Highlights
-
•
A case of acute bowel obstruction caused by the use of barbed suture in laparoscopic myomectomy.
-
•
Bowel complications associated with barbed suture were seldom reported despite it is increasingly used in surgery today.
-
•
Some recommendations arising from this case may help to avoid or reduce this complication.
-
•
A high index of suspicion is necessary in making an early diagnosis and prompt action should be taken to alleviate major bowel complications due to barbed suture.
Keywords: Laparoscopy, Myomectomy, Small bowel, Obstruction, Barbed suture
Abstract
Myomectomy is commonly performed for symptomatic fibroids in women who wish to conserve fertility. Laparoscopic myomectomy provides advantages as a minimally invasive procedure. To facilitate the closure of the uterine wound after enucleation of the fibroid, barbed sutures have been introduced as they can shorten the operative time and reduce the amount of bleeding. However, the use of barbed suture is not without risk. There were a few reports on the risks of barbed sutures in the literature. We report herein a case of acute abdomen because of small bowel entrapment and obstruction following the use of barbed suture in laparoscopic myomectomy. Surgeons using barbed suture in myomectomy should be vigilant on the possibility of this bowel complication whenever adverse clinical situation arises as the outcome could be serious if the condition was left unchecked.
1. Introduction
Laparoscopic myomectomy is commonly performed nowadays because of its advantages as a minimally invasive approach, with less postoperative pain, better cosmesis, shorter hospital stay, and quicker recovery. Laparoscopic myomectomy consists of the following essential steps of fibroid enucleation, suture repair of uterine wound, and the extraction of fibroid specimens through a small portal incision. Laparoscopic suturing technique is a requisite for repair of the uterine wound which is an integral part of myomectomy. Yet one has to go through a long learning curve before one can master the skill of laparoscopic suturing and knot tying to pursue this laparoscopic approach, but often some surgeons find the technique of suturing laparoscopically very skill demanding. Proficiency in laparoscopic suturing is essential not only in serving a proper approximation of the uterine wound, with occlusion of dead spaces, as well as to control any bleeding. Conventional sutures carry the drawbacks of requirement for tying surgical knots for anchorage, higher density of foreign suture material, need to maintain constant tension on the suture, risk of strangulating the tissue with excessive tension, and the reduction in the tension necessary to hold tissues together postoperatively. On the contrary, barbed suture with its special design can eliminate knots altogether because of its non-slip attribute. Although barbed sutures are frequently used in myomectomy [1], bowel complications associated with their use in laparoscopic myomectomy was seldom reported [2], [3], [4]. This case report describes a late complication of entrapment and erosion of the small bowel following the use of barbed suture in laparoscopic myomectomy, and a review of the literature is presented.
2. Presentation of case
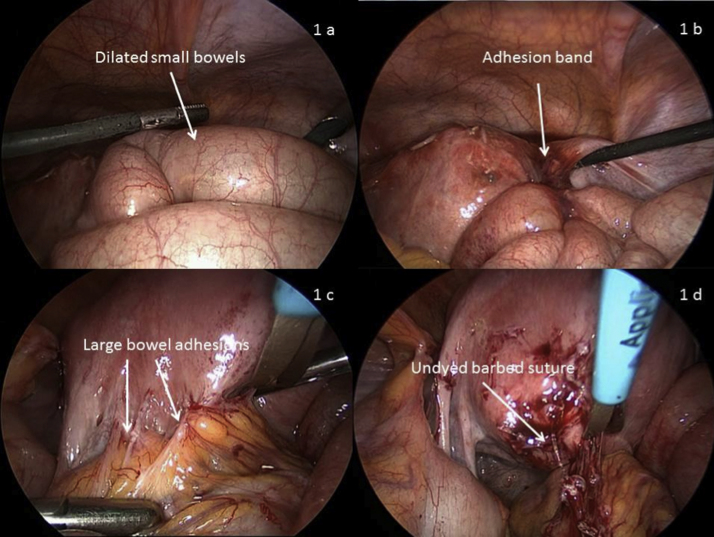
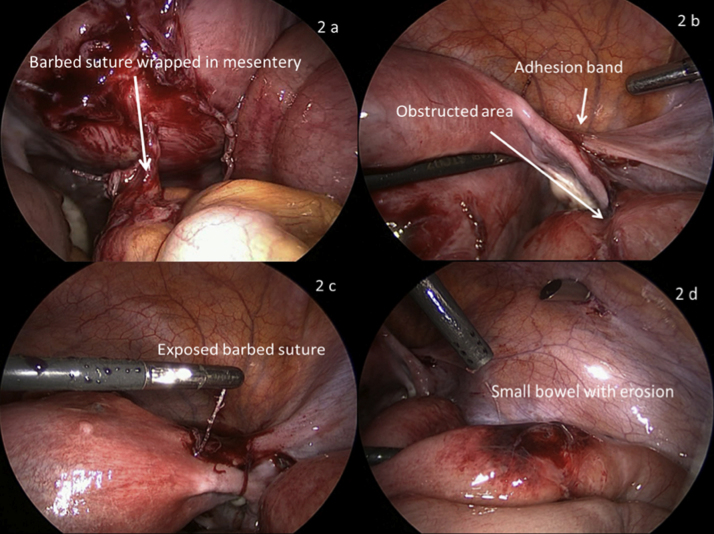
A 33 year-old woman presented as an emergency with severe abdominal pain. The pain became progressively severe. She had regular monthly cycles and she was on the third day of her period. Six weeks ago, hysteroscopy and laparoscopic myomectomy were performed for heavy periods and multiple fibroids. On admission she was afebrile and her vital signs were within normal range. The abdomen was mildly distended and there were significant tenderness and rebound tenderness on palpation. Vaginal examination also elicited marked tenderness on rocking of the cervix. Transvaginal ultrasound scan showed a bulky uterus of normal configuration and normal looking ovaries. No adnexal mass was detected. A small collection of fluid was present in the Pouch of Douglas. In view of the presence of signs consistent with acute peritonitis, an emergency laparoscopy proceeded. Blood stained fluid was found at the vesico-uterine pouch and the Pouch of Douglas. Some small bowels were moderately dilated (Fig. 1a). A loop of small bowel was firmly adhered to the right uterine cornu through a band of adhesion (Fig. 1b), causing an obstruction. Posteriorly the rectum was extensively adhered to the back of the uterus on the left side (Fig. 1c). The adhesions over the rectum were careful lysed using both blunt and sharp dissection. A strand of undyed suture with spiral barbs connecting to the uterus (Fig. 1d) was found to be buried in the mesentery of the rectum (Fig. 2a). The suture was cut and removed and thereby freeing the rectum. The integrity of the rectum was checked and confirmed. The adhesion band connecting the small bowel to the uterus was separated after yielding to gentle traction and counter-traction applied to both organs (Fig. 2b). Thereafter, an undyed barbed suture was revealed following the release of the small bowel (Fig. 2c). Inspection of the detached small bowel revealed the presence of a 2 cm × 1 cm erythematous area that corresponded to the site of the prior adhesion (Fig. 2d). Careful examination of the area concerned showed only erosion of the serosal aspect of the small bowel without any perforation. Suturing of the eroded area using 3/0 Vicryl on the sero-muscular layer of the bowel was performed. All remaining redundant barbed sutures seen arising over the rest of the uterus were excised flush with the myometrium. Peritoneal lavage was then carried out before completion of the procedure. The patient recovered well and was discharged home on the second postoperative day when examination revealed a soft abdomen and that she was able to tolerate food and passed bowel motion.
Fig. 1.
(a) showed dilated small bowels; (b) adhesion band between small bowel and uterus; (c) adhesions between large bowel and uterus; (d) barbed suture arising from uterus exposed after adhesiolysis.
Fig. 2.
(a) barbed suture wrapped in mesentery; (b) showed adhesion band and obstructed area on the small bowel; (c) barbed suture exposed from the uterus; (d) erosion on small bowel.
3. Discussion
Barbed suture was first patented for the use in surgical procedures in 1999. The bidirectional barbed suture Quill™ SRS (Angiotech Pharmaceuticals, Inc., Vancouver, BC, Canada) was approved by the FDA in 2004. Thereafter, the barbed suture V-Loc™ (Covidien, Mansfield, MA, USA) and the Stratafix® (Angiotech Pharmaceuticals and Ethicon Endo-Surgery) have been introduced into the market in 2009 and 2013 respectively. Despite their practical advantages, the use of barbed sutures in surgery has to be careful as it is not without risks. Reports on bowel complication arising from the use of barbed sutures had been published, but the number remained small.
Api et al. in 2015 in a randomized controlled trial in rats found that the barbed suture material was associated with adhesion formation when used intra-abdominally and these adhesions could not be prevented by peritonization [5].
One of the serious complications from the use of barbed suture in surgery is bowel obstruction. Kindinger et al., 2012 reported a case of small bowel entanglement and obstruction involving an unraveled V-Loc suture 4 weeks following a laparoscopic myomectomy. In their case, the myometrial defects were closed in two layers with V-Loc to the uterine serosa and SprayShield™ (Covidien, Waltham, MA) was also applied as an adhesion barrier. They highlighted that the bowel obstruction was likely due to the presence of barbs that had contributed to the bowel entanglement [2]. The bowel complication did not seem to relate to the type of barbed sutures. Rombaut et al., 2014 reported a case of bowel obstruction due to the bidirectional Quill suture causing strangulation of the terminal ileum 3 weeks following a laparoscopic myomectomy [4].
Apart from myomectomy, the use of the barbed suture in the closure of the peritoneum had also been implicated to cause bowel complications. Thubert et al., 2011 reported a case of small bowel volvulus following peritoneal closure at laparoscopic sacral colpopexy using a barbed suture and the patient presented with bowel obstruction 1 month after the procedure [6]. A similar case of bowel obstruction was reported only 8 days postoperatively with diffuse abdominal pain and vomiting and it was caused again by a barbed suture which was inserted for closure of the peritoneum in promonofixation [7]. Small bowel obstruction could present as early as 1 day following the use of barbed suture in closure of peritoneum after laparoscopic ventral mesh rectopexy [8]. Laparoscopic hysterectomy also accounted for a case of bowel complication from the use of barbed suture used for the closure of vaginal vault [9].
A point of interest is the use of adhesion barriers in laparoscopic myomectomy when barbed suture is employed. With the short term degradable sutures like the Stratafix Spiral PGA-PCL Device and the V-Loc 90 Absorbable Device which have an absorption time of 90–120 days and the long term degradable sutures like the Stratafix Spiral PDO and the V-Loc 180 Absorbable Device which have an absorption time of 120–180 days, one can envisage that the use of adhesion barriers like GYNECARE INTERCEED (Ethicon, Johnson and Johnson) and Seprafilm (Genzyme Corporation, Cambridge, MA) which work by physically separating apposing tissue surfaces during the period of reperitonization in preventing formation of pelvic adhesions cannot be effective enough in the presence of exposed barbed suture because these adhesion barriers would be absorbed well within 4 weeks, a time well before a barbed suture is absorbed. This could possibly account for the failure of SprayShield™ used by Kindinger to prevent adhesion [2].
Given the findings of exposed barbed sutures in nearly all cases of bowel complications as well as the finding of adhesion formation of barbed sutures despite peritonization in animal, we are of the view that the length for the end of the barbed suture that would be exposed should be kept to a minimum, and if possible avoid exposing any barbed suture in the peritoneal cavity. Although the use of adhesion barriers might still be useful to prevent wound adhesions, but it probably might not prevent bowel complications due to an exposed barbed suture.
4. Conclusion
The reason to account for the small bowel entanglement in this case was the presence of ‘free’ suture in the peritoneal cavity as it invited adhesions formation and subsequently the bowel obstruction. The suture length had been left too long beyond its exit point on the myometrium and the situation could possibly have been made worse upon the shrinkage of the tissues during the healing process. This complication could have been avoided if there was no exposure of the ‘free’ barbed suture in the peritoneal cavity either through leaving no redundant suture material by cutting the suture flushed with the myometrium or to use the convention suture for repair of the seromuscular layer of the myometrium. In the event that such complication is to happen, a high index of suspicion is necessary in making an early diagnosis and prompt action has to be taken to alleviate major bowel complications that carry a grave prognosis.
Conflicts of interest
No conflicts of interest.
Written informed consent
“Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request”.
Funding for your research
No funding required.
Ethical approval
No ethical approval required for case report in our institute.
Consent
Patient’s consent obtained.
Authors’ contribution
We are co-authors.
Guarantor
Nil.
Acknowledgement
No disclosure or no funding.
References
- 1.Angioli R. A new type of absorbable barbed suture for use in laparoscopic myomectomy. Int. J. Gynecol. Obstet. 2012;117(3):220–223. doi: 10.1016/j.ijgo.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 2.Kindinger L., Setchell T., Miskry T. Bowel obstruction due to entanglement with unidirectional barbed suture following laparoscopic myomectomy. Gynecol. Surg. 2012;9(3):357–358. [Google Scholar]
- 3.Burchett M.A., Mattar S.G., McKenna D.T. Iatrogenic intestinal and mesenteric injuries with small bowel volvulus following use of barbed suture during laparoscopic myomectomy. J. Laparoendosc. Adv. Surg. Tech. 2013;23(7):632–634. doi: 10.1089/lap.2013.0065. [DOI] [PubMed] [Google Scholar]
- 4.Rombaut S. Quill barbed suture-related complication. Gynecol. Surg. 2012;9(3):359–361. [Google Scholar]
- 5.Api M. Peritoneal closure over barbed suture to prevent adhesions: a randomized controlled trial in an animal model. J. Minim. Invasive Gynecol. 2015;22(4):619–625. doi: 10.1016/j.jmig.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 6.Thubert T., Pourcher G., Deffieux X. Small bowel volvulus following peritoneal closure using absorbable knotless device during laparoscopic sacral colpopexy. Int. Urogynecol. J. 2011;22(6):761–763. doi: 10.1007/s00192-010-1348-1. [DOI] [PubMed] [Google Scholar]
- 7.Buchs N.C. Intestinal obstruction following use of laparoscopic barbed suture: a new complication with new material? Minim. Invasive Ther. Allied Technol. 2011;21(5):369–371. doi: 10.3109/13645706.2011.638643. [DOI] [PubMed] [Google Scholar]
- 8.Vasudevan S., Dworkin M. Small bowel obstruction following laparoscopic ventral mesh rectopexy. Colorectal Dis. 2013;15(12):1543–1544. doi: 10.1111/codi.12402. [DOI] [PubMed] [Google Scholar]
- 9.Donnellan N.M., Mansuria S.M. Small bowel obstruction resulting from laparoscopic vaginal cuff closure with a barbed suture. J. Minim. Invasive Gynecol. 2011;18(4):528–530. doi: 10.1016/j.jmig.2011.03.011. [DOI] [PubMed] [Google Scholar]