Abstract
Most clinicians would agree that there is no reason to obtain a magnetic resonance (MR) scan to evaluate a patient with viral conjunctivitis. We scheduled a patient for an annual MR scan to monitor his optic nerve meningiomas. By coincidence, he had florid viral conjunctivitis the day the scan was performed. It showed severe eyelid edema, contrast enhancement of the anterior orbit, enlargement of the lacrimal gland, and obstruction of the nasolacrimal duct. Adenovirus produces deep orbital inflammation, in addition to infection of the conjunctival surface.
Keywords: conjunctivitis, dacryoadenitis, dacryocystitis, epiphora, viral culture, serotype 8
Report of a Case
A 36-year-old man with suspected bilateral optic nerve sheath meningiomas was scheduled for a routine MR scan. The goal was to determine whether comparison with an MR scan obtained a year before would reveal growth of the tumors. When the scan was ordered, he had no eye infection. Two weeks later, when the scan was performed, viral conjunctivitis had developed. The scan was not postponed because the patient did not complain of his new symptoms. After the study was finished, the neuro-radiologist called to report a new inflammatory process in the right orbit. The patient was examined immediately in the eye clinic, revealing classic signs of viral conjunctivitis (Figure 1A). There was ocular injection, chemosis, and swelling of the right eyelids. Slit lamp examination showed follicular conjunctivitis and diffuse epithelial keratitis. Fluid-attenuated inversion recovery (FLAIR) sequences showed diffuse edema of the anterior orbit, which was extensive, extending even into the premalar region (Figure 1B). A conjunctival swab was placed in viral transport medium, which was used to inoculate an A549 cultured cell line1. The specimen from the patient induced cytopathic changes; a direct fluorescent antibody against adenovirus antigen confirmed the diagnosis of adenoviral keratoconjunctivitis (Figure 1C). Sequence analysis of the viral isolate showed that the infection was caused by adenovirus type D, serotype 82.
Figure 1.
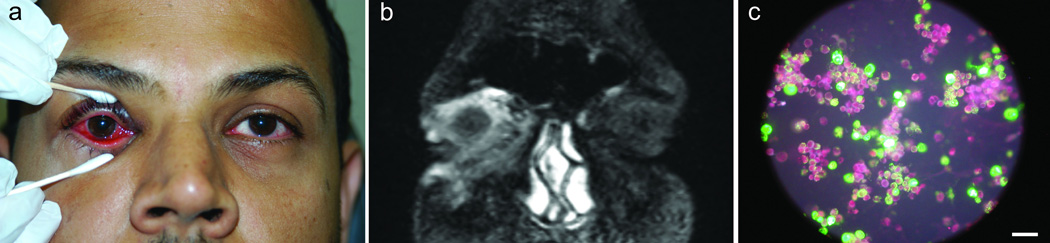
A) Conjunctivitis, right eye. B) Coronal image showing inflammation of the conjunctiva, eyelids, anterior orbit, and pre-malar area. C) Direct fluorescent antibody label (green) against adenovirus antigen, showing punctate cytoplasmic and nuclear staining in A549 cells (red). Scale = 100 microns.
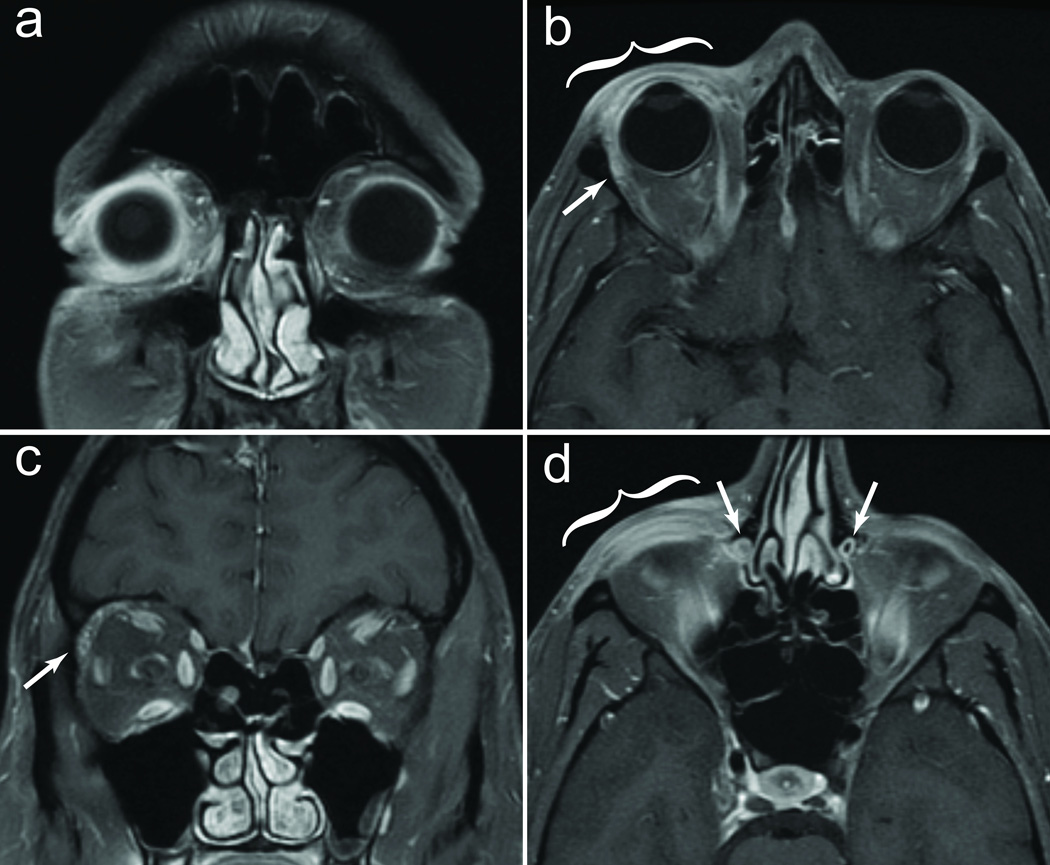
A coronal T1 MR scan showed marked gadolinium enhancement of the conjunctiva and soft tissues surrounding the right globe (Figure 2A). In the axial plane, edema was evident in all layers of the eyelid (Figure 2B). The lacrimal gland was enlarged on the right side. This asymmetry was confirmed by coronal imaging (Figure 2C). The extraocular eye muscles were normal. The meningiomas were visible as rings of gadolinium enhancement around the optic nerves. The right nasolacrimal duct demonstrated thickening of the mucosa and loss of the air signal within the lumen, which was present on the normal left side (Figure 2D).
Figure 2.
A) Fat saturation image, demonstrating enhancement of periocular tissues. B) Thickening of right upper eyelid (bracket) and anterior orbital enhancement. Lacrimal gland is enlarged (arrow). C) Coronal image confirming right lacrimal gland enlargement (arrow). D) Inflammation of lower eyelid (bracket), and right nasolacrimal duct swelling with loss of air signal in the lumen (arrows).
Discussion
Adenoviral conjunctivitis is the most common cause of acute eye infection3. Millions of cases occur every year, but MR findings have been reported previously in only a single patient, who developed massive bilateral eyelid cysts4. Unintentionally, we imaged a patient with a typical case, caused by a viral strain associated with epidemic keratoconjunctivitis5. The main findings were edema and inflammation of periocular tissue in the anterior orbit, enlargement of the lacrimal gland, and nasolacrimal duct compromise. The latter findings suggest that adenovirus conjunctivitis is accompanied by dacryoadenitis, and dacryocystitis. Infection of these structures contributes to epiphora, a common symptom in viral conjunctivitis. It is not surprising that viral infection should spread to the lacrimal adnexa, because they are in anatomical contiguity with the conjunctiva. By analogy, MR imaging in rhinovirus infection often shows mucosal thickening and fluid in the paranasal sinuses6.
Although adenovirus infection targets the conjunctival surface, these MR images reveal that the infection induces an inflammatory process that extends surprisingly deep into the orbit. Our case presented as a typical infection, and the patient recovered uneventfully, indicating that deep tissue inflammation, dacryoadenitis, and dacryocystitis are likely to be common manifestations of adenoviral conjunctivitis.
Acknowledgments
This work was supported by grants EY10217 (J.C.H.), EY02162 (Beckman Vision Center) from the National Eye Institute and a Physician-Scientist Award from Research to Prevent Blindness (J.C.H.). Technical support was provided by Alicia B. Parker. Both authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Financial Disclosure/Conflict of Interest: NONE. Dr. Horton examined the patient and wrote the manuscript; Dr. Miller performed the viral culture and serotyping, and edited the manuscript.
References
- 1.Leland DS, Ginocchio CC. Role of cell culture for virus detection in the age of technology. Clin. Microbiol. Rev. 2007 Jan;20(1):49–78. doi: 10.1128/CMR.00002-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shimada Y, Ariga T, Tagawa Y, Aoki K, Ohno S, Ishiko H. Molecular diagnosis of human adenoviruses d and e by a phylogeny-based classification method using a partial hexon sequence. J. Clin. Microbiol. 2004 Apr;42(4):1577–1584. doi: 10.1128/JCM.42.4.1577-1584.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sambursky RP, Fram N, Cohen EJ. The prevalence of adenoviral conjunctivitis at the Wills Eye Hospital Emergency Room. Optometry. 2007 May;78(5):236–239. doi: 10.1016/j.optm.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 4.Detorakis ET. Epidemic adenoviral keratoconjunctivitis complicated by massive bilateral lower eyelid cysts. Ophthal. Plast. Reconstr. Surg. 2014 Jan-Feb;30(1):82. doi: 10.1097/IOP.0000000000000004. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Adenovirus-associated epidemic keratoconjunctivitis outbreak - four states, 2008–2010. MMWR CDC Surveill. Summ. 2013;62:637–641. [PMC free article] [PubMed] [Google Scholar]
- 6.Turner BW, Cail WS, Hendley JO, et al. Physiologic abnormalities in the paranasal sinuses during experimental rhinovirus colds. J. Allergy Clin. Immunol. 1992 Sep;90(3 Pt 2):474–478. doi: 10.1016/0091-6749(92)90172-x. [DOI] [PubMed] [Google Scholar]