Abstract
The expansion of myeloid-derived suppressor cells (MDSCs) and its correlation with advanced disease stage have been shown in solid cancers. Here, we investigated the functional features and clinical significance of MDSCs in extranodal NK/T cell lymphoma (ENKL). A higher percentage of circulating HLA-DR−CD33+CD11b+ MDSCs was observed in ENKL patients than in healthy controls (P < 0.05, n = 32) by flow cytometry analysis. These MDSCs from ENKL patients (ENKL-MDSCs) consisted of CD14+ monocytic (Mo-MDSCs, >60 %) and CD15+ granulocytic (PMN-MDSCs, <20 %) MDSCs. Furthermore, these ENKL-MDSCs expressed higher levels of Arg-1, iNOS and IL-17 compared to the levels of MDSCs from healthy donors, and they expressed moderate levels of TGFβ and IL-10 but lower levels of CD66b. The ENKL-MDSCs strongly suppressed the anti-CD3-induced allogeneic and autologous CD4 T cell proliferation (P < 0.05), but they only slightly suppressed CD8 T cell proliferation (P > 0.05). Interestingly, ENKL-MDSCs inhibited the secretion of IFNγ but promoted IL-10, IL-17 and TGFβ secretion as well as Foxp3 expression in T cells. The administration of inhibitors of iNOS, Arg-1 and ROS significantly reversed the suppression of anti-CD3-induced T cell proliferation by MDSCs (P < 0.05). Importantly, based on multivariate Cox regression analysis, the HLA-DR−CD33+CD11b+ cells and CD14+ Mo-MDSCs were independent predictors for disease-free survival (DFS, P = 0.013 and 0.016) and overall survival (OS, P = 0.017 and 0.027). Overall, our results identified for the first time that ENKL-MDSCs (mainly Mo-MDSCs) have a prognostic value for patients and a suppressive function on T cell proliferation.
Electronic supplementary material
The online version of this article (doi:10.1007/s00262-015-1765-6) contains supplementary material, which is available to authorized users.
Keywords: Prognosis, Immunosuppression, Hematopoietic malignancy, MDSCs, NK/T cell lymphoma
Introduction
Extranodal natural killer (NK)/T cell lymphoma (ENKL) has distinct epidemiological, clinical, histological and etiological features. Clinically, ENKL predominantly occurs in the nasal–paranasal area, skin, gastrointestinal tract or other extranodal sites, and it has a poor prognosis caused by rapid lesion progression [1]. Among the Epstein–Barr virus (EBV)-related lymphomas including Hodgkin lymphoma and Burkitt lymphoma, ENKL is the one most closely associated with EBV infection. EBV latent type II antigens, including latent membrane protein-1 and protein-2 (LMP1 and LMP2) and EBV nuclear antigen 1 (EBNA1), are present in ENKL tumor cells. Immune imbalance has been shown to be an important feature of ENKL patients [2, 3]. However, the role of immune cells during ENKL progression remains largely unclear.
Myeloid-derived suppressor cells (MDSCs) are a heterogeneous population of bone marrow-derived myeloid progenitors including macrophages, granulocytes, dendritic cells and immature myeloid cells [4, 5]. Studies in recent years have revealed that MDSCs expand dramatically during tumor growth and are a cause of immune evasion of many types of tumors, including multiple myeloma [6, 7]. MDSCs enhance tumor growth by inhibiting immune responses and T cell proliferation as well as facilitating tumor metastasis and angiogenesis [8–12]. MDSCs can inhibit anti-tumor immunity by suppressing T cell and NK cell functions by increasing the production of arginine, reactive oxygen species (ROS) and nitric oxide (NO) as well as by inducing Treg cells and TGF-β secretion to mediate T cell suppression [13–15]. To our knowledge, the role of MDSCs, a novel immune-suppressive cell subset, during ENKL tumor progression has not previously been reported. In this study, we detected the frequency of MDSCs in the peripheral blood of ENKL patients to characterize the phenotypic and functional features of MDSCs in ENKL, and we further assessed its clinical significance and prognostic value.
Materials and methods
Patients
Peripheral blood mononuclear cells (PBMCs) were collected from 32 age-matched healthy donors and 32 patients with ENKL at the first time of diagnosis at Sun Yat-Sen University Cancer Center (Guangzhou, China) from July 2010 to December 2012. The clinical details of the patients are shown in Supplementary Table 1. All patients were diagnosed with ENKL, and the lymphoma involved nasal and paranasal lesions in 25 cases (upper aerodigestive tract NK/T cell lymphoma, UNKTL; 84.4 %). The median age was 40.5 years old, and the age range was from 17 to 70 years. There were 19 patients in stage I, 3 patients in stage II, 3 patients in stage III and 7 patients in stage IV. Nine patients had elevated serum lactate dehydrogenase (LDH) levels, and 20 patients had B symptoms. The International Prognostic Index (IPI) was high-intermediate/high (2–5) in eight patients. For the Korean Prognostic Index (KPI) model, 17 patients (53.1 %) had none or one adverse factor, and 15 patients (46.9 %) had two to four adverse factors. In the Peripheral T cell lymphoma Prognostic Index (PIT) model, the majority of the patients (20 cases, 62.5 %) had none or one adverse factor, and the other 12 cases (37.5 %) had at least two adverse factors. Nine of the 32 patients were deceased, and the 5-year overall survival was 71.9 % with a median follow-up of 52 months.
All patients and healthy donors provided informed consent prior to the blood sampling. The study was approved by the Research Ethics Committee of the Sun Yat-Sen University Cancer Center.
Flow cytometry analysis
Human monoclonal antibodies against HLA-DR, CD33, CD11b, CD14, CD15, CD66b, iNOS, Arg-1, IL-10, IL-17 and TGFβ conjugated to different fluorescent dyes were obtained from BD Pharmingen (San Jose, CA, USA) or eBioscience (San Diego, CA, USA), and they were used to measure the frequency and phenotype of the MDSCs via surface staining or intracellular staining (Supplementary Table 2). PBMCs were isolated via Ficoll-Hypaque gradient centrifugation to measure the proportion and phenotype of MDSCs. For surface staining, the cells were washed twice and stained for 1 h on ice with mixtures of fluorescence-conjugated surface mAbs or isotype-matched controls. The cells were then washed twice and resuspended in PBS buffer for flow cytometry analysis. The intracellular staining of IL-17 and the other cytokines was performed on PBMCs stimulated with lipopolysaccharide (LPS, 1 μg/ml) for 4 h in RPMI 1640 medium, and the cytokine secretion was blocked by the addition of brefeldin A (10 µg/ml, eBioscience). After washing, the cells were stained with anti-CD33, anti-CD11b and anti-HLA-DR. The cells were then fixed, permeabilized with Perm/Fix solution (eBiosciences) and stained intracellularly with anti-IL-17 or fluorescence-conjugated antibodies for other cytokines. The samples were evaluated on a FC500 flow cytometer (Beckman Coulter) and analyzed with CXP Software (Beckman Coulter, Inc., Fullerton, CA, USA).
T cell suppression assay
CD33+ cells were isolated from the PBMCs from the healthy donors or ENKL patients using human CD33 MicroBeads (Miltenyi Biotec, Bergisch Gladbach, Germany) according to the manufacturer’s instructions. The PBMCs from healthy donors were labeled with 5 μM carboxyfluorescein succinimidyl ester (CFSE; Molecular Probes, Eugene, Oregon, USA) in 1 ml of PBS for 15 min at 37 °C. The labeling was halted by adding an excess of FCS, and the samples were washed twice with RPMI 1640 (Gibco, Life Technologies, China) supplemented with 10 % fetal bovine serum (FBS; ExCell Biology, South America). The CSFE-labeled cells were cultured in an anti-CD3 antibody (OKT3)-coated 96-well plate with or without sorting the CD33+ cells from the ENKL patients or healthy donors at different ratios for 3 days, and N-hydroxy-nor-l-arginine (NOHA; 1 mM), l-NG-monomethylarginine (l-NMMA, 100 μM) or N-acetylcysteine (NAC 1, mM) was added to a portion of the samples. The CFSE fluorescence intensity was analyzed by flow cytometry after 7 days of co-culture and proliferation.
Statistical analyses
The numerical data are shown as the mean ± standard error (SEM). The statistical analysis was performed with the SPSS 13.0 software (SPSS, Chicago, IL, USA) or GraphPad Prism analysis tools (La Jolla, CA, USA). Two group comparisons were tested using Student’s t test, and the association of the density of the MDSCs with the clinical pathological features was examined using Pearson’s chi-square test. The overall survival (OS) was measured from the date of the diagnosis to the date of death from any cause or to the date of the last follow-up visit. The disease-free survival (DFS) was defined as the time from the diagnosis to the first occurrence of progression, relapse after a response, death from any cause, or to the date of the last follow-up of the surviving patients. The survival curves were determined by the Kaplan–Meier method and the log-rank test. A Cox proportional hazards regression analysis was performed to identify the independent prognostic factors for the OS or DFS. The cutoff value was the median of all variants. The statistical tests were based on a level of significance at P < 0.05.
Results
The expansion and clinical implication of circulating MDSCs in ENKL
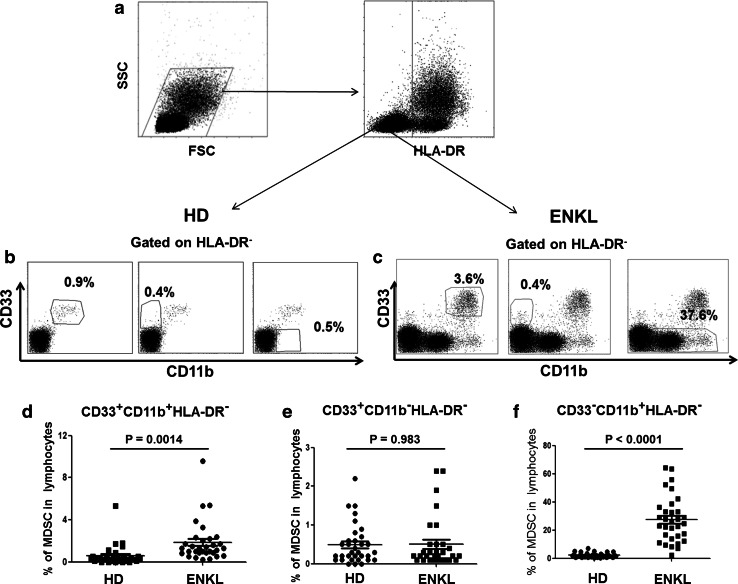
We investigated the frequency of MDSCs in the peripheral blood mononuclear cells (PBMCs) of 32 ENKL patients. Flow cytometry analysis showed that the percentage of HLA-DR−CD33+CD11b+ and HLA-DR−CD33−CD11b+ cells was increased in the PBMCs from ENKL patients compared with those from healthy controls (P = 0.0014 and P = 0.0001, respectively) as shown in Fig. 1. No correlation between the frequency of MDSC populations and clinicopathological factors, including age, gender, Ann Arbor Stage, subtypes, LDH level, B symptoms, KPI, PIT and IPI scores, was observed (P > 0.05) as shown in Supplementary Table 3. Further, no correlation was found between the frequency of the circulating CD14+ monocytic (Mo-MDSCs) or CD15+ granulocytic (PMN-MDSCs) subsets and clinicopathological parameters (P > 0.05, Supplementary Table 4).
Fig. 1.
Expansion of MDSCs in patients with extranodal NK/T cell lymphoma. a Gating routine for MDSC subsets. b–c The dot plots represent the CD33+CD11b+ cell subset, the CD33+CD11b− cell subset and the CD33−CD11b+ cell subset gating on the HLA-DR− fraction among the PBMCs from healthy donors (b) or ENKL patients (c). d–f The statistical analysis of the percentage of the MDSC subsets among the PBMCs from the ENKL patients (n = 32) and healthy donors (n = 32). The error bar represents the SEM. Student’s t test is used. HD healthy donor, ENKL extranodal NK/T cell lymphoma
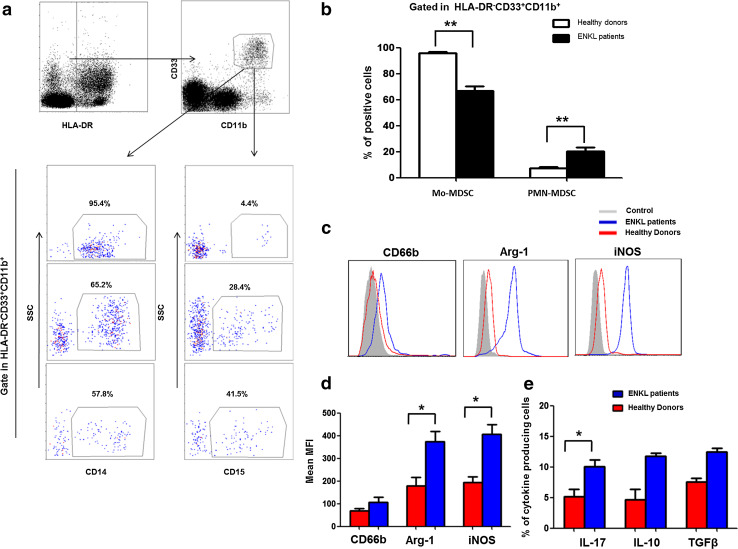
The phenotypic properties and cytokine profile of MDSCs in ENKL
Based on a previous study [12], we described the HLA-DR−CD33+CD11b+ cells as MDSCs in subsequent experiments. To evaluate the phenotypic properties of this population in the PBMCs from patients with ENKL (ENKL-MDSCs), we screened the specific markers and cytokines of ENKL-MDSCs using FACS analysis and a multiple gate strategy. First, based on previous reports, we determined that the ENKL-MDSCs predominantly consisted of CD14+ Mo-MDSCs (>60 %), and the CD15+ PMN-MDSC subset represented approximately 20 % of the MDSC population of ENKL patients. The proportion of Mo-MDSCs and PMN-MDSCs in the peripheral blood of ENKL patients was significantly different to that of healthy donors (P < 0.05, Fig. 2a, b). Furthermore, the ENKL-MDSCs displayed a significantly higher level of Arg-1 and iNOS compared to healthy donors (P < 0.05), and the MDSCs from both ENKL patients and healthy donors displayed a moderate level of CD66b as shown in Fig. 2c, d. In addition, we found that the MDSCs secreted a moderate level of IL-17, IL-10 and TGFβ. Interestingly, the ENKL-MDSCs secreted a significantly higher level of IL-17 (P < 0.05) and a slightly higher level of IL-10 and TGFβ compared to the levels of the MDSCs from healthy donors (Fig. 2e).
Fig. 2.
Phenotypes and cytokine profiles of HLA-DR−CD33+CD11b+ MDSCs in extranodal NK/T cell lymphoma patients. The HLA-DR−CD33+CD11b+ cells are gated as MDSCs from 22 NK/T cell lymphoma patients. The properties of the MDSCs are analyzed via flow cytometry using multiple antihuman mAbs against CD14, CD15, CD66b, iNOS, Arg-1, IL-17, IL-10 and TGFβ. a Representative FACS plots of the CD14+ or CD15+ MDSCs from the same ENKL patients. b Graph of the CD14+ Mo-MDSCs and CD15+ PNM-MDSCs among the PBMCs from 22 ENKL patients and 22 healthy controls. c Representative FACS histogram for CD66b, iNOS and Arg-1 expression in ENKL-MDSCs and MDSCs from healthy control. d The data shown are the MFI of CD66b, iNOS and Arg-1 in ENKL-MDSCs from 22 ENKL patients and MDSCs from healthy controls determined by cytofluorimetric analysis and are corrected for background staining. e The percentage of cytokine-producing ENKL-MDSCs from 22 ENKL patients and MDSCs from healthy controls, including IL-17, IL-10 and TGFβ. MFI, mean fluorescence intensity; **P < 0.01; *P < 0.05
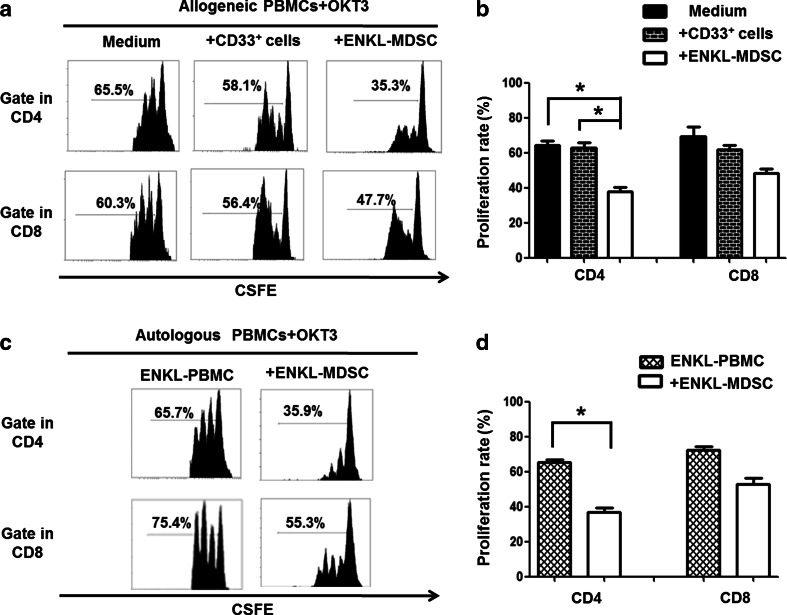
ENKL-MDSC-mediated suppression of T cell proliferation is dependent on NO and ROS production
To further understand the role of MDSCs in ENKL progression, we investigated the immunosuppressive function of MDSCs isolated from the PBMCs of ENKL patients. The CD33+ cells isolated from the ENKL patients showed noticeable inhibition of the proliferation of allogeneic and autologous OKT3-stimulated CD4 T cells (P < 0.05), but only a slight suppression of allogeneic and autologous OKT3-stimulated CD8 T cell proliferation was observed (P > 0.05) as shown in Fig. 3. Our observations indicated that the ENKL-MDSCs displayed a suppressive function dependent on MHC limitation and non-specific suppression, especially for CD4 T cell proliferation.
Fig. 3.
ENKL-MDSCs suppress allogeneic and autologous T cell proliferation. T cell proliferation is examined by CSFE labeling in vitro. The CD33+ cells are sorted from the PBMCs from five patients with ENKL, and CD33+ cells from healthy donors are included as a control. The CSFE-labeled PBMCs are co-cultured with the CD33+ cells at a ratio of 2:1 in OKT3-coated 96-well plates. After 3 days, the cells are collected and quantified using flow cytometry. a, c Allogeneic and autologous OKT3-stimulated PBMCs. Representative FACS density plots from one of the five experiments. b, d The graph of the statistical analyses is presented. The error bars represent the SEM. n = 5; *P < 0.05; HD healthy donors
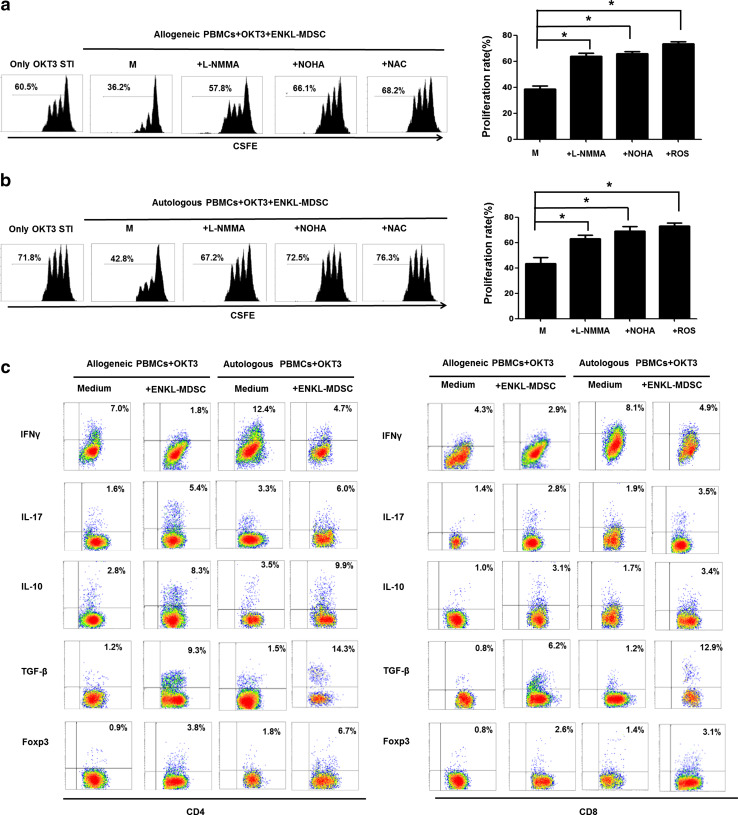
Subsequently, we further explored the potential suppressive mechanism of MDSCs in ENKL. Firstly, in the ENKL-MDSC population, iNOS and Arg-1 were highly expressed (Fig. 2c, d). iNOS and Arg-1 are key enzymes responsible for arginine metabolism and the production of NO, respectively. These enzymes share the same substrate, l-arginine, and are associated with MDSC-mediated suppression [16, 17]. We further investigated the underlying mechanisms controlling MDSC-mediated T cell suppression in ENKL by blocking the activity of iNOS, Arg-1 and ROS production in MDSCs. Suppression of T cells mediated by CD33+ cells isolated from the ENKL patients was almost completely recovered after administration of the arginase inhibitor (NOHA), the nitric oxide synthase inhibitor (l-NMMA) or the ROS inhibitor (NAC) (Fig. 4a, b). When OKT3-stimulated CD4 or CD8 T cells were co-cultured with MDSCs from ENKL patients for 3 days, we found that the secretion of IL-10, TGFβ and IL-17 as well as Foxp3 expression were significantly increased, while the secretion of IFNγ was significantly decreased (Fig. 4c). These data suggested that when T cells are co-cultured with ENKL-MDSCs, the altered cytokine secretion from T cells, including increased IL-10 and TGFβ secretion, as well as induction of Foxp3+ Treg cells, suppresses T cell proliferation.
Fig. 4.
Multiplex mechanisms are involved in the ENKL-MDSC-mediated suppression of T cell proliferation. l-NMMA, NOHA or NAC is added to a portion of the samples in the co-culture system of CSFE-labeled PBMCs and ENKL-MDSCs at ratio 2:1 in OKT3-coated 96-well plates. After 3 days, the cells are collected and quantified using flow cytometry. a, b Allogeneic and autologous OKT3-stimulated PBMCs. c Cytokine secretion (IFNγ, IL-17, IL-10 and TGFβ) and Foxp3 expression in CD4 or CD8 T cells in the presence of allogeneic ENKL-MDSCs, autologous ENKL-MDSCs or only in medium. l-NMMA, NG-methyl-l-arginine; NOHA, N-hydroxy-nor-l-arginine; NAC, N-acetylcysteine; Student’s t test is used
The correlation of MDSC populations and ENKL patient prognosis
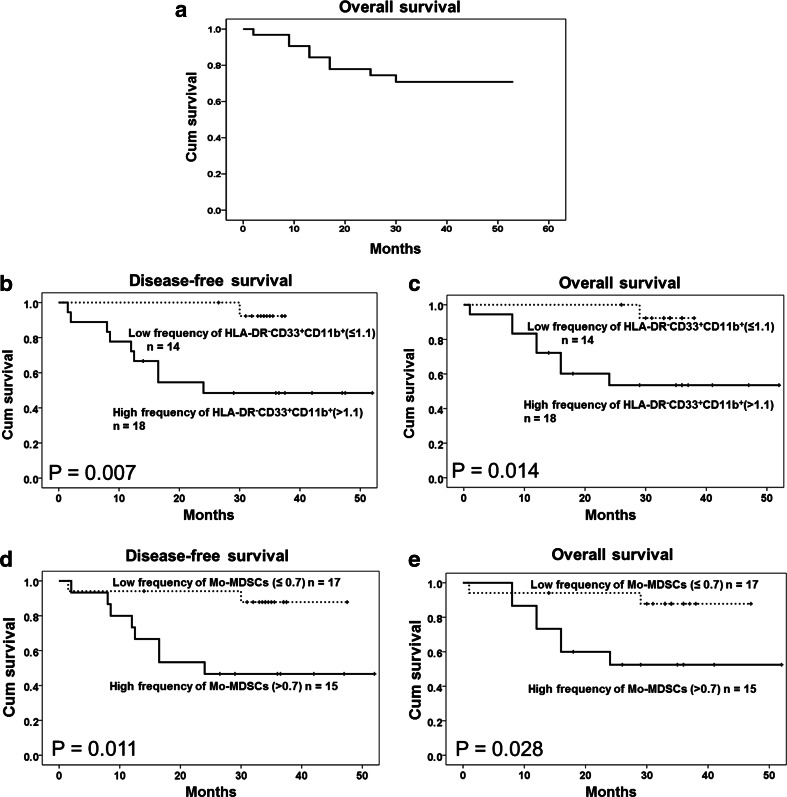
Nine patients (28.1 %) had died by the time of analysis (Supplementary Table 1), and the patients with a higher frequency of circulating HLA-DR−CD33+CD11b+ MDSCs and CD14+ Mo-MDSCs, which are the main composition of MDSC populations, had shorter DFS (P = 0.007 and 0.011) and OS (P = 0.014 and 0.028) (Fig. 5). However, no association was found between patient survival and the frequency of CD15+ PMN-MDSCs or HLA-DR−CD33−CD11b+ cells in ENKL patients (P > 0.05, Supplementary Figure 1). In addition to the frequency of HLA-DR−CD33+CD11b+ MDSCs and CD14+ Mo-MDSCs, the Ann Arbor Stage, LDH level, KPI and IPI scores were significant prognostic indicators for survival (P < 0.05). After adjusting for the key clinical prognostic factors and using a multivariate Cox regression analysis (Table 1), the HLA-DR−CD33+CD11b+ MDSCs and CD14+ Mo-MDSCs remained significant and independent predictors of DFS (P = 0.013, HR 21.633, 95 % CI 1.892–247.378; P = 0.016, HR 7.873, 95 % CI 1.467–42.238) and OS (P = 0.017, HR 19.593, 95 % CI 1.694–226.646; P = 0.027, HR 6.867, 95 % CI 1.243–37.948) in ENKL patients.
Fig. 5.
Correlation of circulating MDSCs or Mo-MDSCs with survival in extranodal NK/T cell lymphoma cases. a The overall survival (OS) curve of 32 ENKL patients. b, c The DFS and OS rates are significantly different between the high and low HLA-DR−CD33+CD11b+ cell counts (P = 0.007 and 0.014, respectively, log-rank test). d, e The DFS and OS rates are significantly different between the high and low CD14+ Mo-MDSC counts (P = 0.011 and 0.028, respectively, log-rank test). The cutoff value is the median of the HLA-DR−CD33+CD11b+ cell or CD14+ Mo-MDSC density
Table 1.
Univariate and multivariate Cox regression analysis for DFS and OS of 32 patients with ENKL
| Variables | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| HR (95 % CI) | P value | HR (95 % CI) | P value | |
| In MDSC population | ||||
| Disease-free survival | ||||
| Age (<40/≥40) | 1.259 (0.355–4.470) | 0.722 | ||
| Gender (female/male) | 1.930 (0.544–6.852) | 0.309 | ||
| Ann Arbor stage (I/II–IV) | 3.434 (0.959–12.293) | 0.045* | 1.748 (0.368–8.295) | 0.482 |
| Subtypes (UNKTL/EUNKTL) | 1.306 (0.277–6.164) | 0.736 | ||
| B symptoms (no/yes) | 55.563 (0.323–9550.869) | 0.126 | ||
| LDH level (normal/elevated) | 3.834 (1.091–13.474) | 0.036* | 0.875 (0.070–10.912) | 0.918 |
| KPI score (0–1/2–4) | 3.417 (0.881–13.250) | 0.076 | ||
| PIT score (0–1/2–4) | 3.031 (0.852–10.785) | 0.084 | ||
| IPI score (0–1/2–5) | 3.718 (1.074–12.874) | 0.038* | 5.327 (0.324–87.663) | 0.242 |
| MDSC frequency (low/high)a | 10.216 (1.285–81.244) | 0.028* | 21.633 (1.892–247.378) | 0.013* |
| Overall survival | ||||
| Age (<40/≥40) | 1.370 (0.342–5.491) | 0.656 | ||
| Gender (female/male) | 1.798 (0.449–7.198) | 0.407 | ||
| Ann Arbor stage (I/II–IV) | 3.894 (0.969–15.650) | 0.046* | 2.090 (0.374–11.678) | 0.401 |
| Subtypes (UNKTL/EUNKTL) | 1.515 (0.315–7.320) | 0.603 | ||
| B symptoms (no/yes) | 53.653 (0.233–12,381.115) | 0.151 | ||
| LDH level (normal/elevated) | 5.011 (1.318–19.059) | 0.018* | 1.155 (0.085–15.622) | 0.914 |
| KPI score (0–1/2–4) | 2.723 (0.680–10.908) | 0.157 | ||
| PIT score (0–1/2–4) | 4.063 (1.014–16.290) | 0.048* | 1.284 (0.095–17.339) | 0.851 |
| IPI score (0–1/2–5) | 4.814 (1.289–17.977) | 0.019* | 6.153 (0.361–104.775) | 0.209 |
| MDSC frequency (low/high) | 8.644 (1.073–69.636) | 0.043* | 19.593 (1.694–226.646) | 0.017* |
| In Mo-MDSC population | ||||
| Disease-free survival | ||||
| Age (<40/≥40) | 1.259 (0.355–4.470) | 0.722 | ||
| Gender (female/male) | 1.930 (0.544–6.852) | 0.309 | ||
| Ann Arbor stage (I/II–IV) | 3.434 (0.959–12.293) | 0.045* | 1.549 (0.402–5.970) | 0.525 |
| Subtypes (UNKTL/EUNKTL) | 1.306 (0.277–6.164) | 0.736 | ||
| B symptoms (no/yes) | 55.563 (0.323–9550.869) | 0.126 | ||
| LDH level (normal/elevated) | 3.834 (1.091–13.474) | 0.036* | 1.843 (0.211–16.130) | 0.581 |
| KPI score (0–1/2–4) | 3.417 (0.881–13.250) | 0.076 | ||
| PIT score (0–1/2–4) | 3.031 (0.852–10.785) | 0.084 | ||
| IPI score (0–1/2–5) | 3.718 (1.074–12.874) | 0.038* | 3.181 (0.358–28.269) | 0.299 |
| Mo-MDSC frequency (low/high)a | 5.956 (1.249–28.411) | 0.025* | 7.873 (1.467–42.238) | 0.016* |
| Overall survival | ||||
| Age (<40/≥40) | 1.370 (0.342–5.491) | 0.656 | ||
| Gender (female/male) | 1.798 (0.449–7.198) | 0.407 | ||
| Ann Arbor stage (I/II–IV) | 3.894 (0.969–15.650) | 0.046* | 2.275 (0.436–11.878) | 0.330 |
| Subtypes (UNKTL/EUNKTL) | 1.515 (0.315–7.320) | 0.603 | ||
| B symptoms (no/yes) | 53.653 (0.233–12,381.115) | 0.151 | ||
| LDH level (normal/elevated) | 5.011 (1.318–19.059) | 0.018* | 2.684 (0.240–30.257) | 0.423 |
| KPI score (0–1/2–4) | 2.723 (0.680–10.908) | 0.157 | ||
| PIT score (0–1/2–4) | 4.063 (1.014–16.290) | 0.048* | 0.544 (0.039–7.604) | 0.651 |
| IPI score (0–1/2–5) | 4.814 (1.289–17.977) | 0.019* | 4.432 (0.342–57.364) | 0.254 |
| Mo-MDSC frequency (low/high) | 4.890 (1.004–23.809) | 0.049* | 6.867 (1.243–37.948) | 0.027* |
DFS disease-free survival, OS overall survival, HR hazard ratio, CI confidence interval, LDH lactate dehydrogenase, IPI International Prognostic Index, KPI Korean Prognostic Index, PIT Peripheral T cell lymphoma Prognostic Index
* Significant difference
aMDSC (high/low) is based on the median value of the MDSC density
Discussion
It has been suggested that tumor pathogenesis is linked to immune imbalance and immune cell dysfunction. In this regard, tumors are found to affect myelopoiesis and induce the expansion of myeloid cells with immunosuppressive activity in tumor-bearing hosts, including animal models and human patients [18–22]. In this study, we found an expansion of HLA-DR−CD33+CD11b+ and HLA-DR−CD33−CD11b+ cells in the peripheral blood of ENKL patients. However, only the density of HLA-DR−CD33+CD11b+ MDSCs and not that of HLA-DR−CD33−CD11b+ cells was a significant and independent predictor for ENKL patient survival. This result was in line with our study on nasopharyngeal carcinoma (NPC) (unpublished data) and indicated that CD33 expression is an important marker for the MDSC population in cancer patients. Although the HLA-DR−CD33−CD11b+ cell population was expanded in ENKL patients, no clinical relevance and prognostic value was found in this cell population, and this cell population lacked the phenotypic features of MDSCs (Supplementary Figure 1). Our observations indicated that the immune-suppressive cell subset of HLA-DR−CD33+CD11b+ MDSCs has a prognostic value similar to that of Treg cells and other clinical parameters, including TNM stage, IPI score, and LDH level, in ENKL [23, 24].
Human MDSCs constitute a heterogeneous group. The definitive identification of human MDSCs is complicated by a lack of a specific marker and by the absence of a human homolog of mouse Gr-1 [12, 25, 26]. Human MDSCs include the Mo-MDSC and the PMN-MDSC subsets and, according to recent data, the myeloid subset, which has suppressive activity. The MDSC phenotypes are commonly evaluated using a single multicolor staining protocol for MDSC1–MDSC6 as follows: MDSC1 (CD14+IL-4Rα+); MDSC2 (CD15+ IL-4Rα+); MDSC3 (Lineage− HLA-DR− CD33+); MDSC4 (CD14+HLA-DRlow/−); MDSC5 (CD11b+CD14−CD15+); and MDSC6 (CD15+ FSClow SSChigh) [27]. The MDSC phenotype varies by differentiation status and function in response to the environmental conditions of different cancers, and the MDSC phenotype has been defined as the HLA-DR−CD33+CD11b+ cell population, including PMN- and Mo-MDSCs, in many human cancers, including multiple myeloma [12, 27]. Based on our observations and those of others, ENKL-MDSCs were immunophenotyped as an HLA-DR−CD33+CD11b+ cell population in this study.
The ENKL-MDSC population consisted predominantly of CD14+ Mo-MDSCs with a minority of CD15+ PMN-MDSCs. Compared to healthy controls, however, the proportion of Mo-MDSCs in ENKL-MDSCs was decreased, and the proportion of PMN-MDSCs in ENKL-MDSCs was increased. The ENKL-MDSC population highly expressed immune mediator molecules, including Arg-1 and iNOS, and it expressed a low level of CD66b. Furthermore, these ENKL-MDSCs secreted moderate levels of suppressive cytokines, including IL-17, IL-10 and TGFβ, and they did not secrete the IFNγ inflammatory cytokine (data not shown). Compared with MDSCs from healthy donors, the ENKL-MDSCs expressed significant higher level of Arg-1 and iNOS, and they secreted higher levels of IL-17 (P < 0.05).
MDSCs can suppress T cell activation and proliferation in tumor-bearing hosts [28]. Our previous study and other studies have identified that human MDSCs from solid tumors or multiple myeloma can suppress anti-CD3-induced autologous or allogeneic T cell proliferation, including CD4+ and CD8+ T cells. There have been reports indicating that MDSC suppression requires antigen presentation through major histocompatibility complex (MHC) class I molecules [25, 29–33]. However, some studies have suggested that the MDSC suppression is dependent on innate immune sensing and that the MDSC-mediated T cell inhibition is a result of the activation of iNOS, leading to increased production of NO and ROS. Thus, the activated antigen-specific CD4+ T cells interact with MDSCs loaded with specific antigens, converting these cells to non-specific suppressors in cancers [16, 34]. In this study, we observed that ENKL-MDSCs strongly suppressed the OKT3-stimulated allogeneic or autologous CD4 T cell proliferation but that they only slightly suppressed the OKT3-stimulated allogeneic and autologous CD8 T cell proliferation. These results indicated that the suppression of T cell proliferation by ENKL-MDSCs is both antigen specific and non-antigen specific, especially for CD4 T cell proliferation. Furthermore, our data were in line with the suggestion that MDSCs from tumor-bearing hosts, as characterized by a high level of iNOS/NOS2 and Arg-1, are potent inhibitors of Ag-specific T cell functions that are able to suppress T cells in an Ag-independent manner [5, 13, 20, 35–40]. Furthermore, our results showed that blockage of iNOS, Arg-1 and ROS recovered the MDSC-mediated inhibition of anti-CD3-induced allogeneic and autologous PBMC proliferation. Interestingly, our observations suggested that the inhibition of T cell proliferation by ENKL-MDSCs also correlated with suppressed cytokine secretion, including IL-10 and TGFβ, as well as induction of Treg cells, which was in line with other reports in solid cancers [41, 42]. Our observations suggested that multiplex mechanisms that include NO production, ROS production, cytokine induction (IL-10 and TGFβ), and Treg cell induction are involved in ENKL-MDSC-mediated suppression.
The percentage or the frequency of MDSC population is always correlated with poor survivals of cancer patients [43, 44]. Here, our study demonstrated that the HLA-DR−CD33+CD11b+ MDSC population was an independent poor prognostic indicator for DFS and OS of ENKL patients. Our data further showed that the Mo-MDSC population, but not the PMN-MDSC population, is an independent predictor for DSF and OS in ENKL patients. These observations may explain why the Mo-MDSCs were the main component of the MDSC population in ENKL patients. Our results are in line with reports by others. Some studies have indicated that the CD14+ MDSC population is associated with disease progression in cancers [29, 45, 46].
In addition, the number of circulating IL-17-producing MDSCs correlated with patient DFS and OS. IL-17 is an inflammatory cytokine typically secreted by CD4 Th17 and CD8 Tc17 cells [47]. Recent findings have indicated that the role of IL-17 in tumor development is controversial, and IL-17 could promote the induction of MDSCs at a tumor site and enhance the suppressive function of MDSCs on T cell proliferation [48–52]. Our observations for the first time indicate that ENKL-MDSCs can secrete higher levels of IL-17 compared to healthy donors and that the number of IL-17-producing MDSCs is correlated with ENKL patient prognosis (Supplementary Figure 2). A functional investigation of IL-17-producing MDSCs should be performed in future studies.
Conclusions
This study analyzed for the first time the phenotypic and functional properties as well as the clinical significance of the MDSC population in ENKL patients. Our results revealed an expansion of circulating MDSCs in ENKL patients; these ENKL-MDSCs mainly consist of CD14+ Mo-MDSCs and express high levels of iNOS, Arg-1 and suppressive cytokines including IL-10, TGFβ and IL-17. The ENKL-MDSC-mediated suppression of OKT3-stimulated allogeneic and autologous T cell proliferation is dependent on iNOS, Arg-1 and ROS activities and is correlated with cytokine changes and Treg cell induction. Moreover, increases in circulating MDSCs and Mo-MDSCs correlate with poor DFS and OS in patients, and they are independent predictors in ENKL. Collectively, these findings demonstrate a novel role and mechanism of MDSCs in the tumor pathogenesis of ENKL, thus unveiling a new avenue for ENKL immunotherapy.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
This work was supported by grants from the General Program (Grant Nos. 81372442 and 81172164, Li J.; 81272341, Zhang X.S.) of the National Natural Science Foundation of China.
Abbreviations
- CFSE
Carboxyfluorescein diacetate succinimidyl ester
- DFS
Disease-free survival
- EBNA1
EBV nuclear antigen 1
- EBV
Epstein–Barr virus
- ENKL
Extranodal natural killer (NK)/T cell lymphoma
- HD
Healthy donor
- IFNγ
Interferon gamma
- iNOS
Inducible nitric oxide synthase
- IPI
International Prognostic Index
- KPI
Korean Prognostic Index
- LDH
Lactate dehydrogenase
- LMP1
Latent membrane protein-1
- LMP2
Latent membrane protein-2
- l-NMMA
NG-methyl l-arginine
- LPS
Lipopolysaccharide
- MDSCs
Myeloid-derived suppressor cells
- MHC
Major histocompatibility complex
- Mo-MDSCs
Monocytic MDSCs
- NAC
N-acetylcysteine
- NO
Nitric oxide
- NOHA
N-hydroxy-nor-l-arginine
- NPC
Nasopharyngeal carcinoma
- OS
Overall survival
- PBMCs
Peripheral blood mononuclear cells
- PMN-MDSCs
Polymorphonuclear MDSCs
- ROS
Reactive oxygen species
- SEM
Standard error of mean
- TGFβ
Transforming growth factor beta
- UNKTL
Upper aerodigestive tract NK/T cell lymphoma
Compliance with ethical standards
Conflict of interest
The authors declare no conflicts of interests.
Footnotes
Han Zhang, Ze-Lei Li and Shu-Biao Ye have contributed equally to this work.
Contributor Information
Xiao-Shi Zhang, Phone: 020-87343269, Email: zhangxsh@sysucc.org.cn.
Jiang Li, Phone: 020-87343174, Email: lijiang2@mail.sysu.edu.cn.
References
- 1.Suzuki R. Pathogenesis and treatment of extranodal natural killer/T-cell lymphoma. Semin Hematol. 2014;51(1):42–51. doi: 10.1053/j.seminhematol.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 2.Carbone A, Gloghini A, Dotti G. EBV-associated lymphoproliferative disorders: classification and treatment. Oncologist. 2008;13(5):577–585. doi: 10.1634/theoncologist.2008-0036. [DOI] [PubMed] [Google Scholar]
- 3.Jaccard A, Hermine O. Extranodal natural killer/T-cell lymphoma: advances in the management. Curr Opin Oncol. 2011;23(5):429–435. doi: 10.1097/CCO.0b013e328349aba6. [DOI] [PubMed] [Google Scholar]
- 4.Monu NR, Frey AB. Myeloid-derived suppressor cells and anti-tumor T cells: a complex relationship. Immunol Invest. 2012;41(6–7):595–613. doi: 10.3109/08820139.2012.673191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haile LA, Greten TF, Korangy F. Immune suppression: the hallmark of myeloid derived suppressor cells. Immunol Invest. 2012;41(6–7):581–594. doi: 10.3109/08820139.2012.680635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Romano A, Vetro C, Adriani M. Advances in understanding regulatory myeloid cells. Cancer Biol Ther. 2011;11(11):923–926. doi: 10.4161/cbt.11.11.15541. [DOI] [PubMed] [Google Scholar]
- 7.Brimnes MK, Vangsted AJ, Knudsen LM, Gimsing P, Gang AO, Johnsen HE, Svane IM. Increased level of both CD4+FOXP3+ regulatory T cells and CD14+HLA-DR(−)/low myeloid-derived suppressor cells and decreased level of dendritic cells in patients with multiple myeloma. Scand J Immunol. 2010;72(6):540–547. doi: 10.1111/j.1365-3083.2010.02463.x. [DOI] [PubMed] [Google Scholar]
- 8.Gantt S, Gervassi A, Jaspan H, Horton H. The role of myeloid-derived suppressor cells in immune ontogeny. Front Immunol. 2014;5:387. doi: 10.3389/fimmu.2014.00387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chandra D, Gravekamp C. Myeloid-derived suppressor cells: cellular missiles to target tumors. Oncoimmunology. 2013;2(11):e26967. doi: 10.4161/onci.26967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brandau S, Moses K, Lang S. The kinship of neutrophils and granulocytic myeloid-derived suppressor cells in cancer: cousins, siblings or twins? Semin Cancer Biol. 2013;23(3):171–182. doi: 10.1016/j.semcancer.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Ostrand-Rosenberg S, Sinha P, Beury DW, Clements VK. Cross-talk between myeloid-derived suppressor cells (MDSC), macrophages, and dendritic cells enhances tumor-induced immune suppression. Semin Cancer Biol. 2012;22(4):275–281. doi: 10.1016/j.semcancer.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Filipazzi P, Huber V, Rivoltini L. Phenotype, function and clinical implications of myeloid-derived suppressor cells in cancer patients. Cancer Immunol Immunother. 2012;61(2):255–263. doi: 10.1007/s00262-011-1161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu T, Ramakrishnan R, Altiok S, Youn JI, Cheng P, Celis E, Pisarev V, Sherman S, Sporn MB, Gabrilovich D. Tumor-infiltrating myeloid cells induce tumor cell resistance to cytotoxic T cells in mice. J Clin Invest. 2011;121(10):4015–4029. doi: 10.1172/JCI45862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ostrand-Rosenberg S. Myeloid-derived suppressor cells: more mechanisms for inhibiting antitumor immunity. Cancer Immunol Immunother. 2010;59(10):1593–1600. doi: 10.1007/s00262-010-0855-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centuori SM, Trad M, LaCasse CJ, Alizadeh D, Larmonier CB, Hanke NT, Kartchner J, Janikashvili N, Bonnotte B, Larmonier N, Katsanis E. Myeloid-derived suppressor cells from tumor-bearing mice impair TGF-beta-induced differentiation of CD4+CD25+FoxP3+Tregs from CD4+CD25−FoxP3− T cells. J Leukoc Biol. 2012;92(5):987–997. doi: 10.1189/jlb.0911465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Skabytska Y, Wolbing F, Gunther C, Koberle M, Kaesler S, Chen KM, Guenova E, Demircioglu D, Kempf WE, Volz T, Rammensee HG, Schaller M, Rocken M, Gotz F, Biedermann T. Cutaneous innate immune sensing of Toll-like receptor 2-6 ligands suppresses T cell immunity by inducing myeloid-derived suppressor cells. Immunity. 2014;41(5):762–775. doi: 10.1016/j.immuni.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 17.Hammami I, Chen J, Bronte V, DeCrescenzo G, Jolicoeur M. L-glutamine is a key parameter in the immunosuppression phenomenon. Biochem Biophys Res Commun. 2012;425(4):724–729. doi: 10.1016/j.bbrc.2012.07.139. [DOI] [PubMed] [Google Scholar]
- 18.Pronier E, Almire C, Mokrani H, Vasanthakumar A, Simon A, da Costa Reis Monte Mor B, Masse A, Le Couedic JP, Pendino F, Carbonne B, Larghero J, Ravanat JL, Casadevall N, Bernard OA, Droin N, Solary E, Godley LA, Vainchenker W, Plo I, Delhommeau F. Inhibition of TET2-mediated conversion of 5-methylcytosine to 5-hydroxymethylcytosine disturbs erythroid and granulomonocytic differentiation of human hematopoietic progenitors. Blood. 2011;118(9):2551–2555. doi: 10.1182/blood-2010-12-324707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fazi F, Racanicchi S, Zardo G, Starnes LM, Mancini M, Travaglini L, Diverio D, Ammatuna E, Cimino G, Lo-Coco F, Grignani F, Nervi C. Epigenetic silencing of the myelopoiesis regulator microRNA-223 by the AML1/ETO oncoprotein. Cancer Cell. 2007;12(5):457–466. doi: 10.1016/j.ccr.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 20.Green KA, Cook WJ, Green WR. Myeloid-derived suppressor cells in murine retrovirus-induced AIDS inhibit T- and B-cell responses in vitro that are used to define the immunodeficiency. J Virol. 2013;87(4):2058–2071. doi: 10.1128/JVI.01547-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yi H, Guo C, Yu X, Zuo D, Wang XY. Mouse CD11b+Gr-1+ myeloid cells can promote Th17 cell differentiation and experimental autoimmune encephalomyelitis. J Immunol. 2012;189(9):4295–4304. doi: 10.4049/jimmunol.1200086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ma Y, Shurin GV, Gutkin DW, Shurin MR. Tumor associated regulatory dendritic cells. Semin Cancer Biol. 2012;22(4):298–306. doi: 10.1016/j.semcancer.2012.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peng RJ, Huang ZF, Zhang YL, Yuan ZY, Xia Y, Jiang WQ, Zeng YX, Li J. Circulating and tumor-infiltrating Foxp3(+) regulatory T cell subset in Chinese patients with extranodal NK/T cell lymphoma. Int J Biol Sci. 2011;7(7):1027–1036. doi: 10.7150/ijbs.7.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim WY, Jeon YK, Kim TM, Kim JE, Kim YA, Lee SH, Kim DW, Heo DS, Kim CW. Increased quantity of tumor-infiltrating FOXP3-positive regulatory T cells is an independent predictor for improved clinical outcome in extranodal NK/T-cell lymphoma. Ann Oncol. 2009;20(10):1688–1696. doi: 10.1093/annonc/mdp056. [DOI] [PubMed] [Google Scholar]
- 25.Solito S, Pinton L, Damuzzo V, Mandruzzato S. Highlights on molecular mechanisms of MDSC-mediated immune suppression: paving the way for new working hypotheses. Immunol Invest. 2012;41(6–7):722–737. doi: 10.3109/08820139.2012.678023. [DOI] [PubMed] [Google Scholar]
- 26.Peranzoni E, Zilio S, Marigo I, Dolcetti L, Zanovello P, Mandruzzato S, Bronte V. Myeloid-derived suppressor cell heterogeneity and subset definition. Curr Opin Immunol. 2010;22(2):238–244. doi: 10.1016/j.coi.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 27.Solito S, Marigo I, Pinton L, Damuzzo V, Mandruzzato S, Bronte V. Myeloid-derived suppressor cell heterogeneity in human cancers. Ann NY Acad Sci. 2014;1319:47–65. doi: 10.1111/nyas.12469. [DOI] [PubMed] [Google Scholar]
- 28.Beury DW, Parker KH, Nyandjo M, Sinha P, Carter KA, Ostrand-Rosenberg S. Cross-talk among myeloid-derived suppressor cells, macrophages, and tumor cells impacts the inflammatory milieu of solid tumors. J Leukoc Biol. 2014;96(6):1109–1118. doi: 10.1189/jlb.3A0414-210R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mao Y, Sarhan D, Steven A, Seliger B, Kiessling R, Lundqvist A. Inhibition of tumor-derived prostaglandin-e2 blocks the induction of myeloid-derived suppressor cells and recovers natural killer cell activity. Clin Cancer Res. 2014;20(15):4096–4106. doi: 10.1158/1078-0432.CCR-14-0635. [DOI] [PubMed] [Google Scholar]
- 30.Schouppe E, Mommer C, Movahedi K, Laoui D, Morias Y, Gysemans C, Luyckx A, De Baetselier P, Van Ginderachter JA. Tumor-induced myeloid-derived suppressor cell subsets exert either inhibitory or stimulatory effects on distinct CD8+ T-cell activation events. Eur J Immunol. 2013;43(11):2930–2942. doi: 10.1002/eji.201343349. [DOI] [PubMed] [Google Scholar]
- 31.Mao Y, Poschke I, Wennerberg E, Pico de Coana Y, Egyhazi Brage S, Schultz I, Hansson J, Masucci G, Lundqvist A, Kiessling R. Melanoma-educated CD14+ cells acquire a myeloid-derived suppressor cell phenotype through COX-2-dependent mechanisms. Cancer Res. 2013;73(13):3877–3887. doi: 10.1158/0008-5472.CAN-12-4115. [DOI] [PubMed] [Google Scholar]
- 32.Nagaraj S, Nelson A, Youn JI, Cheng P, Quiceno D, Gabrilovich DI. Antigen-specific CD4(+) T cells regulate function of myeloid-derived suppressor cells in cancer via retrograde MHC class II signaling. Cancer Res. 2012;72(4):928–938. doi: 10.1158/0008-5472.CAN-11-2863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gorgun GT, Whitehill G, Anderson JL, Hideshima T, Maguire C, Laubach J, Raje N, Munshi NC, Richardson PG, Anderson KC. Tumor-promoting immune-suppressive myeloid-derived suppressor cells in the multiple myeloma microenvironment in humans. Blood. 2013;121(15):2975–2987. doi: 10.1182/blood-2012-08-448548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nagaraj S, Gabrilovich DI. Regulation of suppressive function of myeloid-derived suppressor cells by CD4+ T cells. Semin Cancer Biol. 2012;22(4):282–288. doi: 10.1016/j.semcancer.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Solito S, Bronte V, Mandruzzato S. Antigen specificity of immune suppression by myeloid-derived suppressor cells. J Leukoc Biol. 2011;90(1):31–36. doi: 10.1189/jlb.0111021. [DOI] [PubMed] [Google Scholar]
- 36.Movahedi K, Guilliams M, Van den Bossche J, Van den Bergh R, Gysemans C, Beschin A, De Baetselier P, Van Ginderachter JA. Identification of discrete tumor-induced myeloid-derived suppressor cell subpopulations with distinct T cell-suppressive activity. Blood. 2008;111(8):4233–4244. doi: 10.1182/blood-2007-07-099226. [DOI] [PubMed] [Google Scholar]
- 37.Virtuoso LP, Harden JL, Sotomayor P, Sigurdson WJ, Yoshimura F, Egilmez NK, Minev B, Kilinc MO. Characterization of iNOS(+) Neutrophil-like ring cell in tumor-bearing mice. J Transl Med. 2012;10:152. doi: 10.1186/1479-5876-10-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jayaraman P, Parikh F, Lopez-Rivera E, Hailemichael Y, Clark A, Ma G, Cannan D, Ramacher M, Kato M, Overwijk WW, Chen SH, Umansky VY, Sikora AG. Tumor-expressed inducible nitric oxide synthase controls induction of functional myeloid-derived suppressor cells through modulation of vascular endothelial growth factor release. J Immunol. 2012;188(11):5365–5376. doi: 10.4049/jimmunol.1103553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haverkamp JM, Crist SA, Elzey BD, Cimen C, Ratliff TL. In vivo suppressive function of myeloid-derived suppressor cells is limited to the inflammatory site. Eur J Immunol. 2011;41(3):749–759. doi: 10.1002/eji.201041069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang JR, Tsai YC, Chang YJ, Wu JC, Hung JT, Lin KH, Wong CH, Yu AL. alpha-Galactosylceramide but not phenyl-glycolipids induced NKT cell anergy and IL-33-mediated myeloid-derived suppressor cell accumulation via upregulation of egr2/3. J Immunol. 2014;192(4):1972–1981. doi: 10.4049/jimmunol.1302623. [DOI] [PubMed] [Google Scholar]
- 41.Poschke I, Mao Y, Adamson L, Salazar-Onfray F, Masucci G, Kiessling R. Myeloid-derived suppressor cells impair the quality of dendritic cell vaccines. Cancer Immunol Immunother. 2012;61(6):827–838. doi: 10.1007/s00262-011-1143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhou Z, French DL, Ma G, Eisenstein S, Chen Y, Divino CM, Keller G, Chen SH, Pan PY. Development and function of myeloid-derived suppressor cells generated from mouse embryonic and hematopoietic stem cells. Stem Cells. 2010;28(3):620–632. doi: 10.1002/stem.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cui TX, Kryczek I, Zhao L, Zhao E, Kuick R, Roh MH, Vatan L, Szeliga W, Mao Y, Thomas DG, Kotarski J, Tarkowski R, Wicha M, Cho K, Giordano T, Liu R, Zou W. Myeloid-derived suppressor cells enhance stemness of cancer cells by inducing microRNA101 and suppressing the corepressor CtBP2. Immunity. 2013;39(3):611–621. doi: 10.1016/j.immuni.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cunha LL, Morari EC, Guihen AC, Razolli D, Gerhard R, Nonogaki S, Soares FA, Vassallo J, Ward LS. Infiltration of a mixture of immune cells may be related to good prognosis in patients with differentiated thyroid carcinoma. Clin Endocrinol (Oxf) 2012;77(6):918–925. doi: 10.1111/j.1365-2265.2012.04482.x. [DOI] [PubMed] [Google Scholar]
- 45.Resheq YJ, Li KK, Ward ST, Wilhelm A, Garg A, Curbishley SM, Blahova M, Zimmermann HW, Jitschin R, Mougiakakos D, Mackensen A, Weston CJ, Adams DH. Contact-dependent depletion of hydrogen peroxide by catalase is a novel mechanism of myeloid-derived suppressor cell induction operating in human hepatic stellate cells. J Immunol. 2015;194(6):2578–2586. doi: 10.4049/jimmunol.1401046. [DOI] [PubMed] [Google Scholar]
- 46.Tarhini AA, Butterfield LH, Shuai Y, Gooding WE, Kalinski P, Kirkwood JM. Differing patterns of circulating regulatory T cells and myeloid-derived suppressor cells in metastatic melanoma patients receiving anti-CTLA4 antibody and interferon-alpha or TLR-9 agonist and GM-CSF with peptide vaccination. J Immunother. 2012;35(9):702–710. doi: 10.1097/CJI.0b013e318272569b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martin SF. Allergic contact dermatitis: xenoinflammation of the skin. Curr Opin Immunol. 2012;24(6):720–729. doi: 10.1016/j.coi.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 48.Bruchard M, Ghiringhelli F. Impact of chemotherapies on immunosuppression and discovery of new therapeutic targets. Bull Cancer. 2014;101(6):605–607. doi: 10.1684/bdc.2014.1936. [DOI] [PubMed] [Google Scholar]
- 49.Wu P, Wu D, Ni C, Ye J, Chen W, Hu G, Wang Z, Wang C, Zhang Z, Xia W, Chen Z, Wang K, Zhang T, Xu J, Han Y, Wu X, Wang J, Gong W, Zheng S, Qiu F, Yan J, Huang J. gammadeltaT17 cells promote the accumulation and expansion of myeloid-derived suppressor cells in human colorectal cancer. Immunity. 2014;40(5):785–800. doi: 10.1016/j.immuni.2014.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bruchard M, Mignot G, Derangere V, Chalmin F, Chevriaux A, Vegran F, Boireau W, Simon B, Ryffel B, Connat JL, Kanellopoulos J, Martin F, Rebe C, Apetoh L, Ghiringhelli F. Chemotherapy-triggered cathepsin B release in myeloid-derived suppressor cells activates the Nlrp3 inflammasome and promotes tumor growth. Nat Med. 2013;19(1):57–64. doi: 10.1038/nm.2999. [DOI] [PubMed] [Google Scholar]
- 51.Tartour E, Pere H, Maillere B, Terme M, Merillon N, Taieb J, Sandoval F, Quintin-Colonna F, Lacerda K, Karadimou A, Badoual C, Tedgui A, Fridman WH, Oudard S. Angiogenesis and immunity: a bidirectional link potentially relevant for the monitoring of antiangiogenic therapy and the development of novel therapeutic combination with immunotherapy. Cancer Metastasis Rev. 2011;30(1):83–95. doi: 10.1007/s10555-011-9281-4. [DOI] [PubMed] [Google Scholar]
- 52.Novitskiy SV, Pickup MW, Gorska AE, Owens P, Chytil A, Aakre M, Wu H, Shyr Y, Moses HL. TGF-beta receptor II loss promotes mammary carcinoma progression by Th17 dependent mechanisms. Cancer Discov. 2011;1(5):430–441. doi: 10.1158/2159-8290.CD-11-0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.