Abstract
Objective To apply resilience theory and the extant literature to propose a resilience-risk model for pediatric chronic pain and provide an agenda for research and clinical practice in pediatric chronic pain resilience. Method Literature review to develop a resilience-risk model for pediatric chronic pain. Results The chronic pain literature has identified unique individual and social/environmental resilience resources and pain-related resilience mechanisms that promote pain adaptation. These data support our ecological resilience-risk model for pediatric chronic pain, and the model highlights novel directions for clinical and research efforts for youth with chronic pain. Conclusions The examination of pediatric chronic pain from a strengths-based approach might lead to novel clinical avenues to empower youth to positively adapt and live beyond their pain.
Keywords: chronic and recurrent pain, coping skills and adjustment, psychosocial functioning, resilience
Prevalence rates suggest that 11–38% of children and adolescents experience recurrent or chronic pain, with approximately 5% experiencing significant pain-related dysfunction (King et al., 2011). Our collective energy has focused predominately on understanding and designing treatments that target pain, emotional distress, and disability in pediatric patients with chronic pain. This approach highlights critical areas to be mitigated; however, we have largely neglected strengths (e.g., acceptance, optimism) or resilient qualities that can be fostered in children to optimize living with chronic pain.
Resilience is defined as a person’s ability to respond effectively to risk or adversity (Masten, 2001). Determining how to assess and quantify resilience proves complex and challenging. In the context of pediatric chronic pain, a child’s resilience might be conceptualized as the personal resources and effective responding that protect from dysfunction, lead to adaption, or result in well-being and growth. Resilience is a dynamic and multisystemic process that originates within the individual and is enhanced through developmental, social, cultural, and environmental factors (Masten, 2001).
The purpose of this review is to (1) propose a resilience-risk model specific to pediatric chronic pain, (2) evaluate empirical evidence for protective resources and pain-related mechanisms within the proposed model, and (3) provide an agenda for future research and clinical practice in resilience in pediatric chronic pain.
A Resilience-Risk Model for Pediatric Chronic Pain
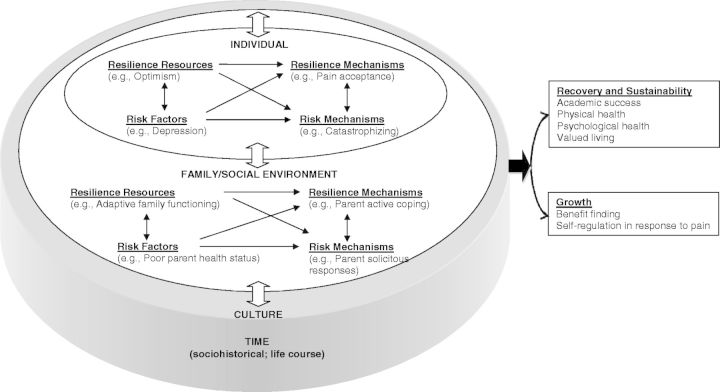
Resilience in chronic pain has primarily been examined among adults. Sturgeon and Zautra (2013) developed the predominant risk-resilience model in adult chronic pain, illustrating the interplay of “resilience resources” and “resilience mechanisms” in the context of pain. Although there are no published risk-resilience models in pediatric pain, this framework has been applied to other pediatric chronic illness populations (e.g., diabetes and asthma), and these models identify multilevel processes that promote health, illness management, adaptability, and psychosocial functioning (Hilliard, Harris, & Weissberg-Benchell, 2012; Koinis-Mitchell et al., 2012). When targeting pediatric patients, it is important to acknowledge the various factors impacting their functioning. Bronfenbrenner’s ecological systems theory (Bronfenbrenner, 1979)—which identifies environmental, societal, and developmental influences on children’s maturation and adaptation to adversity—is particularly relevant to pediatric chronic pain (Cohen, MacLaren, & Lim, 2008). The conceptual frameworks described above provided the basis for our ecological resilience-risk model in pediatric chronic pain (Figure 1). Our model includes resilience resources, mechanisms, and outcomes that have either been previously identified in the broader resilience literature or have received empirical support within the chronic pain literature. We maintained model pathways proposed in Sturgeon and Zautra’s adult chronic pain risk-resilience model, but added variables that have received empirical support in the pediatric chronic pain literature. Lastly, we provided an ecological context to highlight other variables that have been shown to impact pediatric chronic pain. Variables in each level have a bidirectional relation with variables contained within surrounding levels. Although we included widely identified risk factors in our model given their prominence in the pediatric chronic pain literature, thorough discussion of these variables is beyond the scope of this review.
Figure 1.
Ecological resilience-risk model in pediatric chronic pain.
Note. Within this model, resilience resources promote adaptive outcomes by enhancing resilience mechanisms and minimizing risk factors and mechanisms. Conversely, risk factors interfere with resilience and contribute to poor pain adaptation by enhancing risk mechanisms and minimizing resilience factors and mechanisms. These risk and resilience pathways occur within the context of the individual, the family/social environment, culture, and time, which mutually interact with one another.
Resilience Resources in Pediatric Chronic Pain
Research has identified stable individual traits and familial/social factors that appear to serve as resilience resources in the context of chronic pain.
Individual Resilience Resources
One trait that has received attention in the health psychology literature is optimism, defined as generalized favorable expectancies for the future (Scheier & Carver, 1985). Optimism predicted pain-related adjustment and adaptation among healthy adults in laboratory settings and adults with chronic pain (Goodin & Bulls, 2013) and predicted better quality of life via minimizing pain-related fear and catastrophizing in a sample of youth with chronic pain (Cousins, Cohen, & Venable, 2015).
Another important resilience trait is mindfulness, the nonjudgmental focus on and acceptance of present moment experiences (Kabat-Zinn, 1996). A recent study with a community sample of adolescents revealed that in the context of daily pain, trait mindfulness predicted decreased pain interference, which was partially mediated by catastrophizing. In the context of acute experimental pain, adolescents with greater mindfulness endorsed fewer catastrophic thoughts during a cold pressor task, which reduced their self-reported pain and increased their pain tolerance (Petter, Chambers, McGrath, & Dick, 2013).
Minimal empirical attention has been given to the impact of positive affect (i.e., positive emotion) on pediatric pain adaptation; however, adult chronic pain studies support its role as a resilience resource. In the context of adult chronic pain, higher general positive affect predicted lower levels of pain in subsequent weeks among women with osteoarthritis and fibromyalgia (Zautra, Johnson, & Davis, 2005).
Family and Social-Environmental Resilience Resources
Social support or strong social ties might serve a protective role for individuals with chronic pain. The unpredictable and disabling features of chronic pain limit typical social experiences among youth and impact social information processing; however, positive peer relationships can strengthen perceived social competence and development (Forgeron et al., 2011). Prior research also suggests that positive social functioning or social connectedness may mitigate the detrimental effects of the pain experience on school functioning (Simons, Logan, Chastain, & Stein, 2010). In addition to positive peer relationships at school, there is evidence illustrating the protective role of perceived teacher support of children’s and adolescents’ autonomy and competence in buffering against the relation between pain severity and school absenteeism and experiences of bullying (Vervoort, Logan, Goubert, De Clercq, & Hublet, 2014).
Parent support and family functioning are additional resilience resources that may promote pain-related coping, pain management, and adjustment. Although research has provided strong support for the negative impact of pediatric chronic pain on parent stress, emotional functioning, pain-related cognitions and behaviors, and family functioning (Palermo, Valrie, & Karlson, 2014), there is limited research focused on supportive parent and family resilience factors that contribute to pain adaptation. Overall, clear communication, well-defined roles and structure, cohesion, adaptability, effective problem solving, and affect regulation all contribute to adaptive family functioning (Palermo et al., 2014).
Resilience Mechanisms in Pediatric Chronic Pain
In contrast to resilience resources, resilience mechanisms are dynamic, modifiable, and potentially active processes when confronting pain (e.g., cognitions, affect, behaviors).
Individual Resilience Mechanisms
The psychological flexibility model (McCracken & Morley, 2014) has recently been applied to research and treatment for chronic pain. Psychological flexibility is the ability to be present-focused and act effectively and consistently with personal values in the presence of interfering thoughts, emotions, and bodily sensations. Psychological flexibility has been shown to be a mediator of change following ACT (Acceptance and Commitment Therapy; Hayes, Strosahl, & Wilson, 1999) treatment for adolescents (Wicksell, Olsson, & Hayes, 2011) with chronic pain.
A key part of psychological flexibility is the ability to acknowledge and accept difficult sensations and experiences. The construct of acceptance has gained increasing attention and empirical support in the pediatric pain literature (McCracken & Morley, 2014). Pain acceptance might be defined as an individual’s willingness to live life with pain without efforts to control or avoid it to pursue a life consistent with personal values. Increased pain acceptance in the context of interdisciplinary chronic pain rehabilitation predicts decreases in depressive symptoms, pain catastrophizing, and functional disability among children and adolescents (Weiss et al., 2013).
Another process underlying psychological flexibility is committed action. Committed action refers to goal-directed, flexible persistence that enables individuals to live a values-based life. Committed action as measured in adults with chronic pain predicts psychological health and vitality beyond that of pain and pain acceptance (McCracken, 2013).
Self-efficacy is a resilience mechanism that influences pain management and associated situations and denotes belief in the ability to function effectively while experiencing pain (Bursch, Tsao, Meldrum, & Zeltzer, 2006). Pain self-efficacy is associated with better emotional and physical functioning and higher levels of self-esteem (Bursch et al., 2006). Among youth with chronic headache, self-efficacy served as a partial mediator of the relation between pain-related fear and disability and pain-related fear and school functioning (Carpino, Segal, Logan, Lebel, & Simons, 2014). In another recent study among youth with chronic headache, pain self-efficacy in tandem with pain acceptance was associated with less disability, better school functioning, and fewer depressive symptoms, and predicted less functional disability after controlling for demographic and pain-related variables (Kalapurakkel, Carpino, Lebel, & Simons, 2015).
Family and Social-Environmental Resilience Mechanisms
Substantial evidence supports the impact of parent emotions, cognitions, and behaviors on child functioning and pain management in the context of chronic pain (Palermo et al., 2014). Parent catastrophizing and solicitous responses, or frequent attending to a child’s pain symptoms, encourage activity avoidance and enhance disability (Welkom, Hwang, & Guite, 2013). Contrastingly, adaptive parent responses to pain (i.e., parent modeling of active coping or problem-solving and promotion of behavioral activation) are resilience mechanisms that have received less empirical attention in the chronic pain literature. Parent pain acceptance (Smith, Sieberg, Odell, Randall, & Simons, 2015) and the broader construct, parent psychological flexibility, encompassing values-based action, pain acceptance, emotional acceptance, and pain willingness, have initial support as promising resilience mechanisms (Wallace, McCracken, Weiss, & Harbeck-Weber, 2015). Positive social interactions with family or peers would also benefit from further study.
Resilience Outcomes
Resilience outcomes are classified into three primary domains: recovery (i.e., resumed functioning), sustainability (i.e., perseverance with valued activities), and growth (i.e., realization and better understanding of one’s capabilities) (Reich, Zautra, & Hall, 2010). Primary outcomes of recovery and sustainability that are pertinent to the pediatric pain population and often compromised by pain include academic success, physical health, psychological health, and valued living/quality of life. Primary outcomes of growth include benefit finding and self-regulation in response to pain. Benefit finding or posttraumatic growth refers to the positive changes or gains (e.g., sense of purpose, deepened relationships) associated with a significant adversity that facilitates positive adjustment. Benefit finding has been assessed in other pediatric populations, such as pediatric cancer (Phipps, Long, & Ogden, 2007). Self-regulation is defined as the ability to modulate cognitions, emotions, and behavior toward a goal. This construct has recently been proposed as the foundation of individual and interpersonal processes that contribute to risk and resilience for pediatric chronic illness self-management and health behaviors (Lansing & Berg, 2014).
Agenda for Researchers and Clinicians
Based on our proposed ecological resilience-risk model in pediatric pain, we detail the following agenda:
Incorporate resilience resources, mechanisms, and outcomes in pediatric chronic pain research and test model pathways. Unexplored dimensions include positive affect, positive social interactions, benefit finding, and self-regulation in response to pain (Table I).
Develop and validate measures of resilience resources, mechanisms, and relevant outcomes for children with chronic pain (e.g., committed action, self-regulation in response to pain, pain-related self-efficacy/sense of controllability).
Engage in multidisciplinary collaborations to advance the field. For example, exploring neural implications of resilience through neuroimaging and neuroscience research may bridge connections between thoughts, emotions, behaviors, and cortical activity within endogenous pain-inhibitory pathways and brain regions.
Study those individuals who have chronic pain but do not suffer from chronic pain. We tend to rely on convenience samples and target patients who present in specialty clinics likely owing to significant impairment in functioning.
Incorporate a strengths-based approach in current interventions, which may produce more sustained effects and allow individuals to live more vital lives in the presence of pain. Interventions that cultivate resilience resources can enhance psychological, cognitive, and social strengths.
Table I.
Resilience Resources and Mechanisms in Pediatric Chronic Pain
| Level | Resilience resources | Resilience mechanisms |
|---|---|---|
| Individual |
|
|
| Family/social environment |
|
|
| Culture |
|
|
aPreviously investigated in pediatric chronic pain samples.
Conclusions
In summary, pediatric pain research has predominantly focused on risk factors and maladjustment; shifting our focus to protective factors and mechanisms of resilience is a novel and promising pursuit. Developing pediatric pain resilience models through the integration of emerging pediatric chronic illness and adult pain models will not only expand resilience research through model testing and revision, but will also inform future clinical practice and interventions. Given the universality of being confronted with challenges or setbacks, the concept of resilience empowers youth to foster their skills and strengths to positively adapt and live successfully with their pain.
Acknowledgments
The first author is a trainee member of Pain in Child Health, a Strategic Training Initiative in Health Research of the Canadian Institutes of Health Research.
Funding
The preparation of this manuscript was supported by grants from the Health Resources and Service Administration (1D40HP19643; 2D40HP19643) awarded to Lindsey L. Cohen and a National Institutes of Health grant (K23 HD067202) awarded to Laura E. Simons.
Conflicts of interest: None declared.
References
- Bronfenbrenner U. (1979). The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press. [Google Scholar]
- Bursch B., Tsao J. C., Meldrum M., Zeltzer L. K. (2006). Preliminary validation of a self-efficacy scale for child functioning despite chronic pain (child and parent versions). Pain, 125, 35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpino E., Segal S., Logan D., Lebel A., Simons L. E. (2014). The interplay of pain-related self-efficacy and fear on functional outcomes among youth with headache. The Journal of Pain, 15, 527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen L. L., MacLaren J. E., Lim C. S. (2008). Pain and pain management. In Steele R. G., Elkin T. D., Roberts M. C. (Eds.), Handbook of evidence based therapies for children and adolescents: Bridging science and practice (pp. 283–296). New York, NY: Springer Publishers. [Google Scholar]
- Cousins L. A., Cohen L. L., Venable C. (2015). Risk and resilience in pediatric chronic pain: Exploring the protective role of optimism. Journal of Pediatric Psychology, 40, 934–942. [DOI] [PubMed] [Google Scholar]
- Forgeron P. A., McGrath P. J., Stevens B., Evans J., Dick B., Finley G. A., Carlson T. (2011). Social information processing in adolescents with chronic pain: My friends don’t really understand me. Pain, 152, 2773–2780. [DOI] [PubMed] [Google Scholar]
- Goodin B. R., Bulls H. W. (2013). Optimism and the experience of pain: Benefits of seeing the glass as half full. Current Pain and Headache Reports, 17, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes S. C., Strosahl K. D., Wilson K. G. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press. [Google Scholar]
- Hilliard M. E., Harris M. A., Weissberg-Benchell J. (2012). Diabetes resilience: A model of risk and protection in type 1 diabetes. Current Diabetes Reports, 12, 739–748. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. (1996). Full catastrophe living: How to cope with stress, pain and illness using mindfulness meditation. London: Piatkus. [Google Scholar]
- Kalapurakkel S., Carpino E. A., Lebel A., Simons L. E. (2015). “Pain can’t stop me”: Examining pain self-efficacy and acceptance as resilience processes among youth with chronic headache. Journal of Pediatric Psychology, 40, 926–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King S., Chambers C. T., Huguet A., MacNevin R. C., McGrath P. J., Parker L., MacDonald A. J. (2011). The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain, 152, 2729–2738. [DOI] [PubMed] [Google Scholar]
- Koinis-Mitchell D., McQuaid E. L., Jandasek B., Kopel S. J., Seifer R., Klein R. B., Potter C., Fritz G. K. (2012). Identifying individual, cultural and asthma-related risk and protective factors associated with resilient asthma outcomes in urban children and families. Journal of Pediatric Psychology, 37, 424–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansing A. H., Berg C. A. (2014). Topical review: Adolescent self-regulation as a foundation for chronic illness self-management. Journal of Pediatric Psychology, 39, 1091–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten A. S. (2001). Ordinary magic: Resilience processes in development. American Psychologist, 56, 227–238. [DOI] [PubMed] [Google Scholar]
- McCracken L. M. (2013). Committed action: An application of the psychological flexibility model to activity patterns in chronic pain. The Journal of Pain, 14, 828–835. [DOI] [PubMed] [Google Scholar]
- McCracken L. M., Morley S. (2014). The psychological flexibility model: A basis for integration and progress in psychological approaches to chronic pain management. The Journal of Pain, 15, 221–234. [DOI] [PubMed] [Google Scholar]
- Palermo T. M., Valrie C. R., Karlson C. W. (2014). Family and parent influences on pediatric chronic pain: A developmental perspective. American Psychologist, 69, 142–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petter M., Chambers C. T., McGrath P. J., Dick B. D. (2013). The role of trait mindfulness in the pain experience of adolescents. The Journal of Pain, 14, 1709–1718. [DOI] [PubMed] [Google Scholar]
- Phipps S., Long A. M., Ogden J. (2007). Benefit finding scale for children: Preliminary findings from a childhood cancer population. Journal of Pediatric Psychology, 32, 1264–1271. [DOI] [PubMed] [Google Scholar]
- Reich J. W., Zautra A. J., Hall J. S. (Eds.) (2010). Handbook of adult resilience. New York, NY: Guilford Press. [Google Scholar]
- Scheier M. F., Carver C. S. (1985). Optimism, coping, and health: Assessment and implications of generalized outcome expectancies. Health Psychology, 4, 219–247. [DOI] [PubMed] [Google Scholar]
- Simons L. E., Logan D. E., Chastain L., Stein M. (2010). The relation of social functioning to school impairment among adolescents with chronic pain. The Clinical Journal of Pain, 26, 16–22. [DOI] [PubMed] [Google Scholar]
- Smith A. M., Sieberg C. B., Odell S., Randall E., Simons L. E. (2015). Living life with my child’s pain: The parent pain acceptance questionnaire (PPAQ). The Clinical Journal of Pain, 31, 633–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturgeon J. A., Zautra A. J. (2013). Psychological resilience, pain catastrophizing, and positive emotions: Perspectives on comprehensive modeling of individual pain adaptation. Current Pain and Headache Reports, 17, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vervoort T., Logan D. E., Goubert L., De Clercq B., Hublet A. (2014). Severity of pediatric pain in relation to school-related functioning and teacher support: An epidemiological study among school-aged children and adolescents. Pain, 155, 1118–1127. [DOI] [PubMed] [Google Scholar]
- Wallace D. P., McCracken L. M., Weiss K. E., Harbeck-Weber C. (2015). The role of parent psychological flexibility in relation to adolescent chronic pain: Further instrument development. The Journal of Pain, 16, 235–246. [DOI] [PubMed] [Google Scholar]
- Weiss K. E., Hahn A., Wallace D. P., Biggs B., Bruce B. K., Harrison T. E. (2013). Acceptance of pain: Associations with depression, catastrophizing, and functional disability among children and adolescents in an interdisciplinary chronic pain rehabilitation program. Journal of Pediatric Psychology, 38, 756–765. [DOI] [PubMed] [Google Scholar]
- Welkom J. S., Hwang W. T., Guite J. W. (2013). Adolescent pain catastrophizing mediates the relationship between protective parental responses to pain and disability over time. Journal of Pediatric Psychology, 38, 541–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wicksell R. K., Olsson G. L., Hayes S. C. (2011). Mediators of change in acceptance and commitment therapy for pediatric chronic pain. Pain, 152, 2792–2801. [DOI] [PubMed] [Google Scholar]
- Zautra A. J., Johnson L. M., Davis M. C. (2005). Positive affect as a source of resilience for women in chronic pain. Journal of Consulting and Clinical Psychology, 73, 212–220. [DOI] [PMC free article] [PubMed] [Google Scholar]