Abstract
Leveraging technology to enhance antiretroviral therapy (ART) adherence, and factors associated with it, has tremendous appeal as a low-cost, generalizable strategy to offer high-quality adherence support given an increasingly limited workforce. As the numbers of individuals living with HIV entering care and initiating ART are expected to increase substantially worldwide in the next decade, capacity to support ART adherence is needed and use of computers, internet and mobile phones has the potential to offer those efficiencies--providing they are effective. This review summarizes recent advances in the evidence base for technology-driven, -delivered or -enhanced ART adherence intervention approaches. A Pubmed search limited to January 2013 through July 2015 identified 13 qualifying studies evaluating computer-delivered interventions, internet approaches, mobile phone technologies, and electronic dose monitoring with triggered messaging and data-informed counseling. Considerable support for each area has emerged, with the majority of studies reviewed demonstrating significant effects on ART adherence and clinical outcomes. Gaps are identified and recommendations offered.
Keywords: ART adherence, intervention, technology, review, synthesis
Introduction
Advances in technology-driven and -delivered interventions to promote antiretroviral therapy (ART) adherence for adults living with HIV continue to evolve. Dominated by cell phone, text-messaging and computer delivered intervention in previous years [1], the evidence base has expanded to include a number of research syntheses and additional intervention studies. The drive to find intervention modalities that leverage near ubiquitous use of mobile-phones and increasing access to the internet are still dominant themes in the available literature, however the last several years has witnessed an increasingly nuanced understanding of the kinds of technology that may be most acceptable and effective to populations in need. As countries ready for aggressive new targets for controlling the HIV epidemic [2], strategies to engage people living with HIV in settings with a limited workforce to do so are of high interest and potential impact. Mobile technologies offer the potential to remain “connected” with patients in ways previously unimagined. The HIV population is increasingly diverse, with an aging population of individuals living longer lives with HIV and a “youth bulge” in endemic areas that will increase the size of adolescents and young adults living with HIV. While younger adults would be likely to expect the leveraging of well-known technologies (such as texting or other apps offering nearly constant contact), increasingly it appears that older adults are open and eager to utilize technology to assist with their self-care [3].
Recent meta-analytic reviews of text-messaging for ART adherence promotion have suggested that these interventions have a significant effect in comparison to control conditions. Finitis and colleagues' [4] review of 9 separate interventions showed overall significant intervention effects on ART adherence, with greater effects observed when messages were sent less frequently than daily, were bidirectional, and used personalized messages. Similar findings were reported in another innovative meta-analysis that combined individual-level data from 2 randomized controlled trials (RCTs) in Kenya and 1 in Cameroon resulting in a total of 1166 participants.[5] The pooled analysis found a significant intervention effect on adherence, with effects significantly better for those with a higher education and female gender of participant, and when messages were sent weekly rather than daily and had interactive components. Expanded to health care in general, an analysis of 60 studies (15% with HIV positive participants) summarized that 77% reported positive or improved health outcomes, although high variable in response rates were noted.[6] It bears noting that one recent review of use of mobile health technologies for HIV self-management among African American women in the US found no studies met criteria, calling for added efforts to focus on key populations.[7] Mathes and colleagues' systematic review and meta-analysis on adherence interventions in sub-Saharan Africa only identified 6 studies, of which half used SMS.[8] A significant effect on adherence was noted among SMS studies.
The current brief review focuses on the recent (January 2013- June 2015) evidence base for adherence-promoting interventions that utilize technology with adults (extended to young adults aged 20) living with HIV. The intent is to update readers on recent advances and call attention to the considerable volume of work in this area since the last evidence base summary on technology delivered ART interventions was compiled [1]. The evidence base is expressly defined here as the “forward-facing” literature, specifically the evidence that would be readily available to researchers and service provides through a Pubmed search using a combination of common terms.
Main findings, themes and gaps interventions evaluated in this evidence base are provided.
Methods
Literature Search Methods and Criteria for Inclusion
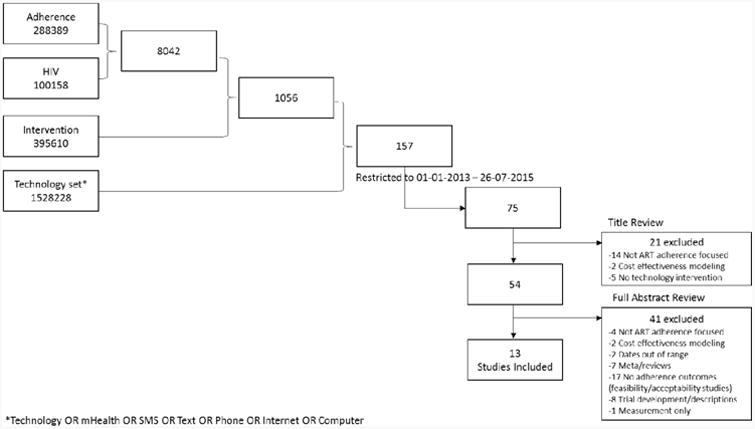
As indicated in Figure 1, the Pubmed database was searched for the combination ((((((((technology) OR mHealth) OR SMS) OR Text) OR Phone) OR Internet) OR Computer)) AND ((((HIV) AND adherence)) AND intervention) which produced 75 unique studies published between 01-01-2013 and 26-07-2015. Criteria for inclusion were: presenting an evaluation of (1) an ART adherence intervention where (2) some form of technology was used in the intervention and (3) the evaluation used a within group or between group difference test on collected data (adherence and/or immunological end-points). And adults? English language? Figure 1 lists reasons for exclusion and distributions. The vast majority of exclusions occurred due to presenting only feasibility and acceptability data (k=17) or descriptions of intervention or trial development (k=8).
Figure 1. Search results and studies excluded and included.
Data extracted
Each of the 13 full-length manuscripts was reviewed and the following data extracted: Year of publication, intervention or project name, study design, sample characteristics, intervention components, study end-points (months post baseline, type, operationalization), whether or not significant effects were reported for adherence and for viral load or CD4 (each yes, no, mixed), and date(s) of data collection. Data not included in text was marked as ‘not reported’.
Synthesis
The current review did not use meta-analytic strategies. Rather, a narrative description of each study nested within the main areas that emerged from the available data was used, with main items of interest (study design, sample sizes, length of follow-up and outcomes) summarized in table form for readers to appreciate both the diversity of the evidence base, as well as commonalities.
Results
The 13 studies published over the last 2-3 years could be categorized by the type of technology (computer [9-12], internet/website [13-15], cell phone [16-20], or dose-monitoring device [21]) and within these categories the manner in which the technology was used to promote ART adherence. Each category will be reviewed, followed by an overall summary of advances and gaps in the evidence base. Data extracted from each study is presented in Table 1.
Table 1. Studies included in synthesis in reverse chronological order.
| Lead Author (publication date) Intervention/Study name Design | Technology | Sample [Dates of implementation/data collection] | Intervention | Outcomes End-point findings | Effect on Adherence; Effect on VL or CD4 |
|---|---|---|---|---|---|
| Sabin (2015) [21] China Adherence through Technology RCT | EDM | China: 120 adults enrolled (116 analyzed: 62 in intervention and 54 in control arms) stratified by prior 3 month EDM history (>=95% and <95% within dose time (+/- 1-hour) adherence) [Dec 2012 - April 2013] |
6 months of Wisepill monitoring with individualized reminders triggered by late (>30 minutes) dosing with data informed counseling implemented in conjunction with clinical care visits. Messages were selected by participants from a pre-specified list of 10 options that had been developed by clinicians and patients that did not refer to HIV (e.g., “Be healthy, have a happy family”). Individual counseling used the Wisepill data to explore barriers to adherence and help participants to develop strategies to improve adherence and were generally brief (15-20 minutes). |
9 months (6 months on intervention) Significant effect on percent with optimal in dose time adherence (87% versus 52%, p< .001) which was evident in both participants non-adherent at baseline (78% vs 33%; p= .003) and those who were adherent at baseline (92% versus 63%; p= .002); Trend towards improvements in CD4 counts and non-significant for viral load. |
YES; TREND |
| Robbins (2015) [12] Masivukeni RCT | Computer software | South Africa: 55 non-adherent (<90% on clinic-based pill count, detectable viral load or other clinical signs of non-adherence) adults [August 2008-April 2010] |
Masivukeni - multimedia computer used by lay counselor and patient, and patient's treatment partner. |
5-6 week post baseline 20 participants with available data (10 per arm) showed 10% improvement in adherence (pill count based) for intervention arm and decrease of 8% in control condition (p= .17). |
TREND; NR |
| Cote (2015) [13] VIH-TAVIE RCT- Quasi-experimental | Internet/Website | Canada: 179 treatment experienced adults (99 in intervention arm clinic; 80 in control arm clinic) [dates not reported] |
Virus de I'immunodeficience humaine-Traitment assistance virtualle infirmiere et enseignement – VIH-TAVIE: Virtual follow-up targeting support focused on developing self-assessment skills, motivation, positive imagery, emotional management, coping, problem-solving and skills to interact with health care teams. |
6 months GEE on self-reported adherence over time showed both groups improved over 3 and 6 months (p=.17) |
NO; NR |
| Kurth (2014) [10] CARE+ RCT | Computer Software | US: 240 (209 reaching 9m) adults randomly assigned to CARE+ (N=118) or SOC (N=120) [dates not reported] |
Computerized counseling program with an audio avatar guiding participants through 4 multicomponent sessions targeted adherence and sexual risk reduction through use of tailored feedback, videos of peers and professionals, planning activities, and printouts based on information, motivation and behavioral skills building and delivered with motivational interviewing strategies |
9 months Significant impact on increased VAS adherence over time (p= .046) and trends on decreased in viral load between study arms (p= .053); subgroup analyses among those entering the study with detectable viral load showed significant gains in adherence (p= .04) and decreases in viral load (p= .04). |
YES: MIXED |
| Shet (2014) [20] HIVIND RCT | Mobile phone-messaging voice | India: 631 ART naive adults (315 in intervention arm; 316 in control arm) followed for 96 weeks [July 2010 – August 2011] |
Customized, automated voice reminders asking about dosing sent weekly with a pictorial text sent weekly. Texts required response with calls repeated up to three times in 24 hours if no response. |
96 weeks (∼24 months) Participants did not differ on pill-count assessed adherence (p= .14) or virologic failure (p= .95). |
NO; NO |
| Belzer (2014) [16] RCT | Mobile phone-counseling | US: 37 non-adherent (<90% adherent on self-report, viral load > 1000, non-persistent or delayed in starting ART) young adults (19 in intervention arm [14 with data at 48 weeks]; 18 in control arm [17 with data at 48 weeks]) [2010] |
One to two daily phone calls Monday through Friday made to participants' own mobile phone or a study provided phone matched to ART dosing schedules where an ‘adherence facilitator’ (typically a research assistant) followed a script in assessing medication dosing, problem solving and providing appropriate referrals to resources or services. |
48-weeks (∼11 months) VAS on last weekend, last 7-days, last month and last 3-months significantly better in intervention arm at weeks 24 and 48. 43% of the intervention arm participants contributing to week 48 data (8/14) reported >=90% adherence while only 6% of those in the control arm met this criteria (1/17, p= .03); Mean viral load and percent undetectable at <400 significantly better in intervention arm at 24 (p= .002) and 48 weeks (p= .043). |
YES; YES |
| Claborn (2013) [9] eLifeSteps RCT | Computer software | US: 92 adults with self-reported adherence <95% randomized to intervention (evaluated N=47) versus standard of care (evaluated N=50) [dates not reported] |
Adaptation of LifeSteps to a single session intervention with 10 steps targeting education, retention (transportation to appointments), obtaining medications, communication with healthcare team, coping with side-effects, creation of a daily medication schedule, medication storage, use of dosing cues and managing “slips” in adherence |
1-month Intervention arm participants trended towards higher self-reported adherence at 1-month follow-up compared to control arm. (p = .056) |
TREND; NR |
| Maduka (2013) [19] RCT | Mobile phone-messaging text | Nigeria: 104 adults non-adherent (estimated adherence < 95%) adults (52 in intervention arm and 52 in control arm) [dates not reported] |
A cognitive intervention session conducted by a junior resident doctor (45-60 minutes) followed by twice weekly (Monday and Thursday mornings) text messaging of an adherence focused message with a reminder to take medications implemented for 4 months. |
4 months Self-reported adherence at 4 months was significantly (77% versus 56%; p= .022) higher in the intervention condition and chart extracted median CD4 was significantly higher in intervention arm (p= .0007) |
YES; YES |
| Hersch (2013) [14] Life-Steps for Managing Medication and Stress RCT | Internet/Website | US: 168 adults enrolled; 164 analyzed (87 in intervention arm; 77 in control arm) [July 2010 – October 2011] |
A web-based version of the LifeSteps intervention with added components for stress and mood management for a total of 10 LifeSteps modules and 9 Stress Management modules. |
9 months MEMs adherence at 3, 6, and 9 months; Sig effects on adh and viral load |
YES; MIXED |
| Horvath (2013) [15] Thrive with Me RCT | Internet/Website | US: 124 MSM reporting imperfect adherence in the past month recruited online and randomly assigned to control (57) or intervention (67: 66 analyzed) [dates not reported] |
A full website with an exchange board (participants could post messages to one another monitored by study staff), an online profile that tracks “Thrive points” earned to date (earned by logging into the program) and has an interactive medication schedule that monitored weekly adherence with optional medication dosing SMS or email reminders which would populate their adherence graph with collected dosing data, and access to video segments, brief HIV related articles, and links to other webpages and resources |
12 weeks (∼3 months) Total self-reported adherence in last month did not significantly differ between arms at 12 weeks although a trend for in-time adherence (p = .095) and significant gains in with-requirements adherence (p=.04) were reported; subgroup effect among substance users (90% vs 58%) was reported (p= .02) |
MIXED; NR |
| Huang (2013) [17] RCT | Mobile phone-counseling | China: 93 Tx experienced (46 enrolled in intervention with 40 analyzed; 47 in control with 42 analyzed) and 103 treatment naïve (52 enrolled in intervention with 47 analyzed; 51 in control with 43 analyzed) [2011] |
Mobile phone calls with nurse or clinic staff placed every two-weeks targeting exploration of barriers in getting to care, adherence, side-effects and any difficulties with either adherence or retention in HIV-care with up to 4 additional calls placed if participant could not be reached. |
3 months CD4 counts and self-reported adherence did not significantly differ between groups. Self-reported adherence remained high in both groups. Secondary significant effects on quality of life dimensions among treatment naïve were reported. |
NO; NR |
| Naar-King (2013) [11] MESA RCT | Computer software | US: 76 young adults new to ART (36 in intervention condition; 40 in the time, attention and modality matched condition) [dates not reported] |
2 session computer delivered MI adherence intervention that uses feedback based on collected assessments from participants as they engage in the intervention, and engages participant in fostering motivation through MI strategies, with several opportunities for choice and autonomy building. |
6 months Viral load and self-reported adherence over the past week measured at baseline, 3 and 6 months suggested intervention arm participants had better viral control at 6 months, as well as higher adherence. Effect sizes were moderate to large- no p values calculated |
YES: YES as effect size estimates |
| Lewis (2013) [18] Within groups | Mobile phone-messaging text | US: Within group study of 52 MSM (46 competing 3 month follow-up) [July – October 2010] |
Dynamic tailored text messaging sent around dose times with messages tailored to reflect encouragement of excellent adherence or increasing adherence based on SMS collected self-reported number of doses missed in the past week, collected each Sunday of the 3 month intervention. |
3 months Significant effects on self-reported adherence (p= .04), as well as viral load (p= .01) and CD4 (p= .04), which were stronger when evaluated only among those entering study with higher viral load and lower CD4 counts. |
YES; YES |
Computer software
Four studies used software to program interventions that engaged participants in clinic with sophisticated interactive programs that tailored intervention content during the user's experience. Programs tended to focus on adapting in-person counseling interventions to computer-delivery [9-11] although also included one intervention developed for use by both adherence lay counselors and the people living with HIV they are counseling [12]. Software offered at point of care has particular interest in resource- limited settings where human resources to provide quality education and adherence support may be less available. Across the 4 different studies included in this category, 3 were conducted in the US and 1 in South Africa, 427 patients were involved, all were RCTs, and significant effects on adherence were reported in half with trends reported in the other half. Viral load, evaluated in 2 studies, had one trend and one significant outcome.
Adapting in-person interventions to computer delivery
Three interventions evaluated counseling programs articulated to computer delivery [9-11]. eLifeSteps adapted the LifeSteps intervention [22, 23] into a single session (33-90 minutes) program and workbook. [9] eLifesteps was evaluated in a predominantly white (59%) male (82%) adult (average age 44) sample reporting non-adherence (<95%). At 1-month follow-up, the control arm appeared to maintain high adherence (81% adherence pre and 81% adherence at follow-up) while the intervention condition increased adherence (67% pre and 81% adherence at follow-up), which was a trend but did not reach significance. Although the authors present viral load and CD4 data, differences between groups were not analyzed. Feasibility and acceptability were rated favorably.
The CARE+ intervention delivered via touch-screen tablet trended towards positive impact on immunological outcomes at 9-month follow-up, although change over time on self-reported visual analogue adherence (VAS) was significant in favor of the intervention.[10] CARE+ is an audio narrated 4 session program that uses avatar assisted assessment and intervention components providing tailored feedback and skills building videos, as well as printed referrals. Overall, although CARE+ participants had reductions in viral load over the 9 months of the study, while control arm participants had increases, the difference was a trend (p=.053 for differences in change in viral load; p=.09 for proportions with undetectable viral load at 9 months). Within the subgroup of participants starting with detectable viral load, these differences were significant, with CARE+ participants significantly decreasing viral load over time and control arm participants non-significantly decreasing; groups significantly differed at 9-months (p= .04). Effects on VAS adherence over time showed that the CARE+ group increased adherence while the control arm decreased over time (p= .05), with sub-group analyses among those with detectable viral load at baseline reaching significance (p=.04). Three-quarters reported preferring the computerized interactions over human-counselor interactions.
Specific to young adults (average age = 20 years), the Motivational Enhancement System for Adherence (MESA), a 2-session (30 minutes each) web-based motivational interviewing (MI) intervention delivered in conjunction with clinical care, was piloted in at 8 different clinical care sites in the US within the Adolescent Trials Network (ATN) among ART naïve, majority African American (71%) males (80%).[11] MESA offers several two-dimensional characters for participants to select from as an avatar who delivers individualized health related feedback using MI based strategies to foster motivation and skills building. In comparison to the control condition where participants engaged in a similar program focused on nutrition and physical activity, at 6 months 51% of participants retained in the MESA condition (17/33) achieved viral suppression (cut off not reported) versus 39% (14/37) at 6-months post baseline, which was calculated as a moderate to large effect in favor of the intervention. Moderate to large effects in these as-treated analyses were noted for change in viral load, percent adherence self-reported over last week, and percent adherence over last weekend. Inferential statistics were not used; no p values were reported.
Using computer program together (counselors, clients, and treatment partners)
The Masivukeni intervention (Let's Wake Up) was piloted in South Africa with 65 non-adherent, Xhosa speaking (94%), adults (average age 38; 66% female)[12]. This multi-media computer program was designed to guide lay adherence counselors in a culturally tailored adaptation of the SMART intervention [24, 25] where the counselor works with patients in completing a brief assessment to identify needs and the patient, counselor and treatment partner (selected by patient with assistance of program and counseling during session 1 to identify an appropriate partner) complete 6 sessions together that use one-on-one discussion and the program to assist in conveying complex ideas and development of common language for adherence and treatment success through culturally tailored metaphors and heuristics. Completion rates were 82% and 88% for intervention and control arms, respectively. Incomplete data limited evaluation of pill-count based adherence. Evaluation of 10 participants per group indicated adherence in the intervention condition improved 10% while control arm participants decreased adherence by 8% (p=.17). Proportion reaching 80% adherence significantly differed at end-point with 67% reaching 80% or greater in the intervention arm, and 16% in the control arm (p < .05). Viral load and CD4 effects were not evaluated.
Internet Websites
Three studies used websites as their main intervention component [14-16]. Although any of these could be offered as stand-alone computer software programs (as above), a unique feature of web applications is their availability from any internet connection. In this category, 471 participants from 2 studies in the US and 1 in Canada are represented. While adherence was generally supported (only one study reported non-significant findings across all analyses), the effect on viral load was mixed. These studies varied in how the internet was leveraged for the main intervention; either for use as virtual follow-up, to deliver a counseling intervention, or to create a social-media/network-like website.
Virtual Follow-up
The impact of VIH-TAVIE was evaluated in a quasi-experimental design where one clinic implemented VIH-TAVIE and another served as the standard of care contrast -- each in Montreal, Canada. [13] The sample was predominantly adult (average 48 years of age) males (87%), on treatment for 11 years. VIH-TAVIE intervention arm participants were asked to engage in 4 sessions (10 – 20 minutes each) with a web-based intervention where a virtual nurse guides the participant through videos and activities over a 3-4 month period (every 2 weeks). Adherence (>90% doses taken on self-report), which was high at baseline, generally improved in both groups through to the 6-month end-point with no significant differences noted between the groups. Immunological functioning was noted as extracted from records and high at baseline, although no follow-up data was provided.
Counseling intervention
The Life-Steps for Managing Medication and Stress Intervention was evaluated with 164 adult (average age 46) predominantly African American (84%) male (73%) treatment experienced (>40% on ART for 10 or more years) patients receiving care at a large urban clinic in Washington DC with a detectable (>48) viral load.[14] Life-Steps participants had access to a web-based program including Life-Steps [23] and coping, stress and mood management modules delivered by a virtual clinician. Participants could access the program from any internet connected computer, with the option to use the clinic computer if needed or desired. At 9 months, control arm participants declined (85% to 66%) in MEMs adherence more than those in the intervention condition (83% to 73%; p <.05). Detectable viral load (>400) decreased significantly more in the intervention condition (p=.02); detectable at >48 was not significant.
Social media/networking-like websites
Thrive with Me is a web-based intervention portal where men who have sex with men (MSM) living with HIV self-reporting less than 100% adherence were offered the opportunity to use a comprehensive site that included networking with other participants, tracking adherence, optional SMS or email reminders and information content and links to resources [15]. Participants were not required to log into the website during its 8-weeks of availability, but were entered into a raffle for a $25 gift card if they had earned 5 or more Thrive points (indicative of checking in with the website at least 5 of the 7 days of a given week). All 123 adult (average age 43) participants living with HIV for an average of 13 years were enrolled from the US online. Self-reported dose adherence at one-month post intervention (12 weeks post baseline) did not significantly differ between study arms, although there was a trend for in-time adherence (increase of 6.6% versus a decrease of 3.0% from baseline, p= .095) and significant effect on with-requirements adherence (increase of 8.3% versus a decrease of 3.7% from baseline, p= .04). In a subgroup analysis, effects of the intervention among substance users were supportive of the intervention across all measures of adherence (p= .02 for overall adherence). Over multiple metrics of utilization, the program appeared to be used as intended by most intervention arm participants, with 25% opting into the SMS feature, and the intervention experience and content was rated highly in feasibility and acceptability.
Mobile Phones
Five studies [16-20] evaluated interventions using some aspect of mobile phone technology including over 1,000 participants across multiple countries. Most (3/5) demonstrated impact on adherence, and on clinical end-points (3/4). Studies were divided into use of mobile phones for one on one (live) phone calls for counseling (k=2) or use of automated messaging (using voice or text: k=3).
Phones calls
Two studies evaluated the impact of calls placed to patients as a method to support adherence outside of the clinical care setting representing 233 participants in China and the US. One intervention in China stratified treatment naïve or experienced, majority female (52%) adults receiving care at one of 3 treating hospitals in Baoshan China to receive a call reminder prompted by not showing up for a clinical care visit that included brief (∼3 minutes) problem solving on both retention and adherence. [17] Reminder calls were placed every 2-weeks except for when the participant attended their scheduled HIV medical visit. At 3 months, no significant differences by study arm in either strata on CD4, retention in care or self-reported adherence, although adherence appeared uniformly high by self-report. Secondary measures of quality of life and successful receipt of placed calls did appear better in the treatment naive strata's intervention condition.
A more intensive phone-delivered intervention was pilot tested with 37 non-adherent, majority male (62%) African American (70%) young adults (average age 20) in 5 different US ATN sites.[16] One to two calls were placed daily (Monday through Friday), matched to ART dosing schedule, for 24 weeks by an “adherence facilitator” (typically a research assistant) that confirmed dose taking, and offered problem solving and referral to services. At 48 weeks, self-reported VAS adherence significantly improved in the intervention arm, and mean viral load and percent undetectable at <400 significantly favored the intervention condition. Per protocol, participants who were non-adherent to the intervention phone calls were discontinued (20% or more missed calls, or 10 consecutive days missing calls), which resulted in 37% (7/19) being discontinued from the study prior to end-point. Of note, only 27% of participants used their own phone for the intervention by study end.
Use of mobile messages
Several studies (k= 3) evaluated interventions where a key component was using mobile phones to reach participants between care visits, outside the clinical care setting. The studies included a total of 787 participants in India, Nigeria, and the US. Of the three studies, the two using interactive texts report positive findings.
The HIVIND study evaluated the effects of a weekly pre-recorded motivational voice message, customized to sex, language and call time of participant's choice asking if doses had been taken as prescribed [20]. Although pre-set responses to texts were expected, there was not an outreach component (response from study to replies). Approximately 4 days after the call, participants received a pictorial text that was a reminder to continue dosing. HIVIND was evaluated with ART naïve participants in India (43% women, 45% rural). Groups did not differ at the 96 week end-point on viral failure (primary end-point), time to failure or pill-count based adherence.
A text-based intervention in Nigeria (57% female) with non-adherent adults (average age 35) used a combined approach of a brief counseling session (45-60 minutes) followed by twice weekly text messaging for 4 months [19]. The text messages could be responded to with a reply or the originating number could be called directly at the participants' discretion. At 4 months, the intervention arm had higher self-reported adherence (past 7 days: 77% versus 56%, p = .022) and higher CD4 counts (extracted from clinical records; 578 cells/ml versus 362 cells/ml, p= .0007). Utilization of intervention data was not reported, although the authors attribute intervention effects to increasing patient knowledge and literacy around HIV medication and adherence. The other text-based intervention was a small within-groups pilot in the Midwestern US with a predominantly white (44%) sample of MSM adults (average age 38) [18]. Participants were sent SMS messages that were tailored to reflect the kind of encouragement needed maintaining or increasing adherence depending on participant's SMS based past-week adherence assessment collected weekly. Among the 46 MSM completing the 3-month follow-up (of 52 enrolled), self-reported number of doses missed per week decreased significantly from baseline (averaging around 2 missed at baseline to about 1 at follow-up, p=.04) and viral load significantly decreased (Cohen's d = -.40, p= .012), particularly among those starting the study with higher viral loads. Similarly CD4 counts increased (Cohen's d= .21, p= .04), which was more pronounced for those starting the study with lower counts. Of note, however, Hispanics enrolled in the study were more likely to drop out before follow-up assessments, and were more likely to have missing data for immunological functioning.
Data informed Counseling
The final type of intervention combined counseling with real-time electronic drug monitoring data. The RCT conducted in Guangxi China with 120 (64% male) adults (average age 38 years) stratified by adherence (optimal/suboptimal) collected during a 3-month pre-randomization run-in with Wisepill. The Wisepill device stored ART medication and wirelessly transmitted device opening [21]. For those assigned to the intervention condition, real-time adherence monitoring identified delays in dosing (30 minutes) which prompted individualized text-messages to be sent. In addition, during the 6-months of intervention, monthly clinical care visits included meeting with a counselor when the Wisepill data suggested <95% on-time adherence. At 9 months intervention arm participants had a higher proportion of optimally adherent participants (within 1 hour of dose time; 87% vs 52%, p<.001). This effect was significant in each strata- even optimal adherers at baseline demonstrated benefit, with 92% retaining optimal adherence in the final study month versus only 63% in the control condition, although the intervention effect was more dramatic in the strata of sub-optimal adherers (78% versus 33%). A trend for improvements in CD4-cell counts was also identified in favor of the intervention arm, but undetectable viral load improved similarly for both arms with no significant difference, perhaps due to high rates of suppression across the groups at end study (94% and 98%).
Strengths in the evidence base
Numerous interventions recently evaluated have demonstrated success on adherence and clinical outcomes. Innovative approaches are well represented, such as using dynamic messaging, real-time monitoring for in-time intervention, full leveraging of networking-like websites, and creating tools to assist counselors in implementing high quality adherence interventions. There was also attention to “triaging” adherence interventions to those who have demonstrated difficulties with adherence, a recommendation emerging from early meta-analytic work on adherence interventions [26] and also a potential cost saving strategy. Use of RCTs and higher powered statistical approaches are apparent suggesting improvements in use of rigorous methodologies. Greater, though not universal, attention to describing the active ingredients in standard care (see [27]) is also evident in the newer evidence base.
Gaps in the Evidence Base and Recommendations
Table 2 summarizes noteworthy limitations in the evidence base and associated recommendations for future research in this area that could make marked improvements.
Table 2. Gaps and recommendations.
| Area | Gaps in the evidence base reviewed | Recommendations for future research efforts |
|---|---|---|
| Follow-up periods | Trials examining longer periods of adherence are needed. This may reflect that most studies were small sample pilot studies, but extending to 12 or more months would be necessary to gather compelling evidence. Across the studies included almost all used 9 months or less. | Use longer follow-up periods (∼12 months). |
| Level of adherence at baseline | Pre-intervention adherence levels continue to appear to show relevance in outcomes. | Attend to pre-intervention levels of adherence as a potential moderator of effects. |
| Measurement of adherence | Adherence was largely measured via self-report and while the combination of this with objective clinical outcomes is meaningful, patterns of dosing and persistence may be better captured by electronic dose monitoring or ecological assessment (eg., SMS) strategies. | Use dose monitoring (electronic or SMS or other strategy) approaches in addition to recall-based self-report adherence data. |
| Utilization reporting | Within main reports of study outcomes, utilization data should be standard. While several studies included percent interacting with the technology as intended, this should be a basic metric included in all technology approaches. | Report utilization data in terms of calls placed, messages sent, reply rates, website use and software use and factors that may have influenced uptake. |
| Characterization of control condition | Attending to active intervention components in the control arm was not uniformly incorporated but may have impact on outcomes.[27] | Better characterize adherence strategies offered as standard of care. |
| Dissemination of findings | Several studies had a 3-5 year lag-time from dates of study to publication date which is enough time for technology availability and use to change dramatically. | Aggressively work to disseminate outcomes in short time-frames (<2 years); prior to shifts in technology and user preferences for certain kinds of technology. |
| Nomenclature | There is inconsistent use of common terms such as “interactive”, “bidirectional”, “targeted messages”, “tailored messages”, and “personalized messaged”. | Build a common nomenclature for describing important aspects of technology used in interventions, particularly for SMS messaging. |
| Key populations | There was limited attention to key populations (eg., substance users, expecting mothers, sex workers). | Focused work including key populations and emerging populations (e.g., those starting treatment immediately post diagnosis) is needed. |
Discussion
This review of pubmed for interventions focused on enhancing ART adherence in adult populations through the use of technology identified 13 studies conducted between 2012 and July 2015 that produced a compelling evidence base for approaches using technology. A maturing evidence base with quality designs and biological outcomes is emerging that could be improved with the noted recommendations (see Table 2) and undoubtedly will double again in the next few years. Overall, the vast majority of interventions included had a direct effect or trend on adherence, and many had effects on a biological outcome.
Recent recommendations for conducting mHealth intervention trials [28] highlight the important role of sufficient time allocation for intervention planning, design and development. In fact, several studies excluded from this outcomes-focused review were focused on this kind of early phase work. In that body of literature, a mobile intervention and assessment tool specific for methamphetamine users (iTab: [29]) demonstrated high acceptability and response rates, and TxText [30], a fully automated text message based tool to monitor and intervene with substance using people living with HIV, similarly reported high acceptably and moderate response rates. The next several years is likely to see considerable advances, particularly in mobile messaging approaches as treatment access and initiation is anticipated to markedly increase in resource limited settings where cell phone use is common and automated outreach meets a specific gap in reach of clinical care services.
Depth of understanding of how technological modalities may operative to impact health is also increasing, suggesting that about half of participants who can reply to texts do and half of those replies involve challenges in logistics that can be problem-solved [31]. These and other results suggest high efficiency in messaging as a tool that can triage resources to those in need. Social exchanges also offer opportunities for communities to build motivation and skills together, further streamlining resources. For example, posts in the Thrive with Me intervention revealed that most focused on mentoring others and providing feedback. [32]
Limitations to the current review include reliance on Pubmed as the sole source for defining the evidence base. As previously noted, the intention was to capture “forward facing literature” – or the evidence that would be readily available for review by most researchers and practitioners. The evidence synthesized in the current review does not intend to capture all evidence, and generalizations are limited to the database and search terms utilized.
Increasingly, technology is connecting individuals to each other and to resources in countries all over the world. Leveraging what is already a high-use modality holds tremendous promise at potential low cost (see for example [33]). To date, there is considerable support for technology as a tool to enhance adherence in diverse populations and, like technology itself, the evidence base is rapidly expanding.
Conclusions
Technology enhanced or focused interventions to promote ART adherence have successfully used computer software, internet websites, mobile phone technologies and smart phone applications. Emerging and future work should seek to uncover “active ingredients,” or the specific aspects of the technology that appear to impact ART adherence, and the context or profiles of individuals most likely to benefit from such approaches, which may be best addressed through qualitative or mixed methods exploration nested within RCTs. Extended to persistence, retention in or return to HIV-care, calls, texts, and technology enhanced outreach (eg., locating those lost to care through social networks) are promising approaches. As we seek to engage more PLWH in care and ART, rapid leveraging of the kinds of “common place” technologies that permeate social life (cell-phones, social networks/sites) and clinical care settings (eg., computers and internet) around the world may help to offer responsive, patient-centered approaches to HIV-care.
Footnotes
Compliance with Ethics Guidelines: Conflict of Interest: Dr. Amico is the recipient of an unrestricted educational grant from Gilead Sciences through the University of Michigan.
Human and Animal Rights and Informed Consent: This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
* Of importance
** Of major importance
- 1**.Pellowski JA, Kalichman SC. Recent advances (2011-2012) in technology-delivered interventions for people living with HIV. Curr HIV/AIDS Rep. 2012;9:326–334. doi: 10.1007/s11904-012-0133-9. A comprehensive review of technology-focused interventions to promote adherence among PLWH. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNAIDS. Joint United Nations Programme on HIV/AIDS (UNAIDS) 2014. 90-90-90: An ambitious treatment target to help end the AIDS epidemic. [Google Scholar]
- 3.Gakumo CA, Enah CC, Vance DE, Sahinoglu E, Raper JL. “Keep it simple”: older African Americans' preferences for a health literacy intervention in HIV management. Patient Prefer Adherence. 2015;9:217–223. doi: 10.2147/PPA.S69763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4*.Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PLoS One. 2014;9:e88166. doi: 10.1371/journal.pone.0088166. A meta-analytic synthesis of research using text messagung to enhance adherence among PLWH. covering research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5**.Mbuagbaw L, van der Kop ML, Lester RT, Thirumurthy H, Pop-Eleches C, Ye C, et al. Mobile phone text messages for improving adherence to antiretroviral therapy (ART): an individual patient data meta-analysis of randomised trials. BMJ Open. 2013;3:e003950. doi: 10.1136/bmjopen-2013-003950. An innovative combination of participant-level data from three different studies using text messaging to promote adherence that distilled aspects of texting (timing and interactivity) that appeared to promote intervention effects. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kannisto KA, Koivunen MH, Valimaki MA. Use of mobile phone text message reminders in health care services: a narrative literature review. J Med Internet Res. 2014;16:e222. doi: 10.2196/jmir.3442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tufts KA, Johnson KF, Shepherd JG, Lee JY, Bait Ajzoon MS, Mahan LB, et al. Novel Interventions for HIV Self-management in African American Women: A Systematic Review of mHealth Interventions. J Assoc Nurses AIDS Care. 2015;26:139–150. doi: 10.1016/j.jana.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 8.Mathes T, Antoine SL, Pieper D. Adherence-enhancing interventions for active antiretroviral therapy in sub-Saharan Africa: a systematic review and meta-analysis. Sex Health. 2014;11:230–239. doi: 10.1071/SH14025. [DOI] [PubMed] [Google Scholar]
- 9.Claborn KR, Leffingwell TR, Miller MB, Meier E, Stephens JR. Pilot study examining the efficacy of an electronic intervention to promote HIV medication adherence. AIDS Care. 2014;26:404–409. doi: 10.1080/09540121.2013.824534. [DOI] [PubMed] [Google Scholar]
- 10.Kurth AE, Spielberg F, Cleland CM, Lambdin B, Bangsberg DR, Frick PA, et al. Computerized counseling reduces HIV-1 viral load and sexual transmission risk: findings from a randomized controlled trial. J Acquir Immune Defic Syndr. 2014;65:611–620. doi: 10.1097/QAI.0000000000000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11*.Naar-King S, Outlaw AY, Sarr M, Parsons JT, Belzer M, Macdonell K, et al. Motivational Enhancement System for Adherence (MESA): pilot randomized trial of a brief computer-delivered prevention intervention for youth initiating antiretroviral treatment. J Pediatr Psychol. 2013;38:638–648. doi: 10.1093/jpepsy/jss132. One of the few RCTs evaluating technology impact on adherence among adolscents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12**.Robbins RN, Mellins CA, Leu CS, Rowe J, Warne P, Abrams EJ, et al. Enhancing Lay Counselor Capacity to Improve Patient Outcomes with Multimedia Technology. AIDS Behav. 2015;19 Suppl 2:163–176. doi: 10.1007/s10461-014-0988-4. An example of using technology to enhance human delivery of counseling services for adherence support in South Africa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cote J, Godin G, Ramirez-Garcia P, Rouleau G, Bourbonnais A, Gueheneuc YG, et al. Virtual intervention to support self-management of antiretroviral therapy among people living with HIV. J Med Internet Res. 2015;17:e6. doi: 10.2196/jmir.3264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hersch RK, Cook RF, Billings DW, Kaplan S, Murray D, Safren S, et al. Test of a web-based program to improve adherence to HIV medications. AIDS Behav. 2013;17:2963–2976. doi: 10.1007/s10461-013-0535-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horvath KJ, Oakes JM, Rosser BR, Danilenko G, Vezina H, Amico KR, et al. Feasibility, acceptability and preliminary efficacy of an online peer-to-peer social support ART adherence intervention. AIDS Behav. 2013;17:2031–2044. doi: 10.1007/s10461-013-0469-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Belzer ME, Naar-King S, Olson J, Sarr M, Thornton S, Kahana SY, et al. The use of cell phone support for non-adherent HIV-infected youth and young adults: an initial randomized and controlled intervention trial. AIDS Behav. 2014;18:686–696. doi: 10.1007/s10461-013-0661-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang D, Sangthong R, McNeil E, Chongsuvivatwong V, Zheng W, Yang X. Effects of a Phone Call Intervention to Promote Adherence to Antiretroviral Therapy and Quality of Life of HIV/AIDS Patients in Baoshan, China: A Randomized Controlled Trial. AIDS Res Treat. 2013;2013:580974. doi: 10.1155/2013/580974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewis MA, Uhrig JD, Bann CM, Harris JL, Furberg RD, Coomes C, et al. Tailored text messaging intervention for HIV adherence: a proof-of-concept study. Health Psychol. 2013;32:248–253. doi: 10.1037/a0028109. [DOI] [PubMed] [Google Scholar]
- 19.Maduka O, Tobin-West CI. Adherence counseling and reminder text messages improve uptake of antiretroviral therapy in a tertiary hospital in Nigeria. Niger J Clin Pract. 2013;16:302–308. doi: 10.4103/1119-3077.113451. [DOI] [PubMed] [Google Scholar]
- 20.Shet A, De Costa A, Kumarasamy N, Rodrigues R, Rewari BB, Ashorn P, et al. Effect of mobile telephone reminders on treatment outcome in HIV: evidence from a randomised controlled trial in India. BMJ. 2014;349:g5978. doi: 10.1136/bmj.g5978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sabin LL, Bachman DeSilva M, Gill CJ, Zhong L, Vian T, Xie W, et al. Improving Adherence to Antiretroviral Therapy With Triggered Real-time Text Message Reminders: The China Adherence Through Technology Study. J Acquir Immune Defic Syndr. 2015;69:551–559. doi: 10.1097/QAI.0000000000000651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Safren SA, O'Cleirigh C, Tan JY, Raminani SR, Reilly LC, Otto MW, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychol. 2009;28:1–10. doi: 10.1037/a0012715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Safren SA, Otto MW, Worth JL, Salomon E, Johnson W, Mayer K, et al. Two strategies to increase adherence to HIV antiretroviral medication: life-steps and medication monitoring. Behav Res Ther. 2001;39:1151–1162. doi: 10.1016/s0005-7967(00)00091-7. [DOI] [PubMed] [Google Scholar]
- 24.Remien RH, Mellins CA, Robbins RN, Kelsey R, Rowe J, Warne P, et al. Masivukeni: development of a multimedia based antiretroviral therapy adherence intervention for counselors and patients in South Africa. AIDS Behav. 2013;17:1979–1991. doi: 10.1007/s10461-013-0438-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Remien RH, Stirratt MJ, Dolezal C, Dognin JS, Wagner GJ, Carballo-Dieguez A, et al. Couple-focused support to improve HIV medication adherence: a randomized controlled trial. AIDS. 2005;19:807–814. doi: 10.1097/01.aids.0000168975.44219.45. [DOI] [PubMed] [Google Scholar]
- 26.Amico KR, Harman JJ, Johnson BT. Efficacy of antiretroviral therapy adherence interventions: a research synthesis of trials, 1996 to 2004. J Acquir Immune Defic Syndr. 2006;41:285–297. doi: 10.1097/01.qai.0000197870.99196.ea. [DOI] [PubMed] [Google Scholar]
- 27.de Bruin M, Viechtbauer W, Schaalma HP, Kok G, Abraham C, Hospers HJ. Standard care impact on effects of highly active antiretroviral therapy adherence interventions: A meta-analysis of randomized controlled trials. Arch Intern Med. 2010;170:240–250. doi: 10.1001/archinternmed.2009.536. [DOI] [PubMed] [Google Scholar]
- 28*.Horvath KJ, Ecklund AM, Hunt SL, Nelson TF, Toomey TL. Developing Internet-based health interventions: a guide for public health researchers and practitioners. J Med Internet Res. 2015;17:e28. doi: 10.2196/jmir.3770. A practical guide for the development of quality technology enhanced or based intervention approaches. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moore DJ, Montoya JL, Blackstone K, Rooney A, Gouaux B, Georges S, et al. Preliminary Evidence for Feasibility, Use, and Acceptability of Individualized Texting for Adherence Building for Antiretroviral Adherence and Substance Use Assessment among HIV-Infected Methamphetamine Users. AIDS Res Treat. 2013;2013:585143. doi: 10.1155/2013/585143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ingersoll K, Dillingham R, Reynolds G, Hettema J, Freeman J, Hosseinbor S, et al. Development of a personalized bidirectional text messaging tool for HIV adherence assessment and intervention among substance abusers. J Subst Abuse Treat. 2014;46:66–73. doi: 10.1016/j.jsat.2013.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mbuagbaw L, Thabane L, Ongolo-Zogo P. Opening communication channels with people living with HIV using mobile phone text messaging: insights from the CAMPS trial. BMC Res Notes. 2013;6:131. doi: 10.1186/1756-0500-6-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kodatt SA, Shenk JE, Williams ML, Horvath KJ. Leadership Qualities Emerging in an Online Social Support Group Intervention. Sex Relation Ther. 2014;29:467–475. doi: 10.1080/14681994.2014.941346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rodrigues R, Bogg L, Shet A, Kumar DS, De Costa A. Mobile phones to support adherence to antiretroviral therapy: what would it cost the Indian National AIDS Control Programme? J Int AIDS Soc. 2014;17:19036. doi: 10.7448/IAS.17.1.19036. [DOI] [PMC free article] [PubMed] [Google Scholar]


