Abstract
We sought to understand how HIV-infected patients, their providers, and HIV care researchers prioritize self-reported domains of clinical care. Participants rank-ordered two lists of domains. A modified Delphi process was used for providers and researchers. Approximately 25% of patients were interviewed to discuss rationale for rank order choices. List 1 included anger, anxiety, depression, fatigue, physical function, pain, and sleep disturbance. List 2 included alcohol abuse, cognitive function, HIV stigma, HIV and treatment symptoms, medication adherence, positive affect, sexual risk behavior, sexual function, social roles, spirituality/meaning of life, and substance abuse. Seventy-four providers, 80 HIV care researchers and 66 patients participated. Patients ranked context-based domains, such as HIV stigma, more highly than providers, while health behaviors, such as drug or alcohol use, ranked lower. Patients described a need to address wider-context challenges such as HIV stigma in order to positively impact health behaviors. Divergent patient and provider priorities highlights the importance of incorporating views from all stakeholders and suggests the need for a care approach that more effectively addresses contextual barriers to adverse health behaviors.
Keywords: HIV care, patient-reported outcomes, patient-based measures, patient-provider communication, HIV-infected patients
INTRODUCTION
Modern quality improvements in health care, inspired in part by the Chronic Care Model (Bodenheimer, Wagner, & Grumbach, 2002; Wagner, 1998; Wagner et al., 2001; Wagner, Austin, & Von Korff, 1996) strive toward “patient-centeredness” and a meaningful integration of the patient’s voice into care. Key to ensuring this is the systematic, routine collection and consideration of patient-reported symptoms, conditions, and health behaviors, known collectively as patient-reported outcomes (PROs) (U.S. Department of Health and Human Services, 2006). PROs are reports generated directly from patients describing function or feelings in relation to one or more health conditions and their treatments (U.S. Department of Health and Human Services, 2006). PROs have been shown to improve identification of conditions and health behaviors (Fredericksen et al., 2011), management of chronic conditions (Dobscha, Gerrity, & Ward, 2001; Marshall, Haywood, & Fitzpatrick, 2006) and patient-provider communication (Brown, Butow, Dunn, & Tattersall, 2001; Detmar, Muller, Schornagel, Wever, & Aaronson, 2002; Velikova et al., 2004).
Meaningful and enduring PRO integration into care requires selection of PRO domains that are clinically relevant to providers, reflect patient priorities, or both. In the NIH funded Patient Reported Outcomes Measurement Information System (PROMIS) initiative, researchers identified key mental, physical, and social health domains for research settings (PROMIS, 2011). The extent to which self-reported domains including those identified by PROMIS investigators are salient for providers caring for people living with HIV (PLWH), or for PLWH themselves, is not known.
We therefore sought to evaluate existing PROMIS domains and selected potential additional domains by determining their importance for PLWH, HIV care providers, and HIV care researchers.
METHODS
Study Participants and Data Collection
PLWH (n=66), HIV care providers (n=110), and HIV care researchers (n=80) were recruited from the Centers for AIDS Research Network of Integrated Clinical Systems (CNICS) cohort. CNICS is a U.S. consortium of eight clinical practice research sites providing care for a demographically heterogeneous cohort of ~30,000 HIV-infected patients. There was considerable overlap between providers and researchers; 70% of providers were researchers, and 98% of researchers were providers. Patients were recruited from 4 CNICS sites collecting PROs: the 1917 Clinic (University of Alabama-Birmingham), Owen Clinic (University of California-San Diego), Fenway Community Health in Boston, MA, and the Madison Clinic (University of Washington/Harborview Medical Center, Seattle, WA).
We used a modified Delphi method (Hasson, Keeney, & McKenna, 2000; Holey, Feeley, Dixon, & Whittaker, 2007) to collect data from HIV care providers and researchers, and a paper-based survey for patients, in addition to individual interviews for ~25% of these patients. Participants ranked two separate lists of PRO domains in order of importance. The first was a list of seven PROMIS PRO domains (“List 1”): anger, anxiety, depression, fatigue, physical function, pain, and sleep disturbance. These domains were developed in the first phase of the PROMIS project (PROMIS, 2011). The second list, “List 2”, consisted of domains considered relevant to HIV clinical care and research, and was developed by providers and researchers in CNICS with expertise in HIV clinical care in partnership with researchers from PROMIS with expertise in PRO implementation and development. These eleven domains were: alcohol abuse, cognitive function, HIV stigma, HIV and treatment symptoms, medication adherence, positive affect, sexual risk behavior, sexual function, social roles, spirituality/meaning of life, and substance abuse.
Ethical Considerations
Institutional review board approval was granted for patient participation by Fenway Community Health, University of California-San Diego, and University of Alabama-Birmingham, and University of Washington. Approval for CNICS-wide provider participation was obtained at the University of Washington.
Provider and Researcher Delphi
We conducted two modified-Delphi rounds with providers to assess importance rankings within each list. For the first round, providers and researchers attending the national in-person CNICS meeting on November 6–7, 2009 were asked to rank in order of importance domains they considered most important for improving clinical care. Responses were anonymous and the exercise took 3–5 minutes. Following this meeting, investigators from the CNICS network were invited to forward an online version of the survey to HIV providers and researchers at their respective medical centers.
The survey for round 2 was administered exclusively online after providers viewed aggregate rank order results from the previous round. Procedures were pilot tested with a Seattle provider group.
Patient Surveys and Interviews
A convenience sample of patients at each PRO collection site placed domains in each list in rank order of importance. One-fourth of respondents were interviewed to explore the rationale for their rankings. Participants were paid $10 for completion of the survey and $25 for the interview. These activities occurred between February and October 2012. Approximately one-fifth of eligible patients agreed to participate.
Data Analysis
Surveys were tallied and domains were ranked in order of importance. Two trained qualitative researchers coded interview transcripts for domain-specific content and direct statements describing rationale for rank orders. Themes regarding rationales were identified using an open coding process by two qualitative researchers, and assessed for inter-rater agreement. The method of Hollander and Sethuraman was used to test whether a difference in rankings between two groups (e.g. patients and providers) was statistically significant (Hollander and Sethuraman, 1978). We compared the following patient subpopulations: women (n=17) vs. men (n=49); African-American (n=20) vs. White patients (n=33); people ≥ age 50 (n=25) vs. <50 (n=41), people diagnosed with HIV ≤5 years (n=21) vs. longer (n=45), and men who have sex with men (MSM) including MSM who are intravenous drug users (IVDU) (n=41) vs. other risk factors (n=25). We did not compare rankings based on Hispanic ethnicity due to small numbers.
RESULTS
Study Participants
There were 110 providers and researchers who completed surveys in round 1, of whom 74 participated in the round 2 online survey. Of the providers, 82% were also researchers; six individuals were researchers but not providers. Sixty-six patients participated in the survey; 15 of them were interviewed (see Table I). Their clinical characteristics were similar to the overall sample.
Table I.
Provider and patient characteristics
| Providers (n=74) | Patients (n=66) | |||
|---|---|---|---|---|
| Demographic | n | % | n | % |
| Male | 31 | 42% | 49 | 74% |
| Age | ||||
| <30 | 2 | 3% | 6 | 9% |
| 30–39 | 30 | 41% | 9 | 14% |
| 40–49 | 21 | 28% | 26 | 39% |
| ≥50 | 21 | 28% | 25 | 38% |
| Race | ||||
| African-American | 20 | 30% | ||
| White | 33 | 50% | ||
| Hawaiian/Pacific Islander | 1 | 2% | ||
| Native American | 3 | 5% | ||
| Other/More than One Race | 9 | 14% | ||
| Latino Ethnicity | 10 | 15% | ||
| Professional Role | ||||
| Attending physician | 53 | 72% | ||
| Fellow | 10 | 14% | ||
| Nurse/PA | 5 | 7% | ||
| Other | 6 | 8% | ||
| Percent time treating patients | ||||
| 0% | 2 | 13% | ||
| 1–25% | 30 | 41% | ||
| 26–50% | 20 | 27% | ||
| 51–75% | 7 | 10% | ||
| 75–100% | 15 | 20% | ||
| Years treatment experience | ||||
| < 5 years | 20 | 27% | ||
| 5–9 years | 18 | 24% | ||
| 10–14 years | 14 | 19% | ||
| ≥15 years | 22 | 30% | ||
| Years living with HIV | ||||
| 0–5 years | 21 | 32% | ||
| 6–10 years | 17 | 26% | ||
| >10 years | 28 | 42% | ||
| Route of transmission | ||||
| MSM* | 37 | 56% | ||
| MSM & IDU | 4 | 6% | ||
| IV Drugs | 5 | 8% | ||
| Heterosexual | 17 | 26% | ||
| Unknown | 3 | 4% | ||
| Most recent CD4 | ||||
| 0–199 | 7 | 11% | ||
| 200–349 | 6 | 9% | ||
| ≥350 | 53 | 80% | ||
MSM= men who have sex with men
IDU= IV drug users
Responses
Agreement Between Providers
The round 2 rank ordering results are presented here. Rank ordering did not differ between providers and researchers (List 1 p=0.74 List 2 p=0.12). Concordance between providers was high for both lists, with depression ranked as most important of the List 1 domains, followed by physical function, pain, and anxiety (Figure I), and medication adherence as most important, followed by HIV and treatment symptoms, and substance abuse in List 2 (Figure II).
Figure I. Provider vs. patient rankings, List 1.
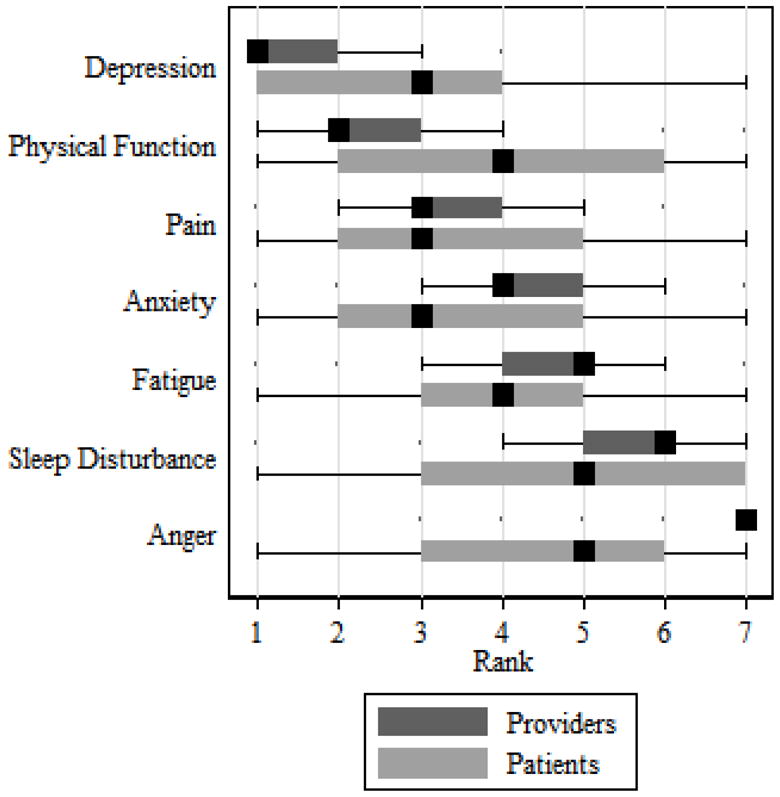
The median rank is in black, and the box spans the 25th to 75th percentiles. The whiskers define 11/2 times the inter-quartile range; individual observations more extreme than this are indicated with dots.
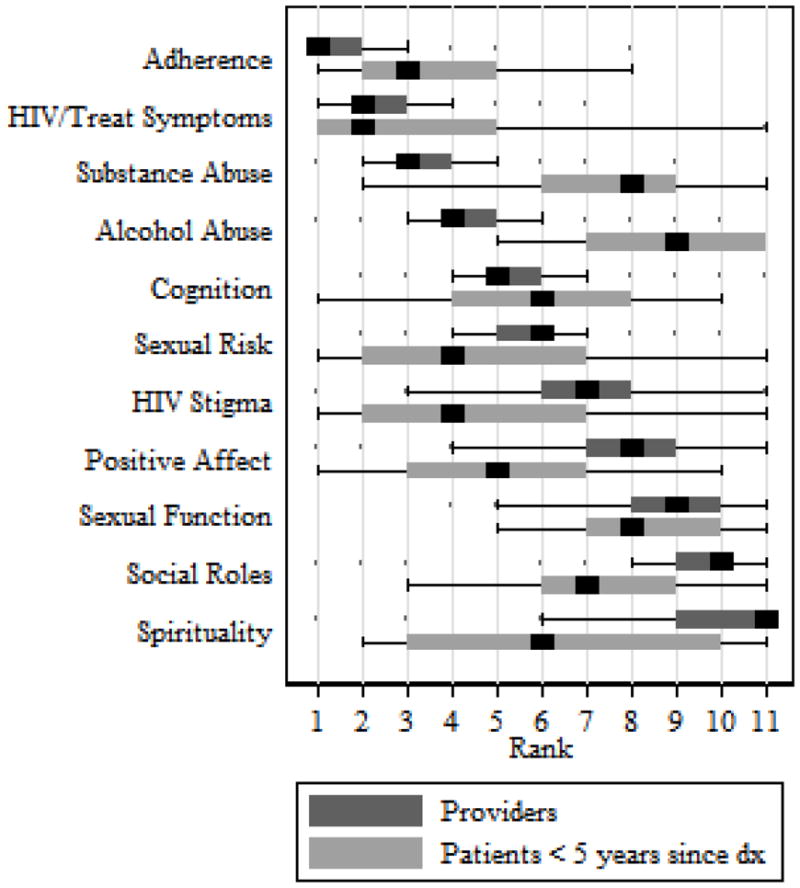
Figure II.
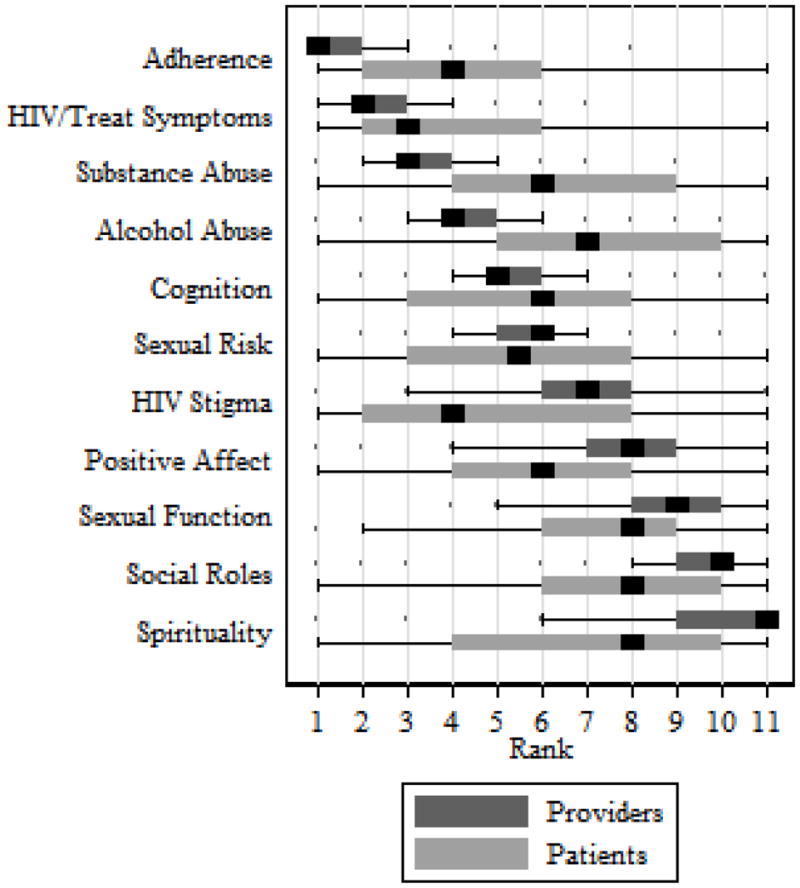
Provider vs. patient rankings, List 2
Agreement Between Patients
Of List 1 domains, patients selected depression, pain, and anxiety as most important to address in clinical care (Figure I). Of List 2 domains, patients selected HIV and treatment symptoms as most important to address in clinical care, followed by medication adherence and HIV stigma. Spirituality/meaning of life, sexual functioning, and social roles were ranked least important (Figure II).
There were statistically significant differences between the ranks in List 1 between males and females (p=0.03) and between African-Americans and Whites (p=0.03) (Figures III and IV). Females ranked pain, anxiety, and anger higher; men, by contrast, ranked physical functioning and fatigue higher. Anxiety and anger were more highly ranked among African-American than White patients, while physical functioning ranked lower.
Figure III.
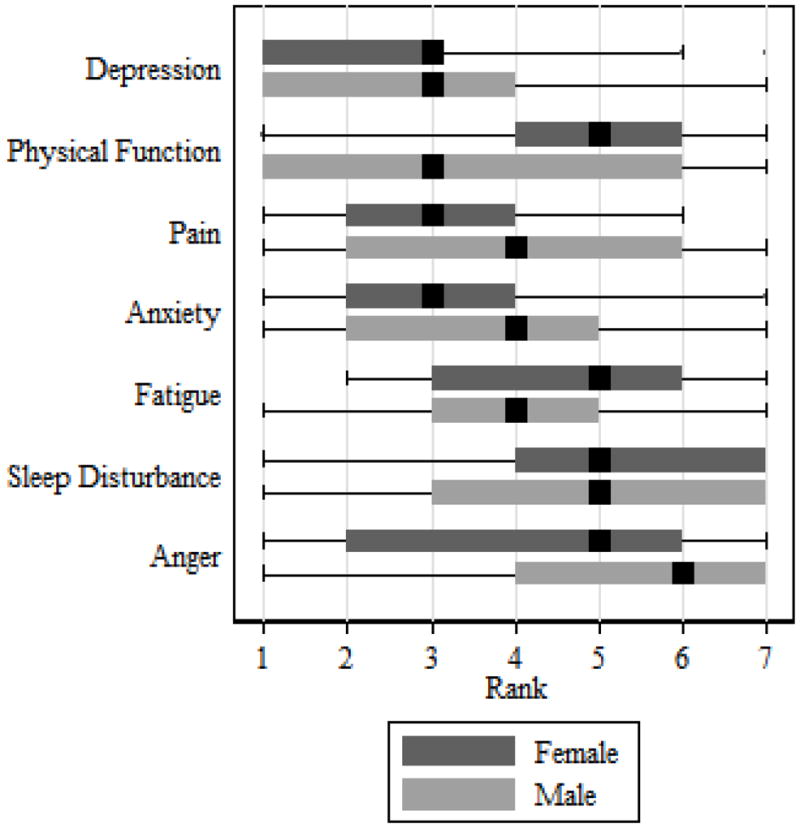
Male vs. female patients, List 1
Figure IV.
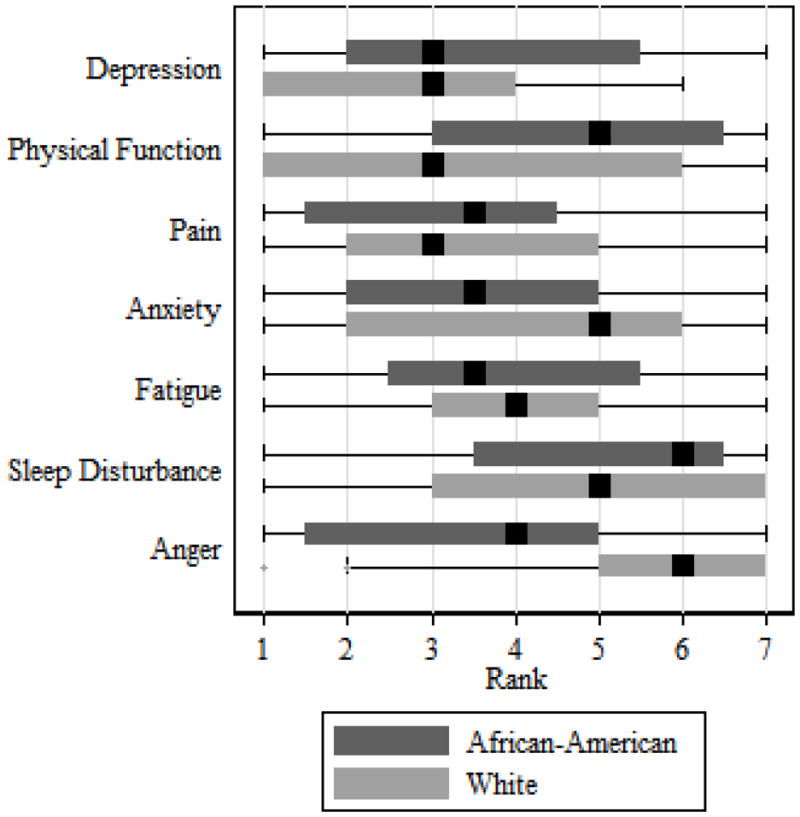
African American vs. White patients, List 1
Agreement Between Providers and Patients
There were statistically significant differences between patients and providers (p<0.001 for both lists). The largest differences were in anger, ranked higher for patients, and physical functioning, ranked lower. (Figure I). Patients ranked HIV stigma much more highly than providers (Figure II). Positive affect, spirituality, and social roles were also ranked more highly by patients. Patients ranked behaviors including medication adherence, substance abuse, and alcohol abuse lower than providers. The difference between patients and providers in List 2 was particularly striking among patients living with HIV ≤5 years (p<0.001). In Figure V, we compare provider ranks from Figure II to recently diagnosed patients, where differences in substance abuse, alcohol abuse, positive affect, spirituality, and social roles were even greater.
Figure V.
Patients <5 years since HIV diagnosis vs. providers, List 2
Qualitative Results: Key Themes
The greatest areas of patient-provider discordance in clinical care priorities were HIV stigma, which patients ranked higher, and alcohol and substance abuse, which providers and researchers ranked higher. Patients typically described the mental health and social impact of stigma as a root problem affecting other domains, specifically, by affecting mood states and health behaviors:
“It’s important that stigma be brought up and talked about [with your provider], because see, that causes my depression…your feelings are hurt, you feel sad, you feel down, you feel like people think they’re better than you.” (Female, 35, Birmingham)
In general, patients believed it necessary to address domains affecting mental health first, in order to have impact on behavior-based domains, particularly alcohol and substance abuse:
“I’d want my doctor to help me deal with the isolation problem before the drinking problem. The isolation could lead to the drinking.” (Female, 26, Seattle)
“…if you are feeling sad because you [have HIV], I think that leads to using more alcohol or drugs and you don’t care about taking your medication….” (Male, 42, San Diego)
Others described the importance of one’s life needing to have meaning in order to affect health behaviors:
“[If] you don’t have the meaning of life, you go to depression…and then you probably won’t take your medication…you probably will start abusing alcohol or [become an] addict…it affects everything.” (Male, 44, Seattle)
Most patients acknowledged that direct assistance with psychosocial issues such as stigma were likely outside their provider’s area of expertise, preferring referrals to mental health or social support services, as one patient stated, “a way to connect with others that have been through it [being diagnosed with HIV]”. Yet most patients felt that their psychosocial challenges, and stigma in particular, were important for providers to at least acknowledge in order to fully understand their impact on other areas of health and overall quality of life.
These examples highlight the patients’ appreciation of and desire for a provider to acknowledge the contexts of their lives in which symptoms and behaviors emerge; a desire to be experienced as more than a sum of presenting problems or behaviors. As one patient stated, “[My provider] is not just treating HIV. [He] is treating my whole life.” (Male, 47, Boston)
DISCUSSION
We found broad agreement between patients and providers in the relative importance for clinical care of the domains of depression, pain, and anxiety. We also found broad agreement between patients and providers in the relative importance of HIV and treatment symptoms. However, patients placed greater importance on assessments of HIV-related stigma; providers, on assessments of alcohol and substance abuse. Domains ranked highly by providers are characterized by the potential to address problems in the context of a clinic visit, and domains with greater direct impact on mortality and serious long-term morbidity. Domains with relatively clear steps toward resolution (e.g., medication adherence, HIV/treatment symptoms) were prioritized more highly by providers than domains with less clinically addressable action plans (e.g., positive affect, spirituality), consistent with prior research among providers treating patients with multiple chronic conditions (Bounthavong & Law, 2008; Law, Ray, Knapp, & Balesh, 2003). Furthermore, providers ranked at-risk behaviors such as substance abuse higher than patients.
Patients placed slightly higher priority on domains of pain and HIV treatment and symptoms than did providers, suggesting that patients may assign higher priority to domains associated with symptomatic conditions or urgent discomfort, echoing prior research among diabetic patients (Zulman, Kerr, Hofer, Heisler, & Zikmund-Fisher, 2010). Patients ranked behavior-based domains somewhat lower than providers, particularly alcohol and substance abuse. Interview data suggested that patients viewed alcohol and substance abuse as difficult to address without also addressing broader psychosocial problems, such as HIV stigma or social isolation.
The interplay of psychosocial context, mental health, and health behaviors described by patients echoes findings from prior studies which have suggested that a high frequency of stressors predicts adverse health behaviors, including sexual risk behavior and poor medication adherence among PLWH (Mugavero et al., 2009; Pence et al., 2010). This lends support for justification of a comprehensive primary care model able to contextualize and address these stressors to effectively impact symptoms and behaviors. Notably, sexual risk behavior was the sole behavior-based domain ranked higher by patients than providers. Some patients, particularly MSM, described an increase in sexual risk behavior as a reaction to psychosocial problems. Prior studies have revealed under-detection of sexual risk behaviors by physicians in both primary care (Morin et al., 2004) and HIV care settings (Marks et al., 2002). Given this context, the higher prioritization of sexual risk behavior by patients as a topic of discussion suggests missed opportunities for HIV transmission prevention education, particularly with HIV-infected men, and that patients in general may be more receptive to such discussion than providers may assume. The most salient theme across all patients interviewed was the negative impact of HIV-related stigma on mental health, social functioning, and overall quality of life, consistent with prior research among those living with HIV in the US (Logie and Gadalla, 2009; Vanable, Carey, Blair, & Littlewood, 2006; Wolitski, Pals, Kidder, Courtenay-Quirk, & Holtgrave, 2009). Patients felt that stigma led to feelings of worthlessness and other depressive symptoms, as well as substance abuse and sexual risk behaviors, consistent with previous findings (Rao et al., 2011). Among the patients interviewed, the issue of disclosure was central to the problem of managing stigma, creating anxiety regardless of whether patients chose to disclose or not. Anticipation of disclosure conjured fears of rejection, including fear of isolation from existing support and/or future partners. Preparation for disclosure was described as stressful and nuanced, involving ongoing decisions regarding who to tell, when, where, and how. Patients who had disclosed their HIV infection described a continuous challenge of anticipating and managing the reactions and misperceptions of others, as well as the impact of those reactions on their own mental health. Yet, choosing not to disclose may also erode mental health, as prior research on self-concealment suggests (Friedlander, Nazem, Fiske, Nadorff, & Smith, 2012). Stress resulting from HIV stigma has been found to permeate other areas of health including medication adherence (Rao et al., 2011; Vanable et al., 2006; Wolitski et al., 2009), increased HIV-related symptoms (Vanable et al., 2006), physical functioning (Larios, Davis, Gallo, Heinrich, & Talavera, 2009), psychological functioning (Larios et al., 2009), mental health including depression (Halkitis, Parsons, Wolitski, & Remien, 2003; Logie, 2009; Rao et al., 2011), substance abuse (Wolitski et al., 2009), and overall physical health (Logie, 2009; Wolitski et al., 2009).
Most concerning is that new HIV infections occur disproportionately among populations that have been historically marginalized by other forms of stigma, such as racism and homophobia. This double- or triple-marginalization may further magnify the burden of HIV-related stigma, with implications for health outcomes (Rao, Pryor, Gaddist, & Mayer, 2008). Some patients noted that the provider is the sole person who knows about their HIV, highlighting the extra importance of the provider in connecting patients to appropriate avenues of support. Many patients suggested that their HIV providers open their treatment approach to include inquiries into their social and family adjustment, so that they might feel more comfortable discussing issues of stigma and feel better supported by their providers.
These discussions prompt two questions: 1) whether and how HIV care providers can realistically and appropriately assist patients in areas such as coping with HIV stigma as a means of helping address their other issues, and 2) are such issues even appropriate to address in clinical HIV care? Given what we found regarding the importance of these domains for patients, and their suggested impact on health behaviors, it may be worthwhile to pursue discussion of these domains with patients as part of the ongoing patient-provider relationship that is at the core of chronic disease management. Even if providers are unable to solve all issues related to these domains, patients valued provider willingness to appreciate these issues in the overall context of their lives. Patients’ comments suggest a desire to be regarded as more than a composite of symptoms and behaviors and a need to be respected as “whole” people living complex lives with interconnected parts. While patients may not necessarily wish to engage in a lengthy discussion of stigma during a clinic visit, there may be other ways for providers to at least meaningfully acknowledge the gravity of the issue and act as an advocate for referral to appropriate resources.
Strengths
A key strength of this study is that it incorporates views from both patients and providers. In addition to soliciting patient priorities, it supplemented this with interviews to ensure an understanding of rationales for patient choices. Finally, this study incorporated patient views from 4 US cities to ensure a diverse representation of views.
Study Limitations
Some factors limit the generalizability of this study. Our patient sample was predominantly male and middle-aged, consistent with the U.S. HIV-infected population. In addition, the process of gathering data differed between providers and patients. There is a chance that procedural differences may have influenced results. Provider race/ethnicity was not collected; this was a missed opportunity to further dimensionalize patient-provider differences in rankings.
CONCLUSION
The high ranking of stigma as a clinical priority among patients living with HIV and lower ranking of health behaviors such as substance and alcohol use relative to providers highlight a potential disparity in priorities. For the provider, understanding differences between clinical and patient priorities may help contextualize barriers toward adopting positive health behaviors, or toward avoiding adverse ones, and improve overall communication. For the patient, it is important that HIV care providers acknowledge the wider context of their lives, and offer referral resources to help address and improve their relationships with self, spirituality, society, and social roles, as well as their overall outlook and sense of meaning. Such resources may allow patients to experience a sense of control over their destiny, and to experience themselves as agents of hope in their own lives. For this to manifest, the concept of “care” would do well to expand to address these domains, encompassing more of patients’ lived realities as people who are managing a lifelong relationship with a stigmatizing and difficult chronic disease. Finally, this study highlights the discrepancies in patient and provider views underscoring the importance of incorporating input from diverse stakeholders.
Supplementary Material
Acknowledgments
Funding: We thank the patients and providers of the CNICS network. This work was supported by grants from the NIH NIMH RO1 Grant (RO1 MH084759), NIH PROMIS Roadmap (U01 AR057954), and NIAAA ARCH-ERA U24 AA020801 and U01AA020793
Footnotes
Authors claim no significant conflicting financial interests.
Contributor Information
Rob Fredericksen, Email: rfrederi@uw.edu, Senior Research Scientist, University of Washington, Center for AIDS Research, 325 9th Avenue, Seattle, WA 98104, Phone: (206) 595-1415, Fax: (206) 744-3693.
Todd Edwards, Email: toddce@uw.edu, Research Assistant Professor, University of Washington, Seattle Quality of Life Group, 4333 Brooklyn Ave NE, Seattle, WA 98195, 206-303-3683.
Heidi M. Crane, Email: hcrane@uw.edu, Associate Professor, University of Washington, Department of Medicine, Box 359931, Seattle, WA 98104, 206-744-6649.
Paul K. Crane, Email: pcrane@uw.edu, Associate Professor, University of Washington, Internal Medicine, 908 Jefferson St., Seattle, WA 98104, 206-744-1831.
Jessica Merlin, Email: jmerlin@uab.edu, Associate Professor, University of Alabama at Birmingham, School of Medicine, Division of Infectious Diseases, 1900 University Boulevard, THT 229, Birmingham, AL 35294, 206-934-5191.
Laura E. Gibbons, Email: gibbonsl@uw.edu, Research Scientist, University of Washington, Department of General Internal Medicine, Box 359781, Seattle, WA 98104, 206-744-1842.
Deepa Rao, Email: deeparao@uw.edu, Associate Professor University of Washington Department of Global Health 325 9th Avenue Seattle, WA 98104 206-685-3064.
D. Scott Batey, Email: dsbatey@uab.edu, Research Scientist, Research and Informatics Service Center, Department of Medicine, Division of Infectious Diseases, University of Alabama at Birmingham, 845 19th St. South, Birmingham, AL 32594, (205) 996-7984.
Lydia Dant, Email: ldant@fenwayhealth.org, Project Manager, The Fenway Institute, Ansin Building, 8th Floor, 1340 Boylston St., Boston, MA 02215.
Edgar Páez, Email: epaez@ucsd.edu, Research Assistant and Coordinator, UCSD Medical Center – OWEN Clinic, 200 W. Arbor Drive # 8681, San Diego, CA 92103-8681, 619-543-3440.
Anna Church, Email: Annac23@uw.edu, Research Coordinator, University of Washington, Center for AIDS Research, 325 9th Avenue, Seattle, WA 98104, Phone: (206) 744-5124.
Donald L. Patrick, Email: donald@uw.edu, Director/Professor, Seattle Quality of Life Group, 4333 Brooklyn Ave NE, Seattle, WA 98195, 206-685-7252.
References
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. Jama. 2002;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- Bounthavong M, Law AV. Identifying health-related quality of life (HRQL) domains for multiple chronic conditions (diabetes, hypertension and dyslipidemia): patient and provider perspectives. Journal Of Evaluation In Clinical Practice. 2008;14(6):1002–1011. doi: 10.1111/j.1365-2753.2007.00933.x. [DOI] [PubMed] [Google Scholar]
- Brown RF, Butow PN, Dunn SM, Tattersall MH. Promoting patient participation and shortening cancer consultations: a randomised trial. Br J Cancer. 2001;85(9):1273–1279. doi: 10.1054/bjoc.2001.2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Detmar SB, Muller MJ, Schornagel JH, Wever LD, Aaronson NK. Health-related quality-of-life assessments and patient-physician communication: a randomized controlled trial. Jama. 2002;288(23):3027–3034. doi: 10.1001/jama.288.23.3027. [DOI] [PubMed] [Google Scholar]
- Dobscha SK, Gerrity MS, Ward MF. Effectiveness of an intervention to improve primary care provider recognition of depression. Eff Clin Pract. 2001;4(4):163–171. [PubMed] [Google Scholar]
- Fredericksen R, Crane PK, Feldman BJ, Tufano J, Harrington RD, Dhanireddy S, Davis T, Brown T, Kitahata MM, Crane HM. Impact of same-day pre-visit electronic patient-reported outcome (PRO) collection on provider assessment of sexual risk and other behaviors of HIV-infected patients in routine clinical care. Paper presented at the American Public Health Association 139th Annual Meeting; Washington, D.C. 2011. [Google Scholar]
- Friedlander A, Nazem S, Fiske A, Nadorff MR, Smith MD. Self-concealment and suicidal behaviors. Suicide & Life-Threatening Behavior. 2012;42(3):332–340. doi: 10.1111/j.1943-278X.2012.00094.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Parsons JT, Wolitski RJ, Remien RH. Characteristics of HIV antiretroviral treatments, access and adherence in an ethnically diverse sample of men who have sex with men. AIDS Care. 2003;15(1):89–102. doi: 10.1080/095401221000039798. [DOI] [PubMed] [Google Scholar]
- Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. Journal Of Advanced Nursing. 2000;32(4):1008–1015. [PubMed] [Google Scholar]
- Holey EA, Feeley JL, Dixon J, Whittaker VJ. An exploration of the use of simple statistics to measure consensus and stability in Delphi studies. BMC Medical Research Methodology. 2007;7:52–52. doi: 10.1186/1471-2288-7-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander M, Sethuraman J. Testing for agreement between two groups of judges. Biometrika. 1978;65(2):403–411. [Google Scholar]
- Larios SE, Davis JN, Gallo LC, Heinrich J, Talavera G. Concerns about stigma, social support and quality of life in low-income HIV-positive Hispanics. Ethnicity & Disease. 2009;19(1):65–70. [PubMed] [Google Scholar]
- Law AV, Ray MD, Knapp KK, Balesh JK. Unmet needs in the medication use process: perceptions of physicians, pharmacists, and patients. Journal Of The American Pharmacists Association: Japha. 2003;43(3):394–402. doi: 10.1331/154434503321831111. [DOI] [PubMed] [Google Scholar]
- Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care. 2009;21(6):742–753. doi: 10.1080/09540120802511877. [DOI] [PubMed] [Google Scholar]
- Marks G, Richardson JL, Crepaz N, Stoyanoff S, Milam J, Kemper C, Larsen R, Bolan R, Weismuller P, Hollander H, McCutchan A. Are HIV care providers talking with patients about safer sex and disclosure?: A multi-clinic assessment. AIDS (London, England) 2002;16(14):1953–1957. doi: 10.1097/00002030-200209270-00013. [DOI] [PubMed] [Google Scholar]
- Marshall S, Haywood K, Fitzpatrick R. Impact of patient-reported outcome measures on routine practice: a structured review. J Eval Clin Pract. 2006;12(5):559–568. doi: 10.1111/j.1365-2753.2006.00650.x. [DOI] [PubMed] [Google Scholar]
- Morin SF, Koester KA, Steward WT, Maiorana A, McLaughlin M, Myers JJ, Vernon K, Chesney MA. Missed opportunities: prevention with HIV-infected patients in clinical care settings. Journal Of Acquired Immune Deficiency Syndromes (1999) 2004;36(4):960–966. doi: 10.1097/00126334-200408010-00010. [DOI] [PubMed] [Google Scholar]
- Mugavero MJ, Raper JL, Reif S, Whetten K, Leserman J, Thielman NM, Pence BW. Overload: impact of incident stressful events on antiretroviral medication adherence and virologic failure in a longitudinal, multisite human immunodeficiency virus cohort study. Psychosomatic Medicine. 2009;71(9):920–926. doi: 10.1097/PSY.0b013e3181bfe8d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pence BW, Raper JL, Reif S, Thielman NM, Leserman J, Mugavero MJ. Incident stressful and traumatic life events and human immunodeficiency virus sexual transmission risk behaviors in a longitudinal, multisite cohort study. Psychosomatic Medicine. 2010;72(7):720–726. doi: 10.1097/PSY.0b013e3181e9eef3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PROMIS. Dynamic tools to measure health outcomes from the patient perspective. 2011 Retrieved August 26, 2011, from http://www.nihpromis.org.
- Rao D, Feldman BJ, Fredericksen RJ, Crane PK, Simoni JM, Kitahata MM, Crane HM. A Structural Equation Model of HIV-Related Stigma, Depressive Symptoms, and Medication Adherence. AIDS Behav. 2011 doi: 10.1007/s10461-011-9915-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao D, Pryor JB, Gaddist BW, Mayer R. Stigma, secrecy, and discrimination: ethnic/racial differences in the concerns of people living with HIV/AIDS. AIDS Behav. 2008;12(2):265–271. doi: 10.1007/s10461-007-9268-x. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health, Human Services FDA. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes. 2006;4:79. doi: 10.1186/1477-7525-4-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanable PA, Carey MP, Blair DC, Littlewood RA. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS And Behavior. 2006;10(5):473–482. doi: 10.1007/s10461-006-9099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velikova G, Booth L, Smith AB, Brown PM, Lynch P, Brown JM, Selby PJ. Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol. 2004;22(4):714–724. doi: 10.1200/JCO.2004.06.078. [DOI] [PubMed] [Google Scholar]
- Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4. [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511–544. [PubMed] [Google Scholar]
- Wolitski RJ, Pals SL, Kidder DP, Courtenay-Quirk C, Holtgrave DR. The effects of HIV stigma on health, disclosure of HIV status, and risk behavior of homeless and unstably housed persons living with HIV. AIDS And Behavior. 2009;13(6):1222–1232. doi: 10.1007/s10461-008-9455-4. [DOI] [PubMed] [Google Scholar]
- Zulman DM, Kerr EA, Hofer TP, Heisler M, Zikmund-Fisher BJ. Patient-provider concordance in the prioritization of health conditions among hypertensive diabetes patients. Journal Of General Internal Medicine. 2010;25(5):408–414. doi: 10.1007/s11606-009-1232-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


