid exposure leads to hyperalgesia, an effect which is blocked only in male rodents by N-methyl-d-aspartate (NMDA) receptor antagonists
What This Article Tells Us That Is New
-
❖
High dose opioid exposure induced hyperalgesia was blocked only in male mice by NMDA receptor antagonists, and only in female mice by melanocortin-1 receptor antagonists
-
❖
Hyperalgesia from low doses was blocked in both sexes by NMDA receptor antagonists
Acknowledgments
Supported by Professional Staff Congress/City University of New York (New York, New York; to B.K.); National Institute for Neurological Diseases and Stroke R01 NS41670 (Bethesda, Maryland; to J.S.M.); National Institute for Digestive and Kidney Diseases 17240 (Bethesda, Maryland; to V.J.H.); and National Institute on Drug Abuse 06248 and 348900 (Bethesda, Maryland; to V.J.H.).
References
- 1.De Conno F, Caraceni A, Martini C, Spoldi E, Salvetti M, Ventafridda V. Hyperalgesia and myoclonus with intrathecal infusion of high-dose morphine. Pain. 1991;47:337–339. doi: 10.1016/0304-3959(91)90225-M. [DOI] [PubMed] [Google Scholar]
- 2.Sjogren P, Thunedborg LP, Christrup L, Hansen SH, Franks J. Is development of hyperalgesia, allodynia and myoclonus related to morphine metabolism during long-term administration? Six case histories. Acta Anaesthesiol Scand. 1998;42:1070–1075. doi: 10.1111/j.1399-6576.1998.tb05378.x. [DOI] [PubMed] [Google Scholar]
- 3.Simonnet G, Rivat C. Opioid-induced hyperalgesia: Abnormal or normal pain? Neuroreport. 2003;14:1–7. doi: 10.1097/00001756-200301200-00001. [DOI] [PubMed] [Google Scholar]
- 4.Ossipov MH, Lai J, King T, Vanderah TW, Malan TP, Jr, Hruby VJ, Porreca F. Antinociceptive and nociceptive actions of opioids. J Neurobiol. 2004;61:126–148. doi: 10.1002/neu.20091. [DOI] [PubMed] [Google Scholar]
- 5.Juni A, Klein G, Kest B. Morphine hyperalgesia in mice is unrelated to opioid activity, analgesia, or tolerance: Evidence for multiple diverse hyperalgesic systems. Brain Res. 2006;1070:35–44. doi: 10.1016/j.brainres.2005.11.054. [DOI] [PubMed] [Google Scholar]
- 6.Juni A, Klein G, Kowalczyk B, Ragnauth A, Kest B. Sex differences in hyperalgesia during morphine infusion: Effect of gonadectomy and estrogen treatment. Neuropharmacol. 2008;54:1264–1270. doi: 10.1016/j.neuropharm.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Juni A, Klein G, Pintar JE, Kest B. Nociception increases during opioid infusion in opioid receptor triple knock-out mice. Neuroscience. 2007;147:439–444. doi: 10.1016/j.neuroscience.2007.04.030. [DOI] [PubMed] [Google Scholar]
- 8.Kozela E, Danysz W, Popik P. Uncompetitive NMDA receptor antagonists potentiate morphine antinociception recorded from the tail but not from the hind paw in rats. Eur J Pharmacol. 2001;423:17–26. doi: 10.1016/s0014-2999(01)01084-6. [DOI] [PubMed] [Google Scholar]
- 9.Nemmani KV, Grisel JE, Stowe JR, Smith-Carliss R, Mogil JS. Modulation of morphine analgesia by site-specific N-methyl-D-aspartate receptor antagonists: Dependence on sex, site of antagonism, morphine dose, and time. Pain. 2004;109:274–283. doi: 10.1016/j.pain.2004.01.035. [DOI] [PubMed] [Google Scholar]
- 10.Kavaliers M, Choleris E. Sex differences in N-methyl-D-aspartate involvement in kappa opioid and non-opioid predator-induced analgesia in mice. Brain Res. 1997;768:30–36. doi: 10.1016/s0006-8993(97)00569-6. [DOI] [PubMed] [Google Scholar]
- 11.Mogil JS, Wilson SG, Chesler EJ, Rankin AL, Nemmani KV, Lariviere WR, Groce MK, Wallace MR, Kaplan L, Staud R, Ness TJ, Glover TL, Stankova M, Mayorov A, Hruby VJ, Grisel JE, Fillingim RB. The melanocortin-1 receptor gene mediates female-specific mechanisms of analgesia in mice and humans. Proc Natl Acad Sci USA. 2003;100:4867–4872. doi: 10.1073/pnas.0730053100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mogil JS, Sternberg WF, Kest B, Marek P, Liebeskind JC. Sex differences in the antagonism of swim stress-induced analgesia: Effects of gonadectomy and estrogen replacement. Pain. 1993;53:17–25. doi: 10.1016/0304-3959(93)90050-Y. [DOI] [PubMed] [Google Scholar]
- 13.Cone RD, Lu D, Koppula S, Vage DI, Klungland H, Boston B, Chen W, Orth DN, Pouton C, Kesterson RA. The melanocortin receptors: Agonists, antagonists, and the hormonal control of pigmentation. Rec Prog Horm Res. 1996;51:287–317. [PubMed] [Google Scholar]
- 14.D’amour FE, Smith DL. A method for determining loss of pain sensation. J Pharmacol Exp Ther. 1941;72:74–79. [Google Scholar]
- 15.Kest B, Palmese C, Hopkins E. A comparison of morphine analgesic tolerance in male and female mice. Brain Res. 2000;879:17–22. doi: 10.1016/s0006-8993(00)02685-8. [DOI] [PubMed] [Google Scholar]
- 16.Vanderah TW, Suenaga NM, Ossipov MH, Malan TP, Jr, Lai J, Porreca F. Tonic descending facilitation from the rostral ventromedial medulla mediates opioid-induced abnormal pain and antinociceptive tolerance. J Neurosci. 2001;21:279–286. doi: 10.1523/JNEUROSCI.21-01-00279.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gutstein HB. The effects of pain on opioid tolerance: How do we resolve the controversy? Pharmacol Rev. 1996;48:403–407. [PubMed] [Google Scholar]
- 18.Yoburn BC, Cohen AH, Inturrisi CE. Pharmacokinetics and pharmacodynamics of subcutaneous naltrexone pellets in the rat. J Pharmacol Exp Ther. 1986;237:126–130. [PubMed] [Google Scholar]
- 19.Haley TJ, McCormick WG. Pharmacological effects produced by intracerebral injection of drugs in the conscious mouse. Br J Pharmacol. 1957;12:12–15. doi: 10.1111/j.1476-5381.1957.tb01354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu XJ, Colpaert F, Wiesenfeld-Hallin Z. Opioid hyperalgesia and tolerance versus 5-HT1A receptor-mediated inverse tolerance. Trends Pharmacol Sci. 2003;24:634–639. doi: 10.1016/j.tips.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Behbehani MM, Fields HL. Evidence that an excitatory connection between the periaqueductal gray and nucleus raphe magnus mediates stimulation produced analgesia. Brain Res. 1979;170:85–93. doi: 10.1016/0006-8993(79)90942-9. [DOI] [PubMed] [Google Scholar]
- 22.Xia Y, Wikberg JES, Chhajilani V. Expression of melanocortin 1 receptor in periaqueductal gray matter. Neuroreport. 1995;6:2193–2196. doi: 10.1097/00001756-199511000-00022. [DOI] [PubMed] [Google Scholar]
- 23.Woolf CJ. Intrathecal high dose morphine produces hyperalgesia in the rat. Brain Res. 1981;209:491–495. doi: 10.1016/0006-8993(81)90176-1. [DOI] [PubMed] [Google Scholar]
- 24.Crain SM, Shen KF. Acute thermal hyperalgesia elicited by low-dose morphine in normal mice is blocked by ultra-low-dose naltrexone, unmasking potent opioid analgesia. Brain Res. 2001;888:75–82. doi: 10.1016/s0006-8993(00)03010-9. [DOI] [PubMed] [Google Scholar]
- 25.Holtman JR, Jr, Wala EP. Characterization of morphine-induced hyperalgesia in male and female rats. Pain. 2005;114:62–70. doi: 10.1016/j.pain.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 26.Labella FS, Pinsky C, Havlicek V. Morphine derivatives with diminished opiate receptor potency show enhanced central excitatory activity. Brain Res. 1979;174:263–271. doi: 10.1016/0006-8993(79)90849-7. [DOI] [PubMed] [Google Scholar]
- 27.Bartlett SE, Dodd PR, Smith MT. Pharmacology of morphine and morphine-3-glucuronide at opioid, excitatory amino acid, GABA and glycine binding sites. Pharmacol Toxicol. 1994;75:73–81. doi: 10.1111/j.1600-0773.1994.tb00327.x. [DOI] [PubMed] [Google Scholar]
- 28.Lipkowski AW, Carr DB, Langlade A, Osgood PF, Szyfelbein SK. Morphine-3-glucuronide: Silent regulator of morphine actions. Life Sci. 1994;55:149–154. doi: 10.1016/0024-3205(94)90106-6. [DOI] [PubMed] [Google Scholar]
- 29.Bartlett SE, Cramond T, Smith MT. The excitatory effects of morphine-3-glucuronide are attenuated by LY274614, a competitive NMDA receptor antagonist, and by midazolam, an agonist at the benzodiazepine site on the GABAA receptor complex. Life Sci. 1994;54:687–694. doi: 10.1016/0024-3205(94)00552-4. [DOI] [PubMed] [Google Scholar]