Abstract
OBJECTIVE
Positive psychological states are linked to superior health and longevity, possibly due to behavioral factors. We evaluated cross-sectional and 5-year associations between positive affect and health behaviors in patients with coronary heart disease (CHD).
METHODS
Outpatients with CHD reported positive affect, physical activity, sleep quality, medication adherence, cigarette smoking, and alcohol use at baseline (N = 1022) and five years later (N = 662). Covariates in regression analyses included demographics, cardiac disease severity, and depressive symptoms.
RESULTS
At baseline, higher positive affect (per 1-SD) was associated with better health behaviors: physical activity (OR = 1.52; 95% CI = 1.30, 1.77; p < 0.001), sleep quality (OR = 1.24; 95% CI = 1.04, 1.48; p = 0.015), medication adherence (OR = 1.46; 95% CI = 1.12, 1.90; p = 0.005), and non-smoking (OR = 1.29; 95% CI = 1.06, 1.57; p = 0.012), but was unrelated to alcohol use. Baseline positive affect did not predict health behaviors at follow-up, accounting for baseline behaviors. However, increases in positive affect across five years co-occurred with improvements in physical activity (B = 0.023; SE = 0.008; p = 0.002), sleep quality (B = 0.011; SE = 0.005; p = 0.039), and medication adherence (B = 0.014; SE = 0.004; p < 0.001), but not smoking status (OR = 1.07; 95% CI = 0.73, 1.55; p = 0.74).
CONCLUSION
Positive affect was associated with health behaviors among CHD patients. Efforts to sustain or enhance positive affect may be promising for promoting better health behaviors.
Keywords: positive affect, health behaviors, coronary heart disease, physical activity, sleep quality, medication adherence
Introduction
Psychological and behavioral factors are important in the development and progression of cardiovascular disease. Although negative psychological states, including depression and hostility, have long been recognized as risk factors for cardiovascular morbidity and mortality (1,2), emerging evidence suggests that positive psychological states confer unique salutary effects on health (3,4). Psychological well-being—such as positive emotions, satisfaction with life, and optimism—has been linked to lower incidence of coronary heart disease, superior biological function, and longevity, independent of the effects of negative psychological states (4–8). Yet, previous studies have also reported null findings between psychological well-being and cardiovascular outcomes (9,10), or significant results for some cardiovascular outcomes but not others (11). The mixed findings in the literature point towards the need to examine physiological and psychosocial pathways that underlie subsequent cardiovascular risk.
The association between positive psychological states and favorable health outcomes is perhaps largely mediated by health behaviors. Individuals with higher well-being may be more motivated and persistent in engaging in healthy behaviors, have greater self-efficacy (12), show more attention to and careful processing of health risk information (13), and are better able to adjust health-relevant goals (14). Indeed, increasing evidence indicates that health behaviors (namely, physical activity) may be the underlying mechanisms linking positive psychological states to physical health status (15), reduced risk of incident coronary heart disease (16), and survival (11,17,18).
Existing studies that examine the relationship between positive psychological states and cardiovascular-related health behaviors are limited in several important ways (7,19). First, nearly all the evidence is cross-sectional. Although health-promoting behaviors (e.g., exercise, sleep habits) can improve mood (20–22), it is unknown whether positive states predict future health behaviors, and whether changes in positive states are associated with health behavior change. Second, some previous studies have not accounted for potential confounding factors, such as negative psychological states and physical health indices. Third, health behaviors are critical in the etiology and prognosis of cardiovascular disease, but the relationship between positive states and health behaviors has rarely been examined among cardiac patients (23,24).
Because cardiovascular disease is the leading cause of death in the world, an understanding of modifiable protective factors and health behaviors may have a substantial impact on morbidity and mortality. We previously found that adjusting for behavioral factors, particularly physical activity, eliminated the association between positive affect and survival (11). However, the cross-sectional and longitudinal relationships between positive affect and a range of health behaviors have yet to be described in a large sample of cardiac patients. We therefore evaluated the associations of positive affect with concurrent, long-term, and change in health behaviors—independent of demographics, depressive symptoms, and disease severity—in a cohort of older patients with stable coronary heart disease.
Methods
Participants
The Heart and Soul Study is a prospective cohort study designed to examine the influence of psychosocial factors on health outcomes in patients with stable coronary heart disease (25). Administrative databases were used to identify patients with coronary heart disease from 12 outpatient clinics in the San Francisco Bay Area. Patients were eligible if they met at least one of the following criteria: a history of myocardial infarction or coronary revascularization, angiographic evidence of at least 50% stenosis in one or more coronary vessels, or evidence of exercise-induced ischemia by treadmill or nuclear testing. Between September 2000 and December 2002, a total of 1024 patients were enrolled, with 1022 providing positive affect data at baseline. Participants underwent a baseline examination that included a comprehensive health interview, blood samples, medical history, self-report questionnaire, and exercise treadmill testing with stress echocardiography. The protocol was approved by Institutional Review Boards at participating sites, and all participants provided written informed consent.
Measures
Predictor: Positive affect
Positive affect was assessed at baseline and at the 5-year follow-up using the 10-item positive affect subscale of the Positive and Negative Affect Schedule (PANAS) (26), which was administered by paper-and-pencil questionnaire. On a 1 (Not at all) to 5 (Extremely) scale, participants rated the extent that they had felt the following emotions during the past week: attentive, interested, excited, strong, enthusiastic, determined, proud, inspired, active, and alert. PANAS scores were calculated by summing the responses to the 10 items, for a minimum score of 10 and a maximum score of 50. Previous work has demonstrated the reliability and validity of the PANAS (26); our sample showed high internal consistency reliability (Cronbach’s α = .93). To minimize respondent burden, the negative affect subscale of the PANAS was not administered.
Outcomes: Health behaviors
All health behaviors were assessed by self-report at baseline and at the 5-year follow-up.
Physical activity was measured using the question, “Which of the following statements best describes how physically active you have been during the last month, that is, done activities such as 15–20 minutes of brisk walking, swimming, general conditioning, or recreational sports?” Possible responses were: Not at all active, a little active (1 to 2 times a month), fairly active (3 to 4 times per month), quite active (1 to 2 times a week), very active (3 to 4 times a week), or extremely active (5 or more times a week). On the basis of prior work (25), participants who reported that they were “not at all active” or “a little active” were considered physically inactive, whereas those who reported that they were “fairly active” to “extremely active” were considered physically active. Physical activity was also analyzed as a continuous variable ranging from 0 to 5, with higher scores indicating greater physical activity. Self-report has been shown to be reliable and valid for measuring physical activity (27–30).
Sleep quality was measured using one item from the Pittsburgh Sleep Quality Index (31). Participants were asked, “During the last month, how would you rate your sleep quality overall?” and chose from one of the following five responses: Very bad, fairly bad, good, fairly good, or very good. On the basis of previous research (32), poor sleep quality was defined as sleep that was “fairly bad” or “very bad,” whereas good sleep quality was defined as sleep that ranged from “good” to “very good.” Sleep quality was also used as a continuous variable ranging from 0 to 4, with higher scores referring to better sleep quality.
Medication adherence was assessed using the question, “In the past month, how often did you take your medications as the doctor prescribed?” Possible response options were: All of the time (100%), nearly all of the time (90%), most of the time (75%), about half the time (50%), or less than half the time (<50%). Participants were considered adherent if they reported taking their medications 90–100% of the time, or nonadherent if they took their medications 75% or less of the time. This single-item measure and cut-off for nonadherence has been shown to predict adverse cardiovascular events (33). Medication adherence was also evaluated as a continuous variable ranging from 0 to 4, with higher scores indicating more adherence.
Alcohol use was measured with the Alcohol Use Disorders Identification Test-Consumption (AUDIT-C). Participants responded to three questions regarding their frequency of drinking, number of drinks they typically had on one occasion, and frequency of having six or more drinks on one occasion. Regular alcohol use was defined using the standard cut-off of 4 or more points on the AUDIT-C (34,35).
Smoking was assessed with a single question, “Do you currently smoke cigarettes?” Responses were “yes” or “no.”
Covariates
We examined potential confounding variables measured at baseline, as well as depressive symptoms measured at both baseline and follow-up. The severity of depressive symptoms in the past two weeks was assessed with the 9-item Patient Health Questionnaire (36). Scores ranged from 0 to 27, with higher scores indicating more severe depressive symptoms. We analyzed depressive symptoms as a continuous variable.
Demographics and medical history were obtained from a questionnaire at baseline. Participants were instructed to bring their medication bottles to the study appointment, and study personnel recorded all current medications. Height and weight were measured and used to calculate body mass index (BMI). Left ventricular ejection fraction (LVEF) was assessed by resting echocardiography. We categorized participants as having diastolic dysfunction if their mitral inflow ratio of peak early-to-late diastolic filling velocity was more than 0.75 and if their velocity time integral in the pulmonary vein was greater during diastole than during systole (37). Low- and high-density lipoprotein (LDL and HDL) cholesterol levels were determined from fasting venous blood samples.
Data analysis
We first examined the bivariate associations between positive affect (split at the median score of 32) with covariates and outcome variables. T-tests were used for continuous variables, and chi-square tests were used for categorical variables. Health behaviors that were related to positive affect were examined in further analyses. Any covariates that were associated with positive affect at p < .10 were included in subsequent multivariate analyses.
Next, logistic regression models were used to test whether baseline positive affect (as a continuous variable) was cross-sectionally associated with optimal health behaviors—that is, being physically active, having good sleep quality, being adherent to medications, and being a non-smoker. The analyses were also conducted using linear regression to examine health behaviors as continuous variables. The models were adjusted sequentially for (a) demographics; (b) BMI, comorbid medical conditions, and cardiac disease severity; and (c) depressive symptoms.
Longitudinal analyses were conducted in two ways using linear regression for continuous variables (i.e., physical activity, sleep quality, and medication adherence) and logistic regression for smoking status. First, baseline positive affect was tested as a predictor of health behaviors at follow-up, adjusting for baseline health behaviors. Second, associations were examined between 5-year change scores (follow-up minus baseline score) for positive affect and 5-year change in health behaviors. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC).
Results
Characteristics of the sample
Of the 1022 participants who completed the PANAS at baseline, 518 were categorized as “low positive affect” (i.e., PANAS score less than median of 32) and 504 were categorized as “high positive affect.” Participants with high positive affect tended to be older, were more likely to have graduated high school, and were less likely to have an annual household income below $20,000 (Table 1). High positive affect was also associated with a history of revascularization and higher HDL cholesterol, as well as lower BMI and less severe depressive symptoms.
Table 1.
Baseline characteristics of 1022 participants with stable coronary heart disease, by positive affect
| Participant characteristic | Low positive affecta (n = 518) | High positive affectb (n = 504) | P-value |
|---|---|---|---|
| Demographics | |||
| Age, mean (SD) years | 66.1 (11.1) | 67.6 (10.6) | 0.027 |
| Male sex, No. (%) | 422 (81.5) | 416 (82.5) | 0.66 |
| White, No. (%) | 311 (60.0) | 304 (60.3) | 0.93 |
| High school graduate, No. (%) | 438 (84.6) | 452 (90.0) | 0.009 |
| Income < $20,000/year, No. (%) | 298 (57.9) | 198 (39.5) | <0.001 |
| BMI and comorbid conditions | |||
| BMI, mean (SD) kg/m2 | 28.8 (5.8) | 28.0 (4.8) | 0.021 |
| Hypertension, No. (%) | 373 (72.4) | 348 (69.0) | 0.24 |
| Myocardial infarction, No. (%) | 270 (52.5) | 277 (55.3) | 0.38 |
| Stroke, No. (%) | 70 (13.6) | 77 (15.3) | 0.45 |
| Revascularization, No. (%) | 289 (56.1) | 312 (61.9) | 0.060 |
| Congestive heart failure, No. (%) | 92 (17.9) | 86 (17.2) | 0.77 |
| Diabetes mellitus, No. (%) | 141 (27.3) | 123 (24.5) | 0.30 |
| Medication use, No. (%) | |||
| Aspirin | 371 (73.2) | 369 (73.5) | 0.91 |
| Beta blocker | 294 (58.0) | 299 (59.6) | 0.61 |
| Angiotensin system inhibitor | 261 (51.5) | 262 (52.2) | 0.82 |
| Statin | 318 (62.7) | 337 (67.1) | 0.14 |
| Cardiac disease severity | |||
| LVEF, mean (SD) % | 61.6 (9.7) | 61.8 (9.5) | 0.84 |
| Diastolic dysfunction, No. (%) | 57 (12.4) | 59 (13.2) | 0.71 |
| LDL cholesterol, mean (SD) mg/dL | 104.0 (33.7) | 104.6 (33.7) | 0.80 |
| HDL cholesterol, mean (SD) mg/dL | 44.9 (13.6) | 46.8 (14.5) | 0.035 |
| Depressive symptomsc, mean (SD) | 7.3 (6.0) | 3.0 (3.8) | <0.001 |
| Health behaviors, No. (%) | |||
| Regular alcohol used | 140 (27.3) | 153 (30.5) | 0.25 |
| Current smoker | 133 (25.8) | 68 (13.5) | <0.001 |
| Adherent to medicationse | 452 (88.5) | 478 (95.2) | <0.001 |
| Sleep quality | |||
| Very bad | 50 (9.7) | 19 (3.8) | <0.001 |
| Fairly bad | 153 (29.6) | 62 (12.3) | |
| Good | 177 (34.3) | 160 (31.7) | |
| Fairly good | 102 (19.8) | 167 (33.1) | |
| Very good | 34 (6.6) | 96 (19.1) | |
| Physical activity | |||
| Not at all active | 136 (26.4) | 52 (10.4) | <0.001 |
| A little active | 108 (20.9) | 74 (14.7) | |
| Fairly active | 84 (16.3) | 72 (14.3) | |
| Quite active | 71 (13.7) | 84 (16.7) | |
| Very active | 82 (15.9) | 136 (27.1) | |
| Extremely active | 35 (6.8) | 84 (16.7) | |
Positive and Negative Affect score < 32
Positive and Negative Affect score ≥ 32
Patient Health Questionnaire-9 scores can range from 0 to 27.
Regular alcohol use was defined as a score of 4 or more on the Alcohol Use Disorders Identification Test – Consumption.
Medication adherence was defined as taking medications as prescribed 90–100% of the time
Cross-sectional associations between baseline positive affect and health behaviors
Higher levels of positive affect were associated with a lower likelihood of smoking, greater physical activity, better sleep quality, and more adherence to medications, whereas alcohol use was not related to positive affect (correlations are provided in Table S1, Supplemental Digital Content 1). In unadjusted logistic regression models, baseline positive affect (as a continuous variable) was cross-sectionally associated with greater odds of being physically active, having good sleep quality, being adherent to medications, and being a non-smoker (Table 2). After adjustment for age, education, income, BMI, history of revascularization, HDL cholesterol, and depressive symptoms, each 1-SD (8.8-point) increase in baseline positive affect was associated with 52% greater odds of being physically active, 24% greater odds of having good sleep quality, 46% greater odds of being adherent to medications, and 29% greater odds of being a non-smoker (all p-values < 0.05; Table 2). Results were comparable in linear regression models when health behaviors were analyzed as continuous variables (except smoking status, which was assessed as a dichotomous variable). In fully adjusted models, higher positive affect was associated with greater physical activity (unstandardized B = 0.037, SE = 0.006, p < 0.001), better sleep quality (B = 0.020, SE = 0.004, p < 0.001), and more adherence to medications (B = 0.011, SE = 0.003, p < 0.001).
Table 2.
Associations between positive affect (per SD [8.8-point] increase) and health behaviors at baseline
| Model | Odds Ratio (95% Confidence Interval)
|
|||
|---|---|---|---|---|
| Physically active (n = 1007) | Good sleep quality (n = 1009) | Medication adherence (n = 1000) | Non-smoker (n = 1008) | |
| Unadjusted | 1.79 (1.56, 2.06) | 1.72 (1.49, 1.99) | 1.61 (1.28, 2.02) | 1.51 (1.29, 1.78) |
| Adjusted for demographicsa | 1.78 (1.54, 2.06) | 1.70 (1.46, 1.98) | 1.54 (1.22, 1.96) | 1.34 (1.13, 1.60) |
| Adjusted for above plus BMI, HDL cholesterol, and history of revascularization | 1.75 (1.52, 2.03) | 1.69 (1.45, 1.97) | 1.60 (1.25, 2.03) | 1.40 (1.17, 1.68) |
| Adjusted for above plus baseline depressive symptoms | 1.52 (1.30, 1.77) | 1.24 (1.04, 1.48) | 1.46 (1.12, 1.90) | 1.29 (1.06, 1.57) |
Notes: All p-values < 0.001, except in fully-adjusted models for medication adherence (p = 0.005), sleep quality (p = 0.015), and non-smoking (p = 0.012).
Age, education (high school graduate), low income (income < $20,000/year)
Physically active was defined as engaging in physical activity at least 3 to 4 times per month (versus 2 or fewer times per month) (Whooley et al. 2008).
Good sleep quality was defined as ratings of “good,” “fairly good,” or “very good” sleep (versus “fairly bad” or “very bad” sleep) (Caska et al. 2009).
Medication adherence was defined as taking medications as prescribed 90–100% of the time (Gehi et al. 2007).
Non-smoking was defined as a response of “No” to the question, “Do you currently smoke cigarettes?”
Baseline positive affect predicting health behaviors five years later
After five years, 829 participants were alive. Of the surviving participants, 662 (80% of survivors) completed the follow-up assessment. Compared to surviving participants who did not provide follow-up data, those with follow-up data were more likely to be older and male, had higher income, and reported lower depressive symptoms at baseline. They also had higher positive affect and tended to be non-smokers, physically active, adherent to medications, and had good sleep quality at baseline. There were no significant differences at baseline in race, education, alcohol use, BMI, diastolic dysfunction, LVEF, or other relevant variables between those who did versus did not provide follow-up data. The cross-sectional associations between positive affect and health behaviors at follow-up were similar to those observed at baseline, except the relationship between positive affect and non-smoking was eliminated after including covariates.
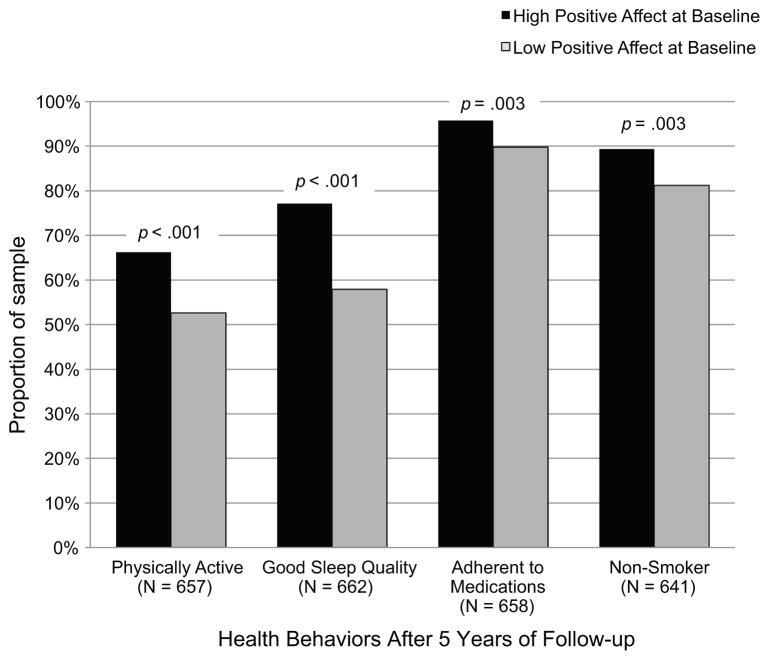
As depicted in Figure 1, participants with high positive affect at baseline were more likely to report optimal health behaviors at the 5-year follow-up. However, these associations were no longer significant after adjusting for baseline health behaviors in linear regression models for physical activity (B = 0.006, SE = 0.007, p = 0.36) and medication adherence (B = 0.005, SE = 0.003, p = 0.16), and in a logistic regression model for non-smoking (OR = 1.15; 95% CI = 0.80, 1.64; p = 0.45). Baseline positive affect predicted better sleep quality five years later, accounting for baseline sleep quality (B = 0.013, SE = 0.005, p = 0.007); this association was reduced to non-significance after additional adjustment for baseline depressive symptoms (B = 0.003, SE = 0.005, p = 0.51).
Figure 1. Health Behaviors at 5-Year Follow-Up, Split by Baseline Positive Affect.
High positive affect at baseline (PANAS ≥ median score of 32) was associated with better health behaviors 5 years later. All p-values were ≤ 0.003 in unadjusted χ² analyses.
Changes in positive affect and changes in health behaviors across five years
Descriptive statistics and bivariate correlations among 5-year changes in positive affect, depressive symptoms, and health behaviors are provided in Table S2, Supplemental Digital Content 1. In unadjusted linear regression analyses (Table 3), increases in positive affect across five years were associated with concurrent improvements in physical activity, sleep quality, and medication adherence (all p-values < 0.001). After multivariate adjustment, 5-year changes in positive affect remained significantly associated with increases in physical activity (B = 0.023, SE = 0.008, p = 0.002), sleep quality (B = 0.011, SE = 0.005, p = 0.039), and medication adherence (B = 0.014, SE = 0.004, p < 0.001). However, change in positive affect was not associated with the odds of being a non-smoker at follow-up, after adjusting for baseline smoking status and covariates (OR = 1.07; 95% CI = 0.73, 1.55; p = 0.74).
Table 3.
Five-year change in positive affect predicting 5-year change in health behaviors
| Model | Unstandardized B (SE)a
|
OR (95% CI)b | ||
|---|---|---|---|---|
| Physical activity (n = 646) | Sleep quality (n = 652) | Medication adherence (n = 641) | Non-smoker (n = 630) | |
| Unadjusted | 0.030 (0.007) | 0.017 (0.005) | 0.015 (0.004) | 1.05 (0.73, 1.49) |
| Adjusted for demographicsc | 0.029 (0.007) | 0.019 (0.005) | 0.015 (0.004) | 1.07 (0.75, 1.52) |
| Adjusted for above plus BMI, HDL cholesterol, and history of revascularization | 0.030 (0.007) | 0.019 (0.005) | 0.015 (0.004) | 1.08 (0.75, 1.56) |
| Adjusted for above plus 5-year change in depressive symptoms | 0.023 (0.008) | 0.011 (0.005) | 0.014 (0.004) | 1.07 (0.73, 1.55) |
Notes:
The unstandardized B coefficient represents change in each health behavior associated with a 1-point increase in positive affect across five years. All B coefficients for physical activity, sleep quality, and medication adherence were significant at p < 0.001, except in fully-adjusted models for physical activity (p = 0.002) and sleep quality (p = 0.039).
Because smoking status was a dichotomous variable, change in positive affect (per SD [8.9-point] increase in positive affect change score) was entered as a predictor of non-smoking at follow-up in logistic regression models. These models adjusted for baseline smoking status.
Age, education (high school graduate), low income (income < $20,000/year)
Discussion
The purpose of our study was to examine the associations between positive affect and long-term health behaviors among patients with stable coronary heart disease. In a sample of 1022 patients, baseline positive affect was cross-sectionally associated with optimal health behaviors (physical activity, sleep quality, medication adherence, and non-smoking), independent of depressive symptoms, demographics, and other confounding variables. Among 662 surviving patients who completed the follow-up exam five years later, baseline positive affect was not predictive of subsequent health behaviors after accounting for baseline health behaviors. Yet, 5-year increases in positive affect co-occurred with improvements in physical activity, sleep quality, and medication adherence. These findings contribute to the growing evidence that positive psychological states are associated with a range of health behaviors and may be involved in promoting cardiovascular health (11,16,18).
The current study supports and extends the literature on positive psychological states and health behaviors in several ways. First, much of the existing research on positive attributes and health behaviors is cross-sectional and therefore cannot evaluate long-term associations (7). Several other longitudinal investigations have found that baseline positive emotions or attitudes predict improvements in, maintenance of, or trajectories in health behaviors. For example, a study of over 2000 sedentary adults showed that, among men only, those who had more a positive outlook on life tended to show increases in physical activity six months later (38). In 153 individuals recently diagnosed with HIV, baseline positive affect predicted linkage to HIV care at 3 months post-diagnosis and antiretroviral therapy persistence across 18 months (39). Among 31 cardiac transplant patients, those who had more positive expectations pre-operation demonstrated more adherence to medical regimens 3 months post-operation (24). A study of 115 older women examined distinct trajectories in sleep quality across a decade; women with high psychological well-being were less likely to show patterns of disrupted sleep (40). Finally, evidence from smoking cessation trials suggests that positive affect is related to tobacco abstinence (41,42). In contrast, we found that positive affect did not independently predict future health behaviors, after accounting for baseline health behaviors and depressive symptoms. Our results may have differed from prior studies due to our longer follow-up period of five years, no intervention or discrete event (e.g., diagnosis or operation), as well as differences in methodology, analytic approach, and clinical sample. Yet, to our knowledge, this study is the first to show that spontaneous, natural changes (i.e., not induced by an intervention) in positive affect co-occur with health behavior change.
Second, we show that positive affect is associated with concurrent optimal health behaviors, independent of potential behavioral and motivational deficits that are characteristic of depression. Some previous studies have not accounted for psychological distress in their analyses (43,44). Our findings indicate that positive affect and depression, although related, are nevertheless distinct constructs and have separate predictive utility. Indeed, previous studies have found only moderate correlations between positive attributes (e.g., optimism, gratitude, and life satisfaction) and negative psychological states (e.g., depression, anger, and anxiety), suggesting that the presence of high positive affect does not merely imply the absence of depressive affect (8).
Third, individuals in better health may be more likely to have both high positive affect—including emotions such as active, alert, and excited—and good health habits, compared to their less-healthy counterparts. Thus, it is important to adjust for potential confounding due to physical health, but previous studies have often relied on self-reported health status rather than objective indicators. A notable strength of our study was the careful consideration for objective measures of cardiac disease severity (left ventricular ejection fraction, diastolic dysfunction, and LDL and HDL cholesterol), body mass index, comorbid medical conditions, and current medications.
Finally, much of the previous work on positive psychological states and health behaviors has been conducted on healthy participants, young adults, or adolescents. However, it is necessary to examine these processes in cardiac patients because both psychological factors and health behaviors are implicated in the progression and prognosis of cardiovascular disease. Moreover, some health behaviors—specifically, medication adherence—are more relevant for clinical populations than for disease-free or younger individuals. Our findings are therefore applicable to patients with coronary heart disease and may extend to other conditions in which health behaviors are particularly important.
Possible mechanisms
A number of mechanisms, driven by both directions of association, may be responsible for the links between positive affect and health behaviors. Individuals with higher positive affect (as measured by the PANAS) are relatively more likely to endorse feelings of being active, alert, determined, and strong; these feelings reflect energy and motivation, which are necessary for activities such as exercise. Among patients experiencing health-related stress, those who generate or sustain positive affect may be relatively better able to proactively cope with chronic stress and challenges—for example, by reappraising or reframing their setbacks in a positive light, taking action to effectively manage problems, and infusing ordinary events with meaning (45). Positive affect is also important for self-regulation, by producing favorable expectations and confidence when one is progressing towards his or her goals, as well as the ability to adjust and disengage from unattainable goals (14). Moreover, positive affect facilitates the processing of self- and goal-relevant health risk information (13). For example, previous work showed that smokers systematically processed health recommendations in a quit smoking message when they were in a positive (but not negative) mood, presumably because positive mood acts as a resource or buffer against the impact of the health message and reduces self-defensiveness (46). Alternatively, positive affect may serve as a marker for other characteristics that are predictive of health behaviors, including self-efficacy (12) or social support (47,48).
Furthermore, it is likely that improvements in health behaviors promote increases in positive affect over time. Studies using naturalistic repeated assessments in daily life have shown that physical activity produces elevations in positive affect (21), and nights of good sleep quality were followed by days with higher positive affect (22). Biological and neural processes—such as elevated proinflammatory cytokines (49) and amplified amygdala reactivity (50)—are potential pathways linking physical inactivity and poor sleep to subsequent psychological distress. However, the mechanisms whereby optimal health behaviors lead to positive well-being have yet to be delineated.
Limitations
Several limitations should be considered when interpreting the results of this study. First, the direction of causality remains unclear. It is unknown whether changes in health behaviors led to changes in positive affect or vice versa. Unmeasured confounding variables also may have contributed to both positive affect and health behaviors. An intervention for enhancing positive affect (or buffering against declines in positive affect) would be ideal for examining the influence of positive affect on subsequent health behaviors.
Second, this study was limited in its measures of health behaviors and positive affect. All health behaviors were self-reported and thus susceptible to recall or response biases. Nonetheless, self-reported measures have been shown to be valid and reliable (27,30,33). We also did not assess other important health behaviors, such as diet and sleep duration. Positive affect was measured using the PANAS (26), a validated and widely-used scale. However, the PANAS consists of high-activation positive emotions; little is known about whether low-activation positive emotions (such as feeling calm, serene, and content) are associated with health behaviors.
Lastly, our sample consisted of older, mostly male patients with stable coronary heart disease. Yet, this sample had characteristics that are representative of typical cardiac outpatients, including ethnic diversity (40% were non-White), recruitment from different types of healthcare settings, and a range of diagnoses. Positive affect was associated with lower risk of all-cause mortality in this cohort (11). Among participants alive after five years, those who returned for the follow-up exam (80% of surviving participants) had higher positive affect and better health behaviors at baseline compared to those with missing follow-up data. Our longitudinal findings were therefore based on a subsample of participants who were relatively healthier; these findings may not be valid for individuals who are in poorer psychological and physical health. Caution should be taken in generalizing the results of this study to the general population.
Implications
Although this study does not provide causal evidence for the influence of positive affect on health behaviors, the findings suggest that interventions to improve health behaviors may benefit from taking into account an individual’s level of positive affect. Interventions that aim to improve psychological well-being, rather than solely addressing maladaptive thoughts or behaviors, are effective for enhancing positive states and alleviating depressive symptoms (51,52); such interventions have been adapted for patients experiencing health-related stress (53). Randomized controlled trials of positive affect interventions—combined with patient education—have shown clinically significant increases in physical activity among patients after percutaneous coronary intervention (54) and improvements in medication adherence among hypertensive African Americans (55), compared to patient education alone. More work is needed to understand the role of positive psychological factors in the processes of health behavior maintenance and change.
Conclusions
In a prospective cohort of patients with stable coronary heart disease, positive affect was cross-sectionally associated with physical activity, sleep quality, medication adherence, and non-smoking, independent of depressive symptoms and cardiac disease severity. Furthermore, 5-year increases in positive affect co-occurred with improvements in physical activity, sleep quality, and medication adherence. Although much research has demonstrated that negative psychological states (such as depression and hostility) are detrimental for cardiovascular health, our study suggests that positive affect is associated with concurrent and long-term health behaviors. Efforts to sustain positive affect may be promising for promoting optimal health among patients with coronary heart disease.
Supplementary Material
Acknowledgments
Sources of Funding: Dr. Sin was supported by grants T32AG000212 and F32AG048698 from the National Institute on Aging. Dr. Moskowitz was supported by K24 MH093225 from the National Institute of Mental Health. The Heart and Soul Study was funded by the Department of Veteran Affairs (Epidemiology Merit Review Program), Washington, DC; grant R01 HL-079235 from the National Heart, Lung, and Blood Institute, Bethesda, Maryland; the Robert Wood Johnson Foundation (Generalist Physician Faculty Scholars Program), Princeton, New Jersey; and the American Federation for Aging Research (Paul Beeson Faculty Scholars in Aging Research Program), New York, New York.
Acronyms
- AUDIT-C
Alcohol Use Disorders Identification Test - Consumption
- BMI
body mass index
- CI
confidence interval
- HDL
high density lipoprotein
- LDL
low density lipoprotein
- LVEF
left ventricular ejection fraction
- OR
odds ratio
- PANAS
Positive and Negative Affect Schedule
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to report.
References
- 1.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802–13. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 2.Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, Newman MF. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med. 2004;66(3):305–15. doi: 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- 3.Pressman SD, Cohen S. Does Positive Affect Influence Health? Psychol Bull. 2005;131(6):925–71. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- 4.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70(7):741–56. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 5.Davidson KW, Mostofsky E, Whang W. Don’t worry, be happy: positive affect and reduced 10-year incident coronary heart disease: The Canadian Nova Scotia Health Survey. Eur Heart J. 2010 May 1;31(9):1065–70. doi: 10.1093/eurheartj/ehp603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boehm JK, Peterson C, Kivimaki M, Kubzansky L. A prospective study of positive psychological well-being and coronary heart disease. Health Psychol. 2011;30(3):259–67. doi: 10.1037/a0023124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boehm JK, Kubzansky LD. The heart’s content: The association between positive psychological well-being and cardiovascular health. Psychol Bull. 2012;138(4):655–91. doi: 10.1037/a0027448. [DOI] [PubMed] [Google Scholar]
- 8.DuBois CM, Beach SR, Kashdan TB, Nyer MB, Park ER, Celano CM, Huffman JC. Positive psychological attributes and cardiac outcomes: associations, mechanisms, and interventions. Psychosomatics. 2012;53(4):303–18. doi: 10.1016/j.psym.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 9.Brummett BH, Boyle SH, Siegler IC, Williams RB, Mark DB, Barefoot JC. Ratings of positive and depressive emotion as predictors of mortality in coronary patients. Int J Cardiol. 2005 Apr 20;100(2):213–6. doi: 10.1016/j.ijcard.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 10.Denollet J, Brutsaert DL. Reducing emotional distress improves prognosis in coronary heart disease: 9-year mortality in a clinical trial of rehabilitation. Circulation. 2001;104(17):2018–23. doi: 10.1161/hc4201.097940. [DOI] [PubMed] [Google Scholar]
- 11.Hoen PW, Denollet J, de Jonge P, Whooley MA. Positive affect and survival in patients with stable coronary heart disease: findings from the Heart and Soul Study. J Clin Psychiatry. 2013 Jul;74(7):716–22. doi: 10.4088/JCP.12m08022. [DOI] [PubMed] [Google Scholar]
- 12.Strecher VJ, DeVellis BM, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health Educ Behav. 1986;13(1):73–92. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- 13.Aspinwall LG. Rethinking the role of positive affect in self-regulation. Motiv Emot. 1998;22(1):1–32. [Google Scholar]
- 14.Rasmussen HN, Wrosch C, Scheier MF, Carver CS. Self-Regulation Processes and Health: The Importance of Optimism and Goal Adjustment. J Pers. 2006;74(6):1721–48. doi: 10.1111/j.1467-6494.2006.00426.x. [DOI] [PubMed] [Google Scholar]
- 15.Steptoe A, Wright C, Kunz-Ebrecht SR, Iliffe S. Dispositional optimism and health behaviour in community-dwelling older people: associations with healthy ageing. Br J Health Psychol. 2006;11(Pt 1):71–84. doi: 10.1348/135910705X42850. [DOI] [PubMed] [Google Scholar]
- 16.Kubzansky LD, Thurston RC. Emotional vitality and incident coronary heart disease: benefits of healthy psychological functioning. Arch Gen Psychiatry. 2007;64(12):1393–401. doi: 10.1001/archpsyc.64.12.1393. [DOI] [PubMed] [Google Scholar]
- 17.Koopmans TA, Geleijnse JM, Zitman FG, Giltay EJ. Effects of happiness on all-cause mortality during 15 years of follow-up: The Arnhem Elderly Study. J Happiness Stud. 2010;11(1):113–24. [Google Scholar]
- 18.Hoogwegt MT, Versteeg H, Hansen TB, Thygesen LC, Pedersen SS, Zwisler A-D. Exercise mediates the association between positive affect and 5-year mortality in patients with ischemic heart disease. Circ Cardiovasc Qual Outcomes. 2013;6(5):559–66. doi: 10.1161/CIRCOUTCOMES.113.000158. [DOI] [PubMed] [Google Scholar]
- 19.Boehm JK, Vie LL, Kubzansky LD. The promise of well-being interventions for improving health risk behaviors. Curr Cardiovasc Risk Rep. 2012;6(6):511–9. [Google Scholar]
- 20.Reed J, Ones DS. The effect of acute aerobic exercise on positive activated affect: A meta-analysis. Psychol Sport Exerc. 2006;7(5):477–514. [Google Scholar]
- 21.Wichers M, Peeters F, Rutten BPF, Jacobs N, Derom C, Thiery E, Delespaul P, van Os J. A time-lagged momentary assessment study on daily life physical activity and affect. Health Psychol. 2012;31(2):135–44. doi: 10.1037/a0025688. [DOI] [PubMed] [Google Scholar]
- 22.Mccrae CS, McNAMARA JP, Rowe MA, Dzierzewski JM, Dirk J, Marsiske M, Craggs JG. Sleep and affect in older adults: using multilevel modeling to examine daily associations. J Sleep Res. 2008;17(1):42–53. doi: 10.1111/j.1365-2869.2008.00621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huffman JC, DuBois CM, Mastromauro CA, Moore SV, Suarez L, Park ER. Positive psychological states and health behaviors in acute coronary syndrome patients: A qualitative study. J Health Psychol. 2014 doi: 10.1177/1359105314544135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leedham B, Meyerowitz BE, Muirhead J, Frist WH. Positive expectations predict health after heart transplantation. Health Psychol. 1995;14(1):74–9. doi: 10.1037//0278-6133.14.1.74. [DOI] [PubMed] [Google Scholar]
- 25.Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, Ali S, Dowray S, Na B, Feldman MD, Schiller NB, Browner WS. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. J Am Med Assoc. 2008;300(20):2379–88. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988 Jun;54(6):1063–70. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 27.Aadahl M, Kjær M, Kristensen JH, Mollerup B, Jørgensen T. Self-reported physical activity compared with maximal oxygen uptake in adults. Eur J Cardiovasc Prev Rehabil. 2007;14(3):422–8. doi: 10.1097/HJR.0b013e3280128d00. [DOI] [PubMed] [Google Scholar]
- 28.Bowles HR, FitzGerald SJ, Morrow JR, Jackson AW, Blair SN. Construct validity of self-reported historical physical activity. Am J Epidemiol. 2004;160(3):279–86. doi: 10.1093/aje/kwh209. [DOI] [PubMed] [Google Scholar]
- 29.Jackson AW, Morrow JR, Jr, Bowles HR, FitzGerald SJ, Blair SN. Construct validity evidence for single-response items to estimate physical activity levels in large sample studies. Res Q Exerc Sport. 2007;78(2):24–31. doi: 10.1080/02701367.2007.10599400. [DOI] [PubMed] [Google Scholar]
- 30.Kurtze N, Rangul V, Hustvedt B-E, Flanders WD. Reliability and validity of self-reported physical activity in the Nord-Trøndelag Health Study—HUNT 1. Scand J Public Health. 2008;36(1):52–61. doi: 10.1177/1403494807085373. [DOI] [PubMed] [Google Scholar]
- 31.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 32.Caska CM, Hendrickson BE, Wong MH, Ali S, Neylan T, Whooley MA. Anger expression and sleep quality in patients with coronary heart disease: findings from the Heart and Soul Study. Psychosom Med. 2009;71(3):280–5. doi: 10.1097/PSY.0b013e31819b6a08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gehi AK, Ali S, Na B, Whooley MA. Self-reported medication adherence and cardiovascular events in patients with stable coronary heart disease: the heart and soul study. Arch Intern Med. 2007;167(16):1798–803. doi: 10.1001/archinte.167.16.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bradley KA, Bush KR, McDonell MB, Malone T, Fihn SD, Project ACQI. Screening for Problem Drinking: Comparison of CAGE and AUDIT. J Gen Intern Med. 1998;13(6):379–88. doi: 10.1046/j.1525-1497.1998.00118.x. [DOI] [PubMed] [Google Scholar]
- 35.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med. 1998;158(16):1789–95. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 36.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a Brief Depression Severity Measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ren X, Ristow B, Na B, Ali S, Schiller NB, Whooley MA. Prevalence and prognosis of asymptomatic left ventricular diastolic dysfunction in ambulatory patients with coronary heart disease. Am J Cardiol. 2007;99(12):1643–7. doi: 10.1016/j.amjcard.2007.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baruth M, Lee D-C, Sui X, Church TS, Marcus BH, Wilcox S, Blair SN. Emotional outlook on life predicts increases in physical activity among initially inactive men. Health Educ Behav. 2011;38(2):150–8. doi: 10.1177/1090198110376352. [DOI] [PubMed] [Google Scholar]
- 39.Carrico AW, Moskowitz JT. Positive affect promotes engagement in care after HIV diagnosis. Health Psychol. 2014;33(7):686–9. doi: 10.1037/hea0000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Phelan CH, Love GD, Ryff CD, Brown RL, Heidrich SM. Psychosocial predictors of changing sleep patterns in aging women: a multiple pathway approach. Psychol Aging. 2010;25(4):858. doi: 10.1037/a0019622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Niemiec CP, Ryan RM, Patrick H, Deci EL, Williams GC. The energization of health-behavior change: Examining the associations among autonomous self-regulation, subjective vitality, depressive symptoms, and tobacco abstinence. J Posit Psychol. 2010;5(2):122–38. [Google Scholar]
- 42.Leventhal AM, Ramsey SE, Brown RA, LaChance HR, Kahler CW. Dimensions of Depressive Symptoms and Smoking Cessation. Nicotine Tob Res. 2008 Mar 1;10(3):507–17. doi: 10.1080/14622200801901971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Strine TW, Chapman DP, Balluz LS, Moriarty DG, Mokdad AH. The Associations Between Life Satisfaction and Health-related Quality of Life, Chronic Illness, and Health Behaviors among U.S. Community-dwelling Adults. J Community Health. 2008 Feb 1;33(1):40–50. doi: 10.1007/s10900-007-9066-4. [DOI] [PubMed] [Google Scholar]
- 44.Grant N, Wardle J, Steptoe A. The relationship between life satisfaction and health behavior: a cross-cultural analysis of young adults. Int J Behav Med. 2009;16(3):259–68. doi: 10.1007/s12529-009-9032-x. [DOI] [PubMed] [Google Scholar]
- 45.Folkman S, Moskowitz JT. Positive affect and the other side of coping. Am Psychol. 2000;55(6):647–54. doi: 10.1037//0003-066x.55.6.647. [DOI] [PubMed] [Google Scholar]
- 46.Das E, Vonkeman C, Hartmann T. Mood as a resource in dealing with health recommendations: How mood affects information processing and acceptance of quit-smoking messages. Psychol Health. 2012;27(1):116–27. doi: 10.1080/08870446.2011.569888. [DOI] [PubMed] [Google Scholar]
- 47.DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23(2):207. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 48.Steptoe A, Wardle J, Pollard TM, Canaan L, Davies GJ. Stress, social support and health-related behavior: a study of smoking, alcohol consumption and physical exercise. J Psychosom Res. 1996;41(2):171–80. doi: 10.1016/0022-3999(96)00095-5. [DOI] [PubMed] [Google Scholar]
- 49.Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 2006 Jan;27(1):24–31. doi: 10.1016/j.it.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Walker MP, van der Helm E. Overnight therapy? The role of sleep in emotional brain processing. Psychol Bull. 2009 Sep;135(5):731–48. doi: 10.1037/a0016570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol. 2009;65(5):467–87. doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- 52.Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health. 2013;13(1):1–20. doi: 10.1186/1471-2458-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moskowitz JT, Hult JR, Duncan LG, Cohn MA, Maurer S, Bussolari C, Acree M. A positive affect intervention for people experiencing health-related stress: Development and non-randomized pilot test. J Health Psychol. 2012 Jul 1;17(5):676–92. doi: 10.1177/1359105311425275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Peterson JC, Charlson ME, Hoffman Z, Wells MT, Wong S-C, Hollenberg JP, Jobe JB, Boschert KA, Isen AM, Allegrante JP. A randomized controlled trial of positive-affect induction to promote physical activity after percutaneous coronary intervention. Arch Intern Med. 2012 Feb 27;172(4):329–36. doi: 10.1001/archinternmed.2011.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ogedegbe GO, Boutin-Foster C, Wells MT, Allegrante JP, Isen AM, Jobe JB, Charlson ME. A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive African Americans. Arch Intern Med. 2012 Feb 27;172(4):322–6. doi: 10.1001/archinternmed.2011.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.