Abstract
Rationale
Sociological analyses of the psychological distress experienced by persons indirectly exposed to traumatic stressors have been conceptualized as a form of communal bereavement, defined by Catalano and Hartig (2001) as the experience of distress among persons not attached to the deceased. Their theory predicts communal bereavement responses particularly in the setting of loss of essential state, religious, or economic institutions.
Objective
To estimate the extent to which the September 11, 2001 attacks on the U.S. World Trade Center had a causal effect on psychological distress nationwide.
Methods
We used a difference-in-differences framework applied to repeated cross-sectional data from more than 300,000 participants in the 2000 and 2001 Behavioral Risk Factor Surveillance System surveys. Psychological distress was measured using three questions eliciting days of poor mental health-related quality of life. The September 11 attacks served as our exposure of interest.
Results
The September 11 attacks had a statistically significant, adverse, causal effect on psychological distress nationally. Both the magnitude and statistical significance of the estimated effects were larger in the New York City region compared to the rest of the country. Our estimates were robust to probes of the parallel trends assumption and potential sources of selection bias, as well as to falsification tests. However, these effects had largely resolved within four weeks.
Conclusions
Contrary to findings from the medical and public health literature, we conclude that the September 11 attacks did not have lasting effects on communal bereavement.
Keywords: September 11 Terrorist Attacks, Terrorism, Stress Disorders, Post-Traumatic, Disasters
INTRODUCTION
More than a decade after the September 11, 2001 attacks on the U.S. World Trade Center, its health and social consequences continue to be discussed. Both first responders as well as persons who resided in the immediate vicinity experienced a wide range of adverse health and psychosocial sequelae (Brackbill et al., 2006; Galea et al., 2002; Lin et al., 2005; U.S. Centers for Disease Control and Prevention, 2002). The September 11 attacks also led to increases in personal experiences of abuse or discrimination related to race, ethnicity, or religion (Lauderdale, 2006; Padela & Heisler, 2010). The findings of this body of literature are consistent with the documented health and social consequences of other large-scale mass casualty events, such as the 1972 Agnes Flood in the Wyoming Valley region of Pennsylvania (Logue, Hansen, & Struening, 1979), the bombing of the Alfred P. Murrah Federal Building in Oklahoma City (North et al., 1999), and Hurricane Katrina (Paxson, Fussell, Rhodes, & Waters, 2012), among others (Galea, Nandi, & Vlahov, 2005). Also of relevance to this literature are observational studies linking individual traumatic exposures and emotional distress (Devries et al., 2013; Tsai, Weiser, Dilworth, Shumway, & Riley, 2015). In twin studies, stressful life events including violent assault have been shown to be associated with the development of major depressive episodes (Kendler, Karkowski, & Prescott, 1999; Kendler et al., 1995; Kendler, Thornton, & Prescott, 2001). Econometric analyses of data obtained from men exposed to violence and other traumatic stressors through military service have demonstrated increases in suicide and motor vehicle accident-related mortality (Hearst, Newman, & Hulley, 1986); suicidal ideation and self-reported diagnosis of posttraumatic stress disorder (Cesur, Sabia, & Tekin, 2013); and smoking, heart disease, and lung cancer (Bedard & Deschênes, 2006). While other studies have yielded less precise estimates (Angrist, Chen, & Frandsen, 2010; Dobkin & Shabani, 2009), the overall thrust of the literature is that exposure to traumatic stressors has a direct, adverse, causal influence on health and mental health.
An important unanswered question is whether the September 11 attacks had a causal influence on psychological distress among people not directly affected by the event (Galea & Resnick, 2005). While numerous surveys conducted after the September 11 attacks have documented significant elevations in psychological distress among people not directly affected by the event (Galea et al., 2002; Schlenger et al., 2002; Schuster et al., 2001; Silver, Holman, McIntosh, Poulin, & Gil-Rivas, 2002), few of these estimates have a casual interpretation given their lack of a counterfactual framework or availability of pre-September 11 measures. To address this gap in the literature, we analyzed repeated cross-sectional data collected nationwide through the 2000 and 2001 Behavioral Risk Factor Surveillance System (BRFSS) surveys, employing a difference-in-differences framework to explore the causal relationship between the September 11 attacks and psychological distress nationwide.
CONCEPTUAL FRAMEWORK
By definition, the diagnosis of posttraumatic stress disorder requires “exposure to an extreme traumatic stressor,” either through “direct personal experience of an event,” “witnessing an event,” or “learning about” the event (American Psychiatric Association, 2000) (p.463). Indirect exposures to traumatic stressors may be salient to psychotherapists and family members who experience psychological distress as a result of their affiliation with a traumatized person (a concept that has been described as “secondary trauma” (Figley, 1983) or “vicarious trauma” (McCann & Pearlman, 1990)); or they may occur through other channels like word of mouth, witnessing a distressing event from afar, or even viewing media images of a distressing event (Ahern et al., 2002; Bernstein et al., 2007; Holman, Garfin, & Silver, 2014; Neria & Sullivan, 2011; Silver et al., 2013). Precise classification of the psychological distress resulting from such indirect exposures has so far eluded the field. North and Pfefferbaum (2002) argued that exposure to a distressing event through the viewing of media images is unlikely to meet the diagnostic criteria for “witnessing.” Neither the fourth edition, nor the recently published fifth edition, of the Diagnostic and Statistical Manual of Mental Disorders provide detailed guidance about the potential mechanisms through which indirect exposure may occur (American Psychiatric Association, 2000, 2013).
Sociological analyses of the psychological distress experienced by persons indirectly exposed to traumatic stressors have conceptualized these spillover impacts as a form of “communal bereavement” (Hawdon, 2009). Catalano and Hartig (2001) defined communal bereavement in response to loss as “the widespread experience of distress among persons who never met the deceased” (p.333), particularly when the loss implicates the “failure of institutions essential to the normal functioning of the community” (p.334). Using an interrupted time-series design, they showed that the incidence of very low birth weight increased in Sweden immediately subsequent to two events of nationwide salience to Swedish citizens. In the U.S., the September 11 attacks provided the most relevant example of a recent event that could provide an occasion for psychological distress on a national scale (Alexander, Eyerman, Giesen, Smelser, & Sztompka, 2004), given that the events crystallized for many Americans the fear that the U.S. could be vulnerable to attack on a scale previously unimagined. The most highly cited studies in the medical literature provide descriptive point prevalence estimates consistent with heightened levels of psychological distress in the days to weeks following the September 11 attacks (Galea et al., 2002; Schlenger et al., 2002; Schuster et al., 2001; Silver, Holman, McIntosh, Poulin, & Gil-Rivas, 2002). Rates of alcohol and other substance use were similarly elevated (DiMaggio, Galea, & Li, 2009; Vlahov et al., 2002). Other studies in this literature have focused on the extent to which viewing media images (e.g., on television) of the September 11 attacks, and other mass casualty events, may contribute to symptoms of depression or posttraumatic stress (Ahern et al., 2002; Bernstein et al., 2007; Holman, Garfin, & Silver, 2014; Neria & Sullivan, 2011; Silver et al., 2013). In general, however, we are fairly limited in our ability to draw robust inferences from this literature about the extent to which the September 11 attacks had a causal influence on psychological distress among persons indirectly exposed to the event.
This is an important and heretofore unresolved issue of public importance in the study of health and social behavior because mental and substance use disorders account for a large portion of disability-adjusted life years worldwide - with the largest shares attributable to mood and anxiety disorders like major depressive disorder and post-traumatic stress disorder (Murray et al., 2013; Whiteford et al., 2013). The economic burden of these conditions is substantial, with the most recent estimates from 2000 suggesting that depressive and anxiety disorders combined accounted for more than $80 billion in direct costs, mortality costs, and lost productivity (Greenberg et al., 2003; Greenberg et al., 1999). Even subthreshold symptoms that are clinically significant, but do not meet diagnostic criteria, have important social and economic consequences (Judd, Paulus, Wells, & Rapaport, 1996; Judd, Schettler, & Akiskal, 2002).
Three studies from the literature on the September 11 terrorist attacks and communal bereavement, drawn from public health, sociology, and economics, are most similar to ours. Ford, Udry, Gleiter, and Chantala (2003) and Knudsen, Roman, Johnson, and Ducharme (2005) conducted cross-sectional analyses of the National Longitudinal Study of Adolescent Health and the National Employee Survey. They sought to assess the extent to which temporal proximity to September 11, 2001 was associated with changes in mental health-related outcomes like psychological distress and substance use. Their key identifying assumption was that the timing of the study interviews relative to September 11 was randomly distributed. While their approach was similar to modern regression-discontinuity designs (Bor, Moscoe, Mutevedzi, Newell, & Barnighausen, 2014), the authors did not follow this literature in formally testing their identifying assumptions. Metcalfe, Powdthavee, and Dolan (2011) used panel data from the British Household Panel Survey and applied a difference-in-differences approach with participant fixed effects to estimate the causal influence of the September 11 attacks on psychological distress in the United Kingdom. All three studies found that the September 11 attacks were associated with heightened levels of psychological distress.
The empirical contribution of our study is fourfold. First, in comparison to Ford, Udry, Gleiter, and Chantala (2003) and Knudsen, Roman, Johnson, and Ducharme (2005), we used a broader sample of data. Ford, Udry, Gleiter, and Chantala (2003) analyzed data from a national survey of young adults, while Knudsen, Roman, Johnson, and Ducharme (2005) analyzed data from a national survey of employed Americans. The BRFSS surveys are nationally representative, thereby enabling us to generalize our findings beyond young adults or employed persons to the non-institutionalized U.S. population. Second, our use of data from 2000 permitted us not only to examine whether there were differences in psychological distress before and after September 11 in 2001, but also to do so in the context of a differences-in-differences design, which would allay concerns that seasonal effects may have contaminated the findings reported by Ford et al. (2003) and Knudsen et al. (2005). Third, the analysis by Metcalfe, Powdthavee, and Dolan (2011), which is methodologically most similar to the present work, focuses mainly on year-by-year and month-by-month comparisons in psychological distress. Our study permitted a more detailed, week-by-week assessment of the elevations in, and subsequent resolution of, psychological distress. Fourth, in addition to estimating changes in psychological distress, we conducted falsification tests (Prasad & Jena, 2013) by estimating changes in outcomes a priori not expected to be affected by the September 11 attacks. We also more formally evaluated whether the timing of the September 11 attacks was indeed exogenous with respect to the BRFSS surveys. Thus, we were able to test the assumptions underlying the Ford, Udry, Gleiter, and Chantala (2003), Knudsen, Roman, Johnson, and Ducharme (2005), and Metcalfe, Powdthavee, and Dolan (2011) studies in a more direct manner.
DATA AND METHODS
Ethics Statement
As this manuscript relies solely on public-use data from the Behavioral Risk Factor Surveillance Survey, ethics approval was not required.
The Behavioral Risk Factor Surveillance System (BRFSS)
The BRFSS is a large, ongoing, nationally representative, telephone-based survey, conducted annually by state health departments and the health departments of the District of Columbia and several inhabited territories, with technical assistance and support from the U.S. Centers for Disease Control and Prevention (Mokdad, 2009). For this analysis, we pooled the data from the 2000 and 2001 BRFSS surveys. During these years, the health departments of three inhabited territories also participated in the BRFSS (Guam, Puerto Rico, and the U.S. Virgin Islands), but these data were excluded from estimation.
Measures
Since 1993, the BRFSS has included core “healthy days” health-related quality of life (HRQOL) questions (Hennessy, Moriarty, Zack, Scherr, & Brackbill, 1994; U.S. Centers for Disease Control and Prevention, 1994), with five “supplemental” symptom-related HRQOL questions added in 1995 (U.S. Centers for Disease Control and Prevention, 1998). These measures have been shown to have acceptable internal validity, construct validity, criterion-related validity, and test-retest reliability, and are generally regarded as valid and reliable measures of HRQOL (Moriarty, Zack, & Kobau, 2003; U.S. Centers for Disease Control and Prevention, 2000). For this analysis, we were primarily interested in HRQOL outcomes related to mental health. Each implementing state health department has flexibility to participate in specific modules or add survey questions based on state health priorities. Thus, not all states collected data on all of the outcome variables each year. This “healthy days” mental health question was administered in all participating states in 2000 and 2001: “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” (Appendix A). As secondary outcomes, we analyzed two additional questions that were administered in a partial sample of participating states: “During the past 30 days, for about how many days have you felt sad, blue, or depressed?” and “During the past 30 days, for about how many days have you felt worried, tense, or anxious?” The three variables can be combined into a single mental health summary index with good internal consistency (Horner-Johnson, Krahn, Andresen, & Hall, 2009).
Statistical Analysis
The Stata statistical software package was used for statistical analysis (version 13.1 for Mac, StataCorp LP, College Station, Tex.). All estimates were weighted with the BRFSS-provided sampling weights, with robust estimates of variance corrected for clustering at the level of the county (Froot, 1989; Rogers, 1993; Williams, 2000). We pooled the 2000 and 2001 data and employed a difference-in-differences framework (Card & Krueger, 1994; Meyer, 1995) to assess the extent to which the pre/post-September 11 differences in outcomes were different in 2001 compared to 2000, fitting the following least squares regression model:
where Yi represents the outcome for participant i and Ti represents the timing of the BRFSS interview for participant i, flexibly parameterized as a vector of ten dummy variables representing the period (in any given year) between January 1 and August 13, the four one-week periods prior to September 11, the four one-week periods following September 11, and the period between October 9 and December 31. Although the most flexible specification would have been to include 52 dummy variables corresponding to the 52 one-week periods in any given year, we aggregated the time periods outside of the assessment window of interest (January 1–August 13 and October 9–December 31) for the sake of parsimony. We revisited this aggregation in a sensitivity analysis. These specific periods were chosen so that we could examine week-by-week changes in the outcomes for a four-week period prior to September 11 and for a four-week period beginning on September 11. The Xi represent socio-demographic variables, as well as known correlates of psychological distress, including: age, race, gender, marital status, educational attainment, unemployment, and income. We also adjusted for the number of calling occasions required to reach the study participant. Finally, we included day-of-week (δi), month (γi), and year (φi) fixed effects to account for circaseptum cycles (Helliwell & Wang, 2014; Larsen & Kasimatis, 1990; Stone, Schneider, & Harter, 2012; Taylor, 2006; Tumen & Zeydanli, 2014) and seasonal or other systematic variations in subjective well-being (Briere, Downes, & Spensley, 1983; Rosenthal et al., 1984; Schwarz & Clore, 1983; Smith, 1979).
The estimated parameters of interest are the β, with a specific focus on the estimated regression coefficients corresponding to the four one-week periods after September 11. Statistically significant positive coefficients on the time period-by-year dummy variables indicate worsened mental health in the post-September 11 period in 2001 compared to 2000. We employed Wald-type F-tests to assess for the joint statistical significance of the coefficient estimates on the four product terms corresponding to the four-week period after September 11. Thus, the regression models we fitted to the data advance beyond those used in Ford, Udry, Gleiter, and Chantala (2003) and Knudsen, Roman, Johnson, and Ducharme (2005) in that participants who were interviewed on the same days of the month in 2000 served as an additional comparison group. The double differencing purges our estimates of bias that could result from secular trends in the outcomes unrelated to the September 11 attacks. In addition, as described above, our analyses accounted for the number of calling occasions required and day-to-day and other systematic variations in subjective well-being. Interpretation of our estimates as causal relies on the exogeneity of the September 11 attacks with respect to the timing of the interviews, the correct specification of our regression model, lack of confounding from unobserved variables (i.e., aside from those that were constant across participants, which would be accounted for with the time fixed effects), and other assumptions as described in more detail below.
To determine whether any observed effects could have been sustained over a longer period of time, in a secondary analysis we doubled the length of the assessment window. We flexibly parameterized the timing of the interview as a series of 18 dummy variables representing the period (in any given year) between January 1 and July 16, the eight one-week periods prior to September 11, the eight one-week periods following September 11, and the period between November 6 and December 31. As with the primary analysis, we employed Wald-type F-tests to assess for the joint statistical significance of the coefficient estimates on the four product terms corresponding to the second four-week period from October 9 to November 5.
Although the theory of communal bereavement elaborated by Catalano and Hartig (2001) does not suggest geographic specificity, it is reasonable to expect that persons who more closely identify with the failed institutions may experience more heightened levels of psychological distress. Therefore we explored the extent to which any observed elevations in psychological distress in the four weeks after September 11, 2001 compared with the four weeks after September 11, 2000 were greater in the New York City region compared with the rest of the country. The metropolitan statistical areas of focus were New York City, New York; Newark, New Jersey; and Jersey City, New Jersey.
Robustness Checks
The internal validity of the differences-in-differences framework rests on the “parallel trends” assumption, which requires similar pre-treatment trajectories in the outcomes of interest for both the treatment and comparison groups, as well as the assumption that that the observed trends would have continued had the treatment not been administered. In the case of the present study, this assumption stipulates that trends in mental health outcomes prior to the September 11 attacks were similar for BRFSS participants who were interviewed in 2000 compared to those who were interviewed in 2001, and that these trends would have continued had the September 11 attacks not occurred. Therefore, we explored temporal changes in mental health outcomes prior to September 11 (in both 2000 and 2001) to explore the validity of this assumption. We also explored the extent to which the same patterns were observed in the data for 1997, 1998, and 1999.
Second, in addition to potential violations of the parallel trends assumption, selection bias could have affected our results. As described previously, not all states participated in the supplemental HRQOL module. Because each implementing state health department has flexibility to participate in specific modules based on state health priorities, it is possible that states with worse population mental health (and greater susceptibility to the psychological impacts of the September 11 attacks) would be overrepresented in the analyses of the HRQOL outcomes derived from the supplemental module. Because the “healthy days” mental health question was administered in all states in 2000 and 2001, we checked for this potential bias by simply assessing the extent to which the estimates from that regression model were consistent with the other two variables (and the mental health summary index). We also used t-tests to determine whether the states that participated in the supplemental HRQOL module had similar levels of mentally “healthy days” compared to states that did not participate.
Third, differential selection into the BRFSS sample could represent an important source of bias. Specifically, factors related to the exposure could have enriched the post-September 11, 2001 sample for mental health problems, thereby biasing our estimates away from the null (Galea et al., 2003). On its face, we believe this possibility to be unlikely given that, in general, persons with higher socioeconomic status, persons with less psychiatric comorbidity, and persons who do not engage in unhealthy risk behaviors are more likely to participate in such surveys (Galea & Tracy, 2007). Furthermore, our regression models adjust for the number of calling occasions required to reach the study participant. Nevertheless, we also assessed the extent to which selection bias could have affected our results by analyzing trends in the daily and weekly volume of completed surveys to determine whether a lower volume of completed surveys was observed after the September 11 attacks. We also explicitly examined the possibility of bias resulting from changing sample composition by examining whether socio-demographic characteristics of respondents were different before vs. after September 11 in 2001 compared to 2000. In this analysis, we used the same difference-in-differences framework as the primary analysis, except that age, race, gender, marital status, educational attainment, unemployment, income, and number of calling occasions required were specified as the dependent variable (in eight separate regression models). We then employed Wald-type F-tests to assess for the joint statistical significance of the coefficient estimates on the four product terms corresponding to the four-week period after September 11.
Finally, we analyzed physical HRQOL as a falsification test. As this variable was a priori not expected to be affected by the September 11 attacks, finding an association between the event and physical HRQOL would suggest bias in our study design (Prasad & Jena, 2013). The physical health summary index was constructed in a manner similar to the mental health summary index also has comparable internal consistency (Horner-Johnson, Krahn, Andresen, & Hall, 2009). Because the physical health summary index could potentially capture somatization of psychological distress, we analyzed a number of other falsification outcomes as well, including current pregnancy (among women), body mass index, and history of asthma. The question about current pregnancy was administered only to women. Body mass index was defined as self-reported weight (in kilograms) divided by self-reported height (in meters) squared. Finally, history of asthma was elicited with the question, “Have you ever been told by a doctor, nurse, or other health professional that you had asthma? These specific outcomes were selected because indicators of physical health and physical attributes were considered a priori unlikely to be affected by the exposure.
RESULTS
Characteristics of the pooled sample are shown in Table 1. In any given year, approximately 15 percent of the surveys were administered in the eight-week window from August 14 through October 8. The pooled mean number of days (in the past 30 days) with poor mental health was 3.4 (standard deviation [SD], 7.6). For the other two mental health questions that were administered in a subsample of states, the mean number of days feeling sad, blue, or depressed was similar (mean, 3.3; SD, 7.0), while the number of days feeling worried, tense, or anxious was greater (mean, 5.4; SD, 8.8). The combined mental health summary index had a mean of 3.9 (SD, 6.6), with good internal consistency according to conventional rules of thumb (Cronbach’s alpha, 0.80).
Table 1.
Summary characteristics for the pooled sample
| 2000 BRFSS | 2001 BRFSS | |||
|---|---|---|---|---|
| N | Pct. | N | Pct. | |
| Date of interview | ||||
| January 1–August 13 | 111,658 | 60.5 | 133,731 | 62.9 |
| August 14–20 | 3,104 | 1.7 | 3,929 | 1.8 |
| August 21–27 | 1,811 | 1 | 1,573 | 0.7 |
| August 28–September 3 | 1,056 | 0.6 | 724 | 0.3 |
| September 4–10 | 4,132 | 2.2 | 5,366 | 2.5 |
| September 11–17 | 4,621 | 2.5 | 4,653 | 2.2 |
| September 18–24 | 3,261 | 1.8 | 3,969 | 1.9 |
| September 25–October 1 | 2,506 | 1.4 | 2,572 | 1.2 |
| October 2–8 | 5,552 | 3 | 5,764 | 2.7 |
| October 9–December 31 | 46,749 | 25.3 | 50,229 | 23.6 |
| Mental health summary index (mean [s.d.]) | 3.87 | 6.33 | 4.06 | 6.58 |
| Days with poor mental health (mean [s.d.]) | 3.31 | 7.47 | 3.48 | 7.69 |
| Days sad, blue, or depressed (mean [s.d.]) | 3.26 | 6.75 | 3.41 | 6.99 |
| Days worried, tense, or anxious (mean [s.d.]) | 5.32 | 8.57 | 5.55 | 8.79 |
| Age, years (mean [s.d.]) | 46.9 | 17.2 | 47.3 | 17.2 |
| Non-Hispanic white | 143,510 | 78.3 | 161,650 | 76.9 |
| Female | 109,680 | 59.5 | 126,048 | 59.3 |
| Married | 99,085 | 53.9 | 112,604 | 53.2 |
| Educational attainment | ||||
| Incomplete high school | 22,041 | 12 | 25,135 | 11.9 |
| High school graduate | 58,049 | 31.6 | 66,517 | 31.4 |
| Incomplete college | 50,664 | 27.5 | 57,316 | 27.1 |
| College graduate | 53,225 | 28.9 | 62,912 | 29.7 |
| Unemployed or unable to work | 14,076 | 7.6 | 18,029 | 8.5 |
| Annual household income | ||||
| Less than $25,000 | 51,582 | 32.6 | 57,313 | 31.7 |
| $25,000–49,999 | 55,794 | 35.3 | 61,665 | 34.1 |
| $50,000 or greater | 50,784 | 32.1 | 61,832 | 34.2 |
| Number of calling occasions | ||||
| One call | 43,764 | 23.7 | 49,435 | 23.3 |
| 2–3 calls | 53,379 | 28.9 | 60,998 | 28.7 |
| ≥4 calls | 87,307 | 47.3 | 102,077 | 48 |
During the eight-week window of interest, relatively flat trajectories of psychological distress were observed nationwide prior to September 11 in either 2000 or 2001 (Figure 1). Prior to September 11, the trajectories for 2001 closely match those for 2000, suggesting no violations of the parallel trends assumption. The same pre-September 11 patterns in the data are observed in 1997, 1998, and 1999 (Appendix B). Foreshadowing our difference-in-differences estimates, after September 11, an upward trajectory in psychological distress was observed in 2001 but not in 2000. The average mental health summary index increased from 3.9 (SD, 6.5) during January 1–September 10, 2001 to 4.6 (SD, 6.4) during September 11–October 8, 2001, and then declined to 4.3 (SD, 6.8) during October 9–December 31, 2001.
Figure 1.
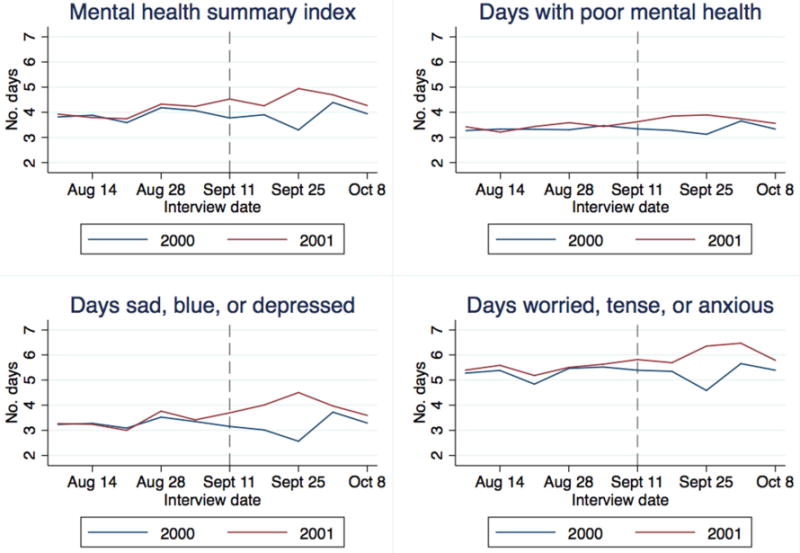
Week-by-week trends in psychological distress in the eight-week window from August 14 through October 8 in 2000 vs. 2001
Table 2 presents coefficient estimates for the difference-in-differences regression models, specifically focusing on the product terms between the dummy variable for 2001 and the four one-week periods from September 11–October 8. (The full set of regression estimates appears in Appendix C.) In the analysis of the mental health summary index, three of the four product terms were positive and two were statistically significant. An F-test confirmed the joint statistical significance of the product terms (F=4.3, P=0.003), suggesting that psychological distress was elevated in the four weeks following September 11, 2001 compared with the four weeks following September 11, 2000. When the three variables that comprise the mental health summary index were examined as separate outcomes, qualitatively similar patterns were observed in the product terms, with P-values for the F-tests ranging from <0.001 to 0.14. The magnitudes of the regression coefficients indicate that participants reported approximately 1–2 additional days of poor mental HRQOL, depending on the specific outcome, in the four weeks after September 11, 2001 compared with the four weeks after September 11, 2000. Focusing specifically on the one-week time period for which the estimates were the most consistently precise (September 25–October 1, 2001), when compared to the sample means these estimates suggest relative increases ranging from 25–60 percent, and when compared to the sample standard deviations these estimates translated into effect sizes of 0.11–0.28 standard deviation units.
Table 2.
Psychological impacts of the September 11 attacks, August 14–October 8
| Mental health summary index | Days with poor mental health | Days sad, blue, or depressed | Days worried, tense, or anxious | |||||
|---|---|---|---|---|---|---|---|---|
| Coef. | Std. err. | Coef. | Std. err. | Coef. | Std. err. | Coef. | Std. err. | |
| Year × time period interaction | ||||||||
| January 1–August 13, 2001 | Ref | Ref | Ref | Ref | ||||
| August 14–20, 2001 | −1.533** | 0.517 | −1.332*** | 0.367 | −0.676 | 0.497 | −1.277 | 0.796 |
| August 21–27, 2001 | 0.381 | 0.691 | −0.107 | 0.492 | 0.493 | 0.565 | 0.546 | 1.006 |
| August 28–September 3, 2001 | 0.715 | 1.523 | 0.092 | 0.735 | 0.597 | 1.558 | 0.850 | 1.404 |
| September 4–10, 2001 | 0.035 | 0.546 | −0.198 | 0.363 | −0.298 | 0.626 | −0.549 | 0.634 |
| September 11–17, 2001 | 0.860* | 0.426 | −0.261 | 0.224 | 1.211** | 0.427 | 0.523 | 0.706 |
| September 18–24, 2001 | −0.537 | 0.882 | −0.191 | 0.554 | 0.375 | 0.588 | −0.890 | 1.128 |
| September 25–October 1, 2001 | 1.586*** | 0.444 | 0.849 | 0.433 | 1.966*** | 0.432 | 1.417* | 0.542 |
| October 2–8, 2001 | 0.156 | 0.569 | −0.160 | 0.329 | 0.591 | 0.515 | 0.240 | 0.828 |
| October 9–December 31, 2001 | 0.224 | 0.157 | 0.157 | 0.108 | 0.188 | 0.189 | 0.178 | 0.247 |
| F-test for the year × time period interactions for September 11–October 8 | F=4.30 (P=0.003) | F=2.19 (P=0.07) | F=7.53 (P<0.001) | F=1.76 (P=0.14) | ||||
p<0.05;
p<0.01;
p<0.001
There was evidence of geographic specificity. Depending on the specific outcome, there was more than a twofold difference in the magnitudes of the estimated effects among persons in the New York City region compared with the rest of the country (Appendix D). The statistical significance of these estimates was also greater among persons in the New York City region, with F-statistics ranging from 4.52–13.9 (and P-values ranging from <0.001 to 0.02), compared with persons in the rest of the country (F-statistics ranged from 1.14–5.53 and P-values ranged from <0.001 to 0.34).
The effects of the September 11 attacks did not appear to consistently extend beyond four weeks. Visual inspection of the trends in psychological distress in the 16-week window from July 17 through November 5 in 2000 compared with 2001 suggested that mean levels of psychological distress had returned to their baseline after four weeks (Appendix E). The product terms corresponding to the period from October 9–November 5 did not achieve joint statistical significance (F=0.84, P=0.50). When the three variables that comprise the mental health summary index were examined as separate outcomes, only the regression model for poor mental health days had statistically significant product terms (F=3.01, P=0.02). The relevant product terms in the regression models for the other two variables did not achieve joint statistical significance, with F-statistics ranging from 1.12–1.52 (and P-values ranging from 0.20–0.35). Finally, including a full set of dummy variables corresponding to all 52 one-week periods yielded no appreciable differences compared with the estimated treatment effects shown in Table 2, with F-tests ranging from 3.14–4.83 (and P-values ranging from <0.001 to 0.02).
Our estimates were robust to a series of checks. First, there did not appear to be evidence of selection (at the state level) into participation in the supplemental HRQOL module. In the 2000 BRFSS, the average number of days with poor mental health was similar among participants whose state health departments participated in the module vs. those whose states did not (3.222 vs. 3.223; t=0.23, P=0.82); a statistically significant difference was observed in the 2001 BRFSS, but the magnitude of the difference was negligible (3.15 vs. 3.25; t=3.47, P<0.001). Second, there did not appear to be any systematic changes in the daily volume of completed surveys around the September 11 attacks (Appendix F). Third, we used difference-in-differences to examine the possibility that the September 11 attacks induced substantive compositional changes in the pool of study participants. These regression models were similar to our primary analysis, except that the observed participant characteristics (age, race, gender, marital status, educational attainment, unemployment, income, and number of calling occasions required) were specified as the dependent variables. The P-values corresponding to the F-tests ranged from <0.001 to 0.94, but any differences that were statistically significant (due to the large sample size) were small in magnitude. Appendix G provides a graphical display of trends in the four socio-demographic variables for which the F-tests showed the strongest degree of statistical significance (P-values ranged from <0.001 to 0.20), and the lack of substantive differences is apparent. Fourth, the falsification tests yielded null results (Appendix H). Namely, the September 11 attacks did not lead to increases in reported pregnancy (among women) or asthma, worsened physical health, or increased obesity. The F-test values were all less than 2, with P-values ranging from 0.20–0.95.
DISCUSSION
In this population-based study, we used a difference-in-differences framework to show that the September 11, 2001 attacks on the U.S. World Trade Center had a causal effect on psychological distress nationally. The mean increase in the number of days of poor mental HRQOL is equivalent to the excess burden observed among American Indians and Alaska Natives (Jia, Muennig, Lubetkin, & Gold, 2004) and is consistent with what is known about historically-ingrained mental health disparities in the U.S. (Beals et al., 2005). However, the impacts had largely resolved within four weeks of the event. In contrast to the previous studies by Ford, Udry, Gleiter, and Chantala (2003) and Knudsen, Roman, Johnson, and Ducharme (2005), our empirical strategy and falsification tests permit a causal interpretation. The interpretation of our estimates as causal relies on the usual assumptions that the regression model was correctly specified, that there was no unmeasured confounding after adjustment for covariates (i.e., socio-demographic variables, calling occasions, and time fixed effects), and that the timing of the September 11 attacks were exogenous with respect to the timing of the interviews. In this vein, our study builds on the robust methodological approach of Metcalfe, Powdthavee, and Dolan (2011) but applies it to data from the U.S. context. We additionally improved upon that study by using data that permitted more detailed, week-by-week assessments of the elevations in, and subsequent resolution of, psychological distress.
An important strength of our study in comparison to previous work is that we were able to address two important potential sources of bias. First, as discussed previously, the difference-in-differences study design relies on the counterfactual assumption that trends in psychological distress would have been the same in 2001 (compared with trends in 2000) in the absence of the September 11 attacks. Differential macro trends in 2001 prior to the attacks (compared with trends prior to September 11, 2000) could certainly bias our estimates. While this counterfactual assumption cannot be directly refuted, it can be indirectly assessed by examining trends in outcomes prior to the exogenous shock for the exposed and unexposed. We explored the validity of this parallel trends assumption by presenting graphical displays of the raw data that clearly demonstrate this assumption was met. Second, while unlikely, it is possible that the post-September 11, 2001 sample could have been enriched for mental health comorbidity. However, we adjusted for known socio-demographic confounders, demonstrated that there were no systematic changes in the volume of completed surveys around the September 11 attacks, and showed that there was no evidence that the September 11 attacks induced substantive compositional changes in the pool of study participants. Taken together, these robustness checks increase our confidence in the conclusion that the September 11 attacks had a short-lived, causal effect on psychological distress nationally.
Limitations
The principal limitations of our study related to the primary outcome variables, both of which would suggest caution in interpreting the magnitudes of the estimated effects. First, the primary outcome variables were based on a 30-day measurement window. There is no consensus on the “optimal” recall period for measures of psychological distress in general (Stull, Leidy, Parasuraman, & Chassany, 2009), but given our specific study design and exposure of interest, the regression models ideally would have used psychological distress outcomes with measurement windows smaller by an order of magnitude (e.g., past 24 hours, or past 7 days). Such variables, however, are not available in the BRFSS data. For participants interviewed after September 11 in either 2000 or 2001, depending on how soon after September 11 they were interviewed, the 30-day measurement window potentially lumps together changes in psychological distress before September 11 with changes in psychological distress after September 11. Our estimates indicate that study participants reported approximately 1–2 additional days of poor mental HRQOL in the four weeks after September 11, 2001 compared with the four weeks after September 11, 2000. Thus, our results are still consistent with post-September 11 effects, given that aggregation over the 30-day measurement window would have had the effect of substantially biasing our estimates toward the null. Furthermore, our findings are consistent with previous validation studies showing that the “healthy days” variables are responsive to short-term changes (Moriarty, Kobau, Zack, & Zahran, 2005; Moriarty, Zack, & Kobau, 2003). A second limitation is that our outcome variables did not permit us to make inferences about the extent to which the September 11 attacks could have led to incident major depressive disorder, post-traumatic stress disorder, or other mental disorders consistent with the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2000). Nor were we able to assess the extent to which the observed changes in psychological distress resulted in actual functional impairment. That being said, even subthreshold depressive symptoms that do not meet diagnostic criteria have important social and economic consequences (Judd, Paulus, Wells, & Rapaport, 1996; Judd, Schettler, & Akiskal, 2002). Transient elevations in psychological distress are consistent with normal bereavement responses in response to individually experienced stressful life events (Horwitz & Wakefield, 2007; Wakefield, Schmitz, First, & Horwitz, 2007) or (as we argue on the basis of the data presented in this article) to nationally experienced losses of essential institutions. More data would be needed to extend our conclusions to clinically significant pathology (e.g., major depressive disorder or post-traumatic stress disorder).
Conclusions
Notwithstanding these important limitations, our findings suggest not only the salience of large-scale traumatic events for those who experience them indirectly but also resilience in that these impacts may, on average, be relatively short-lived. Viewed through the lens of Catalano and Hartig (2001)’s theory of communal bereavement, our estimates are consistent with the theory that widespread psychological distress could be experienced by persons who were not directly affected by a major event in the life of the nation. On the other hand, the observed elevations in psychological distress had largely abated within four weeks. In this respect our findings are consistent with those of Schlenger et al. (2002), who showed that the levels of clinically significant psychological distress in a nationally representative sample of adults in the U.S. returned to within normal limits 1–2 months following the September 11 attacks. Future research may focus on identifying the kinds of mass casualty events that generate communal bereavement, identifying specific subgroups that may experience the largest and most meaningful changes in psychological distress, and understanding the role of community-level factors in building resilience. While our results demonstrate short-term resilience on average, there may be significant heterogeneity in effects (e.g., by prior psychiatric history and/or access to social institutions such as religious or community organizations). Understanding such heterogeneity may enrich our understanding of the mechanisms underpinning communal bereavement and interventions to target any possible significant health, social, and economic consequences of the events leading to such phenomena.
Supplementary Material
HIGHLIGHTS.
Losses of nationally significant institutions may result in communal bereavement.
This study explores national distress after the September 11 terrorist attacks.
Our study estimates are based on the method of difference-in-differences.
The attacks had an adverse causal effect on psychological distress nationally.
The estimated psychological impacts were, on average, relatively short-lived.
Acknowledgments
No specific funding was received for this study. ACT acknowledges salary support from U.S. National Institutes of Health K23 MH096620 and the Robert Wood Johnson Health and Society Scholars Program. No funders had any role in the collection, analysis, or interpretation of data; in the writing of the article; or in the decision to submit it for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahern J, Galea S, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, Vlahov D. Television images and psychological symptoms after the September 11 terrorist attacks. Psychiatry. 2002;65(4):289–300. doi: 10.1521/psyc.65.4.289.20240. [DOI] [PubMed] [Google Scholar]
- Alexander JC, Eyerman R, Giesen B, Smelser NJ, Sztompka P. Cultural trauma and collective identity. Berkeley: University of California Press; 2004. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, D.C: American Psychiatric Association; 2000. (text rev.) [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington: American Psychiatric Publishing; 2013. [Google Scholar]
- Angrist JD, Chen SH, Frandsen BR. Did Vietnam veterans get sicker in the 1990s? The complicated effects of military service on self-reported health. Journal of Public Economics. 2010;94(11–12):824–837. [Google Scholar]
- Beals J, Manson SM, Whitesell NR, Spicer P, Novins DK, Mitchell CM. Prevalence of DSM-IV disorders and attendant help-seeking in 2 American Indian reservation populations. Archives of General Psychiatry. 2005;62(1):99–108. doi: 10.1001/archpsyc.62.1.99. [DOI] [PubMed] [Google Scholar]
- Bedard K, Deschênes O. The long-term impact of military service on health: evidence from World War II and Korean War veterans. American Economic Review. 2006;96(1):176–194. doi: 10.1257/000282806776157731. [DOI] [PubMed] [Google Scholar]
- Bernstein KT, Ahern J, Tracy M, Boscarino JA, Vlahov D, Galea S. Television watching and the risk of incident probable posttraumatic stress disorder: a prospective evaluation. Journal of Nervous and Mental Disease. 2007;195(1):41–47. doi: 10.1097/01.nmd.0000244784.36745.a5. [DOI] [PubMed] [Google Scholar]
- Bor J, Moscoe E, Mutevedzi P, Newell ML, Barnighausen T. Regression discontinuity designs in epidemiology: causal inference without randomized trials. Epidemiology. 2014;25(5):729–737. doi: 10.1097/EDE.0000000000000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brackbill RM, Thorpe LE, DiGrande L, Perrin M, Sapp JH, Wu D, 2nd, Thomas P. Surveillance for World Trade Center disaster health effects among survivors of collapsed and damaged buildings. Morbidity and Mortality Weekly Report Surveillance Summaries. 2006;55(2):1–18. [PubMed] [Google Scholar]
- Briere J, Downes A, Spensley J. Summer in the city: urban weather conditions and psychiatric emergency-room visits. Journal of Abnormal Psychology. 1983;92(1):77–80. doi: 10.1037//0021-843x.92.1.77. [DOI] [PubMed] [Google Scholar]
- Card D, Krueger AB. Minimum wages and employment: a case study of the fast-food industry in New Jersey and Pennsylvania. American Economic Review. 1994;84(4):772–793. [Google Scholar]
- Catalano R, Hartig T. Communal bereavement and the incidence of very low birthweight in Sweden. Journal of Health and Social Behavior. 2001;42(4):333–341. [PubMed] [Google Scholar]
- Cesur R, Sabia JJ, Tekin E. The psychological costs of war: military combat and mental health. Journal of Health Economics. 2013;32(1):51–65. doi: 10.1016/j.jhealeco.2012.09.001. [DOI] [PubMed] [Google Scholar]
- Devries K, Mak J, Bacchus LJ, Child JC, Falder G, Petzold M, Watts C. Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. Public Library of Science Medicine. 2013;10(5):e1001439. doi: 10.1371/journal.pmed.1001439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMaggio C, Galea S, Li G. Substance use and misuse in the aftermath of terrorism. A Bayesian meta-analysis. Addiction (Abingdon, England) 2009;104(6):894–904. doi: 10.1111/j.1360-0443.2009.02526.x. [DOI] [PubMed] [Google Scholar]
- Dobkin C, Shabani R. The health effects of military service: evidence from the Vietnam draft. Economic Inquiry. 2009;47(1):69–80. [Google Scholar]
- Figley CR. Catastrophes: an overview of family reactions. In: Figley CR, McCubbin HI, editors. Stress and the family, vol.2: coping with catastrophe. New York: Routledge; 1983. pp. 3–20. [Google Scholar]
- Ford CA, Udry JR, Gleiter K, Chantala K. Reactions of young adults to September 11, 2001. Archives of Pediatrics and Adolescent Medicine. 2003;157(6):572–578. doi: 10.1001/archpedi.157.6.572. [DOI] [PubMed] [Google Scholar]
- Froot KA. Consistent covariance matrix estimation with cross-sectional dependence and heteroskedasticity in financial data. Journal of Financial and Quantitative Analysis. 1989;24(3):333–355. [Google Scholar]
- Galea S, Ahern J, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, Vlahov D. Psychological sequelae of the September 11 terrorist attacks in New York City. New England Journal of Medicine. 2002;346(13):982–987. doi: 10.1056/NEJMsa013404. [DOI] [PubMed] [Google Scholar]
- Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiologic Reviews. 2005;27:78–91. doi: 10.1093/epirev/mxi003. [DOI] [PubMed] [Google Scholar]
- Galea S, Resnick H. Posttraumatic stress disorder in the general population after mass terrorist incidents: considerations about the nature of exposure. CNS Spectrums. 2005;10(2):107–115. doi: 10.1017/s1092852900019441. [DOI] [PubMed] [Google Scholar]
- Galea S, Tracy M. Participation rates in epidemiologic studies. Annals of Epidemiology. 2007;17(9):643–653. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Galea S, Vlahov D, Resnick H, Ahern J, Susser E, Gold J, Kilpatrick D. Trends of probable post-traumatic stress disorder in New York City after the September 11 terrorist attacks. American Journal of Epidemiology. 2003;158(6):514–524. doi: 10.1093/aje/kwg187. [DOI] [PubMed] [Google Scholar]
- Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, Corey-Lisle PK. The economic burden of depression in the United States: how did it change between 1990 and 2000? Journal of Clinical Psychiatry. 2003;64(12):1465–1475. doi: 10.4088/jcp.v64n1211. [DOI] [PubMed] [Google Scholar]
- Greenberg PE, Sisitsky T, Kessler RC, Finkelstein SN, Berndt ER, Davidson JR, Fyer AJ. The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatry. 1999;60(7):427–435. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- Hawdon J. Communal bereavement. In: Bryant CD, Peck DL, editors. Encyclopedia of death and the human experience. Vol. 1. Thousand Oaks: SAGE Publications, Inc; 2009. pp. 213–216. [Google Scholar]
- Hearst N, Newman TB, Hulley SB. Delayed effects of the military draft on mortality. A randomized natural experiment. New England Journal of Medicine. 1986;314(10):620–624. doi: 10.1056/NEJM198603063141005. [DOI] [PubMed] [Google Scholar]
- Helliwell JF, Wang S. Weekends and subjective well-being. Social Indicators Research. 2014;116(2):389–407. [Google Scholar]
- Hennessy CH, Moriarty DG, Zack MM, Scherr PA, Brackbill R. Measuring health-related quality of life for public health surveillance. Public Health Reports. 1994;109(5):665–672. [PMC free article] [PubMed] [Google Scholar]
- Holman EA, Garfin DR, Silver RC. Media’s role in broadcasting acute stress following the Boston Marathon bombings. Proceedings of the National Academy of Sciences of the United States of America. 2014;111(1):93–98. doi: 10.1073/pnas.1316265110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horner-Johnson W, Krahn G, Andresen E, Hall T. Developing summary scores of health-related quality of life for a population-based survey. Public Health Reports. 2009;124(1):103–110. doi: 10.1177/003335490912400113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz AV, Wakefield JC. The loss of sadness: how psychiatry transformed normal sorrow into depressive disorder. New York: Oxford University Press; 2007. [DOI] [PubMed] [Google Scholar]
- Jia H, Muennig P, Lubetkin EI, Gold MR. Predicting geographical variations in behavioural risk factors: an analysis of physical and mental healthy days. Journal of Epidemiology and Community Health. 2004;58(2):150–155. doi: 10.1136/jech.58.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judd LL, Paulus MP, Wells KB, Rapaport MH. Socioeconomic burden of subsyndromal depressive symptoms and major depression in a sample of the general population. American Journal of Psychiatry. 1996;153(11):1411–1417. doi: 10.1176/ajp.153.11.1411. [DOI] [PubMed] [Google Scholar]
- Judd LL, Schettler PJ, Akiskal HS. The prevalence, clinical relevance, and public health significance of subthreshold depressions. Psychiatric Clinics of North America. 2002;25(4):685–698. doi: 10.1016/s0193-953x(02)00026-6. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry. 1999;156(6):837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kessler RC, Walters EE, MacLean C, Neale MC, Heath AC, Eaves LJ. Stressful life events, genetic liability, and onset of an episode of major depression in women. American Journal of Psychiatry. 1995;152(6):833–842. doi: 10.1176/ajp.152.6.833. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, Prescott CA. Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. American Journal of Psychiatry. 2001;158(4):587–593. doi: 10.1176/appi.ajp.158.4.587. [DOI] [PubMed] [Google Scholar]
- Knudsen HK, Roman PM, Johnson JA, Ducharme LJ. A changed America? The effects of September 11th on depressive symptoms and alcohol consumption. Journal of Health and Social Behavior. 2005;46(3):260–273. doi: 10.1177/002214650504600304. [DOI] [PubMed] [Google Scholar]
- Larsen RJ, Kasimatis M. Individual differences in entrainment of mood to the weekly calendar. Journal of Personality and Social Psychology. 1990;58(1):164–171. doi: 10.1037//0022-3514.58.1.164. [DOI] [PubMed] [Google Scholar]
- Lauderdale DS. Birth outcomes for Arabic-named women in California before and after September 11. Demography. 2006;43(1):185–201. doi: 10.1353/dem.2006.0008. [DOI] [PubMed] [Google Scholar]
- Lin S, Reibman J, Bowers JA, Hwang SA, Hoerning A, Gomez MI, Fitzgerald EF. Upper respiratory symptoms and other health effects among residents living near the World Trade Center site after September 11, 2001. American Journal of Epidemiology. 2005;162(6):499–507. doi: 10.1093/aje/kwi233. [DOI] [PubMed] [Google Scholar]
- Logue JN, Hansen H, Struening E. Emotional and physical distress following Hurricane Agnes in Wyoming Valley of Pennsylvania. Public Health Reports. 1979;94(6):495–502. [PMC free article] [PubMed] [Google Scholar]
- McCann IL, Pearlman LA. Vicarious traumatization: a framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress. 1990;3(1):131–149. [Google Scholar]
- Metcalfe R, Powdthavee N, Dolan P. Destruction and distress: using a quasi-experiment to show the effects of the September 11 attacks on mental well-being in the United Kingdom. Economic Journal. 2011;121(550):F81–F103. [Google Scholar]
- Meyer BD. Natural and quasi-experiments in economics. Journal of Business & Economic Statistics. 1995;13(2):151–161. [Google Scholar]
- Mokdad AH. The Behavioral Risk Factors Surveillance System: past, present, and future. Annual Review of Public Health. 2009;30:43–54. doi: 10.1146/annurev.publhealth.031308.100226. [DOI] [PubMed] [Google Scholar]
- Moriarty DG, Kobau R, Zack MM, Zahran HS. Tracking Healthy Days – a window on the health of older adults. Preventing Chronic Disease. 2005;2(3):A16. [PMC free article] [PubMed] [Google Scholar]
- Moriarty DG, Zack MM, Kobau R. The Centers for Disease Control and Prevention’s Healthy Days Measures - population tracking of perceived physical and mental health over time. Health and Quality of Life Outcomes. 2003;1:37. doi: 10.1186/1477-7525-1-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Lopez AD. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- Neria Y, Sullivan GM. Understanding the mental health effects of indirect exposure to mass trauma through the media. Journal of the American Medical Association. 2011;306(12):1374–1375. doi: 10.1001/jama.2011.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- North CS, Nixon SJ, Shariat S, Mallonee S, McMillen JC, Spitznagel EL, Smith EM. Psychiatric disorders among survivors of the Oklahoma City bombing. Journal of the American Medical Association. 1999;282(8):755–762. doi: 10.1001/jama.282.8.755. [DOI] [PubMed] [Google Scholar]
- North CS, Pfefferbaum B. Research on the mental health effects of terrorism. Journal of the American Medical Association. 2002;288(5):633–636. doi: 10.1001/jama.288.5.633. [DOI] [PubMed] [Google Scholar]
- Padela AI, Heisler M. The association of perceived abuse and discrimination after September 11, 2001, with psychological distress, level of happiness, and health status among Arab Americans. American Journal of Public Health. 2010;100(2):284–291. doi: 10.2105/AJPH.2009.164954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paxson C, Fussell E, Rhodes J, Waters M. Five years later: recovery from post traumatic stress and psychological distress among low-income mothers affected by Hurricane Katrina. Social Science and Medicine. 2012;74(2):150–157. doi: 10.1016/j.socscimed.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad V, Jena AB. Prespecified falsification end points: can they validate true observational associations? Journal of the American Medical Association. 2013;309(3):241–242. doi: 10.1001/jama.2012.96867. [DOI] [PubMed] [Google Scholar]
- Rogers WH. Regression standard errors in clustered samples. Stata Tech Bull. 1993;13:19–23. [Google Scholar]
- Rosenthal NE, Sack DA, Gillin JC, Lewy AJ, Goodwin FK, Davenport Y, Wehr TA. Seasonal affective disorder. A description of the syndrome and preliminary findings with light therapy. Archives of General Psychiatry. 1984;41(1):72–80. doi: 10.1001/archpsyc.1984.01790120076010. [DOI] [PubMed] [Google Scholar]
- Schlenger WE, Caddell JM, Ebert L, Jordan BK, Rourke KM, Wilson D, Kulka RA. Psychological reactions to terrorist attacks: findings from the National Study of Americans’ Reactions to September 11. Journal of the American Medical Association. 2002;288(5):581–588. doi: 10.1001/jama.288.5.581. [DOI] [PubMed] [Google Scholar]
- Schuster MA, Stein BD, Jaycox L, Collins RL, Marshall GN, Elliott MN, Berry SH. A national survey of stress reactions after the September 11, 2001, terrorist attacks. New England Journal of Medicine. 2001;345(20):1507–1512. doi: 10.1056/NEJM200111153452024. [DOI] [PubMed] [Google Scholar]
- Schwarz N, Clore GL. Mood, misattribution, and judgments of well-being: Informative and directive functions of affective states. Journal of Personality and Social Psychology. 1983;45(3):513–523. [Google Scholar]
- Silver RC, Holman EA, Andersen JP, Poulin M, McIntosh DN, Gil-Rivas V. Mental- and physical-health effects of acute exposure to media images of the September 11, 2001, attacks and the Iraq War. Psychological Science. 2013;24(9):1623–1634. doi: 10.1177/0956797612460406. [DOI] [PubMed] [Google Scholar]
- Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11. Journal of the American Medical Association. 2002;288(10):1235–1244. doi: 10.1001/jama.288.10.1235. [DOI] [PubMed] [Google Scholar]
- Smith TW. Happiness: time trends, seasonal variations, intersurvey differences, and other mysteries. Social Psychology Quarterly. 1979;42(1):18–30. [Google Scholar]
- Stone AA, Schneider S, Harter JK. Day-of-week mood patterns in the United States: on the existence of ‘Blue Monday’, ‘Thank God it’s Friday’ and weekend effects. Journal of Positive Psychology. 2012;7(4):306–314. [Google Scholar]
- Stull DE, Leidy NK, Parasuraman B, Chassany O. Optimal recall periods for patient-reported outcomes: challenges and potential solutions. Current Medical Research and Opinion. 2009;25(4):929–942. doi: 10.1185/03007990902774765. [DOI] [PubMed] [Google Scholar]
- Taylor MP. Tell me why I don’t like Mondays: investigating day of the week effects on job satisfaction and psychological well-being. Journal of the Royal Statistical Society: Series A. 2006;169(1):127–142. [Google Scholar]
- Tsai AC, Weiser SD, Dilworth SE, Shumway M, Riley ED. Violent victimization, mental health, and service utilization outcomes in a cohort of homeless and unstably housed women living with or at risk of becoming infected with HIV. American Journal of Epidemiology. 2015;181(10):817–826. doi: 10.1093/aje/kwu350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumen S, Zeydanli T. Day-of-the-week effects in subjective well-being: does selectivity matter? Social Indicators Research. 2014;119(1):139–162. [Google Scholar]
- U.S. Centers for Disease Control and Prevention. Quality of life as a new public health measure–Behavioral Risk Factor Surveillance System, 1993. Morbidity and Mortality Weekly Report. 1994;43(20):375–380. [PubMed] [Google Scholar]
- U.S. Centers for Disease Control and Prevention. Health-related quality of life and activity limitation–eight states, 1995. Morbidity and Mortality Weekly Report. 1998;47(7):134–140. [PubMed] [Google Scholar]
- U.S. Centers for Disease Control and Prevention. Measuring healthy days: population assessment of health-related quality of life. Atlanta: U.S. Department of Health and Human Services; 2000. [Google Scholar]
- U.S. Centers for Disease Control and Prevention. Injuries and illnesses among New York City Fire Department rescue workers after responding to the World Trade Center attacks. Morbidity and Mortality Weekly Report. 2002;51:1–5. Spec No. [PubMed] [Google Scholar]
- Vlahov D, Galea S, Resnick H, Ahern J, Boscarino JA, Bucuvalas M, Kilpatrick D. Increased use of cigarettes, alcohol, and marijuana among Manhattan, New York, residents after the September 11th terrorist attacks. American Journal of Epidemiology. 2002;155(11):988–996. doi: 10.1093/aje/155.11.988. [DOI] [PubMed] [Google Scholar]
- Wakefield JC, Schmitz MF, First MB, Horwitz AV. Extending the bereavement exclusion for major depression to other losses: evidence from the National Comorbidity Survey. Archives of General Psychiatry. 2007;64(4):433–440. doi: 10.1001/archpsyc.64.4.433. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Vos T. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


