Abstract
Background
African Americans have the highest burden of colorectal cancer (CRC) in the United States yet lower CRC screening rates than whites. Although poor screening has prompted efforts to increase screening uptake, there is a persistent need to develop public health interventions in partnership with the African American community.
Purpose
To conduct focus groups with African Americans to determine preferences for the content and mode of dissemination of culturally-tailored CRC screening interventions.
Methods
In June 2013, 45-75 year-old African Americans were recruited through online advertisements and from an urban VA system to create four focus groups. A semi-structured interview script employing open-ended elicitation was used, and transcripts were analyzed using ATLAS.ti software to code and group data into a concept network.
Results
A total of 38 participants (mean age=54) were enrolled, and 59 ATLAS.ti codes were generated. Commonly reported barriers to screening included perceived invasiveness of colonoscopy, fear of pain, and financial concerns. Facilitators included poor diet/health and desire to prevent CRC. Common sources of health information included media and medical providers. CRC screening information was commonly obtained from medical personnel or media. Participants suggested dissemination of CRC screening education through commercials, billboards, influential African American public figures, Internet, and radio. Participants suggested future interventions include culturally specific information, including details about increased risk, accessing care, and dispelling of myths.
Conclusions
Public health interventions to improve CRC screening among African Americans should employ media outlets, emphasize increased risk among African Americans, and address ethnic-specific barriers. Specific recommendations are presented for developing future interventions.
Keywords: African American, colorectal cancer, screening, disparities, qualitative
Introduction
Colorectal cancer (CRC) is the third most common cause of cancer-related mortality and the second costliest cancer in the United States (US).[1, 2] Compared to other racial and ethnic groups in the US, African Americans have the highest incidence of CRC, higest prevalence of polyps at time of screening colonoscopy, and highest prevalence of advanced stage CRC at disease presentation.[3-6] In short, African Americans are disproportionately affected by CRC; this poses a major research challenge and an opportunity to improve population health on a large scale.
CRC is a potentially preventable disease. Screening for CRC with colonoscopy, flexible sigmoidoscopy, or fecal occult blood testing reduces cancer mortality and is cost-effective.[7-10] Despite the benefits of screening and the high burden of CRC among African Americans, research from our group and others reveals that screening uptake in African Americans is 6% to 18% lower than in White Americans. This disparity is especially concerning given the disproportionate burden of disease.[11, 12]
There have been many efforts to increase screening among African Americans. Population-based interventions include health-marketing campaigns, patient educational sessions, print media campaigns, telephone counseling, and use of computer-based or patient-navigator education programs.[13] These approaches have demonstrated modest improvements in screening uptake in small cohorts of African Americans.[13] However, on a population level, while the incidence of CRC decreased by 3% per year for Whites between 2000 and 2009, the incidence decreased by only 2% per year in African Americans –a 50% difference.[14] This indicates that despite best efforts to date, we have not closed the gap in CRC burden between African Americans and other groups.
Culturally tailored education has emerged as a viable strategy to enhance CRC screening uptake among African Americans. For example, a culturally tailored ninety-minute educational session in African American churches and community-based organizations resulted in increased knowledge about CRC and increased uptake of screening within six months compared to those not exposed to the intervention.[13] In addition, a recent randomized trial that compared a tailored computer-based CRC screening intervention vs. a non-tailored informational brochure found increased screening uptake in the group receiving the tailored intervention.[15]
Despite previous efforts, there have been few attempts to learn directly from African Americans regarding the preferred mode of dissemination of tailored interventions. Previous interventions were rarely developed in partnership with members of the African American community. The objective of this study was to inform the development of patient-oriented interventions to improve uptake of CRC screening among African Americans by conducting focus groups and exploring the knowledge, attitudes, beliefs, needs, and preferences of African Americans regarding CRC risk and screening. As an extension to previous focus groups on this topic,[16-18] the goal was to generate recommendations for future interventions to address CRC screening disparities among African Americans.
Methods
Study Overview
In order to inform development of patient-oriented interventions to improve uptake of CRC screening among African Americans, focus groups were conducted to explore the knowledge, attitudes, beliefs, needs, and preferences of African Americans regarding CRC risk and screening. The study involved five phases: (1) development of a conceptual framework and interview guide; (2) subject recruitment and administration of a pre-focus group survey; (3) semi-structured focus groups; (4) administration of a post-focus group survey; (5) data analysis and interpretation. The methods are described for each study phase in the sections below.
Phase 1: Interview Script Development
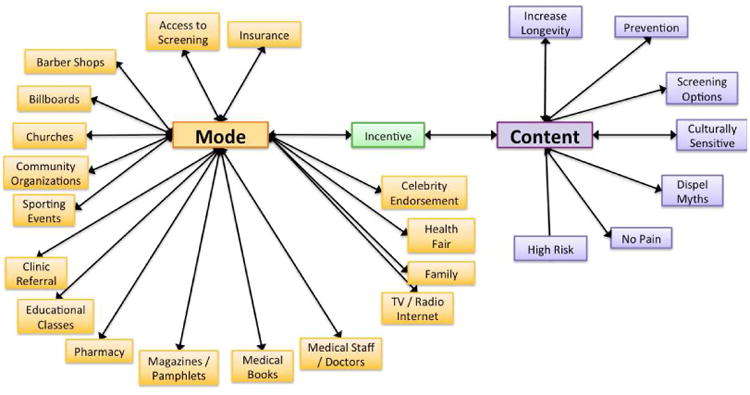
Prior to the focus groups, a semi-structured interview script employing open-ended elicitation and scripted probes was created (Table 1). The script was informed by a previous literature review of published studies identifying barriers and facilitators to CRC screening, and was further guided by a conceptual model for CRC screening utilization among African Americans developed by our research group (Figure 1).[12, 17, 19, 20]
Table 1. Selected items from the semi-structured focus group interview script.
| Sources of general health information | Please tell us where you get most of your information about health. |
| Sources of CRC screening information | Where have you heard information about colon cancer? |
| CRC risk perception | Some people know almost nothing about colon cancer risk in African Americans, and others know a lot. What do you know about the risk of colon cancer in African Americans? |
| CRC risk perception | At the start of this focus group, I asked you to complete a survey. Let's take a look at the responses. Most of the people in this group believe they are at [low/medium/high] risk for colorectal cancer. Why do you think that is? |
| Barriers to CRC screening | I'd like to talk about what encourages and discourages people like you from getting screened. First, what discouraged you from getting screened? |
| Facilitators to Screening | Many people find it difficult to get screened, yet all of you were able to do so. What helped you get screened? |
| Desired mode of CRC interventions | Statistically, African Americans over 45 years old are at the highest risk for colon cancer. Colonoscopy screening is one of the best ways to identify early signs of cancer before it's serious. Knowing this information now, what would be the best way to share this with other people like you? |
| Desired content for CRC interventions | We want more African Americans to get screened for colon cancer, and we need your help to make that happen. What information would you need to know to make a decision about getting screened? |
Figure 1. Conceptual model for the uptake of colorectal cancer screening in African Americans.

Phase 2: Recruitment and Pre-Focus Group Survey
During May and June of 2013, a diverse population of African Americans was recruited. Participants were recruited from the Greater Los Angeles community through online Craigslist advertisements. In addition, participants were recruited through flyers distributed within the Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS), a large and demographically diverse urban healthcare network. Individuals were eligible for inclusion if they were an African American male or female between the ages of 45 and 75. The aim was to recruit a balanced sample of male and female individuals who had successfully completed CRC screening and who had never been screened for CRC.
A survey was administered at the beginning of each focus group to collect demographic information and to assess knowledge about CRC and CRC screening, perceptions of CRC risk among participants, and perceived barriers to screening. Participants were asked to write three reasons why African Americans might defer colonoscopy. Participants also ranked self-perceived risk of developing CRC during their lifetime using an 11-point numeric rating scale, where zero indicated no perceived risk at all and ten indicated the highest possible risk. The student's t-test was used to compare the mean self-perceived risk rankings between screened and unscreened participants.
Phase 3: Focus Groups
Participants were stratified into four focus groups by sex and CRC cancer screening status: (1) African American males who had been screened; (2) African American males who had not been screened; (3) African American females who had been screened; and (4) African American females who had not been screened. Patients were stratified by sex and screening status because sociocultural perceptions about CRC screening, colonoscopy, and health care education vary by these characteristics.[21, 22]
The lead author (F.M.) moderated each focus group with assistance from two co-facilitators (C.W. and K.V.) in July, 2013. The moderator encouraged participants to share individual experiences of barriers and facilitators to CRC screening as well as sources of health and screening information. In addition, participants were asked to recommend interventions they believed would improve uptake of CRC screening in the African American community, commenting specifically on the desired informational content and mode for CRC educational interventions. Intervention mode was defined as the physical form in which an intervention might be delivered, including but not limited to educational reading material, online modules, and patient-directed videos. Intervention content refers specifically to the minimal educational content ideally included in an intervention.
Interviews were audiotaped for transcription and coded by Keystrokes Medical Transcription Service (Yorkville, IL). In addition, one co-facilitator transcribed meeting notes during each session. Participants received $50 as reimbursement for their time and participation and were informed that they could discontinue participation at any time.
Phase 4: Post-focus Group Survey
At the conclusion of each focus group session, the moderator provided participants with a 15-minute information session on the benefits of CRC screening and the seven CRC screening options suggested by the American Cancer Society.[23] Following this overview and a question-and-answer period, participants completed a post-focus group survey to indicate: (1) the number of screening options they would prefer to learn about during a discussion with their physician; and (2) rank-order preference among six different modes of CRC information dissemination.
Phase 5: Data Analysis and Interpretation
Descriptive statistics were used to summarize subject demographic characteristics, including age, sex, marital status, employment status, educational attainment, and income level. Two reviewers (K.V and C.W) individually analyzed the transcribed interviews using ATLAS.ti software (ATLAS.ti Scientific Software Development, Berlin, Germany), a qualitative analysis program that allows researchers to code subject language into major and minor themes. For this study, the evaluation process included the generation of key words, phrases, and quotes related to six pre-determined major domains based on previous literature review: barriers to screening colonoscopy, facilitators to screening colonoscopy, sources of general health information, sources of CRC screening information, and preferred modes and content for CRC educational interventions. Domains were considered credible if raised spontaneously by more than one participant in the same focus group or by at least two participants in separate focus groups. Each reviewer coded patient language into minor domain categories before using ATLAS.ti to generate a network of concepts to depict relationships between minor and major domains, whereby minor domain codes could be associated with more than one major domain. This study was approved by the institutional review board of the WLAVA (IRB Spiegel #0024), and free and informed consent was obtained from all participating individuals.
Results
Participants
A total of 38 African Americans were enrolled into four focus groups: screened African American males (n=7), unscreened African American males (n=6), screened African American females (n=12), and unscreened African American females (n=13). Focus groups ranged from 6 to 13 participants and lasted approximately 120 minutes each. Table 2 provides participant demographic and clinical characteristics. In all, 76 individuals responded to study advertisements, and 38 met the inclusion criteria and our pre-determined focus group strata specifications. In the final sample, 28 participants were recruited via Craigslist, nine were respondents to VAGLAHS flyers, and one was referred by a friend or relative. The mean age was 54, and 66% (n=25) of participants were female. Half (n=19) of the participants reported a history of screening colonoscopy.
Table 2. Focus group participant demographics.
| All Passing Screening (N=76) | Focus Group Participant (N=38) | |
|---|---|---|
|
| ||
| Sex | ||
| Male | 30 (39%) | 13 (34%) |
| Female | 46 (61%) | 25 (66%) |
|
| ||
| Age | ||
| 45-55 years old | 51 (66%) | 25 (66%) |
| 56-65 years old | 23 (30%) | 12 (32%) |
| 66-75 years old | 2 (3%) | 1 (2%) |
|
| ||
| Where did patient hear about study?* | ||
| Craigslist posting | 61 (80%) | 28 (74%) |
| Flyer on the West LA VA Campus | 12 (16%) | 9 (24%) |
| Friend or Relative | 2 (3%) | 1 (3%) |
| Other | 1 (1%) | -- |
|
| ||
| Reason for Responding* | ||
| Learn more about colon cancer | 42 (55%) | 21 (55%) |
| Learn more about colon cancer screening | 34 (45%) | 19 (50%) |
| Learn more about colonoscopy screening | 19 (25%) | 10 (26%) |
| A friend or relative told me to call | 1 (1%) | -- |
| Other | 8 (11%) | -- |
|
| ||
| Had Previous Colonoscopy | ||
| Yes | 31 (41%) | 19 (50%) |
| No | 45 (59%) | 19 (50%) |
|
| ||
| Relationship Status | ||
| Never Married | 26 (34%) | 14 (37%) |
| Separated | 4 (5%) | -- |
| Divorced | 15 (20%) | 6 (16%) |
| Living with Partner in Committed Relationship | 6 (8%) | 4 (11%) |
| Married | 24 (32%) | 13(34%) |
| Widowed | 1 (1%) | 1 (3%) |
|
| ||
| Highest Education | ||
| Some High School | 5 (7%) | 2 (5%) |
| High School | 5 (7%) | 2 (5%) |
| Some college (1-4 years, no degree) | 29 (38%) | 16 (42%) |
| Associate's degree (including occupational or academic degrees) | 6 (8%) | 3 (8%) |
| Bachelor's degree (BA, BS, AB, etc) | 23 (30%) | 12 (32%) |
| Master's degree (MA, MS, MSW, etc) | 8 (11%) | 3 (8%) |
|
| ||
| Occupational Status* | ||
| Homemaker | 3 (4%) | 2 (5%) |
| On leave of absence | 1 (1%) | 1 (3%) |
| Unemployed | 12 (16%) | 3 (8%) |
| Full-time employed | 27 (36%) | 13 (34%) |
| Part-time employed | 9 (12%) | 5 (13%) |
| On disability | 18 (24%) | 11 (29%) |
| Full-time student | 7 (9%) | 4 (11%) |
| Retired | 1 (1%) | -- |
|
| ||
| Total Household Income (from all sources) | ||
| Less than $20,000 | 19 (25%) | 7 (18%) |
| Between $20,001 and $40,000 | 15 (20%) | 8 (21%) |
| Between $40,001 and $60,000 | 16 (21%) | 8 (21%) |
| Between $60,001 and $80,000 | 9 (12%) | 6 (16%) |
| $80,001 or greater | 17 (22%) | 9 (24%) |
Pre-Focus Group Survey Results
The most commonly reported reason for avoiding colonoscopic CRC screening was fear (n=24). This included fear of the procedure itself, fear of pain associated with the procedure, and fear of receiving negative results. Other common barriers included: inability to pay, lack of insurance, embarrassment associated with the procedure's invasive nature, low perceived personal risk of CRC, and lack of education about screening and CRC. On the 11-point numeric rating scale, the mean perceived risk of developing CRC over a lifetime was 4.4. The average perceived risk was low among unscreened participants (4.8, SD=2.61) and among unscreened participants (4.1, SD=2.43); however, there was not a significant difference between these two groups (p=0.34).
ATLAS.ti Coding Results
Code Counts and Domains
ATLAS.ti coding yielded 59 unique codes, 50 of which were endorsed by at least two participants. In some cases, unique minor domains were found to be associated with more than one major domain (Figure 2). For example, three codes were considered both barriers and facilitators to screening: an individual's genetic/family health history, perceived risk of developing CRC, and exposure to pictures or videos of a colonoscopy.
Figure 2. Concept network depicting the full list of the modes and content suggested during the focus groups.
Barriers to Screening
The barriers to screening reported during focus group sessions included invasiveness of the colonoscopy procedure (n=12), fear of pain associated with the colonoscopy or DRE procedure (n=9), not being able to afford screening without healthcare (n=9), and aversion to bowel preparation (n=8) (Table 3). Other barriers included having a previous negative clinical experience (n=4), knowing someone who had a previous negative clinical experience (n=2), lack of insurance (n=5), lack of access to screening (n=2), and lack of education about the risks associated with CRC or the available methods of screening (n=6).
Table 3. Quotations and domain themes from focus groups.
| Barrier to screening | “Fear of the unknown, fear of what happens next if I do screen and I do have (colon cancer).” |
| Facilitator to screening | “I didn't want anything lying dormant in my body…(so) I made a promise that when it comes to my health, that is paramount. That's number one.” |
| Source of health information | “I'll research something and I'll “Google” it and try to get to the bottom of it.” |
| Source of CRC information | “I get annual physicals so I continue to transition and get older and it becomes more prevalent, something the doctor discussed with me when I turned forty.” |
| Mode of interventions | “The need is especially on the predominantly black radio stations, they don't mention this. …They don't mention colon cancer.” |
| Content for interventions | “To get people to hear the story and really understand, you have to meet people on their level. If you've got to get to the street level…then you have to go to the street level.” |
Facilitators to Screening
The most frequently reported screening facilitators related to self-perceptions of health status. Participants who described a poor diet or poor general health (n=8), and those who reported an interest in preventive medicine (n=6) endorsed a higher interest in CRC screening (Table 3). Other facilitators included use of CRC risk and screening education resources (n=5), receipt of insurance or monetary incentives (n=3), and celebrity endorsement of screening (n=3). Knowledge about methods to increase access to screening (n=2), use of media outlets to encourage screening (Internet, TV, or radio) (n=2), and access to information about alternative methods to screening (n=2) were also mentioned as facilitators to screening uptake.
Sources of Health and Screening Information
Participants identified exposure to varied sources of general health information about CRC screening. Most reported Internet or media sources as their most commonly accessed resource for information, including television, radio programs, magazines, health websites, health forum groups (e.g. WebMD, Google, Yahoo Answers), and television shows (e.g. Dr. Oz, Oprah) (n=24) (Table 3). Additional common resources for general health information included friends and family (n=10), medical staff, primary care providers, and other providers (n=9). Participants obtained information specifically regarding CRC screening from medical staff/doctors (n=8), Internet/television/radio (n=7), and family members (n=3) (Table 3).
Subject Intervention Mode and Content Recommendations
Figure 2 provides the concept network depicting the full list of modes and content suggested during the focus groups as well as code counts. Participants overwhelmingly reported the Internet, television or radio broadcasts as the mode to receive CRC screening information (n=12) (Table 3). Participants also suggested celebrity endorsements (n=6) and health fairs (n=6) as useful modes of distributing CRC screening information. Magazine advertisements and articles (n=5), billboards (n=5), screening facilities (n=3), educational classes (n=2), churches (n=2), community organizations (n=2), insurance providers (n=2), and advertisement of incentives (monetary or other) (n=2) were also mentioned.
Respondents suggested using culturally-tailored and culturally-sensitive educational materials that highlight the increased risk of CRC among African Americans and the specific benefits of screening (n=6). Specifically, participants suggested including comprehensive but clear information about the colonoscopy procedure (n=4) with attention to dispelling myths about pain or embarrassment (n=3). Screening endorsements by African American role models (n=5) and use of basic language (n=4) was also described as essential (Table 3). Others emphasized a need for interventions to relay the effectiveness of prevention (n=2) and the potential for increased longevity (n=2).
Post-Focus Group Survey Results
Most participants (n=24) indicated that they wanted to learn about all available options when determining which CRC screening method to pursue. Of the 33 respondents, 20 indicated that having a discussion with their doctor at the time of screening eligibility would be their preferred mode to receive education about CRC screening options. An educational booklet was the next preferred mode (n=6), followed by an interactive website (n=5).
Discussion
In this qualitative study, key elements were identified to improve the effectiveness of interventions aimed to increase CRC screening uptake among African Americans in the United States. Despite higher absolute risk for CRC among African Americans, focus group participants revealed a low perceived risk of CRC. In addition, participants reported that cost, lack of insurance and fear of colonoscopy prohibited CRC screening uptake while perception of poor health and exposure to CRC education were facilitators to screening. Participants reported that they currently obtained most of their health information from media or Internet sources but also stressed in the post-focus group survey that receiving information about CRC screening from providers at the time of screening eligibility was a preferred mechanism for education about CRC screening options. Participants strongly supported use of Internet or media outlets and celebrity endorsement as effective methods to disseminate information about CRC screening. Lastly, participants suggested that intervention content should include comprehensive and understandable education about the increased risk of CRC in African Americans and focus on dispelling myths about colonoscopy and screening.
These qualitative findings offer potential models for developing future culturally-tailored interventions to improve CRC screening among African Americans. While there has been criticism of interventions that require computer or Internet access in certain socioeconomic groups,[24] our findings highlight that these avenues are vital distribution channels for CRC screening information among African Americans. As we consider interventions to improve knowledge about CRC risk and screening, we should investigate ways to harness the influence of these media towards improving screening uptake. This result is consistent with literature supporting a pervasive use of the Internet among higher income and lower income African American families and an increasing desire to use Internet and mobile technologies for health information.[25]
Another novel finding of our study was that focus group participants endorsed use of African American celebrities or well-known members of the African American community as proponents of CRC screening. Participants believed this approach to be an effective facilitator to prompt screening, as well as an avenue to distribute information readily and efficiently to the African American population. Future public health interventions should employ prominent African American celebrities to improve awareness, dispel myths, and promote timely CRC screening.
There are several strengths to our study. By partnering with members of the African American community, we aimed to understand the root causes of disparities in CRC screening among African Americans in the U.S. Our interview script was based on a review of the literature about screening disparities in African Americans and an informed conceptual model of the patient-, provider-, and system-level factors that contribute to these differences.[20] Open-ended focus groups were performed with both screened and unscreened participants. In addition, while prior research in this area has focused mainly on the positive and negative predictors of screening uptake, few studies have utilized focus groups to inform the mode and content of future interventions to improve CRC screening uptake in the African American community.
This study also has important limitations. 38 African American participants were recruited whose opinions and sentiments may not fully reflect the broader population of African Americans in the U.S. Nonetheless, by recruiting participants across age, sex, and screening status, we sought to recruit a diverse cross-section of the African American community. Second, as is a limitation of all focus groups, conversations with groups of individuals may be influenced by the interview script or by a few dominant members of the group. As a result, our study may not represent all sentiments of the group members. In order to minimize this concern, involvement from all group members was encouraged and focus group dominance by one or two members was discouraged. Lastly, as this analysis is a qualitative observational study, the results cannot provide inferences about causal associations between participant sentiments and CRC screening behavior.
Although eliminating racial and ethnic disparities in healthcare has become a major public policy goal in the U.S., there is limited information on how to develop and implement appropriate interventions to reduce inequities in health. As healthcare reform extends health insurance options to individuals who previously had limited access to care, it will be important to develop tailored interventions to maximize the uptake of newly accessible preventive services. The use of qualitative studies in implementation science assures that interventions will be appropriately patient-centered and patient-tailored. By assessing the specific sentiments and needs of African Americans eligible for CRC screening, this information can be used in the service of developing appropriate interventions and eliminating CRC screening disparities.
Acknowledgments
Funding Support: This research was supported by the NIH Training grant (T32DK07180—40) for Dr. May. There was no sponsor for this research or publication.
Abbreviations
- CRC
Colorectal Cancer
- VA
Veterans Affairs
- ACA
Affordable Care Act
Footnotes
Disclaimer: The opinions and assertions contained herein are the sole views of the authors and are not to be construed as official or as reflecting the views of the Department of Veteran Affairs. The corresponding author confirms full access to all aspects of the research and writing process, and takes final responsibility for the paper.
Conflicts of Interest: None of the authors acknowledge any conflict of interest related to the conduction of this study.
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012 Jan-Feb;62(1):10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. Journal of the National Cancer Institute. 2011 Jan 19;103(2):117–28. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rise L, Eisner M, Kosary C. SEER cancer statistic review 1975-2000. Bethesda, MD: National Cancer Institute; 2003. [Google Scholar]
- 4.Lieberman DA, Holub JL, Moravec MD, Eisen GM, Peters D, Morris CD. Prevalence of colon polyps detected by colonoscopy screening in asymptomatic black and white patients. JAMA. 2008 Sep 24;300(12):1417–22. doi: 10.1001/jama.300.12.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashktorab H, Nouraie M, Hosseinkhah F, Lee E, Rotimi C, Smoot D. A 50-year review of colorectal cancer in African Americans: implications for prevention and treatment. Dig Dis Sci. 2009 Sep;54(9):1985–90. doi: 10.1007/s10620-009-0866-5. [DOI] [PubMed] [Google Scholar]
- 6.Murphy G, Devesa SS, Cross AJ, Inskip PD, McGlynn KA, Cook MB. Sex disparities in colorectal cancer incidence by anatomic subsite, race and age. Int J Cancer. 2011 Apr 1;128(7):1668–75. doi: 10.1002/ijc.25481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. The New England journal of medicine. 2013 Sep 19;369(12):1095–105. doi: 10.1056/NEJMoa1301969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hewitson P, Glasziou P, Watson E, Towler B, Irwig L. Cochrane systematic review of colorectal cancer screening using the fecal occult blood test [hemoccult]: an update. Am J Gastroenterol. 2008 Jun;103(6):1541–9. doi: 10.1111/j.1572-0241.2008.01875.x. [DOI] [PubMed] [Google Scholar]
- 9.Zauber AG, Winawer SJ, O'Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. The New England journal of medicine. 2012 Feb 23;366(8):687–96. doi: 10.1056/NEJMoa1100370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pignone M, Rich M, Teutsch SM, Berg AO, Lohr KN. Screening for colorectal cancer in adults at average risk: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002 Jul 16;137(2):132–41. doi: 10.7326/0003-4819-137-2-200207160-00015. [DOI] [PubMed] [Google Scholar]
- 11.May FP, Bromley EG, Reid MW, Baek M, Yoon J, Cohen E, et al. Low uptake of colorectal cancer screening among African Americans in an integrated Veterans Affairs health care network. Gastrointest Endosc. 2014 Aug;80(2):291–8. doi: 10.1016/j.gie.2014.01.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agrawal S, Bhupinderjit A, Bhutani MS, Boardman L, Nguyen C, Romero Y, et al. Colorectal cancer in African Americans. Am J Gastroenterol. 2005 Mar;100(3):515–23. doi: 10.1111/j.1572-0241.2005.41829.x. [DOI] [PubMed] [Google Scholar]
- 13.Naylor K, Ward J, Polite BN. Interventions to improve care related to colorectal cancer among racial and ethnic minorities: a systematic review. Journal of general internal medicine. 2012 Aug;27(8):1033–46. doi: 10.1007/s11606-012-2044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jemal A, Simard EP, Dorell C, Noone AM, Markowitz LE, Kohler B, et al. Annual Report to the Nation on the Status of Cancer, 1975-2009, featuring the burden and trends in human papillomavirus[HPV]-associated cancers and HPV vaccination coverage levels. Journal of the National Cancer Institute. 2013 Feb 6;105(3):175–201. doi: 10.1093/jnci/djs491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Christy SM, Perkins SM, Tong Y, Krier C, Champion VL, Skinner CS, et al. Promoting colorectal cancer screening discussion: a randomized controlled trial. Am J Prev Med. 2013 Apr;44(4):325–9. doi: 10.1016/j.amepre.2012.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Palmer RC, Midgette LA, Mullan ID. Colorectal cancer screening preferences among African Americans: which screening test is preferred? Journal of cancer education : the official journal of the American Association for Cancer Education. 2010 Dec;25(4):577–81. doi: 10.1007/s13187-010-0081-2. [DOI] [PubMed] [Google Scholar]
- 17.James AS, Daley CM, Greiner KA. Knowledge and attitudes about colon cancer screening among African Americans. American journal of health behavior. 2011 Jul;35(4):393–401. doi: 10.5993/ajhb.35.4.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Winterich JA, Quandt SA, Grzywacz JG, Clark P, Dignan M, Stewart JH, et al. Men's knowledge and beliefs about colorectal cancer and 3 screenings: education, race, and screening status. American journal of health behavior. 2011 Sep;35(5):525–34. doi: 10.5993/ajhb.35.5.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palmer RC, Midgette LA, Dankwa I. Colorectal cancer screening and African Americans: findings from a qualitative study. Cancer control. 2008 Jan;15(1):72–9. doi: 10.1177/107327480801500109. [DOI] [PubMed] [Google Scholar]
- 20.Bromley EG, May FP, Federer L, Spiegel BM, van Oijen MG. A Systematic Review of Patient, Provider, and System Barriers to Colorectal Cancer Screening With Colonoscopy in African-Americans. Gastroenterology. 2013:S581. AB Mo1110. [Google Scholar]
- 21.Palmer RC, Chhabra D, McKinney S. Colorectal cancer screening adherence in African-American men and women 50 years of age and older living in Maryland. Journal of community health. 2011 Aug;36(4):517–24. doi: 10.1007/s10900-010-9336-4. [DOI] [PubMed] [Google Scholar]
- 22.Wallace PM, Suzuki R. Regional, racial, and gender differences in colorectal cancer screening in middle-aged African-Americans and Whites. Journal of cancer education : the official journal of the American Association for Cancer Education. 2012 Dec;27(4):703–8. doi: 10.1007/s13187-012-0396-2. [DOI] [PubMed] [Google Scholar]
- 23.American Cancer Society. Colorectal Cancer Facts & Figures 2011-2013. Atlanta G: ACS; 2011. [Google Scholar]
- 24.McCleary-Jones V, Scheideman-Miller C, Rev Dorn JA, Jr, Johnson B, Overall M, Dwyer K. Health information technology use and health literacy among community-dwelling African Americans. The ABNF journal : official journal of the Association of Black Nursing Faculty in Higher Education, Inc. 2013 Winter;24(1):10–6. [PubMed] [Google Scholar]
- 25.Mitchell SJ, Godoy L, Shabazz K, Horn IB. Internet and mobile technology use among urban African American parents: survey study of a clinical population. Journal of medical Internet research. 2014;16(1):e9. doi: 10.2196/jmir.2673. [DOI] [PMC free article] [PubMed] [Google Scholar]


