Highlights
-
•
Epidermoid cysts are benign tumors -IEIC-that originate in the spine or intracraneally.
-
•
Intradural compose 75% of epidermoid cysts and 25% are extradural in the diploic space—IEIC.
-
•
These benign lesions although they are of low incidence, are seen very rarely in intradiploic locations and above all, of significant size, may produce significant mass effect in patients, which was initially tolerated because of its slow growth, however, they may become decompensate and cause intracranial hypertension syndrome.
Keywords: Squamous, Intradiploic, Extradural cyst, Intradiploic epidermoid cyst, Hypertension syndrome
Abstract
Introduction
Intradiploic epidermoid intracranial cysts (IEIC) derive from ectodermal cells and are covered with stratified squamous epithelium. They are extremely rare, and most common locations are in the occipital, frontal and parietal bones. They have a very slow growth and can be asymptomatic until becoming evident by the deformation produced. The treatment is based on the removal of the lesion, and subsequent histopathological confirmation.
Presentation of case
Two cases are reported, with intracranial hypertension syndrome, which is very uncommon because of the slow growth of this type of pathology; however, decompensations occurring in the space-occupying lesions at intracranial level explain this type of clinical presentation.
Discussion
The most common presentation of intracranial intradiploic epidermoid cysts (IEIC) is asymptomatically, which is made evident by the prominence at the level of the soft tissues and then presenting less frequently local pain and cephalea; rarely the size of the lesion can cause focal neurological signs.
Conclusion
These benign lesions, although they are of low incidence, are seen very rarely in intradiploic locations and above all, of significant size, may produce significant mass effect in patients, which was initially tolerated because of its slow growth, however, they may become decompensate and cause intracranial hypertension syndrome.
1. Introduction
Epidermoid cysts are benign tumors that originate in the spine or intracraneally [1]. Love and Kernohan in 1936, referred to epidermoid cysts as congenital epithelial tumors [2]. They originate from granulation alterations producing a defect in the closure of the neural tube during the third to sixth week of gestation, at level surface of the ectoderm [3].
At intracranial level represents 0.2–1.8% of all tumor lesions; they can be located intra- or extradurally [4], [5]. Intradural compose 75% of epidermoid cysts and -IEIC-25% are extradural in the diploic space—IEIC [6], [7].
IEICs are very rare; as the name indicates are found among the two tables of the skull bones, having a slow growth [8], [9]. The first IEIC was reported by Müller in 1838, Cushing in 1922, also performed a description of an IEIC [12], [10] and the first case of giant IEIC in the posterior cranial fossa was reported by Rengachary [11].
Two cases are reported, that in a particular way, go to the emergency room because they display intracranial hypertension syndrome, which is very intriguing because of the slow growth of this type of pathology; however, decompensation occurring in the pathophysiology of space-occupying lesions at intracranial level explain this type of clinical presentation.
2. Presentation of cases
2.1. Case 1
Male, 42, with a history of smoking and drug use—methamphetamines. Presents occipital headache with 3 months evolution that radiates to the frontal region, pulsatile, which increases with Valsalva maneuvers with a frequency initially described as sporadic until evolving to daily, in the week prior to admission; accompanied by vomiting, on the day of admission, with intensified headache intensity. On physical examination, the patient exhibits intracranial hypertension symptoms (papilledema) without rostrocaudal deterioration, which is accompanied by indifferent lateropulsion; in imaging studies, extra-axial (Fig. 1) lesion is observed. Study protocol is completed, and resection of the lesion is performed by means of a right lateral suboccipital approach. Among the findings an important erosion of the occipital squama was observed due to extra-axial injury, eroding the bone, avascular, not infiltrating with surrounding tissues, of pearly aspect with fatty content inside (Fig. 2). Histopathological studies, reports us soft lesion with granular areas and firm membranous areas with calcifications, reporting an epidermal cyst. The patient progressed favorably, without neurological deficits with one-year follow-up (Fig. 3).
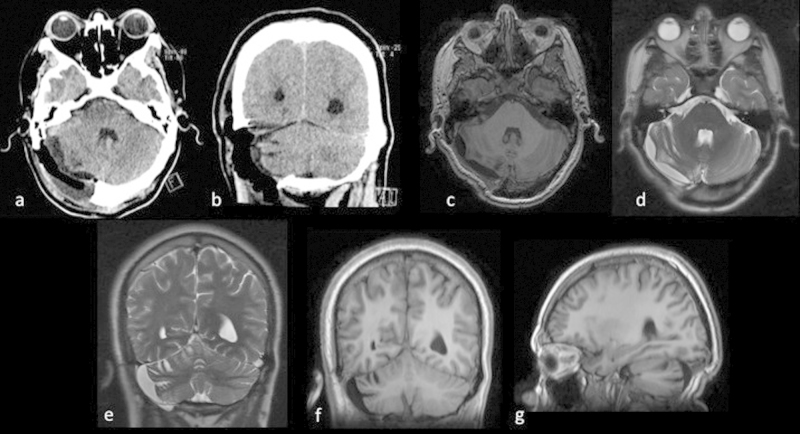
Fig. 1.
Tomography images (a–d) and MRI (e and f): where space occupying lesion is observed, extra-axial, right suboccipital, with significant erosion of the occipital squama (c, d), heterogeneous, predominantly hypo dense in tomography (a, b) and in the T1 weighted MRI sequence (e), hyper intense on T2-weighted sequence (h), which does not enhance with gadolinium administration (e, g) and restricts the diffusion sequence (f). Significant mass effect upon the cerebellar hemisphere and the right middle cerebellar peduncle is observed, in addition to compression of the fourth ventricle, without causing acute hydrocephaly.
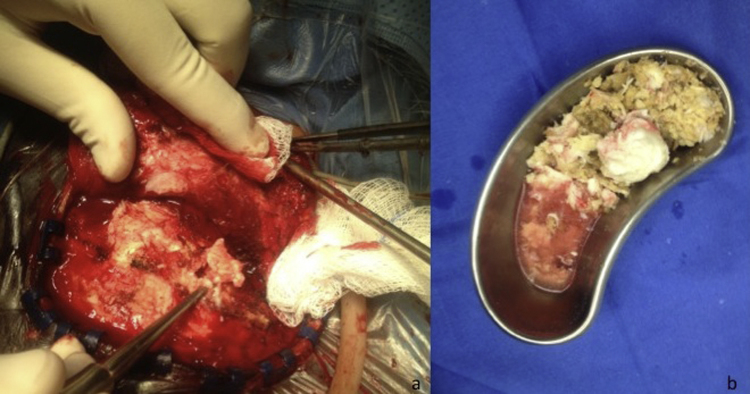
Fig. 2.
Intraoperative photos, where it is observed how the injury causes significant injury to the occipital squama (a); at the end of resection the greasy appearance of the lesion content (b) is observed.
Fig. 3.
Images of post-surgery studies tomography (a and b) and MRI (c–g), where we can observe the absence of lesion and how the structures compressed by it, return to their place.
2.2. Case 2
Male 46 years old, without major importance history. Sine 6 months ago presents painless right frontal region deformation; since 2 months ago with palpebral edema, which lasted four days, and was treated at another health facility as cellulitis, with antibiotics and anti-inflammatory therapy, resolving favorably; due to increasing deformity of the right frontal region, consults with private doctor who diagnosed intracranial lesion with respective imaging studies and subsequently refers to our hospital, by the mass effect is admitted (Fig. 4); at the time of admission the patient develops severe holocraneal cephalea, accompanied by vomiting, papilledema and stupor, therefore is decided to take to the OR suite for resection of the lesion, through a centered approach; during surgery important right frontal bone erosion was observed due to extra-axial injury, not vascularized, not infiltrating with neighboring tissues, with fatty content inside (Fig. 5); histopathological result is epidermoid cyst; during the immediate post-surgery period, the patient develops mixed delirium, which is solved in three days; is discharged without any complications; craneoplasty is later performed at 3 months after resection surgery of intradiploic epidermoid cyst (Fig. 6).
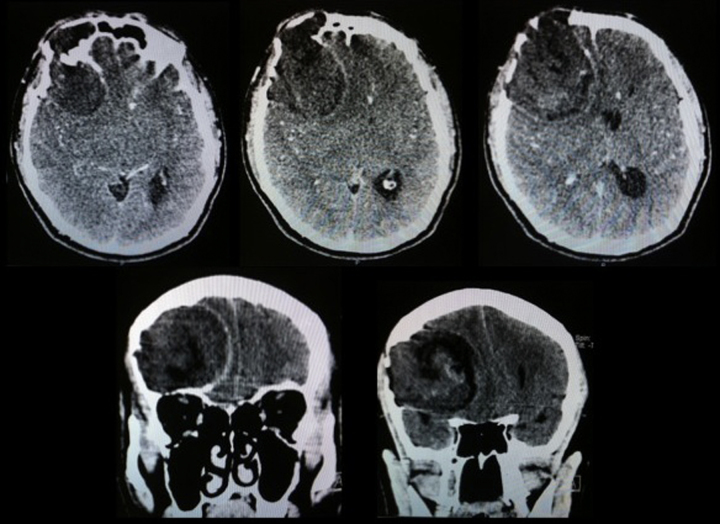
Fig. 4.
Simple skull tomography images, where lesion with important extra-axial intracranial mass effect is observed, with significant bone erosion with heterogeneous content.
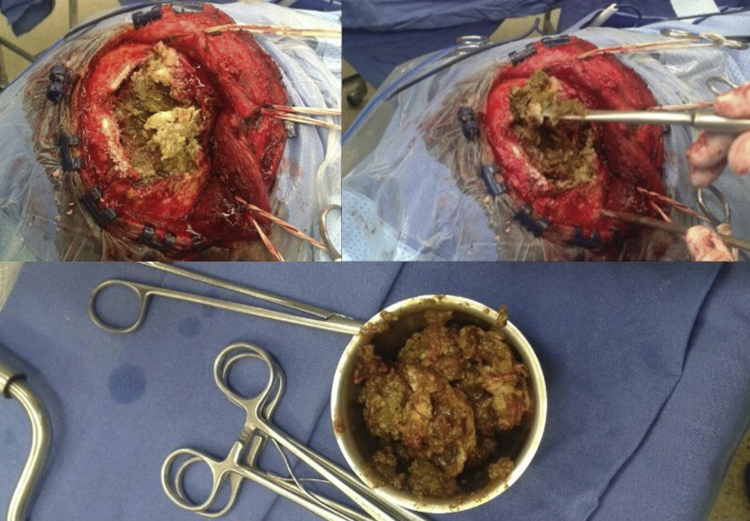
Fig. 5.
Intraoperative photos, where the lesion characteristic and the significant erosion of the right frontal bone is observed.
Fig. 6.
Postoperative tomography images where the resolution of the mass effect that produced the lesion (a, b) is observed; also the bone defect that was observed (c) and subsequent cranioplasty images with methyl methacrylate (d, e) are observed.
3. Discussion
Intracranial epidermoid cysts are generally located in the cerebellopontine angle or paraselar region [13]. Extradural lesions manifest with local mass effect, with or without cephalea [14]. The incidence of intracranial epidermoid cysts is higher in the intradural location, as reported in their work Love and Kernohan—70% and Gormley et al.—72.7% [2], [14].
Akar et al. reported 28 cases of intradural epidermoid cysts, of which the majority are found in the cerebellopontine angle—17; other locations were in the fourth ventricle, into the cisterna magna, in the fissure of Silvio, in the occipital lobe, in the lateral ventricles and diploic space [4]. The intradiploic extradural epidermoid cysts are located in the cranial vault, destroy the internal table and thin the external table [15]. The most common presentation of IEIC is the prominence at the level of the soft tissues and then presenting less frequently local pain and cephalea; rarely the size of the lesion can cause focal neurological signs [16], [17].
They can be located in the paranasal sinus, in the temporal and sphenoid bone, however it occurs most frequently at the level of the occipital, frontal and parietal bones [18].
The differential diagnosis of an intradiploic cranial lesion includes the aneurysmal bone cyst, dermoid cyst, cavernous hemangioma, Langerhans cells histiocytosis, fibrous dysplasia and eosinophilic granuloma [16], [19]. Atypical lesions may be larger than 5 cm and irregular [1].
Histologically, it is covered by fibrous tissue capsule, in which are included keratin, cholesterol, proteins and detritus crystals [20]. Malignant transformation of epidermoid cysts is very rare; the possibility of squamous cell carcinoma originated from a IEIC is described with poor prognosis even after radio or chemotherapy [21], [22].
Resection of these lesions are done to protect the patient from mass effect on intracranial mass, abscess formation and to avoid potential complications such as bleeding and malignant transformation of IEIC [1], [23], [24].
4. Conclusion
These benign lesions although they are of low incidence, are seen very rarely in intradiploic locations and above all, of significant size, may produce significant mass effect in patients, which was initially tolerated because of its slow growth, however, they may become decompensate and cause intracranial hypertension syndrome.
Dates of congress
This paper has not been presented in any congress.
Conflict of interest
None.
Funding
None funding.
Ethical approval
The name of the ethics committee is “collegial session neurosurgery”, with number 213892 for case 1 and214450 for case 2, of the Neurology and Neurosurgery National Institute.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Moreira-Holguín Juan Carlos: writing the paper.
Medélez-Borbonio Rafael:data collection.
Quintero-López Eduardo: traducing.
García-González Ulises: data collection.
Gómez-Amador Juan Luís: concept of paper and interpretation.
Guarantor
Moreira-Holguín Juan Carlos.
Acknowledgements
None.
References
- 1.Hassaneen W., Sawaya R. Epidermoid, dermoid, and neuroenteric cysts. In: Winn H.R., editor. Youmans Neurological Surgery. 6th ed. Elsevier Saunders; 2011. pp. 1523–1528. [Google Scholar]
- 2.Love J., Kernohan J. Dermoid and epidermoid tumors (cholesteatomas) of central nervous system. JAMA. 1936;107:1876–1883. [Google Scholar]
- 3.Iaconetta G., Carvalho G.A., Vorkapic P. Intracerebral epidermoid tumor: a case report and review of the literature. Surg. Neurol. 2001;55:218–222. doi: 10.1016/s0090-3019(01)00346-9. [DOI] [PubMed] [Google Scholar]
- 4.Akar Z., Tanriover N., Tuzgen S. Surgical treatment of intracranial epidermoid tumors. Neurol. Med. Chir. (Tokyo) 2003;43:275–281. doi: 10.2176/nmc.43.275. [DOI] [PubMed] [Google Scholar]
- 5.Kalgutkar A., Kini S., Jambhekar N. Intradiploic primary epitelial inclusion cyst of the skull. Ann. Diagn. Pathol. 2006;10:20–23. doi: 10.1016/j.anndiagpath.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Narlawar R.S., Nagar A., Hira P. Intradiploic epidermoid cyst. J. Postgrad. Med. 2002;48:213–214. [PubMed] [Google Scholar]
- 7.Khan A.N., Khalid S., Enam S.A. Intradiploic epidermoid cyst overlying the torcula: a surgical challenge. BMJ Case Rep. 2011 doi: 10.1136/bcr.08.2010.3245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hasturk A.E., Basmaci M., Yilmaz E.R. Giant intradiploic epidermoid cyst presenting as solitary skull mass with intracranial extensión. J. Craniofac. Surg. 2013;24(6):2169–2171. doi: 10.1097/SCS.0b013e3182a2d820. [DOI] [PubMed] [Google Scholar]
- 9.Demir M.K., Yapocier Ö., Onat E. Rare and challeging extra-axial brain lesions: CT and MRI findings with clínico-radiological differential diagnosis and pathological correlation. Diagn. Interv. Radiol. 2014;20:448–452. doi: 10.5152/dir.2014.14031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Müller J. ed. 1. G. Reimer; Berlin: 1838. Über den feineren Bau und die Formen der krankhaften Geschwfilste; pp. 73–81. [Google Scholar]
- 11.Rengachary S., Kishore P.R., Watanabe I. Intradiploic epidermoid cyst of the occipital bone with torcular obstruction: case report. J. Neurosurg. 1978;48:475–478. doi: 10.3171/jns.1978.48.3.0475. [DOI] [PubMed] [Google Scholar]
- 12.Cushing H. A large epidermal cholesteatoma of the parietotemporal región deforming the left hemipshere without cerebral symptoms. Surg. Gynecol. Obstet. 1922;34:557–566. [Google Scholar]
- 13.Darrouzet V., Franco-Vidal V., Hilton M. Surgery of cerebellopontine angle epidermoid cysts: role of the widened retrolabyrinthine approach combined with endoscopy. Otolaryngol. Head Neck Surg. 2004;131:120–125. doi: 10.1016/j.otohns.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 14.Gormley W.B., Tomecek F.J., Qureshi N. Craniocerebral epidermoid and dermoid tumours: a review of 32 cases. Acta Neurochir. (Wien) 1994;128:115–121. doi: 10.1007/BF01400660. [DOI] [PubMed] [Google Scholar]
- 15.Osborn A.G., Preece M.T. Intracranial cysts: radiologic–pathologic correlation and imaging approach. Radiology. 2006;239:650–664. doi: 10.1148/radiol.2393050823. [DOI] [PubMed] [Google Scholar]
- 16.Narlawar R.S., Nagar A., Hira P., Raut A.A. Intradiploic epidermoid cyst. J. Postgrad. Med. 2002;48:213–214. [PubMed] [Google Scholar]
- 17.Enchev Y., Kamenov B., William A. Posttraumatic giant extradural intradiploic epidermoid cysts of posterior cranial fossa: case report and review of the literatura. J. Korean Neurosurg. 2011;49:53–57. doi: 10.3340/jkns.2011.49.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cho J.H., Jung T.Y., Kim I.Y. A giant intradiploic epidermoid cyst with perforation of the dura and brain parenchymal involvement. Clin. Neurol. Neurosurg. 2007;109:368–373. doi: 10.1016/j.clineuro.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 19.Krupp W., Heckert A., Holland H. Giant intradiploic epidermoid cyst with large osteolytic lesions of the skull: a case report. J. Med. Case Rep. 2012;85(6):1–5. doi: 10.1186/1752-1947-6-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jaiswal A.K., Mahapatra A.K. Giant intradiploic epidermoid cysts of the skull. A report of eight cases. Br. J. Neurosurg. 2000;14:225–228. doi: 10.1080/026886900408405. [DOI] [PubMed] [Google Scholar]
- 21.Bretschneider T., Dorenbeck U., Strotzer M. Squamous cell carcinoma arising in an intradiploic epidermoid cyst. Neuroradiology. 1999;41:570–572. doi: 10.1007/s002340050807. [DOI] [PubMed] [Google Scholar]
- 22.Hoeffel C., Heldt N., Chelle C. Malignant change in an intradiploic epidermoid cyst. Acta Neurol. Belg. 1997;97:45–49. [PubMed] [Google Scholar]
- 23.Fox B.D., Smitherman S.M., Amhaz H., Ruiz M.I., Rouah E., Radaideh M. A supratentorial, hemorrhagic, intraparenchymal epidermoid cyst. J. Clin. Neurosci. 2009;16:1101–1105. doi: 10.1016/j.jocn.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 24.Chen C.Y., Wong J.S., Hsieh S.C. Intracranial epidermoid cyst with hemorrhage: MR imaging findings. Am. J. Neuroradiol. 2006;27:427–429. [PMC free article] [PubMed] [Google Scholar]