Abstract
Objective
The Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) is the most commonly used instrument to assess the clinical severity of obsessive-compulsive symptoms. Treatment determinations are often based on Y-BOCS score thresholds. However, these benchmarks are not empirically based, which may result in non-evidence based treatment decisions. Accordingly, the present study sought to derive empirically-based benchmarks for defining obsessive-compulsive symptom severity.
Method
Nine hundred and fifty-four adult patients with obsessive-compulsive disorder (OCD), recruited through the Brazilian Research Consortium on Obsessive-Compulsive Spectrum Disorders, were evaluated by experienced clinicians using a structured clinical interview, the Y-BOCS, and the Clinical Global Impressions–Severity scale (CGI-Severity).
Results
Similar to results in treatment-seeking children with OCD, our findings demonstrated convergence between the Y-BOCS and global OCD severity assessed by the CGI-Severity (Nagelkerke R2=.48). Y-BOCS scores of 0–13 corresponded with ‘mild symptoms’ (CGI-Severity = 0–2), 14–25 with ‘moderate symptoms’ (CGI-Severity = 3), 26–34 with ‘moderate-severe symptoms’ (CGI-Severity = 4) and 35–40 with ‘severe symptoms’ (CGI-Severity = 5–6). Neither age nor ethnicity was associated with Y-BOCS scores, but females demonstrated more severe obsessive-compulsive symptoms than males (d=.34). Time spent on obsessions/compulsions, interference, distress, resistance, and control were significantly related to global OCD severity although the symptom resistance item pairing demonstrated a less robust relationship relative to other components of the Y-BOCS.
Conclusions
These data provide empirically-based benchmarks on the Y-BOCS for defining the clinical severity of treatment seeking adults with OCD, which can be used for normative comparisons in the clinic and for future research.
Keywords: Obsessive-compulsive disorder, Yale-Brown Obsessive-Compulsive Scale, Treatment, Assessment, Validity
Introduction
Obsessive compulsive disorder (OCD) is an impairing psychiatric condition [1, 2] that runs a chronic course without intervention [3]. Both cognitive behavioral therapy (CBT) and pharmacotherapy with serotonin reuptake inhibitors have demonstrated efficacy [4, 5]. Treatment guidelines for application of each intervention alone or in combination are typically based on obsessive-compulsive symptom severity levels, which are most commonly defined by the Yale-Brown Obsessive Compulsive Scale (Y-BOCS;[6, 7]), a widely used clinician administered measure that assesses the severity of obsessive-compulsive symptoms over the past week. The ten items that comprise the Y-BOCS Severity Scale assess time occupied, associated distress, impairment, resistance, and control of obsessions and compulsions.
Despite its wide use and acceptance as the “gold standard” for OCD assessment [8], empirically established metrics for differentiating qualitative differences in symptom severity have been established among children [9], but not with adults. This has significant implications in terms of applied clinical practice and research. Clinically, lack of more reliable severity thresholds could result in non-evidence based treatment decisions being made in which first-line intervention approaches are not applied per practice guidelines or treatment augmentation decisions are based largely on subjective interpretations of testing. Without empirically informed benchmarks for defining this level of severity, treatment decisions may be made that lack empirical support, potentially attenuating the quality of clinical care and/or increasing the potential for adverse effects. Regarding research, inclusion criteria often set a benchmark for severity depending on the nature of the study (i.e., high thresholds may be used for more invasive procedures such as neurosurgery, somewhat lower thresholds for pharmacological and/or CBT intervention studies). Yet, in the absence of established guidelines, it is unclear what such scores are measuring in the context of overall illness severity, potentially resulting in inclusion of subjects that should not qualify or excluding those who may be eligible. These data may also have implications for defining those with sub-threshold OCD who experience significant disability [10] and require further study with regards to appropriate intervention strategies.
In the only published study examining guidelines for interpreting obsessive-compulsive symptom severity scores, Lewin et al. [9] studied a large sample of geographically diverse treatment seeking children and adolescents with OCD (N = 815). Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS; [11]) score ranges corresponded with clinician ratings of clinical severity (Nagelkerke pseudo-R2=.37). Scores above 30 corresponded with severe symptoms; scores between 25 and 30 corresponded with moderate-severe symptoms; scores between 14 and 24 corresponded with moderate symptoms; scores between five and 13 corresponded with mild symptoms; and scores below five were linked with slight or less illness.
Given the lack of corresponding data in adults, we sought to examine several understudied aspects of the Y-BOCS in a large cohort of well-characterized patients with OCD. There were three study aims. First, we evaluated how well obsessive-compulsive symptom severity on the Y-BOCS corresponds with global OCD syndrome severity via the Clinical Global Impression–Severity scale (CGI-Severity; [12]). Second, we examined the extent to which individual Y-BOCS symptom pairs (time spent on obsessions/compulsions, interference, distress, resistance, and control) are associated with global OCD syndrome severity (CGI-Severity). Third, we provide normative data through descriptive and inferential statistics as well as a cumulative distribution function, which enables clinicians and researchers to compare individual patients and patient samples to a larger OCD comparison group.
Method
Participants and Procedures
The sample consisted of 955 patients (555 females; mean age=35.82 years, SD=12.49 years, age range=18–82) recruited through the Brazilian Research Consortium on Obsessive-Compulsive Spectrum Disorders, which spanned seven universities across different regions of Brazil. With regard to self-reported ethnicity, participants were 82.9% Caucasian, 3.9% African, 1.4% Asian, 11.6% mixed race, and 0.2% reported as “other”. Participants were enrolled between August 2003 and August 2009, with all meeting DSM-IV criteria for OCD determined by the Structural Clinical Interview for DSM-IV Axis I disorders (SCID-I; [13]). Exclusion criteria included documented cognitive disability, schizophrenia, and OCD secondary to a general medical condition.
All Consortium sites obtained ethics approval from their respective Research Ethics Committee. Written informed consent was obtained prior to conducting study procedures (see [14]). Thereafter, a trained doctoral-level clinician administered the SCID-I, Y-BOCS, CGI-Severity, and other measures not reported in the present study. Ongoing training and supervision was used to assure quality assessments.
Measures
Y-BOCS
The Y-BOCS [6, 7] is a psychometrically-sound semi-structured clinician-administered interview that assesses the presence and severity of OCD symptoms over the prior week [15].a While the Y-BOCS contains both a detailed Symptom Checklist and Severity scale, we focused on the Severity scale only which consists of a total score and subscales assessing the severity of obsessions and compulsions, respectively. Ten questions, with scores ranging from 0 to 4 (most severe), address time, interference, distress, resistance and control over obsessions and compulsions (total score range from 0 to 40). A Portuguese translation of the Y-BOCS, developed using accepted methods of cross-language translation [16], was used in the present study. The Portuguese Y-BOCS demonstrates sound psychometric properties [17–19] comparable to those found in North American samples [20, 21].
CGI-Severity
The CGI-Severity is a single-item rating by the clinician pertaining to the global severity of the patient’s psychopathology [22]. Items are rated on a 0–6 scale (0 = “no illness,” 1 = “illness slight, doubtful, transient,” 2 = “mild symptoms, little functional impairment,” 3 = “moderate symptoms, functions with effort,” 4 = “moderate-severe symptoms, limited functioning,” 5 = “severe symptoms, functions with assistance,” 6 = “extremely severe symptoms, completely nonfunctional”). The CGI-Severity rating demonstrates convergence with clinician-rated OCD assays [23, 24], and has been extensively used in treatment studies [25–27].
Analytic Plan
Relationships between Y-BOCS total scores and demographic variables were evaluated by an independent t-test (for sex), a one-way ANOVA (for ethnicity), and a Pearson product-moment correlation (for age). To evaluate how different aspects of OCD are related to overall severity, corresponding Y-BOCS item pairs that have parallel content for obsessions and compulsions (i.e., time spent on obsessions/compulsions, interference, distress, resistance, and control) were summed and then correlated with CGI-Severity scores via bivariate correlations. Effect sizes were measured in the metric of Cohen’s d, Pearson’s r, and eta-squared. According to criteria provided by Cohen [28], small, medium, and large effect sizes are respectively associated with Cohen’s d values of .2, .5, and .8, Pearson’s r values of .1, .3, and .5, and eta-squared values of .01, .06, and .14. When an observed effect size was in between these anchors, we referred to both categories when evaluating effects (e.g., medium-large). To create predicted CGI-Severity levels based on Y-BOCS score ranges, ordinal logistic regression was employed through use of the PLUM function in SPSS 22.0, with Nagelkerke R2 reported as an estimate of the overall amount of variance explained by the predictive model. A cumulative distribution function was created based on study data to provide a basis for normative Y-BOCS comparisons.
Results
Small-medium group differences in Y-BOCS total scores were observed by sex (t(953)=5.21, p<.01, d=.34), but differences by ethnicity were not observed (F(4, 950)=1.62, p=.17, eta-squared=.01), and no significant relationship was observed between current age and Y-BOCS total scores (r(952)=−.02, p=.65). A similar pattern was observed for Y-BOCS subscales, where small-medium sex differences were observed for both the obsessions (t(953)=4.07, p<.01, d=.26) and compulsions (t(953)=5.58, p<.01, d=.36) subscales, but no differences in ethnicity were observed among Y-BOCS obsessions (F(4, 950)=1.38, p=.24, eta-squared=.01) or compulsions (F(4, 950)=1.49, p=.20, eta-squared=.01) scores, and no significant relationships were observed between current age and Y-BOCS obsessions (r(952)= −.03, p=.37) or compulsions (r(952) =.00, p=.98) scores. Given that significant group differences were only observed based on patient sex, means and standard deviations of Y-BOCS and CGI-Severity scores stratified by sex can be found in Table 1.
Table 1.
Means, Standard Deviations, and Difference Tests for Y-BOCS and CGI-Severity scores by Sex
| Males | Females | Total | Sex Differences t, p, d | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Mean | SD | Mean | SD | Mean | SD | ||
| Y-BOCS Total Score | 24.12 | 7.84 | 26.64 | 7.02 | 25.58 | 7.48 | t=5.21, p<.01, d=.34 |
| Y-BOCS Obsessions | 12.12 | 4.16 | 13.16 | 3.66 | 12.72 | 3.91 | t=4.07, p<.01, d=.26 |
| Y-BOCS Compulsions | 12.00 | 4.30 | 13.48 | 3.88 | 12.86 | 4.12 | t=5.58, p<.01, d=.36 |
| Y-BOCS Item Pairs | |||||||
| Time Spent | 5.06 | 1.85 | 5.56 | 1.82 | 5.35 | 1.85 | t=4.17, p<.01, d=.27 |
| Interference | 4.34 | 1.84 | 4.64 | 1.68 | 4.51 | 1.76 | t=2.62, p<.01, d=.17 |
| Distress | 5.23 | 1.76 | 5.74 | 1.52 | 5.53 | 1.64 | t=4.81, p<.01, d=.31 |
| Resistance | 4.12 | 2.27 | 4.74 | 2.10 | 4.48 | 2.20 | t=4.38, p<.01, d=.28 |
| Control | 5.38 | 2.04 | 5.96 | 1.68 | 5.71 | 1.86 | t=4.81, p<.01, d=.31 |
| CGI-S | 3.45 | 1.08 | 3.64 | 1.02 | 3.56 | 1.05 | t=2.75, p<.01, d=.18 |
Note. Y-BOCS = Yale Brown Obsessive Compulsive Scale; CGI-Severity = Clinical Global Impression-Severity
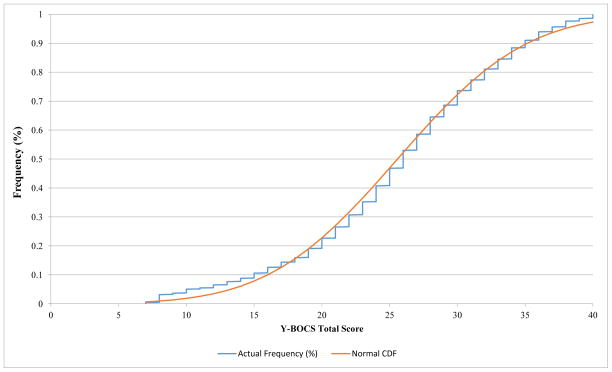
Predicted CGI-Severity ratings based on Y-BOCS score ranges can be found in Table 2; the ordinal logistic model used to create the predictions accounted for a substantial amount of variance in CGI-Severity scores (Nagelkerke R2=.48). Y-BOCS scores of 0–13 corresponded with ‘mild symptoms’ or lower (CGI-Severity = 0–2), 14–25 with ‘moderate symptoms’ (CGI-Severity = 3), 26–34 with ‘moderate-severe symptoms’ (CGI-Severity = 4) and 35–40 with ‘severe symptoms’ (CGI-Severity = 5–6). To provide a basis for normative Y-BOCS comparisons, a cumulative distribution function based on study data can be found in Figure 1.
Table 2.
Y-BOCS Classification of CGI-Severity Ratings Based on Ordinal Logistic Regression
| Y-BOCS Range | CGI-Severity Rating |
|---|---|
| 0–13a,b | Mild symptoms or less (Little to no functional impairment); CGI-Severity = 0 to 2 |
| 14–25 | Moderate symptoms (Functions with effort); CGI-Severity = 3 |
| 26–34 | Moderate-severe symptom (Limited functioning); CGI-Severity = 4 |
| 35–40b | Severe or greater symptoms (Functions with assistance or completely non- functional); CGI-Severity = 5 to 6 |
Note. Y-BOCS = Yale Brown Obsessive Compulsive Scale; CGI-Severity = Clinical Global Impressions-Severity
Because a clinical sample was employed, no Y-BOCS scores below 7 were available for use. It was assumed that scores below 7 would follow the predictions made by the ordinal logistic model for patients with very mild symptoms, and thus we included scores below 7 in the Y-BOCS range, resulting in a range of 0–13.
The ordinal logistic model employed only predicted CGI-Severity scores in the range of 2 to 5. This is due to the nature of an outpatient clinical sample, which has relatively few participants in these extreme CGI-Severity ranges, as well the CGI-Severity possibly not discriminating as well at very high and very low extremes of its measurement range. It was assumed that a predicted score of 5 would mean that CGI-Severity scores of greater severity would also be incorporated in this range, and similarly a predicted score of 2 would also incorporate CGI-Severity scores of lesser severity.
Figure 1.
Cumulative distribution function of the Y-BOCS Total Severity Score. This figure illustrates the frequency of Y-BOCS Total Severity score compared to the normal curve; Y-BOCS = Yale Brown Obsessive Compulsive Scale
Large and medium-large correlations were observed between CGI-Severity scores and all Y-BOCS item pairs evaluated, including those corresponding to time spent on obsessions/compulsions (r(952)=.55, p<.01), interference (r(952)=.59, p<.01), distress (r(952)=.58, p<.01), resistance (r(952)=.43, p<.01), and control (r(952)=.54, p<.01).
Discussion
These data build on Lewin et al.’s [9] report in children and adolescents (age range: 4–18 years) in the USA provide the first empirically based guidelines for interpreting obsessive-compulsive symptom severity among treatment seeking adults with OCD. Our findings were similar relative to Lewin et al. [9] with modest differences. Ratings of ‘severe’ to ‘extremely severe’ on the CGI-Severity corresponded to Y-BOCS scores of 35–40 versus scores of 31–40 on the CY-BOCS in Lewin et al.’s study [9]. Scores of 26–34 corresponded with ‘moderate-severe symptoms, limited functioning’ in our sample versus scores of 25–30 in youth. ‘Moderate symptoms, function with effort’ corresponded with ratings of 14–25 in this sample which was nearly identical to the 14–24 range found by Lewin et al. [9]. The more truncated range of Y-BOCS scores for those adult patients considered to be severely or extremely severely affected may reflect how OCD manifests in adults versus children. Children are enmeshed in families and school systems; more modest but still elevated OCD symptom severity scores on the CY-BOCS may correspond with greater global illness severity compared to adults by virtue of its impact on multiple life domains and family members.
Significant correlations of large and medium-large effect size were observed between Y-BOCS domains of severity and global illness severity, suggesting that global OCD severity may be best conceptualized as being comprised of time spent engaging in obsessions/compulsions, interference due to obsessions/compulsions, distress related to obsessions/compulsions, resistance against obsessions/compulsions, and control of obsessions/compulsions. Resistance against obsessions/compulsions exhibited a modestly weaker association with global severity (r=.43) relative to other item pairs, which is consistent with findings that this construct is not a reliable manifestation of psychological health [29]. The resistance against obsessions/compulsions items have demonstrated the lowest correlations with the Y-BOCS Severity Scale [30], are inconsistent with the CBT treatment model [31], and the resistance against obsessions item loads weakly on the Obsession Severity subscale in factor analytic studies (e.g., [32–34]).
There are several study limitations. First, while we had a large, well-characterized clinical sample, there were fewer patients at the extremes of clinical severity. This led to the need to use inference when associating CGI-Severity and Y-BOCS responses across the entire range of scores. However, the use of model-based inference permits the extrapolation of findings to other clinical samples beyond the literal data points employed, provided that the other samples come from the same population (i.e., outpatients with OCD). While the lowest score range of the CGI-Severity addresses the possibility of no functional impairment, we relied on modeling to infer the relationship between the CGI-Severity and Y-BOCS for very low scores (e.g., Y-BOCS scores below 8); in this instance additional sources of clinical information should be incorporated to determine if symptoms have clinical significance (i.e., are impairing). Second, although the sample was comprised of participants from throughout Brazil, findings may not generalize to other geographic regions and to community-based (or non-treatment seeking) samples. Third, the same clinician rated both the Y-BOCS and CGI-Severity; scores on one may have influenced the other. On balance, this method allowed clinicians to have a structured method of ascertaining clinical information, and using two different raters would introduce potential challenges in terms of understanding clinical severity. Finally, no inter-rater reliability checks were employed although raters were experienced clinicians under the supervision of experts in OCD care and research.
Within these limitations, this study has significant implications. First, this report objectively defines symptom severity levels that can inform treatment decisions. For example, a patient who presents with a Y-BOCS score of 20 would be classified as having moderate symptoms, indicating that s/he should initiate CBT as the initial intervention. Conversely, a patient with a Y-BOCS score of 35 would be classified as having symptoms in the severe range, indicating the role of multimodal treatment and/or more intensive CBT. Prior to this study, these evaluations would be subject to clinical judgment without empirical support. Second, these data provide researchers with empirically defined benchmarks to inform inclusion or exclusion criteria that can be individualized for the nature of the study. For example, a study of deep brain stimulation may require that participants have at least moderately-severe symptoms for inclusion so as not to expose participants unnecessarily to risk and more costly treatments. Likewise, in clinical trials, response to treatment or resistance/refractoriness can also be more clearly defined in terms of categorical levels of clinical severity. With this in mind, the current study provides guidance as to how this severity threshold would be defined using the Y-BOCS. Finally, these data provide information supporting that those with subthreshold symptoms may experience significant impairment. That Y-BOCS scores in the 14–18 range were best characterized by “Moderate symptoms, functions with effort” underscores the need for further study of this cohort, usually excluded from treatment trials.
Highligths.
Y-BOCS score thresholds used in applied practice are not empirically-based.
Y-BOCS scores were logically associated with ratings of global illness severity.
We provide benchmarks on the Y-BOCS for defining the clinical severity.
Acknowledgments
The authors would like to acknowledge the contributions of all of the people involved in the Brazilian Research Consortium on Obsessive-Compulsive Spectrum Disorders (CTOC) for making this study possible. This research was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico Grant (CNPq 420.122/2005-2). Mr. De Nadai is supported by the National Institutes of Health under Ruth L. Kirschstein National Research Service Award F31 MH094095 from the National Institute of Mental Health.
Footnotes
Although the Y-BOCS-II has been developed, the Y-BOCS remains the standard in the field.
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kugler BB, et al. Quality of life in obsessive-compulsive disorder: the role of mediating variables. Psychiatry Res. 2013;206(1):43–9. doi: 10.1016/j.psychres.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 2.Koran LM. Quality of life in obsessive-compulsive disorder. Psychiatr Clin North Am. 2000;23(3):509–17. doi: 10.1016/s0193-953x(05)70177-5. [DOI] [PubMed] [Google Scholar]
- 3.Rasmussen SA, Eisen JL. The epidemiology and clinical features of obsessive compulsive disorder. Psychiatr Clin North Am. 1992;15:743–758. [PubMed] [Google Scholar]
- 4.McKay D, et al. Efficacy of cognitive-behavioral therapy for obsessive-compulsive disorder. Psychiatry Res. 2015;225(3):236–46. doi: 10.1016/j.psychres.2014.11.058. [DOI] [PubMed] [Google Scholar]
- 5.Fineberg NA, et al. Obsessive-compulsive disorder (OCD): Practical strategies for pharmacological and somatic treatment in adults. Psychiatry Res. 2015 doi: 10.1016/j.psychres.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Goodman WK, et al. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch Gen Psychiatry. 1989;46(11):1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- 7.Goodman WK, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46(11):1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 8.Lewin AB, et al. Refining clinical judgment of treatment outcome in obsessive-compulsive disorder. Psychiatry Res. 2011;185:394–401. doi: 10.1016/j.psychres.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 9.Lewin AB, et al. Defining clinical severity in pediatric obsessive-compulsive disorder. Psychol Assess. 2014;26(2):679–84. doi: 10.1037/a0035174. [DOI] [PubMed] [Google Scholar]
- 10.de Bruijn C, et al. Subthreshold symptoms and obsessive-compulsive disorder: evaluating the diagnostic threshold. Psychol Med. 2010;40(6):989–97. doi: 10.1017/S0033291709991012. [DOI] [PubMed] [Google Scholar]
- 11.Scahill L, et al. Children’s Yale-Brown Obsessive Compulsive Scale: reliability and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(6):844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- 12.Guy W. ECDEU Assessment Manual for Psychopharmacology. National Institute for Mental Health; Rockville, MD: 1976. Clinical Global Impressions; pp. 218–222. [Google Scholar]
- 13.First MB, et al. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version-(SCID-CV) Washington, DC: American Psychiatric Press, Inc; 1996. [Google Scholar]
- 14.Miguel EC, et al. The Brazilian Research Consortium on Obsessive-Compulsive Spectrum Disorders: recruitment, assessment instruments, methods for the development of multicenter collaborative studies and preliminary results. Rev Bras Psiquiatr. 2008;30(3):185–96. doi: 10.1590/s1516-44462008000300003. [DOI] [PubMed] [Google Scholar]
- 15.Benito K, Storch EA. Assessment of obsessive-compulsive disorder: review and future directions. Expert Rev Neurother. 2011;11(2):287–98. doi: 10.1586/ern.10.195. [DOI] [PubMed] [Google Scholar]
- 16.Harkness J, Pennell B-E, Schoua-Glusberg A. Survey questionnaire translation and assessment. Methods for testing and evaluating survey questionnaires. 2004;546:453–473. [Google Scholar]
- 17.Asbahr FR, et al. Escala Yale-Brown de Sintomas Obsessivo-Compulsivos. Sao Paulo, Brazil: 1992. [Google Scholar]
- 18.Souza FP, et al. Psychometric properties of the Brazilian Portuguese version of the Obsessive-Compulsive Inventory: Revised (OCI-R) Revista Brasileira de Psiquiatria. 2011;33(2):137–142. doi: 10.1590/s1516-44462011000200008. [DOI] [PubMed] [Google Scholar]
- 19.Bortoncello CF, et al. Psychometric properties of the Brazilian version of the Obsessive Beliefs Questionnaire (OBQ-44) Journal of anxiety disorders. 2012;26(3):430–434. doi: 10.1016/j.janxdis.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 20.Storch EA, et al. Yale-Brown Obsessive Compulsive Scale: the dimensional structure revisited. Depression and Anxiety. 2005;22(1):28–35. doi: 10.1002/da.20088. [DOI] [PubMed] [Google Scholar]
- 21.Deacon BJ, Abramowitz JS. The Yale-Brown Obsessive Compulsive Scale: factor analysis, construct validity, and suggestions for refinement. Journal of anxiety disorders. 2005;19(5):573–585. doi: 10.1016/j.janxdis.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 22.National Institute of Mental Health. Clinical global impressions. In: Guy W, editor. ECDEU assessment manual of psychopharmacology. United States Department of Health, Education, and Welfare; Rockville, MD: 1976. pp. 218–222. [Google Scholar]
- 23.Storch EA, et al. Defining treatment response and remission in obsessive-compulsive disorder: a signal detection analysis of the children’s yale-brown obsessive compulsive scale. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(7):708–717. doi: 10.1016/j.jaac.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 24.Tolin DF, Abramowitz JS, Diefenbach GJ. Defining response in clinical trials for obsessive-compulsive disorder: a signal detection analysis of the Yale-Brown obsessive compulsive scale. The Journal of clinical psychiatry. 2005;66(12):1549–1557. doi: 10.4088/jcp.v66n1209. [DOI] [PubMed] [Google Scholar]
- 25.Storch EA, et al. D-cycloserine does not enhance exposure–response prevention therapy in obsessive–compulsive disorder. International clinical psychopharmacology. 2007;22(4):230–237. doi: 10.1097/YIC.0b013e32819f8480. [DOI] [PubMed] [Google Scholar]
- 26.Foa EB, et al. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. 2007. [DOI] [PubMed] [Google Scholar]
- 27.Tolin DF, et al. Cognitive-behavioral therapy for medication nonresponders with obsessive-compulsive disorder: a wait-list-controlled open trial. Journal of Clinical Psychiatry. 2004;65(7):922–931. doi: 10.4088/jcp.v65n0708. [DOI] [PubMed] [Google Scholar]
- 28.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 29.Storch EA, et al. Development and psychometric evaluation of the Yale-Brown Obsessive-Compulsive Scale--Second Edition. Psychol Assess. 2010;22(2):223–32. doi: 10.1037/a0018492. [DOI] [PubMed] [Google Scholar]
- 30.Woody SR, Steketee G, Chambless DL. The usefulness of the Obsessive Compulsive Scale of the Symptom Checklist-90-Revised. Behaviour Research and Therapy. 1995;33(5):607–611. doi: 10.1016/0005-7967(94)00090-7. [DOI] [PubMed] [Google Scholar]
- 31.Lewin AB, et al. Cognitive behavior therapy for obsessive-compulsive and related disorders. Psychiatr Clin North Am. 2014;37(3):415–45. doi: 10.1016/j.psc.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 32.McKay D, et al. Factor structure of the Yale-Brown Obsessive-Compulsive Scale: a two dimensional measure. Behav Res Ther. 1995;33(7):865–9. doi: 10.1016/0005-7967(95)00014-o. [DOI] [PubMed] [Google Scholar]
- 33.McKay D, et al. The Yale-Brown obsessive-compulsive scale: confirmatory factor analytic findings. Journal of Psychopathology and Behavioral Assessment. 1998;20(3):265–274. [Google Scholar]
- 34.Amir N, Foa EB, Coles ME. Factor structure of the Yale–Brown Obsessive Compulsive Scale. Psychological Assessment. 1997;9(3):312. [Google Scholar]