Abstract
Introduction
To anaylse the current evidence regarding the safety, feasibility and advantages of intact specimen extraction via various extraction sites after conventional laparoscopic nephrectomy (LN).
Material and methods
A comprehensive literature search was performed identifying studies evaluating outcomes from Pfannenstiel (PFN) versus extended port site (EPS) extraction sites, after conventional laparoscopic nephrectomy/nephroureterectomy (LRN/LNU) and donor nephrectomy (LDN). Outcome measures included procedure duration, incision length, duration of inpatient stay, analgesic requirements, complications and warm ischemia time (for donor nephrectomy cases).
Results
This systematic review of five comparative studies found no significant difference in morbidity, wound length, wound complications or opioid consumption across all studies. Inpatient stay (p = 0.03) and estimated blood loss (p = 0.03) were significantly less in favour of a PFN extraction site. When comparing radical nephrectomy cases alone, the PFN group had a shorter procedure time (NS), less estimated blood loss (p = 0.04), shorter inpatient stay (p <0.05), significantly less morphine use (p <0.006) and fewer wound complications.
Conclusions
This review demonstrates the viability of retrieving a nephrectomy specimen/graft through a PFN incision in relation to the benefits of cosmesis and reduced pain. As reported in several trials, morbidity is not significantly increased and key outcome measures, such as duration of inpatient stay, pain scores, complications, analgesic requirements and time taken to return to normal activities, remain non-inferior. This study is limited by the small number of generally low quality studies available for analysis. Further well-constructed randomised controlled trials are needed to shed more light on this subject area.
Keywords: laparoscopic nephrectomy extraction, Pfannenstiel nephrectomy, pfannenstiel nephroureterectomy
INTRODUCTION
The first laparoscopic nephrectomy (LN) for malignant disease was performed in 1991. Since then, the approach has gained worldwide acceptance and many consider it to be standard treatment for some T1 and most T2 tumours, with current evidence suggesting a nephron sparing approach to localized cancers [1, 2, 3]. Furthermore, its uses have expanded to include nephrectomy for renal transplants, chronic infections and renal stones. LN results in less post-operative pain, improved cosmesis, a shorter hospital stay and an earlier return to daily activities when compared with open nephrectomy. These benefits are achieved without compromising oncological outcomes [4]. Current options for intact specimen extraction include an expanded port site (EPS), connecting port site incisions, utilising old abdominal scars or by creating new incisions (such as a paramedian, Pfannenstiel (PFN) or modified iliac fossa) [2]. Gill [5] maintained that although their subjective impression was that the degree of comfort and cosmesis from a modified Pfannenstiel incision was better than via an expanded primary port site, a detailed comparison of these two approaches is required. Given that more than a decade after this assertion, there is still a lack of consensus as to which technique is optimal, we aimed to conduct a systematic review to summarize the evidence relating to the safety and feasibility of the above extraction sites.
METHODS
The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines were adhered to in conducting this review [6].
Literature search
A literature search was conducted in January 2015; no restrictions to regions or publication types were placed. The search was limited to the English language to allow data extraction. References from articles and reviews were thoroughly evaluated for inclusion.
The following terms were used:
“laparoscopic nephrectomy extraction”,
“Pfannenstiel nephrectomy”,
“laparoscopic Pfannenstiel nephroureterectomy”,
“expanded port site nephrectomy”,
“laparoscopic nephrectomy”,
“radical nephrectomy extraction”,
“donor nephrectomy extraction.”
Study selection and data collection
Three authors (D.B, M.A, R.H) followed pre-defined inclusion criteria as per a predetermined protocol to select potential articles for inclusion independently. Where differences of opinion emerged between the researchers regarding article eligibility, senior authors acted as arbiters. This involved re-scrutinizing said studies according to our eligibility criteria below.
Eligibility criteria
Comparative studies evaluating outcomes relating to the extraction of the intact specimen after conventional laparoscopic nephrectomy or nephroureterectomy (LNU) were included in this review. Dates of inclusion were set from 2000 – 2015. Papers investigating laparoscopic single site nephrectomy (LESS) were excluded as this would lead to a significant lack of equipoise.
Data were extracted from each paper separately and outcome measures set as: (1) mean procedure time, (2) estimated blood loss, (3) incision length, (4) duration of inpatient stay, (5) convalescence period, (6) pain scoring, (7) analgesia requirements, (8) complications (major and minor), and (9) warm ischaemia, assessed for donor nephrectomy subgroups.
Datasets
Data for each included paper were entered in an Excel spreadsheet and checked by two authors prior to analysis.
Data analysis
The quality of the included studies was assessed using the Cochrane bias assessment tool and statistical analysis performed using Revman software (Cochrane Collaboration). The weighted mean difference (WMD) and relative risk (RR) were used to compare continuous and dichotomous variables, respectively. Statistical heterogeneity was assessed using the chi-square test with significance set at p <0.05, and heterogeneity was quantified using the I2 statistic. The random-effects model was used if significant heterogeneity was identified otherwise a fixed-effects model was used.
RESULTS
Characteristics of eligible studies
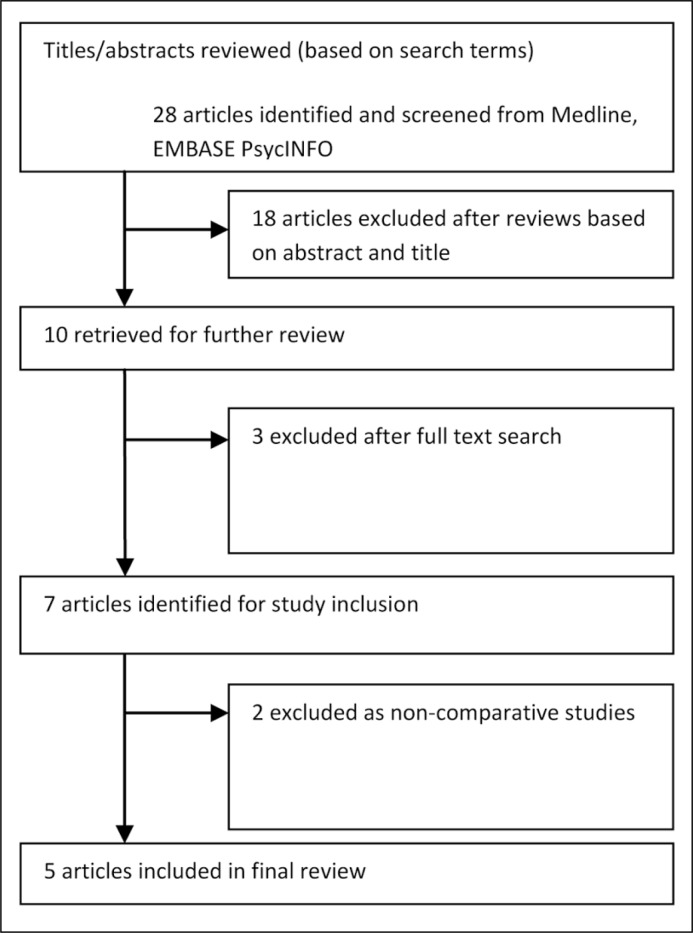
Three retrospective and two prospective (one randomised) studies were included in this review. These studies spanned four countries and included 890 patients. A reference search of these publications yielded no further studies for inclusion. Four comparative studies related to LN and one assessed outcomes from LN/LNU. In this same study, Tisdale et al. [2] also included a subset of donor nephrectomies. Only two studies [2, 7] assessed radical nephrectomy, whilst the remainder investigated donor nephrectomy (Figure 1).
Figure 1.
Study inclusion process.
Methodological quality of included studies
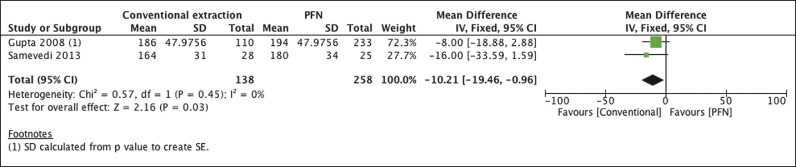
The quality of included studies was generally low with randomisation occurring in only one study [8]. In the retrospective studies, there was no clear protocol for treatment allocation; this tended to be performed at the discretion of the surgeon. The studies did not discuss blinding or allocation concealment. Several of the outcome measures were deemed suitable for meta-analysis as follows (Figure 2).
Figure 2.
Forest plot comparing procedure duration (minutes).
Comparison 1: expanded port site versus a Pfannenstiel incision
Two studies, performing donor nephrecromy (DN) [8, 9], found the procedure to be statistically longer in the PFN group ((two studies, 396 participants): 95% MD -10.21, 95% CI from -19.46 to -0.96, p = 0.03, I2 = 0%). A limitation to this dataset is that Gupta [9] did not provide variance data and as such, the standard error was extrapolated from the provided p-value (0.15) to generate a t-value (SD = t/SE). Tisdale et al., meanwhile, found no difference in procedure duration [2] (Figure 3).
Figure 3.
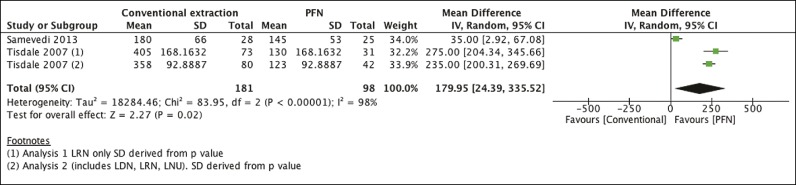
Forest plot comparing estimated blood loss (ml).
Estimated blood loss was less in the two analyses by Tisdale [2] and in the RCT by Adiyat [8], and found to be statistically significant on meta-analysis ((three studies, 279 participants): MD 179.95 ml, 95% CI from 24.39 to 335.52, p = 0.02, I2 = 98%) favouring the PFN group. However, the large difference in the Tisdale study was attributed to 3 outliers, having large bleeds between 2-3L. The authors comment that the difference in estimated blood loss lost significance after repeating the analysis without these outliers [2]. There is significant heterogeneity between the studies and this may be attributable to differences in sample size, as well as standard deviations having to be inferred from the provided p-values by the method described above (Figure 4).
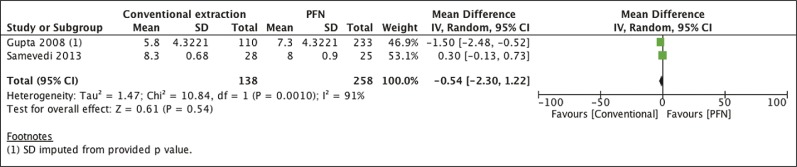
Figure 4.
Forest plot comparing incision length (cm).
Incision length was an outcome measure in two studies comparing extraction sites for donor nephrectomy [8, 9]. On meta-analysis there was no statistically significant difference for PFN versus EPS ((two studies, 396 participants): MD = -0.54, 95% CI from -2.3 to 1.22, p = 0.54). There was significant heterogeniety (I2 = 91%). Once again there is a significant difference in sample sizes between the studies (Figure 5).
Figure 5.
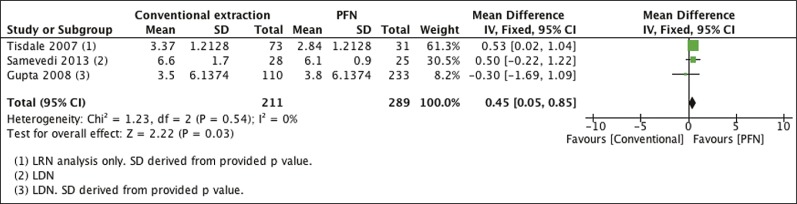
Forest plot comparing duration of inpatient stay (days).
Duration of stay was significantly shorter in the PFN group ((three studies, 500 participants): MD = 0.45, 95% CI from 0.05 to 0.85, p = 0.03, I2 = 0%) [2, 8, 9] (Figure 6).
Figure 6.
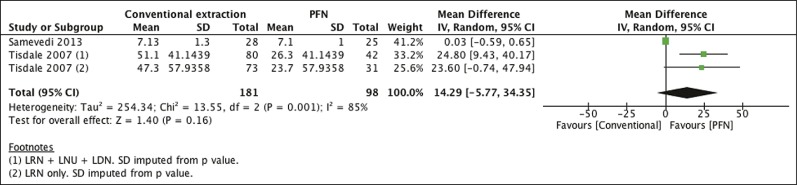
Forest plot comparing IV morphine consumption (mg).
In both analyses by Tisdale [2], the PFN group had a significant reduction in narcotic use when compared with the EPS group; p <0.006 and p <0.002 respectively. The difference is not significant on meta-analysis (two studies, 279 participants): MD 14.29, 95% CI from -5.77 to 34.35, p = 0.16, I2 = 85%). The Adiyat [8] study is limited by very small sample sizes, however, and this may well explain the significant heterogeneity encountered. (Figure 7).
Figure 7.
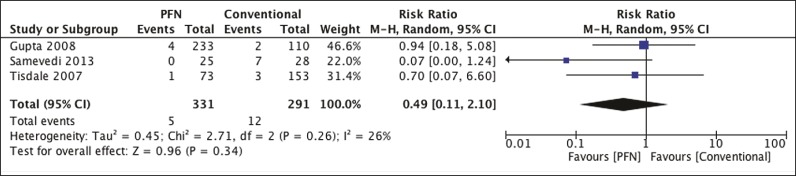
Forest plot comparing wound complications.
There were no significant differences in wound complications between the groups [2, 8, 9] (three studies, 622 participants): RR 0.49, 95% CI from 0.11 to 2.10, p = 0.34). Heterogeneity was not significant (I2 = 26%) (Figure 8).
Figure 8.
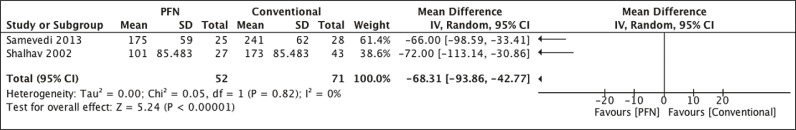
Forest plot comparing warm ischaemia time (mins).
Two studies [8, 10] (123 participants) demonstrated a significant reduction in warm ischaemia time when utilizing a PFN incision (MD – 93.86 95%; CI from -113.14 to -30.66, p <0.00001). There is no significant heterogeneity in this analysis.
Gupta [9] reported comparable warm ischaemia times between the PFN and conventional groups. No variance data or p-values are provided in their paper and, as such, this cannot be included for meta-analysis.
Operative complications
Gupta [9] reported 3 complications when making the expanded port site incision (1 bleed, 2 instances necessitating extension of the wound, where the specimen was too large). When making the PFN incision, the same authors noted 1 episode of small bowel injury and 2 cases of bladder injury. There was also 1 episode of injury to the inferior epigastric artery. Shalhav [10] reported two complications relating to conventional donor graft extraction via an expanded port site, namely a splenic laceration requiring emergency laparotomy, and one in which the specimen fell out of the EndoCatch bag. They reported no complications with regards to manual extraction via a PFN incision.
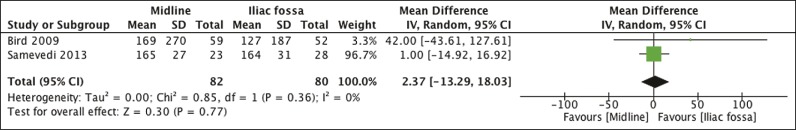
Comparison 2: Midline versus Iliac fossa
Two studies [7, 8] had arms comparing a midline (umbilicus) extraction site versus an iliac fossa site. Several outcomes were suitable for meta-analysis (Figure 9).
Figure 9.
Forest plot comparing estimated blood loss.
There was no significant difference in estimated blood loss between the groups ((two studies, 162 participants): MD 2.37, 95% CI from -13.29 to 18.03, p = 0.77, I2 = 0%) (Figure 10).
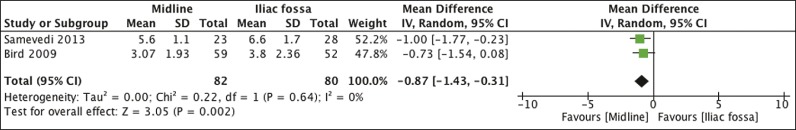
Figure 10.
Forest plot comparing duration of inpatient stay.
Hospitalization was significantly shorter for patients having a midline incision versus an iliac fossa incision ((two studies, 162 participants) MD -0.87, 95% CI from -1.43 to -0.31, p = 0.002, I2 = 0%) (Figure 11).
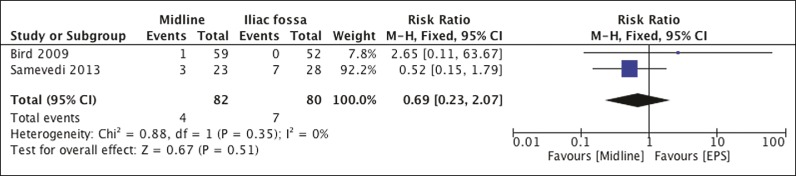
Figure 11.
Forest plot comparing wound complications.
There was no significant difference in wound complications ((two studies, 162 participants): RR 0.69, 95% CI from 0.23 to 2.07, p = 0.51, I2 = 0%).
Bird and colleagues [7] stress that the site of intact specimen extraction in LN cases should be considered carefully. They found a significantly increased risk of incisional hernia formation when using a paramedian extraction site versus an iliac fossa or a midline incision (p = 0.026).
Adiyat [8] found that whilst the length of the incision was significantly shorter in the midline (MD) group compared with either a PFN or an EPS incision (p> 0.001), graft extraction complications were significantly higher in the MD group (p = 0.002). Wound complications were significantly less in the PFN group when compared with either a midline or EPS extraction site (p = 0.02).
DISCUSSION
This systematic review has confirmed that extracting kidney specimens via a PFN incision after laparoscopic nephrectomy is technically feasible and associated with several benefits. These include a shorter inpatient stay, less bleeding and a reduction in warm ischaemia time for donor nephrectomy cases. There was no significant increase in incision length or wound complications. Two authors had arms comparing a midline incision versus an iliac fossa incision. They found that whilst duration of stay favoured the midline extraction site, estimated blood loss and wound complications were comparable. One study [8] determined that whilst the length of the incision was significantly shorter in the midline (MD) group compared with other groups (p >0.001), graft extraction complications were significantly higher (p = 0.002). The same author that found wound complications were significantly less common in the PFN group when compared with the other two groups (p = 0.02). One study established that there was a significantly increased risk of incisional hernia formation when using a paramedian extraction site versus an iliac fossa or a midline incision (p = 0.026) [7].
This systematic review, comparing the safety and peri-operative variables of several approaches of removing specimens after laparoscopic nephrectomy, included 890 patients. Meta-analysis of two papers (radical and donor nephrectomy) [2, 8] demonstrates that estimated blood loss is significantly reduced when using a PFN extraction site (p = 0.02). There is no difference in incision length when using a PFN extraction site (p = 0.98). There was no significant difference in duration of stay (p = 0.32) in the two studies of LDN. However, when introducing an analysis of LN cases into the meta-analysis, this figure became significant, favouring the PFN site (p = 0.03).
In both analyses by Tisdale [2], the PFN group had a significant reduction in narcotic use when compared with the EPS. The difference is not significant on pooled analysis (p = 0.75).
There is no significant difference in wound complications [2, 8], but warm ischaemia time is significantly reduced in cases of donor nephrectomy [2, 8, 10]. Duration of inpatient stay showed no significant difference in the donor nephrectomy subgroup and in the same subgroup, operation duration was actually longer when using a Pfannenstiel incision (p = 0.03). One study [9] offers a potential reason for this; the time taken to make the incision is significantly longer for a PFN incision versus an EPS incision (5 mins versus 2 mins, p = 0.001).
Tisdale et al. [2] carried out a retrospective cohort study comparing parameters after transperitoneal laparoscopic nephrectomy, with intact specimen extraction through Pfannenstiel (PFN) or expanded port site (EPS) incision. In the first analysis, the LR only analysis, PFN group had shorter procedure time, less estimated blood loss, shorter inpatient stay (p <0.05), significantly less morphine use (p <0.006) and fewer wound complications (1 case of cellulitis in the PFN group and 3 incisional herniae in the EPS group). In the second analysis, which included LN, LNU and LDN, the PFN group had shorter procedure time, less estimated blood loss, shorter inpatient stay and significantly less morphine use (p <0.002).
Adiyat et al. [8] compared the outcomes of three different methods of graft extraction after a conventional five port LDN; (a) iliac fossa (IF) incision, (b) midline (MD) periumbilical with lower polar fat stitch incorporating the gonadal vein for traction during retrieval, (c) PFN with gel port extraction. There were no significant differences among all three groups in terms of age, sex, estimated blood loss, body mass index, vascular anatomy, operating time, post-operative pain score, analgesic consumption, delayed graft function, hospital stay and recipient creatinine, after six weeks. Warm ischemia time was significantly reduced in the PFN group compared with the IF group (p >0.001). Incision length was shorter in the MD group compared with other groups (p >0.001). Significantly fewer wound complications occurred in the PFN group than in the other two groups. Graft extraction complications were significantly higher in the MD group compared with the other two groups (p = 0.002). The authors concluded that the PFN incision was their preferred extraction method
In contrast, Gupta et al. [9] compared the IF (an expanded port site) and PFN incisions for kidney retrieval in laparoscopic transperitoneal donor nephrectomy in 343 patients. The EPS group had a shorter procedure time, significantly shorter incision length (p <0.003), shorter inpatient stay, shorter convalescence period, quicker return to regular diet, less tramadol use, less intra-operative and post-operative complications and shorter warm ischemia time (all NS). They also report more incisions being made for PFN versus an IF approach: 5 vs. 4 (NS) and that the time taken for incisions was longer: 5 minutes versus 2 minutes (p = 0.001). The authors concluded that IF incision had less morbidities but poorer cosmesis.
Shalhav et al. [10} compared the use of an EndoCatch bag device for graft retrieval via an EPS against a manual retrieval technique through a Pfannenstiel incision in 70 laparoscopic live donor nephrectomies. There was a statistically significant difference in warm ischemia time favouring the manual extraction technique via the PFN incision (p <0.001) and this technique also had fewer complications.
Kishore et al. [11] assessed the safety and feasibility of laparoscopic donor nephrectomy with transvaginal extraction and impact of body mass index (BMI), menopausal status, previous surgery and uterine fibroids in 30 patients, and they recommend this procedure for a premenopausal donor with a BMI <30. Several other animal and human studies have demonstrated the technical feasibility of performing nephrectomy through a natural orifice transluminal endoscopic surgery (NOTES) approach [12–15, 16]. Indeed one series from Spain demonstrated successful surgery in 14 women. However, with a mean inpatient stay of 4 days and one patient having a colon injury (7%) [16] requiring a colostomy, more comparative studies will be needed to assess the long term viability of such an approach.
This study distills the comparative work in this area. It demonstrates that morbidity is not compromised and key outcome measures such as estimated blood loss and duration of inpatient stay are significantly reduced using the PFN approach. Post-operative pain (using narcotic consumption as a surrogate) is significantly reduced when extracting a specimen via a PFN incision in LN cases. This may be attributable to the muscle-splitting nature of the incision as compared with a muscle-cutting incision [2]. The paper highlights that there is no difference in incision length or wound complications between extraction sites [2, 8]. The significant reduction in warm ischaemia time in two studies [2, 10] is relevant to this debate with regards to the role this incision plays in DN caes. Extended PFN incisions are not entirely benign [2]. Gupta [9] reported 1 episode of small bowel injury and 2 cases of bladder injuries when making PFN incisions, and surgeons should be mindful of such risks if performing this incision. Another limitation is an increase in procedure duration for donor nephrectomy cases. As well as improved cosmesis [2, 9], the above outcomes must undoubtedly stimulate further debate as to optimal extraction site.
This review is limited by the small number of generally low quality, single centre and heterogeneous studies to analyse, thus limiting the generalizability of our outcomes. It is suboptimal to make comparisons between donor nephrectomy and radical nephrectomy cases. Nevertheless, the parallels in operative technique and the paucity of high quality studies make such comparisons necessary at this moment. We have compensated by performing a descriptive review where meta-anaylsis is not possible and delineating, as far as possible, between donor nephrectomy and radical nephrectomy cases throughout this brief review. Further randomised, multi-centre trials will contribute objective evidence to this debate and a pilot study is under way at our own institution as a prequel to a larger multi-centre randomised trial.
CONCLUSIONS
The benefits of extracting a nephrectomy specimen via a Pfannenstiel incision are a shorter inpatient stay, fewer wound complications, less bleeding and a reduction in warm ischaemia time for donor nephrectomy cases. One study found that graft extraction complications were significantly higher when extracting via a midline incision versus an iliac fossa or paramedian incision. Incisional hernia formation is significantly higher when utilising a paramedian extraction site versus an iliac fossa or a midline incision. From an operative point of view, the ideal extraction site is that with which the surgeon is comfortable. However, this review has demonstrated some obvious advantages of this approach, which future research should aim to corroborate.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Clayman RV, Kavoussi LR, Figenshau RS, Chandhoke PS, Albala DM. Laparoscopic nephroureterectomy: initial clinical case report. J Laparoendosc Surg. 1991;1:343–349. doi: 10.1089/lps.1991.1.343. [DOI] [PubMed] [Google Scholar]
- 2.Tisdale BE, Kapoor A, Hussain A, Piercey K, Whelan JP. Intact specimen extraction in laparoscopic nephrectomy procedures: Pfannenstiel versus expanded port site incisions. Urology. 2007;69:241–244. doi: 10.1016/j.urology.2006.09.061. [DOI] [PubMed] [Google Scholar]
- 3.Steinway ML, Lengu IJ, Cherullo EE, Ponsky LE. Laparoendoscopic single-site (LESS) nephrectomy through a Pfannenstiel incision: porcine model. J Endourol. 2009;23:1293–1296. doi: 10.1089/end.2009.0091. [DOI] [PubMed] [Google Scholar]
- 4.Branco AW, Kondo W, Stunitz LC, Valente J, Branco Filho AJ. Laparoendoscopic Pfannenstiel nephrectomy using conventional laparoscopic instruments--preliminary experience. Int Braz J Urol. 2010;36:718–723. doi: 10.1590/s1677-55382010000600010. [DOI] [PubMed] [Google Scholar]
- 5.Matin SF, Gill IS. Modified Pfannenstiel incision for intact specimen extraction after retroperitoneoscopic renal surgery. Urology. 2003;61:830–832. doi: 10.1016/s0090-4295(02)02579-7. [DOI] [PubMed] [Google Scholar]
- 6.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bird VG, Au JK, Sandman Y, De Los Santos R, Ayyathurai R, Shields JM. Comparison of different extraction sites used during laparoscopic radical nephrectomy. J Urol. 2009;181:1565–1570. doi: 10.1016/j.juro.2008.11.113. [DOI] [PubMed] [Google Scholar]
- 8.Adiyat KT, Tharun BK, Shetty A, Samavedi S. Comparison of three different techniques of extraction in laparoscopic donor nephrectomy. Indian J Urol. 2013;29:184–187. doi: 10.4103/0970-1591.117279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta M, et al. A comparison of kidney retrieval incisions in laparoscopic transperitoneal donor nephrectomy. Urol Int. 2008;81:296–300. doi: 10.1159/000151407. [DOI] [PubMed] [Google Scholar]
- 10.Shalhav AL, Siqueira TM, Gardner TA, Paterson RF, Stevens LH. Manual specimen retrieval without a pneumoperitoneum preserving device for laparoscopic live donor nephrectomy. J Urol. 2002;168:941–944. doi: 10.1016/S0022-5347(05)64547-8. [DOI] [PubMed] [Google Scholar]
- 11.Kishore TA, Shetty A, Balan T, et al. Laparoscopic donor nephrectomy with transvaginal extraction: initial experience of 30 cases. J Endourol. 2013;27:1361–1365. doi: 10.1089/end.2013.0412. [DOI] [PubMed] [Google Scholar]
- 12.Raman JD, Bergs RA, Fernandez R, et al. Complete transvaginal NOTES nephrectomy using magnetically anchored instrumentation. J Endourol. 2009;23:367–371. doi: 10.1089/end.2008.0220. [DOI] [PubMed] [Google Scholar]
- 13.Isariyawongse JP, McGee MF, Rosen MJ, Cherullo EE, Ponsky LE. Pure natural orifice transluminal endoscopic surgery (NOTES) nephrectomy using standard laparoscopic instruments in the porcine model. J Endourol. 2008;22:1087–1091. doi: 10.1089/end.2007.0404. [DOI] [PubMed] [Google Scholar]
- 14.Haber G-P, et al. Pure “natural orifice transluminal endoscopic surgery” for transvaginal nephrectomy in the porcine model. BJU Int. 2009;104:1260–1264. doi: 10.1111/j.1464-410X.2009.08561.x. [DOI] [PubMed] [Google Scholar]
- 15.Sánchez-Margallo FM, Pérez FJ, Sánchez MA, Bachiller J, Juárez A, et al. Transvaginal NOTES-assisted laparoscopic nephrectomy: a survival study in a sheep model. Surg Endosc. 2012;26:926–932. doi: 10.1007/s00464-011-1969-6. [DOI] [PubMed] [Google Scholar]
- 16.Alcaraz A, Peri L, Molina A, et al. Feasibility of transvaginal NOTES-assisted laparoscopic nephrectomy. Eur Urol. 2010;57:233–237. doi: 10.1016/j.eururo.2009.09.025. [DOI] [PubMed] [Google Scholar]