Abstract
Purpose
Earlier, the association of single nucleotide polymorphisms (SNPs) with toxicity and efficacy of sunitinib has been explored in patients with metastatic renal cell carcinoma (mRCC). Recently, additional SNPs have been suggested as potential biomarkers. We investigated these novel SNPs for association with sunitinib treatment outcome in mRCC patients.
Methods
In this exploratory study, we selected SNPs in genes CYP3A4, NR1I2, POR, IL8, IL13, IL4-R, HIF1A and MET that might possibly be associated with sunitinib treatment outcome. Each SNP was tested for association with progression-free survival (PFS) and overall survival (OS) by Cox-regression analysis and for clinical response and toxicity using logistic regression.
Results
We included 374 patients for toxicity analyses, of which 38 patients with non-clear cell renal cell cancer were excluded from efficacy analyses. The risk for hypertension was increased in the presence of the T allele in IL8 rs1126647 (OR = 1.69, 95 % CI = 1.07–2.67, P = 0.024). The T allele in IL13 rs1800925 was associated with an increase in the risk of leukopenia (OR = 6.76, 95 % CI = 1.35–33.9, P = 0.020) and increased prevalence of any toxicity > grade 2 (OR = 1.75, 95 % CI = 1.06–2.88, P = 0.028). No significant associations were found with PFS, OS or clinical response.
Conclusions
We show that polymorphisms in IL8 rs1126647 and IL13 rs1800925 are associated with sunitinib-induced toxicities. Validation in an independent cohort is required.
Electronic supplementary material
The online version of this article (doi:10.1007/s00228-015-1935-7) contains supplementary material, which is available to authorized users.
Keywords: Tyrosine kinase inhibitor, Sunitinib, Metastatic renal cell carcinoma, Single nucleotide polymorphism, Toxicity, Progression-free survival
Introduction
Several targeted therapies have been approved for the treatment of metastatic renal cell carcinoma (mRCC). Of these, the tyrosine kinase inhibitor (TKI) sunitinib is widely used as first-line treatment option [1–4]. The response to sunitinib varies largely among patients. Only 35 % of mRCC patients benefit from sunitinib, and about 30 % of patients need dose reductions due to adverse events of which grades vary among patients [1, 5, 6]. To optimize treatment efficacy and to minimize the risk of adverse events of higher grades, it would be helpful to predict the individual treatment outcome at the initiation of therapy. Unfortunately, no biomarkers are yet available to fulfil this need.
Several studies used a candidate gene approach to select single nucleotide polymorphisms (SNPs) in genes involved in the pharmacokinetics and pharmacodynamics of sunitinib. SNPs and haplotypes in CYP1A1, CYP3A5, ABCB1, ABCG2, NR1I3, VEGFA, NOS3 (=eNOS), FLT1 (=VEGFR1), KDR (=VEGFR2), FLT-4 (=VEGFR3) and FLT3 have been described to have an association with either toxicity or efficacy of sunitinib (P < 0.05) in mRCC patients [5–11]. The associations of CYP3A5 and ABCB1 with dose reductions and efficacy, respectively, have been confirmed recently [12]. Not all clinical outcomes can be explained by these potential biomarkers, which make identification of other markers possibly associated with clinical outcome an attractive prospect.
Novel SNPs in CYP3A4, NR1I2, POR, IL8, IL4-R, IL13, HIF1A and MET have been reported in patients with RCC, either prognostic or associated with treatment outcome, and might play a role in sunitinib treatment outcome (Table 1) [13–20]. In some studies on these novel SNPs, the TKI pazopanib was given to patients with mRCC. Sunitinib and pazopanib have similar efficacy and both are used as first-line treatment options [2]. Further, both drugs have similarities in their metabolic pathways and affected targets, because of which SNPs associated with pazopanib outcome might also be meaningful for the sunitinib treatment outcome, i.e. toxicity or efficacy [21]. The T allele of SNP rs35599367 in CYP3A4 (CYP3A4*22) was associated with decreased clearance of sunitinib [13–15]. The T allele of SNP rs3814055 in NR1I2 was associated with a reduction in response to pazopanib and inferior progression-free survival (PFS) from sunitinib and pazopanib in univariate analysis [6, 16]. The TT genotype of SNP rs1057858 in the P450 oxidoreductase gene (POR*28) was associated with higher CYP3A activity [17, 18]. Variant alleles of rs4073 and rs1126647 in IL8 were associated with an inferior PFS on pazopanib treatment [16]. SNPs rs1800925 and rs20541 in IL13 and rs180510 in IL4-R are likely to influence tumour immune response and carcinogenesis [19]. The AG genotype of rs11549467 in HIF1A compared to wild-type GG was associated with a decreased PFS and a reduced response rate on pazopanib treatment [16]. The A-allele of SNP rs11762213 in MET was associated with an increased risk of recurrence or death in RCC patients [20].
Table 1.
Polymorphisms in candidate genes in the current study. Genetic polymorphisms were included if in previous exploratory studies associations were reported with a P value <0.05
| Gene | SNP | Reported results | References |
|---|---|---|---|
| CYP3A4 | rs35599367C>T | CYP3A4*22 is associated with decreased CYP3A4 expression and decreased clearance of sunitinib. | Elens et al. [13, 14] Diekstra et al. [15] |
| NR1I2 | rs3814055C>T | T allele is associated with reduction of response to pazopanib and inferior PFS on sunitinib and pazopanib. | van der Veldt et al. [6] Xu et al. [16] |
| POR*28 | rs1057868C>T | POR*28 is associated with higher in vivo CYP3A activity. | de Jonge et al. [17] Oneda et al. [18] |
| IL8 | rs4073T>A | AA shows inferior PFS of pazopanib compared to wild-type TT. | Xu et al. [16] |
| rs1126647A>T | TT shows inferior PFS of pazopanib compared to wild-type AA. | Xu et al. [16] | |
| Correlated SNPs rs4073T>A and rs1126647A>T | Inferior PFS for variant genotypes (r4073 AA + rs1126647 TT) compared to wild types (rs4073 TT + rs1126647 AA) | Xu et al. [16] | |
| HIF1A | rs11549467G>A | AG genotype is associated with inferior PFS and reduced response rate of pazopanib compared to wild-type GG. | Xu et al. [16] |
| IL4-R | rs1805010T>C | CT/TT genotype is associated with decreased risk of RCC compared to CC genotype. | Chu et al. [19] |
| IL13 | rs1800925C>T | TT genotype is associated with decreased risk of RCC. | Chu et al. [19] |
| rs20541C>T | |||
| MET | rs11762213G>A | A-allele is associated with an increased risk of recurrence or death. | Schutz et al. [20] |
SNP single nucleotide polymorphism, PFS progression-free survival, OS overall survival
In this exploratory study, we evaluated the polymorphisms in the above-mentioned genes for possible associations with toxicity or efficacy of sunitinib in a large cohort of mRCC patients.
Methods
Study population
Patient data were collected from three exploratory studies (SUTOX, SOGUG and CCF) between the years 2004 and 2010 (Supplementary document 1) [12]. SUTOX samples were anonymized by a third party, according to the instructions stated in the Codes for Proper Use and Proper Conduct in the Self-Regulatory Codes of Conduct (www.federa.org). The study was conducted in accordance with the Declaration of Helsinki and approved by the medical ethics review board of all participating groups. Patients provided their written informed consent for participation [12].
Study endpoints
PFS, defined as the time in months between the first day of sunitinib treatment and the date of progressive disease (PD) according to Response Evaluation Criteria in Solid Tumours (RECIST) v.1.0 or v1.1, was used as the primary endpoint to assess efficacy. Another endpoint was overall survival (OS), which was measured from the first day of sunitinib treatment until death or time of last follow-up.
We classified objective clinical response into three categories: (i) partial and complete response, (ii) stable disease and (iii) progressive disease (according to RECIST).
Specific sunitinib-related adverse events, i.e. thrombocytopenia, leukopenia, mucosal inflammation, hand-foot syndrome, hypertension and any toxicity > grade 2, were collected for this study (Supplementary document 1) [12].
Statistical analysis
For univariate analysis, a log-rank test was used for the association of each SNP with PFS and OS, and a chi-square test for clinical response and toxicity. SNPs with a P value <0.1 were included in the multivariate model. Based on previous results, we included well-established covariates age, gender and Heng prognostic risk group in the multivariate model for correction of PFS and OS [22]. In addition, the CGT haplotype of ABCB1 was also used as covariate in multivariate Cox model because of the previously confirmed significant association with PFS [6, 12]. For multivariate analysis of clinical response, we also included age, gender and Heng prognostic risk group as covariates. For multivariate analysis on toxicity endpoints, no biomarker was widely validated, so we corrected for age and gender. Because this association study used data from three study groups (SUTOX, SOGUG and CCF), study group was also tested as a covariate for all endpoints. It was not needed to correct for previous treatment in efficacy analyses, because this was already justified by using study group as a covariate.
Reported results from the multivariate analysis with a P value <0.05 were considered clinically significant. All tests were two-sided and carried out by SPSS Statistical Package for Windows (version 20.0 Armonk, NY: IBM Corp).
Results
Patient characteristics
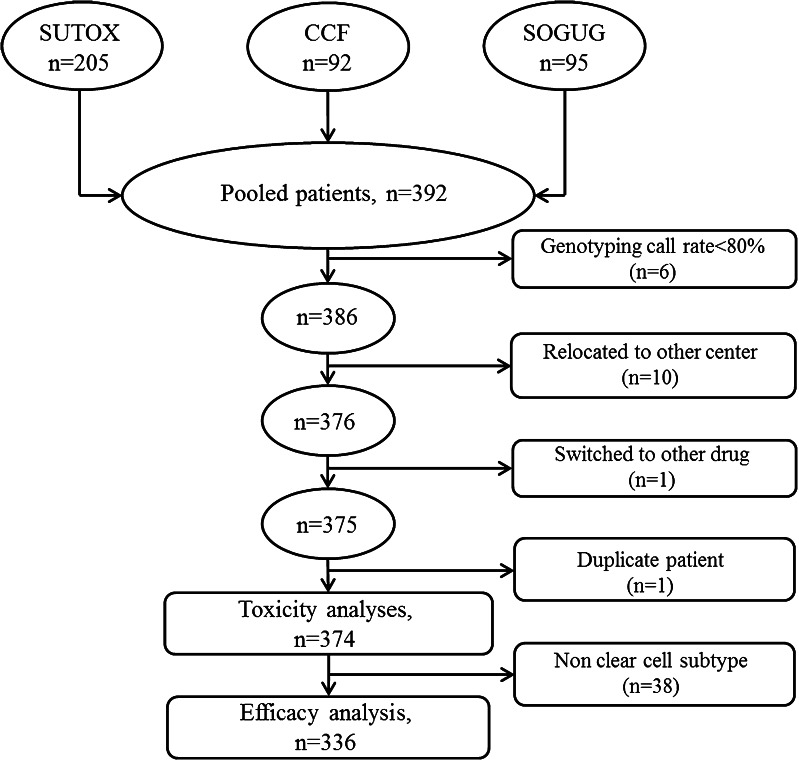
A total of 374 patients with mRCC treated with sunitinib were included for association analyses on toxicity endpoints. For efficacy analyses, only clear cell subtypes (N = 336) were included (Fig. 1). Patient characteristics are presented in Table 2. Median age of patients was 61 years, and most were men of Caucasian ethnicity. The majority of patients had undergone nephrectomy. For the clear cell subjects, the good or intermediate Heng prognostic risk group consisted of 73 % of the patients. Forty-five percent (N = 143) of patients showed a partial response (PR) or complete response (CR) to sunitinib.
Fig. 1.
Patient flowchart on included patients. Fifty-six patients had to be excluded from association analyses because of individual genotyping call rates <80 % (N = 6), relocation to another medical center during follow-up (N = 10), double patient (N = 1), a change to another treatment than sunitinib directly after enrolment (N = 1) or non-clear cell subtypes (N = 38). A total of 374 sunitinib-treated clear cell mRCC patients were available for analysis of toxicity in the present study. For efficacy analysis, 336 sunitinib-treated clear cell mRCC patients were available [12]
Table 2.
Patient characteristics
| Characteristic | Efficacy cohort (N = 336) |
Toxicity cohort (N = 374) |
|---|---|---|
| Age | ||
| Median | 61 | 61 |
| Percentiles (25th, 75th) | 55, 69 | 54, 68 |
| BSA | ||
| Median | 1.98 | 1.96 |
| Percentiles (25th, 75th) | 1.82, 2.13 | 1.82, 2.12 |
| Race | ||
| White | 324 (96 %) | 358 (96 %) |
| Asian | 3 (0.89 %) | 3 (0.80 %) |
| Black | 5 (1.5 %) | 8 (2.1 %) |
| Arabian | 3 (0.89 %) | 4 (1.0 %) |
| Latin American | 1 (0.30 %) | 1 (0.27 %) |
| Gender | ||
| Male | 229 (68 %) | 258 (69 %) |
| Female | 107 (32 %) | 116 (31 %) |
| Clinical response | ||
| PR + CR | 143 (43 %) | 149 (40 %) |
| SD | 130 (39 %) | 149 (40 %) |
| PD | 43 (13 %) | 55 (15 %) |
| Unknown | 20 (6.0 %) | 21 (5.6 %) |
| Heng prognostic risk groupa | ||
| Good (0 risk factor) | 64 (19 %) | 68 (18 %) |
| Intermediate (1–2 risk factors) | 182 (54 %) | 197 (53 %) |
| Poor (3–6 risk factors) | 90 (27 %) | 108 (29 %) |
| Metastatic sites | ||
| 1 | 91 (27 %) | 105 (28 %) |
| 2 | 137 (41 %) | 149 (40 %) |
| ≥3 | 104 (31 %) | 116 (31 %) |
| Prior nephrectomy | ||
| No | 49 (15 %) | 63 (17 %) |
| Yes | 283 (85 %) | 307 (82 %) |
| Prior treatment | ||
| No | 254 (76 %) | 276 (74 %) |
| Yes | 82 (24 %) | 98 (26 %) |
BSA body surface area, CR complete response, PR partial response, SD stable disease, PD progressive disease
aPatients are classified according to the six Heng risk criteria: poor WHO performance status (≥2), low haemoglobin (<lower limit of normal), high calcium (>upper limit of normal) and time from initial diagnosis to treatment with sunitinib (<1 year), neutrophil count (>upper limit of normal) and thrombocytes (>upper limit of normal)
95.7 to 99.5 % of patients had no toxicities at baseline. Within four cycles of sunitinib treatment, any grade of thrombocytopenia was observed in 61 % of patients, mucosal inflammation in 59 %, leukopenia in 49 %, hand-foot syndrome in 41 % and hypertension in 38 %. Twenty-six percent of patients developed any toxicity > grade 2 (Supplementary Table S1).
For clear cell subtypes, median follow-up times for PFS and OS analysis were 43 and 49 months, respectively. Median PFS and OS of patients were 16 and 26 months, respectively.
Genotyping
IL8 rs4073 was excluded from statistical analysis because the call rate was less than 95 %. The SNP genotype call rate for the remaining SNPs ranged from 97.6 to 99.7 %. All SNPs were in Hardy-Weinberg equilibrium (HWE) (P > 0.05 and χ2 < 3.84). The allele frequencies of genotyped polymorphisms were similar as reported in the National Center for Biotechnology Information (NCBI) SNP database [23]. Only three patients with the HIF1A rs11549467 heterozygous genotype were detected. As a consequence, the effects of this SNP could not be analysed.
Genetic association analysis
No significant associations between SNPs and PFS, OS or objective response to sunitinib were observed in this study. Although not significant, A-allele carriers of MET rs11762213 had a better PFS compared to wild-type GG (HR = 0.63, 95 % CI = 0.38–1.05, P = 0.076), adjusted for age, gender, Heng prognostic risk group, study group and CGT haplotype in ABCB1 (Table 3).
Table 3.
Univariate and multivariate analyses for SNPs associated with sunitinib treatment outcome
| Treatment outcome | Number of patients | Univariate analyses | Multivariate analyses | ||||
|---|---|---|---|---|---|---|---|
| HR or OR | 95 % CI | P value | HR or OR | 95 % CI | P value | ||
| PFS | |||||||
| MET rs11762213 G>A | 0.58 | 0.36–0.96 | 0.032 | 0.63 | 0.38–1.05 | 0.076a | |
| GG versus | 302 | ||||||
| AG+AA | 33 | ||||||
| Hypertension | |||||||
| IL8 rs1126647 A>T | 1.70 | 1.08–2.68 | 0.022 | 1.69 | 1.07–2.67 | 0.024b | |
| AA versus | 128 | ||||||
| AT versus | 174 | ||||||
| TT | 61 | ||||||
| Thrombocytopenia | |||||||
| IL13 rs20541 C>T | 1.97 | 0.90–4.35 | 0.092 | 1.87 | 0.82–4.23 | 0.136b | |
| CC versus | 235 | ||||||
| CT+TT | 117 | ||||||
| Leukopenia | |||||||
| IL13 rs1800925 C>T | 6.13 | 1.25–30.0 | 0.025 | 6.76 | 1.35–33.9 | 0.020b | |
| CC versus | 232 | ||||||
| CT+TT | 137 | ||||||
| Any toxicity > grade 2 | |||||||
| IL13 rs1800925 C>T | 1.91 | 1.15–3.15 | 0.012 | 1.75 | 1.06–2.88 | 0.028b | |
| CC versus | 234 | ||||||
| CT+TT | 137 | ||||||
HR hazard ratio, OR odds ratio, CI confidence interval, PFS progression-free survival
aAdjusted by age, gender, Heng prognostic risk group, study center and ABCB1 haplotype
bAdjusted by age, gender and study center
In multivariate toxicity analysis, the T allele of IL8 rs1126647 was associated with an increased risk of hypertension compared to wild-type AA (OR = 1.69, 95 % CI = 1.07–2.67, P = 0.024) after adjustment by age, gender and study group. Presence of the IL13 rs1800925 T allele was associated with an increased risk of leukopenia (OR = 6.76, 95 % CI = 1.35–33.9, P = 0.020) and also with development of any toxicity > grade 2 (OR = 1.75, 95 % CI = 1.06–2.88, P = 0.028) (Table 3).
Discussion
In the present study, we analysed eight candidate SNPs in seven genes for potential association with response and/or toxicity of sunitinib in a large cohort of mRCC patients. To our knowledge, we report for the first time that genetic polymorphisms in interleukin genes IL8 and IL13 are associated with the occurrence of clinically relevant adverse events from sunitinib. Patients carrying a T allele of IL8 rs1126647 had an increased risk of hypertension compared to wild-type AA (OR = 1.69). T carriers of IL13 rs1800925 had an increased risk of leukopenia (OR = 6.76) and an increased risk of any toxicity > grade 2 (OR = 1.75).
Hypertension is a frequent toxicity caused by TKIs. The potential mechanism is suggested to be related to inhibition of VEGFR-2 and decrease of nitric oxide, resulting in vasoconstriction and elevated blood pressure [8, 24]. It has been recognized that IL8, possibly by upregulating VEGF levels through NFkappaB [25, 26], can play a role in stimulating VEGFR-2 transactivation. In our data, presence of the variant allele in IL8 rs1126647A>T is significantly associated with hypertension. IL8 rs1126647A>T is in linkage with IL8 rs4073T>A (r2 = 0.78) [16]. It was shown that a haplotype of IL8, including the variant allele of rs4073T>A and rs1126647A>T, was associated with increased IL8 expression [27]. In contrast, Amaya et al. [28] have reported that the variant allele of rs4073 was associated with a lower production of IL8. It remains to be elucidated whether particular SNPs in IL8 have prognostic or even predictive significance in metastatic renal cell carcinoma.
The occurrence of hypertension is a well-known predictor for increased survival in metastatic renal cell carcinoma treated with a TKI [29]. In addition to an increased occurrence of hypertension, patients with the variant allele in IL8 rs1126647A>T showed a trend towards improved PFS/OS (22 vs 14 months for median PFS and 40 vs 25 months for median OS), although the differences between groups did not reach statistical significance. One possible reason for the lack of statistical significance in the above association may be the ∼2 fold larger (n = 544) sample size of the study from Rini et al. [29]. Xu et al. [16] described an inferior PFS of pazopanib for carriers of the variant allele of IL8 rs1126647A>T. In a follow-up study, Xu et al. [30] reported that the variant allele of IL8 rs1126647A>T was significantly associated with worse OS in mRCC patients treated with pazopanib or sunitinib, but could not confirm the initial association with PFS. Unfortunately, Xu et al. do not report data on associations between IL8 rs1126647 and hypertension. In addition, many factors can have an impact on OS, including baseline conditions and previous and posterior treatments. Therefore, it is not possible to directly compare the association of IL8 rs1126647 and hypertension/survival between the two datasets and further study in an independent cohort is required.
We observed an increased risk of leukopenia in carriers of the variant allele of IL13 rs1800925C>T. Leukopenia is a common haematologic adverse event in sunitinib treatment of which the mechanism remains uncertain. It was reported that VEGF and its receptors (VEGFR) are essential for development of aberrant haematopoiesis, including leukopenia [31]. Shen et al. [32] have reported that VEGFR-2 can be upregulated by IL13. The T allele of IL13 rs1800925 has been found to be associated with increased IL13 protein function [33].
Little is known about the effects of SNPs in IL8 and IL13, but it is likely that these SNPs will either increase or decrease the protein expression of IL8 and IL13 proteins [24–26, 29, 31–34]. It also remains unclear whether the function of these interleukins will affect TKI treatment outcome and if and how these interleukin proteins would influence the VEGF(R) pathway directly or indirectly [25–28, 30–36]. Xu et al. [30] speculate that patients with the IL8 variants having a high IL8 expression may have more aggressive tumours, and therefore a reduced survival. However, it is difficult to hypothesize because we noticed conflicting results: Hacking et al. [27] reported increased expression for IL8 variants, while a more recent paper of Amaya et al. [28] reported the opposite effect on IL8 expression. If variant alleles in IL8 and IL13 SNPs alter protein expression and have an effect on VEGF-R2, a stronger inhibition of VEGF-R2 in the concomitant presence of sunitinib would explain our results on a higher risk for any toxicity, including hypertension and leukopenia.
HIF1A protein regulates the transcription of a large number of genes that respond to hypoxia, among which is angiogenesis. The A-allele frequency of HIF1A rs11549467 in our cohort was 0.45 %, which is lower than that (A = 3.0 %) reported by Xu et al. [16], but corresponds with the result (A = 0.6 %) from Beuselinck et al. [10]. The difference in A-allele frequency is potentially caused by the subject selection. Of note, the subjects recruited here and in the study of Beuselinck typically have Western European ancestry, whereas the patients in Xu’s study are mostly from Eastern Europe [10, 16].
This study was conducted in a relatively large cohort, which decreases the chance for false-positive findings. In addition to Xu et al. [30], we have tested on toxicity as well as efficacy endpoints, which is essential for clinical interpretation. SNPs could influence the drug exposure to the TKI and consequently have an effect on both adverse events, PFS and OS. Because this study only presents explorative findings without external validation, and our results are based on mainly Caucasian subjects, extrapolation to the entire mRCC population is difficult.
To capture adverse events that occur later on in treatment, all toxicity outcomes were recorded and evaluated up to four cycles of sunitinib treatment. In our cohort, hypertension and fatigue have a large contribution in the endpoint any toxicity > grade 2. Because it is difficult to evaluate fatigue objectively, we did not test fatigue as separate toxicity endpoint. Since our study represents data collected from 2004 to 2010, it is likely that clinical practice (i.e. toxicity management) has evolved in the course of time. In earlier years with limited experience on sunitinib treatment, dose reductions were applied in the case of grade 3 or 4 toxicities. Nowadays, physicians anticipate on the development of severe adverse events by already reducing the dose on the occurrence of grade 2 toxicity. However, we did not observe a difference in dose reductions between earlier years and later years (data not shown). Further, our dataset lacks sufficiently detailed information on the reasons and time points of dose reductions.
Our SNP selection was based on reported associations with toxicity and efficacy outcomes on treatment and the risk of developing RCC. SNPs are often categorized as being either predictive or prognostic biomarkers. However, this distinction may not have to be as rigorous as we currently assume. In fact, prediction and prognosis may be strongly correlated. Antitumour treatment can have a different effect in patients with a more aggressive tumour type that is possibly caused by an underlying SNP. For example, high IL8 protein levels in RCC are considered to have a poor prognosis [35]. However, elevated IL8 levels investigated in preclinical models resulted in resistance to sunitinib, which would be considered predictive [36]. Functional studies on immunological and angiogenic factors and a genome-wide approach can help us in understanding the mechanisms on the predictive or prognostic character of the SNPs.
In conclusion, this study suggests a relationship between interleukin genes IL8 and IL13 and the development of sunitinib-induced adverse events. Further validation in an independent cohort is warranted to confirm our findings. In addition, we consider functional studies on IL8 and IL13, with respect to regulation of VEGF(R) genes and sVEGF(R) plasma levels, to be crucial for our understanding of the mechanisms involved in sunitinib exposure and occurrence of adverse events.
Electronic supplementary material
(DOC 36 kb)
(DOCX 15 kb)
Acknowledgments
We thank Dr. Tahar van der Straaten and Renée Baak-Pablo for their assistance with data management and genotyping.
Contributions of authors
Study concept and design: Rini, Garcia-Donas, Guchelaar
Acquisition of data: Diekstra, Swen, Boven, Castellano, Gelderblom, Mathijssen, Rodriguez-Antona, Garcia-Donas, Rini, Guchelaar
Analysis and interpretation of data: Diekstra, Liu, Swen, Rini, Garcia-Donas, Rodriguez-Antona, Gelderblom, Guchelaar
Drafting of the manuscript: Diekstra, Liu, Swen, Boven, Castellano, Gelder- blom, Mathijssen, Rodriguez-Antona, Garcia-Donas, Rini, Guchelaar
Critical revision of the manuscript: Diekstra, Swen, Boven, Castellano, Gelderblom, Mathijssen, Rodríguez- Antona, García-Donas, Rini, Guchelaar
Statistical analysis: Diekstra, Liu, Swen, Rini, Garcia-Donas, Rodríguez- Antona, Gelderblom, Guchelaar.
Administrative, technical or material support: Diekstra, Swen, Boven, Castellano, Gelderblom, Mathijssen, Rodríguez-Antona, García-Donas, Rini, Guchelaar
Supervision: Guchelaar
Funding
Pfizer supports this research. The European Union’s Seventh Framework Programme (FP7/2007–2013) supports Meta Diekstra under grant agreement no. 259939. Xiaoyan Liu is supported by the Chinese Scholarship Council under grant agreement no. [2014]3026.
Conflict of interest
Dr. Brian Rini and Dr. Garcia-Donas report consulting and research funding from Pfizer. The other authors declared no conflicts of interest.
Footnotes
Meta H. M. Diekstra and Xiaoyan Liu contributed equally to this work.
References
- 1.Motzer RJ, Rini BI, Bukowski RM, et al. Sunitinib in patients with metastatic renal cell carcinoma. JAMA. 2006;295:2516–2524. doi: 10.1001/jama.295.21.2516. [DOI] [PubMed] [Google Scholar]
- 2.Motzer RJ, Hutson TE, Cella D, et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med. 2013;369:722–731. doi: 10.1056/NEJMoa1303989. [DOI] [PubMed] [Google Scholar]
- 3.Shibata SI, Chung V, Synold TW, et al. Phase I study of pazopanib in patients with advanced solid tumors and hepatic dysfunction: a National Cancer Institute Organ Dysfunction Working Group study. Clin Cancer Res. 2013;19:3631–3639. doi: 10.1158/1078-0432.CCR-12-3214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Houk BE, Bello CL, Kang D, Amantea M. A population pharmacokinetic meta-analysis of sunitinib malate (SU11248) and its primary metabolite (SU12662) in healthy volunteers and oncology patients. Clin Cancer Res. 2009;15:2497–2506. doi: 10.1158/1078-0432.CCR-08-1893. [DOI] [PubMed] [Google Scholar]
- 5.van Erp NP, Eechoute K, van der Veldt AA, et al. Pharmacogenetic pathway analysis for determination of sunitinib-induced toxicity. J Clin Oncol. 2009;27:4406–4412. doi: 10.1200/JCO.2008.21.7679. [DOI] [PubMed] [Google Scholar]
- 6.van der Veldt AA, Eechoute K, Gelderblom H, et al. Genetic polymorphisms associated with a prolonged progression-free survival in patients with metastatic renal cell cancer treated with sunitinib. Clin Cancer Res. 2011;17:620–629. doi: 10.1158/1078-0432.CCR-10-1828. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Donas J, Esteban E, Leandro-García LJ, et al. Single nucleotide polymorphism associations with response and toxic effects in patients with advanced renal-cell carcinoma treated with first-line sunitinib: a multicentre, observational, prospective study. Lancet Oncol. 2011;12:1143–1150. doi: 10.1016/S1470-2045(11)70266-2. [DOI] [PubMed] [Google Scholar]
- 8.Eechoute K, van der Veldt AA, Oosting S, et al. Polymorphisms in endothelial nitric oxide synthase (eNOS) and vascular endothelial growth factor (VEGF) predict sunitinib-induced hypertension. Clin Pharmacol Ther. 2012;92:503–510. doi: 10.1038/clpt.2012.136. [DOI] [PubMed] [Google Scholar]
- 9.Kim JJ, Vaziri SA, Rini BI, et al. Association of VEGF and VEGFR2 single nucleotide polymorphisms with hypertension and clinical outcome in metastatic clear cell renal cell carcinoma patients treated with sunitinib. Cancer. 2010;118:1946–1954. doi: 10.1002/cncr.26491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beuselinck B, Karadimou A, Lambrechts D, et al. Single-nucleotide polymorphisms associated with outcome in metastatic renal cell carcinoma treated with sunitinib. Br J Cancer. 2013;108:887–900. doi: 10.1038/bjc.2012.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beuselinck B, Karadimou A, Lambrechts D, et al. VEGFR1 single nucleotide polymorphisms associated with outcome in patients with metastatic renal cell carcinoma treated with sunitinib—a multicentric retrospective analysis. Acta Oncol. 2014;53:103–112. doi: 10.3109/0284186X.2013.770600. [DOI] [PubMed] [Google Scholar]
- 12.Diekstra MH, Swen JJ, Boven E et al (2015) CYP3A5 and ABCB1 polymorphisms as predictors for sunitinib outcome in metastatic renal cell carcinoma. Eur Urol 68:621–629 [DOI] [PubMed]
- 13.Elens L, Bouamar R, Hesselink DA, et al. A new functional CYP3A4 intron 6 polymorphism significantly affects tacrolimus pharmacokinetics in kidney transplant recipients. Clin Chem. 2011;57:1574–1583. doi: 10.1373/clinchem.2011.165613. [DOI] [PubMed] [Google Scholar]
- 14.Elens L, van Gelder T, Hesselink DA, et al. CYP3A4*22: promising newly identified CYP3A4 variant allele for personalizing pharmacotherapy. Pharmacogenomics. 2013;14:47–62. doi: 10.2217/pgs.12.187. [DOI] [PubMed] [Google Scholar]
- 15.Diekstra MH, Klümpen HJ, Lolkema MP, et al. Association analysis of genetic polymorphisms in genes related to sunitinib pharmacokinetics, specifically clearance of sunitinib and SU12662. Clin Pharmacol Ther. 2014;96:81–89. doi: 10.1038/clpt.2014.47. [DOI] [PubMed] [Google Scholar]
- 16.Xu CF, Bing NX, Ball HA, et al. Pazopanib efficacy in renal cell carcinoma: evidence for predictive genetic markers in angiogenesis-related and exposure-related genes. J Clin Oncol. 2011;29:2557–2564. doi: 10.1200/JCO.2010.32.9110. [DOI] [PubMed] [Google Scholar]
- 17.De Jonge H, Metalidis C, Naesens M, et al. The P450 oxidoreductase *28 SNP is associated with low initial tacrolimus exposure and increased dose requirements in CYP3A5-expressing renal recipients. Pharmacogenomics. 2011;12:1281–1291. doi: 10.2217/pgs.11.77. [DOI] [PubMed] [Google Scholar]
- 18.Oneda B, Crettol S, Jaquenoud Sirot E, et al. The P450 oxidoreductase genotype is associated with CYP3A activity in vivo as measured by the midazolam phenotyping test. Pharmacogenet Genomics. 2009;19:877–883. doi: 10.1097/FPC.0b013e32833225e7. [DOI] [PubMed] [Google Scholar]
- 19.Chu H, Wang M, Yan F, et al. Polymorphisms in the IL13 and IL-4R genes are associated with the development of renal cell carcinoma. Ann Oncol. 2012;23:2114–2121. doi: 10.1093/annonc/mdr607. [DOI] [PubMed] [Google Scholar]
- 20.Schutz FA, Pomerantz MM, Gray KP, et al. Single nucleotide polymorphisms and risk of recurrence of renal-cell carcinoma: a cohort study. Lancet Oncol. 2013;14:81–87. doi: 10.1016/S1470-2045(12)70517-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar R, Crouthamel MC, Rominger DH, et al. Myelosuppression and kinase selectivity of multikinase angiogenesis inhibitors. Br J Cancer. 2009;101:1717–1723. doi: 10.1038/sj.bjc.6605366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heng D, Xie W, Regan M, et al. Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor-targeted agents: results from a large, multicenter study. J Clin Oncol. 2009;27:5794–5799. doi: 10.1200/JCO.2008.21.4809. [DOI] [PubMed] [Google Scholar]
- 23.Sherry ST, Ward MH, Kholodov M et al (2001) National Center for Biotechnology Information (NCBI) SNP database: the NCBI database of genetic variation. Nucleic Acids Res 29:308–311. Available from URL: http://www.ncbi.nlm.nih.gov/snp/ [DOI] [PMC free article] [PubMed]
- 24.Lankhorst S, Kappers M, van Esch J, et al. Hypertension during vascular endothelial growth factor inhibition: focus on nitric oxide, endothelin-1, and oxidative stress. Antioxid Redox Signal. 2014;20:135–145. doi: 10.1089/ars.2013.5244. [DOI] [PubMed] [Google Scholar]
- 25.Petreaca ML, Yao M, Liu Y, et al. Transactivation of vascular endothelial growth factor receptor-2 by interleukin-8 (IL8/CXCL8) is required for IL8/CXCL8-induced endothelial permeability. Mol Biol Cell. 2007;18:5014–5023. doi: 10.1091/mbc.E07-01-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin D, Galisteo R, Gutkind JS. CXCL8/IL8 stimulates vascular endothelial growth factor (VEGF) expression and the autocrine activation of VEGFR2 in endothelial cells by activating NFkappaB through the CBM (Carma3/Bcl10/Malt1) Complex. J Biol Chem. 2009;284:6038–6042. doi: 10.1074/jbc.C800207200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hacking D, Knight JC, Rockett K, et al. Increased in vivo transcription of an IL8 haplotype associated with respiratory syncytial virus disease susceptibility. Genes Immun. 2004;5:274–282. doi: 10.1038/sj.gene.6364067. [DOI] [PubMed] [Google Scholar]
- 28.Amaya MP, Criado L, Blanco B, et al. Polymorphisms of pro-inflammatory cytokine genes and the risk for acute suppurative or chronic nonsuppurative apical periodontitis in a Colombian population. Int Endod J. 2013;46:71–78. doi: 10.1111/j.1365-2591.2012.02097.x. [DOI] [PubMed] [Google Scholar]
- 29.Rini BI, Cohen DP, Lu DR, et al. Hypertension as a biomarker of efficacy in patients with metastatic renal cell carcinoma treated with sunitinib. J Natl Cancer Inst. 2011;103:763–773. doi: 10.1093/jnci/djr128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu CF, Johnson T, Garcia-Donas J, et al. IL8 polymorphisms and overall survival in pazopanib- or sunitinib-treated patients with renal cell carcinoma. Br J Cancer. 2015;112:1190–1198. doi: 10.1038/bjc.2015.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang Y, Chen X, Dikov MM, et al. Distinct of VEGFR-1 and VEGFR-2 in the aberrant hematopoiesis associated with elevated levels of VEGF. Blood. 2007;110:624–631. doi: 10.1182/blood-2007-01-065714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shen R, Ye Y, Chen L, et al. Precancerous stem cells can serve as tumor vasculogenic progenitors. PLoS One. 2008;3 doi: 10.1371/journal.pone.0001652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van der Pouw Kraan TC, van Veen A, Boeije LC, et al. An IL13 promoter polymorphism associated with increased risk of allergic asthma. Genes Immun. 1999;1:61–65. doi: 10.1038/sj.gene.6363630. [DOI] [PubMed] [Google Scholar]
- 34.Tran HT, Liu Y, Zurita AJ, et al. Prognostic or predictive plasma cytokines and angiogenic factors for patients treated with pazopanib for metastatic renal-cell cancer: a retrospective analysis of phase 2 and phase 3 trials. Lancet Oncol. 2012;13:827–837. doi: 10.1016/S1470-2045(12)70241-3. [DOI] [PubMed] [Google Scholar]
- 35.Harmon CS, DePrimo SE, Figlin RA, et al. Circulating proteins as potential biomarkers of sunitinib and interferon-α efficacy in treatment-naïve patients with metastatic renal cell carcinoma. Cancer Chemother Pharmacol. 2014;73:151–161. doi: 10.1007/s00280-013-2333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Huang D, Ding Y, Zhou M, et al. Interleukin-8 mediates resistance to antiangiogenic agent sunitinib in renal cell carcinoma. Cancer Res. 2010;70:1063–1071. doi: 10.1158/0008-5472.CAN-09-3965. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC 36 kb)
(DOCX 15 kb)