Highlights
-
•
Identify the preoperative radiologic features of adrenal hemangioma.
-
•
We examine the better surgical approach for adrenal tumors and adrenal hemangioma.
-
•
Controindication to laparoscopic adrenalectomy.
Keywords: Adrenal hemangioma, Adrenal cavernous hemangioma, Laparoscopic adrenalectomy, Laparoscopy, Laparoscopic surgery
Abstract
Introduction
Cavernous hemangioma of the adrenal gland is a rare benign tumor. The diagnosis is often postoperative on histological exam with the presence of blood-filled, dilated vascular spaces.
Presentation of case
We report the clinical case of a 49 years-old woman who came to our observation with aspecific abdominal pain. A computed tomography (CT) abdominal scan revealed a 11 cm right adrenal mass. This lesion was well circumscribed, round, encapsulated. After iodinated-contrast we observed a progressive, inhomogeneous enhancement without evidence of active bleeding and with pre-operative diagnosis of adrenal hemangioma. Laparoscopic adrenalectomy was performed by a transperitoneal flank approach. Pathological examination revealed a 11 cm adrenal mass with extensive central necrotic areas mixed to sinusoidal dilation and fibrotic septa. Postoperative diagnosis was adrenal hemangioma.
Discussion
Adrenal hemangiomas occur infrequently. Generally these adrenal masses are non-functioning and there is no specific symptoms. Recent records demonstrate that laparoscopic adrenalectomy is technically safe and feasible for large adrenal tumors, but controversy exists in cases of suspected malignancy. We choose laparoscopic approach to adrenal gland on the basis of preoperative CT abdominal scan that excludes radiological signs of adrenocortical carcinoma (ACC) such as peri-adrenal infiltration and vascular invasion.
Conclusion
Laparoscopic adrenalectomy is considered the standard treatment in case of diagnosis of benign lesions. In this case report we discussed a large adrenal cavernous hemangioma treated with laparoscopic approach. Fundamental is the study of preoperative endocrine disorders and radiologic findings to exclude signs of malignancy.
1. Introduction
Cavernous hemangioma of the adrenal gland is a rare benign tumor. The diagnosis is often postoperative on histological exam with the presence of blood-filled, dilated vascular spaces. These adrenal masses are usually non-functioning and the clinical presentation is usually incidental with no specific abdominal symptoms. Johnson and Jeppesen published the first report of adrenal hemangioma in 1955 [1] and today there are about 90 cases documented in literature.
2. Presentation of case
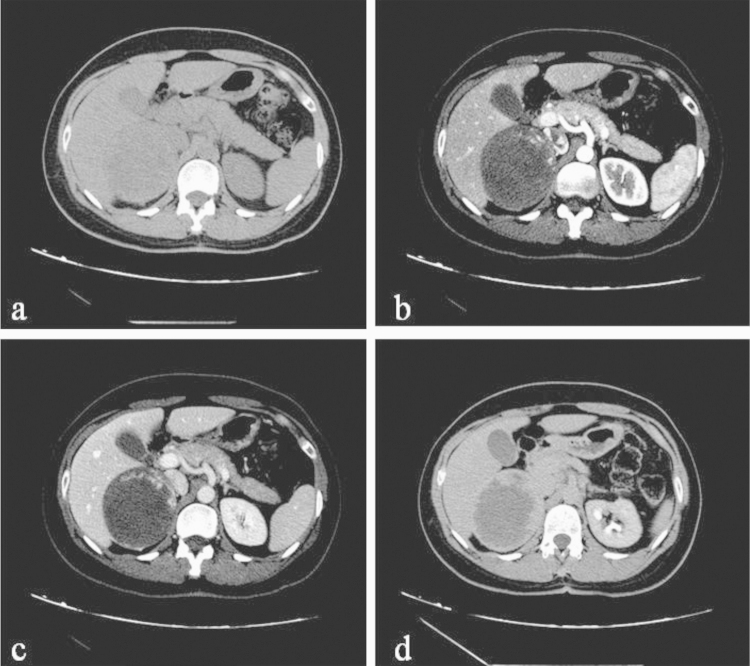
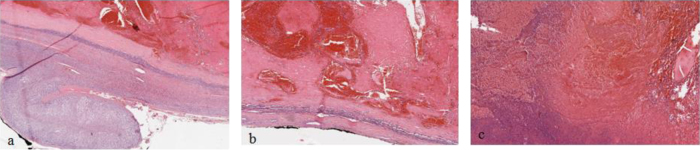
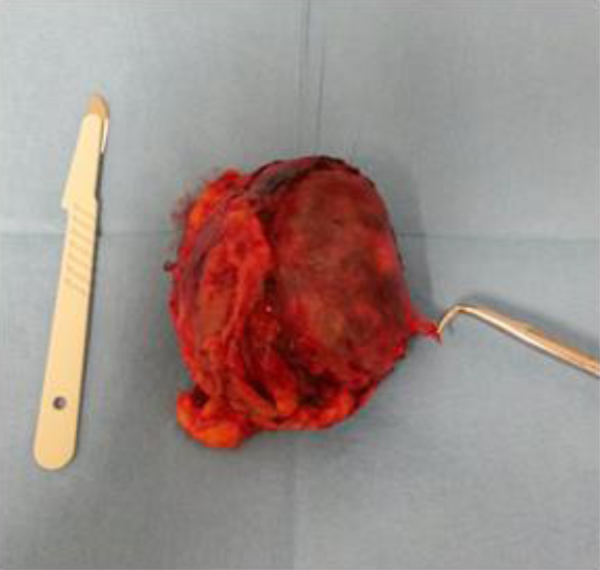
We report the clinical case of a 49 years-old woman who came to our observation with aspecific abdominal symptoms like acute epigastric pain, nausea and vomiting. She had never experienced similar pain in the past and the symptoms were progressive. She had hypertension but no other comorbidities [2]. We performed routine blood tests (Hb 13.2 g/dl, WBC 11000). On clinical examination, the patient had significant pain in epigastric and right flank region, but there were no signs of acute cholecystitis or peritonitis. So, we decided to perform a computed tomography (CT) abdominal scan that revealed a 11 cm right adrenal mass. This lesion was well circumscribed, round, encapsulated. After iodinated-contrast we observed a progressive, inhomogeneous enhancement without evidence of active bleeding and with pre-operative diagnosis of adrenal hemangioma (Fig. 1) [3]. The left adrenal gland was normal and there were no others significant radiologic findings. Abdominal magnetic resonance imaging (MRI) was not performed in this patient. The patient did not have clinical features suggestive of a functioning adrenal tumor, but we however performed complete hormonal tests. The diagnosis of pheochromocytoma was excluded with normal levels of urinary catecholamines on 24 h collection [4]. The only size of lesion was not considered a contraindication to laparoscopic approach, but we considered the possibility of conversion to open surgery in case of peri-adrenal infiltration or vascular invasion. Laparoscopic adrenalectomy (LA) was performed by a transperitoneal flank approach in the left lateral decubitus position with an inclination of 50–60° relative to the operating table which is broken to extend the space between the last rib and the iliac crest [5]. We used Veress needle to induce pneumoperitoneum and then we positioned four trocars in the right subcostal region [6]. The right lobe of the liver was mobilized by division of triangular ligament. Then the peritoneum overlying the right adrenal gland, in Albarran–Chatelin space, was dissected using harmonic scalpel. Adrenal mass appeared with regular margins and a thin fibrous capsula without invasion of periadrenal organs. Tissue dissection along the lateral border of the inferior vena cava allowed the identification of a very short adrenal vein which was clipped and divided. Then, by dissecting from medial to lateral and from inferior to superior the gland was mobilized until it was completely free. We positioned a tubular drainage in subhepatic space. At the end of the procedure the tumor was positioned in endo-bag and removed with a sovrapubic mini-laparotomy. Operative time was 145 min and blood loss 50 mL. The post-operative hospital stay was 3 days. Pathological examination revealed a 11 cm × 7.5 cm × 7 cm adrenal mass weighted 260 g with peripheral sectors of regular adrenal tissue (Fig. 2). Microscopically, extensive central necrotic areas were found mixed to sinusoidal dilation and fibrotic septa with post-operative diagnosis of adrenal hemangioma (Fig. 3). There was no evidence of malignancy.
Fig. 1.
(a) noncontrast-enhanced CT scan showing encapsulate large right adrenal lesion with regular margins; (b–d) contrast-enhanced CT images obtained in arterial, portal and late phase, 3 min after iodinated contrast administration, showing a hypodense centre with no infiltration of peri-adrenal organs.
Fig. 2.
Resected adrenal gland with a smooth surface and adrenal vein.
Fig. 3.
(a) representative tissue section with residual adrenal parenchyma (H&E 10x); (b) multiple dilated interconnecting vascular channels with thrombosis (H&E 20x); (c) areas of hemorrhage and necrosis (H&E 40 x).
3. Discussion
Adrenal incidentalomas are adrenal tumors, greater than 1 cm, identified with imaging performed for other indications. With the major diffusion of ultrasonography and CT these lesions are always more frequent. On the other side the general advantages of the laparoscopic approach [7], [8], [9] enlarge the indications for surgical treatment of adrenal masses. Adrenal hemangiomas occur infrequently. The causes of these tumors are unknown, probably many of these are congenital with involvement of hereditary factors and ectasia of blood vessels [10]. Generally these adrenal masses are non-functioning and there are no specific symptoms. In this case we find a large non-functioning adrenal mass without radiological signs of malignancy. LA is today considered the standard treatment for benign adrenal tumors and the size cannot be considered as an absolute contraindication to laparoscopy. From literature review the largest adrenal hemangioma treated by laparoscopy had a diameter of 12 cm [11]. Recent records demonstrate that laparoscopic adrenalectomy is technically safe and feasible for large adrenal tumors, but controversy exists in cases of suspected malignancy. We choose laparoscopic approach to adrenal gland on the basis of preoperative CT abdominal scan that excludes radiological signs of adrenocortical carcinoma (ACC) such as peri-adrenal infiltration and vascular invasion [12]. The typical findings of adrenal hemangioma on CT scan include a heterogeneous, hypodense lesion with variable calcification due to phleboliths within the dilated vascular spaces of the lesion [13]. On histopathological inspection most of the tumors reported are cavernous and rarely in capillary type. We can also describe degenerative changes like thrombosis, hemorrhage, necrosis and calcification. Surgical treatment is indicated in case of adrenal masses larger than 3.5 cm because (1) in literature cavernous hemangioma can be associated with malignant hemangioendothelioma and (2) some authors described also risk of traumatic or spontaneous bleeding with retroperitoneal hematoma and hypovolemic shock treated with laparotomic approach [14], [15]. Laparoscopic adrenalectomy reducing surgical trauma can reduce the manipulation of the gland and the risk related to this surgery. Despite these features the traditional open technique is the most frequent approach described in literature for the treatment of adrenal hemangiomas, especially in the past.
4. Conclusion
Laparoscopic adrenalectomy is considered the standard treatment in case of diagnosis of benign lesions. In this case report we discuss a large adrenal cavernous hemangioma treated with laparoscopic approach. In most cases these lesions appear as non-functioning adrenal masses. Anyway, fundamental is the study of preoperative endocrine disorders to exclude functioning tumors. In this case the pre-operative radiologic findings of cavernous hemangioma and the absence of signs of local invasion induced us to perform a laparoscopic adrenalectomy. In presence of local invasion or vascular infiltration LA should be converted to the open technique. So the better decision for the correct management of these tumors should be based on the patient factors, endocrine studies, radiologic characteristics and the experience of the operator.
Contributor Information
A. Agrusa, Email: antonino.agrusa@unipa.it.
G. Romano, Email: giorgio.romano@unipa.it.
G. Salamone, Email: salamone.giuseppe@unipa.it.
G. Di Buono, Email: g.dibuono@libero.it.
D. Chianetta, Email: chianetta83@libero.it.
V. Sorce, Email: vincenzosorce@me.com.
M. Galia, Email: massimo.galia@unipa.it.
G. Gulotta, Email: gaspare.gulotta@unipa.it.
References
- 1.Johnson C.C., Jeppesen F.B. Hemangioma of the adrenal. J. Urol. 1955;74(November (5)):573–577. doi: 10.1016/S0022-5347(17)67320-8. [DOI] [PubMed] [Google Scholar]
- 2.Novo G., Corrado E., Tortorici E., Novo A., Agrusa A., Saladino V., Marturana I., Lentini R., Ferrandes M., Visconti C., Massenti F., D’Arienzo M., Vitale F., Gulotta G., Novo S. Cardiac risk stratification in elective non-cardiac surgery: role of NT-proBNP. Int. Angiol. 2011;30(June (3)):242–246. [PubMed] [Google Scholar]
- 3.Galea N., Noce V., Ciolina F., Liberali S., Francone M. Giant adrenal cavernous hemangioma: a rare abdominal mass. Urology. 2013;82(July (1)):e3–e4. doi: 10.1016/j.urology.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Romano G., Agrusa A., Chianetta D., Frazzetta G., Sorce V., Di Buono G., Gulotta G. Laparoscopic management of adrenal tumors: a four-year experience in a single center. Minerva Chirurgica. 2014;69(2):125–129. Suppl. 1. [Google Scholar]
- 5.Agrusa A., Romano De Vita G.G., Frazzetta G., Chianetta D., Di Buono G., Gulotta G. Adrenal gunshot wound: Laparoscopic approach. Report of a case. Int. J. Surg. Case Rep. 2014;5(2):70–72. doi: 10.1016/j.ijscr.2013.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agrusa A., Romano G., Frazzetta G., Chianetta D., Sorce V., Di Buono G., Gulotta G. Laparoscopic adrenalectomy for large adrenal masses: single team experience. Int. J. Surg. 2014;12(Suppl. 1):S72–S74. doi: 10.1016/j.ijsu.2014.05.050. [DOI] [PubMed] [Google Scholar]
- 7.Agrusa A., Romano G., Frazzetta G., Chianetta D., Sorce V., Di Buono G., Gulotta G. Role and outcomes of laparoscopic cholecystectomy in the elderly. Int. J. Surg. 2014;12(Suppl. 2):S37–S39. doi: 10.1016/j.ijsu.2014.08.385. [DOI] [PubMed] [Google Scholar]
- 8.Agrusa A., Romano G., Cucinella G., Cocorullo G., Bonventre S., Salamone G., Di Buono G., De Vita G., Frazzetta G., Chianetta D., Sorce V., Bellanca G., Gulotta G. Laparoscopic, three-port and SILS cholecystectomy: a retrospective study. G Chir. 2013;34(September–October (9–10)):249–253. [PMC free article] [PubMed] [Google Scholar]
- 9.Romano G., Agrusa A., Frazzetta G., De Vita G., Chianetta D., Di Buono G., Amato G., Gulotta G. Laparoscopic drainage of liver abscess: case report and literature review. G Chir. 2013;34(May–June (5–6)):180–182. doi: 10.11138/gchir/2013.34.5.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noh J.J., Choi S.H., Hwang H.K., Kang C.M., Lee W.J. Adrenal cavernous hemangioma: a case report with review of the literature. JOP. 2014;15(May (3)):254–257. doi: 10.6092/1590-8577/2402. Review. [DOI] [PubMed] [Google Scholar]
- 11.Telem D.A., Nguyen S.Q., Chin E.H., Weber K., Divino C.M. Laparoscopic resection of giant adrenal cavernous hemangioma. JSLS. 2009;13:260–262. [PMC free article] [PubMed] [Google Scholar]
- 12.Benassai G., Desiato V., Benassai G., Bianco T., Sivero L., Compagna R., Vigliotti G., Limite G., Amato B., Quarto G. Adrenocortical carcinoma: what the surgeon needs to know. Case report and literature review. Int. J. Surg. 2014;12(Suppl. 1):S22–S28. doi: 10.1016/j.ijsu.2014.05.030. [DOI] [PubMed] [Google Scholar]
- 13.Edwards J.P., Stuart H.C., Urbanski S.J., Pasieka J.L. A rare cavernous hemangioma of the adrenal gland. Int. J. Surg. Case Rep. 2014;5(2):52–55. doi: 10.1016/j.ijscr.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Forbes T.L. Retroperitoneal hemorrhage secondary to a ruptured cavernous hemangioma. Can. J. Surg. 2005;48(February (1)):78–79. [PMC free article] [PubMed] [Google Scholar]
- 15.Agrusa A., Romano G., Chianetta D., De Vita G., Frazzetta G., Di Buono G., Sorce V., Gulotta G. Right diaphragmatic injury and lacerated liver during a penetrating abdominal trauma: case report and brief literature review. World J. Emerg. Surg. 2014;25(April):33. doi: 10.1186/1749-7922-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]