Abstract
Objective
Increases in body weight and declining physical activity that may accompany aging are linked to a range of problems affecting daily life (i.e., decreased mobility and overall quality of life). This study investigates the actual and perceived neighborhood environment on overweight and obese urban older adults.
Method
We selected 217 individuals aged 65+ who answered questions about their neighborhood on the 2009 Speak to Your Health survey. Using multinomial regression models and geospatial models, we examined relationships between neighborhood environment and BMI.
Results
We found that obese older adults were 63% less likely to have a park within their neighborhood (p = .04). Our results also show that older adults who perceive their neighborhood crime as very high are 12 times more likely to be overweight (p = .04).
Discussion
Findings suggest that parks may affect BMI in older adults; however, neighborhood perceptions play a greater role.
Keywords: neighborhoods, older adults, obesity, urban health, crime
Introduction
Older adults represent a growing segment of the population in most industrialized nations (King et al., 2011). It is expected that by 2050, the number of Americans aged 65 and older will reach 88.5 million (Vincent & Velkoff, 2010). Currently, about one third of U.S. older adults have a body mass index (BMI) equal or greater than 30 (Fakhouri, Ogden, Carroll, Kit, & Flegal, 2012). Increases in body weight and declining physical activity, which often accompany aging, are linked to a range of problems affecting daily life, such as, decreased mobility (Stenholm et al., 2007), independence (Shepard, 1993), and overall quality of life (Dale et al., 2013). The dramatic increases in overweight and obesity over the past several decades is considered a major cause for the parallel rise in serious chronic conditions such as cardiovascular disease. Both aging and obesity contribute to increased health care use (K. F. Adams et al., 2006; Fakhouri et al., 2012); therefore, it is important to study these trends.
Social and Physical Environment
The neighborhood refers to a person’s immediate residential environment (Diez-Roux, 2001). Neighborhoods have been studied using both the social and physical environment (Weiss, Ompad, Galea, & Vlahov, 2007). Aspects of the social environment include socioeconomic status (occupation, income, and education), social conditions (i.e., neighborhood deterioration; Kruger, Reischl, & Gee, 2007), and change over time (e.g., changes in social circumstances over the life course and societal changes over time). A broad view of the physical environment includes food availability, sidewalks, opportunities for physical activity, and perception of safety, which have been implicated in physical activity patterns and related obesity patterns (Ferrer, Cruz, Bruge, Bayles, & Castilla, 2014; Gordon-Larsen, Nelson, Page, & Popkin, 2006).
The obesity epidemic is a result of obesity-promoting environmental factors interacting with relatively stable underlying genes among individuals who are susceptible in the population (King et al., 2011). As a consequence, public health research and health behavior intervention programs have focused primarily on social and physical environmental determinants, which either directly or indirectly influence dietary intake (Larson, Story, & Nelson, 2009) and physical activity (Bracy et al., 2014). Previous research on the characteristics of neighborhoods investigated their contribution to health behaviors and health status within a broader range of social, behavioral, and health concerns (Eilers, Lucey, & Stein, 2007; Sugiyama et al., 2014). Diez-Roux (2001) proposed a schematic representation of links across these dimensions of residential neighborhoods. Aspects of physical and social environments were seen as influencing physical activity, stress and psychosocial factors, diet, smoking, and sleep disturbance. These factors in turn, whether arising from the physical or social environment or both, would bear on proximate biological risk factors (i.e., blood pressure, BMI, blood glucose levels [A1C], blood lipids, stress response, and others) and ultimately cardiovascular diseases (King et al., 2011).
Older Adults
The link between the social and physical environments and obesity may be more important for older adults with long-term neighborhood residency, where poor environmental contexts may increase their vulnerability (Glass & Balfour, 2003). In addition, a growing U.S. older adult population may lead to more difficulties with comorbidities and health care spending (Federal Interagency Forum on Aging-Related Statistics, 2012). But the effect of obesity, which contributes to many chronic diseases, has mixed findings among older adults (K. F. Adams et al., 2006; Flegal, Kit, Orpana, & Graubard, 2013; Ralf, Jockel, Trautner, Spraul, & Berger, 1999). Earlier evidence regarding excess weight suggests mild obesity is a risk factor for mortality in older adults (Ralf et al., 1999); however, more recent reports show that BMI of greater than 35 is associated with significantly higher all-cause mortality relative to individuals of normal weight (Flegal et al., 2013). Lower mortality occurs among the moderately obese (BMI less than 35; Harris, Launer, Madans, & Feldman, 1997) and overweight (BMI of 25 to 30; Janssen, Katzmarzyk, & Ross, 2005). Alternatively, other studies of BMI show increased rates of morbidity among the overweight and obese (Flegal et al., 2013). Evidence also suggests that higher centralized obesity leads to greater risks of metabolic syndrome, particularly among older women (So & Yoo, 2015). These previous studies included older adults of different age ranges (50+ to 65+). In addition, the studies did not measure the effects of environment. Because older adults are becoming a larger segment of the U.S. population (Administration on Aging, 2013) and more are located in urban settings (Population Issues, 1999), it is important to study the effects of the urban environment on older adults. The purpose of this study is to examine the effects of environment, particularly neighborhood determinants, on BMI in older adults. This study adds to current research by comparing how actual and perceived neighborhood environment may affect overweight and obesity in older adults.
A theoretical framework for understanding social inequalities in health and aging proposed by House (House, 2005) graphically depicts how social, political, and economic conditions and policies as well as ascribed status and position are believed to affect a wide range of health outcomes among older adults. These outcomes may include mortality, morbidity, and functional limitations. Similar to Diez-Roux’s (2001) neighborhood model, which suggests that disadvantaged neighborhoods may lead to poor health outcomes, House proposes that social and environmental hazards such as lack of safety particularly at home may “get under the skin” causing changes in blood pressure or immune response. Our study uses variables from the House framework to examine how neighborhood environment may influence BMI among older adults. The proposal for this study was submitted for review to the university’s IRB and was determined to be exempt because of its use of de-identified survey data.
Method
The following analyses used data from the 2009 Speak to Your Health! Community survey, the 2010 U.S. Census, and Location, Inc. Speak to Your Health! is a telephone survey conducted by the Prevention Research Center of Michigan to collect demographic, environmental (i.e., neighborhood characteristics), services, and health information from a cross-section of individuals living in Genesee County, Michigan. Additional details on the Speak to Your Health survey were published in an earlier article (Kruger et al., 2010). Location, Inc. is a provider of location-based statistical data, which include crime statistics, lifestyle, and demographic data on neighborhoods across the United States. For our study, we collected crime information from November 2010 for Flint, Michigan. For census tract information, we used TIGER shapefiles for Genesee County, Michigan, from the 2010 U.S. Census.
Setting
Flint, Michigan, the urban center of Genesee County, is a de-industrialized city whose economy and population declined during the latter part of the 20th century. Flint has high unemployment and, based on local crime rates, was recently ranked in the top five most dangerous cities in the United States (D. Adams, 2013).
Participants
From 1,698 participants, who answered questions on the 2009 Speak to Your Health! survey, we selected 217 individuals over 65 years of age who lived within Flint. Because the number of survey participants from other races was very low (<5), we selected only White and Black participants and stratified the study subjects by racial categories. The terms Black and African American are used interchangeably and refer to the same group.
Outcome Measures
We calculated BMI for each of the participants based on self-reported weight and height. BMI is a measure of body fat based on height and weight in adults (National Heart, Lung, & Blood Institute, n.d.). Participants were then placed into one of three categories: normal weight (<18.5–24.9), overweight (25–29.9), and obese (30+).
Demographic Measures
The survey participants were mostly female—70% White females compared with 30% White males and 73% Black females versus 23% Black males. Education was collected as a categorical variable. For the purpose of this study, it was collapsed into four categories: less than high school, high school graduate, some college/technical school/associate’s degree, and bachelors’ degree or above. The study also included marital status—single (includes divorced, or widowed) and married or in a committed relationship (see Table 1).
Table 1.
Descriptive Statistics of the Study Population.
| Total (N = 217) | White | African American | Range |
|---|---|---|---|
| Demographics | |||
| Race | 112 | 105 | |
| Age (years) | 74.26 | 74.18 | 65–91 |
| Gender (%) | |||
| Male | 30 | 27 | |
| Female | 70 | 73 | |
| Social/economic | |||
| Education (%) | 1–4 | ||
| <High school | 7 | 27 | |
| High school or GED | 40 | 29 | |
| College/tech/associate degree | 30 | 28 | |
| Bachelor’s or above | 22 | 15 | |
| Marital status (%) | 0–1 | ||
| Single | 67 | 59 | |
| Married/committed relationship | 32 | 40 | |
| Health factors | |||
| BMIa | 29.80 | 28.39 | 17.2–46.4 |
| Cardiovascular disease (%) | 39.80 | 24.00 | 24.0–40.0 |
| Moderate physical activityb | 3.06 | 3.25 | 0–7 |
Note. BMI = body mass index; GED = General Educational Development.
The average BMI is given for each group.
The average number of days per week is reported.
Neighborhood Environment
The neighborhood was defined by census tract. A census tract is an area established by the Bureau of Census for analyzing populations. They generally encompass a population between 2,500 and 8,000 people (Geographic Products Branch U.S. Census Bureau, 2012). Neighborhood environment was measured using four items, availability of a park in the neighborhood (yes/no), availability of a library in the neighborhood (yes/no), grocery store in the neighborhood (yes/no), and neighborhood crime. Neighborhood crime was measured using multiple indicators. The crime rate in the neighborhood was measured using an index, which ranged from 1 to 100 with 1 being the most dangerous. Crime indices for each neighborhood are based on data from the Federal Bureau of Investigations (FBI) and the U.S. Justice Department. The crime indices used in this study gathered from Location, Inc. are the same as the FBI-defined crime index composed of the eight offenses the FBI combines to produce its annual index. These offenses include willful homicide, forcible rape, robbery, burglary, aggravated assault, larceny, motor vehicle theft, and arson. In addition to this objective indicator of neighborhood crime, survey participants also evaluated crime in the community. Participants were asked to rate the crime rate in their neighborhood compared with other neighborhoods (very high to very low). Finally, they were asked whether they had been the victim of a crime in the last 2 years (yes/no). To measure participation in neighborhood activities, respondents were asked whether they were “involved in neighborhood clean-up, beautification, or community garden projects” (yes or no).
Health Status/Behavior
Individuals were asked about their health status using self-reported indicators. They were asked whether or not they had been diagnosed with high blood pressure, heart disease, stroke, cancer, depression, anxiety, and diabetes (yes or no). A percentage of respondents answering yes were calculated for each group. The study calculated the average number of chronic conditions that the respondents reported. The participants were also asked to rate their health on a 5-point scale. The indicators excellent, very good, good, fair, and poor were converted to numeric values 1 through 5 with higher value indicating excellent health.
Finally, for participants’ self-reported physical activity levels, they were asked, “How many days per week do you engage in moderate physical activity, such as brisk walking, bicycling, vacuuming, gardening, for at least 10 min at a time?” Responses were grouped into four categories: No Physical Activity (0 days per week), Low Physical Activity (1–2 days per week), Average Physical Activity (3–4 days per week), High Physical Activity (5–7 days per week).
Statistical Analyses
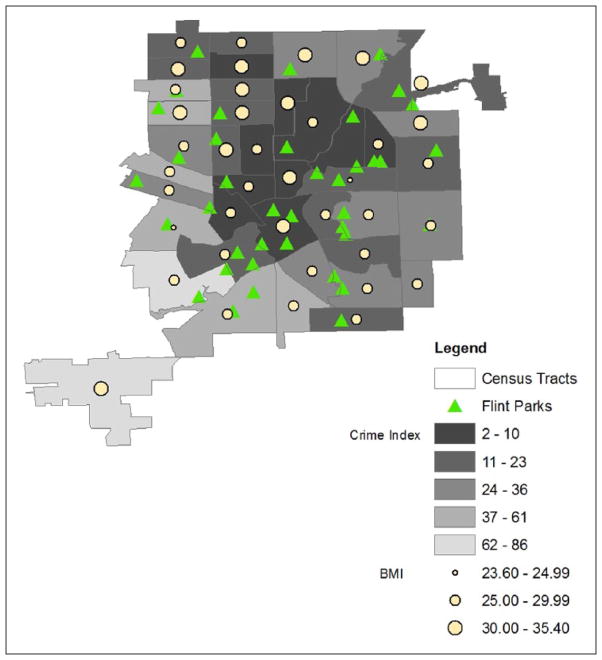
We stratified our study population by race (White and African American) and calculated the average age for each group. Then we assessed the proportions of each group based on gender, education level, and marital status (see Table 1). For analysis of neighborhood characteristics, we used a multinomial logistic regression model to examine the relationship between BMI and actual neighborhood environment (see Table 2). Using ARCGIS software, we created a geospatial comparison of parks, crime indices, and obesity levels for each neighborhood designated by census tract (see Figure 1). Next, we used a multinomial regression model to determine the relationship between BMI and perceived neighborhood environment, including perception of neighborhood crime and whether they had actually been a victim of crime (see Table 3). For our final analysis, we used a multinomial regression model to evaluate the relationship between moderate physical activity and neighborhood participation (see Table 4). We reported adjusted odds ratios, 95% confidence intervals, and p values. All regression models were analyzed using SPSS, Version 19.
Table 2.
Neighborhood Environment and BMI.
| Normal BMI vs. obese
|
Normal BMI vs. overweight
|
|||||
|---|---|---|---|---|---|---|
| Variables | OR | 95% CI | p value | OR | 95% CI | p value |
| Demographic | ||||||
| Age | 0.36 | [0.16, 0.83] | .02 | 1.14 | [0.53, 2.50] | .74 |
| Race | ||||||
| White | 1.00 | Reference | 1.00 | Reference | ||
| Black | 1.94 | [0.86, 4.42] | .11 | 1.39 | [0.63, 3.10] | .41 |
| Gender | ||||||
| Male | 1.00 | Reference | 1.00 | Reference | ||
| Female | 1.17 | [0.49, 2.83] | .26 | 0.90 | [0.39, 2.05] | .80 |
| Social/economic | ||||||
| Marital status | ||||||
| Singlea | 0.76 | [0.34, 1.73] | .52 | 0.68 | [0.31, 1.50] | .34 |
| Married | 1.00 | Reference | 1.00 | Reference | ||
| Education | ||||||
| <High school | 4.07 | [0.94, 17.71] | .06 | 1.01 | [0.28, 3.62] | .98 |
| High school graduate | 3.03 | [0.87, 10.62] | .08 | 0.78 | [0.29, 2.09] | .61 |
| College/associate degree | 5.67 | [1.55, 20.76] | .01 | 1.27 | [0.43, 3.73] | .66 |
| Bachelor’s and above | 1.00 | Reference | 1.00 | Reference | ||
| Neighborhood environment | ||||||
| Park | 0.37 | [0.14, 0.98] | .04 | 1.18 | [0.43, 3.21] | .75 |
| Library | 1.33 | [0.24, 3.41] | .98 | 2.62 | [0.57, 12.09] | .22 |
| Grocery store | 0.72 | [0.20, 2.62] | .62 | 0.94 | [0.24, 3.63] | .93 |
| Crime | 0.85 | [0.31, 2.35] | .76 | 0.26 | [0.08, 0.93] | .04 |
| N | 213 | |||||
Note. BMI = body mass index; OR = odds ratio; CI = confidence interval.
Single includes widowed, separated, and divorced participants.
Figure 1.
Flint neighborhoods showing parks, crime index, and BMI.
Note. BMI = body mass index.
Table 3.
Neighborhood Crime and BMI.
| Normal BMI vs. obese
|
Normal BMI vs. overweight
|
|||||
|---|---|---|---|---|---|---|
| Variables | OR | 95% CI | p value | OR | 95% CI | p value |
| Demographic | ||||||
| Age | 0.43 | [0.19, 0.96] | .03 | 1.24 | [0.55, 2.79] | .61 |
| Race | ||||||
| White | 1.00 | Reference | 1.00 | Reference | ||
| Black | 1.55 | [0.67, 3.57] | .31 | 1.66 | [0.72, 3.82] | .24 |
| Gender | ||||||
| Male | 1.00 | Reference | 1.00 | Reference | ||
| Female | 1.50 | [0.60, 3.76] | .40 | 0.70 | [0.29, 1.66] | .41 |
| Social/economic | ||||||
| Marital status | ||||||
| Singlea | 0.46 | [0.19, 1.12] | .09 | 0.51 | [0.21, 1.24] | .14 |
| Married | 1.00 | Reference | 1.00 | Reference | ||
| Education | ||||||
| <High school | 7.33 | [1.48, 36.31] | .01 | 0.89 | [0.24, 3.31] | .87 |
| High school graduate | 4.83 | [1.18, 19.78] | .03 | 0.76 | [0.26, 2.25] | .62 |
| College/associate degree | 10.04 | [2.31, 43.57] | <.01 | 1.15 | [0.35, 3.79] | .82 |
| Bachelor’s and above | 1.00 | Reference | 1.00 | Reference | ||
| Neighborhood crime | ||||||
| Very high | 1.70 | [0.14, 21.25] | .68 | 12.24 | [1.05, 142.41] | .04 |
| High | 0.59 | [0.14, 2.41] | .46 | 2.45 | [0.63, 9.56] | .20 |
| Average | 1.29 | [0.41, 3.98] | .66 | 2.15 | [0.63, 7.37] | .22 |
| Low | 0.85 | [0.27, 2.65] | .78 | 3.73 | [0.08, 0.93] | .02 |
| Very low | 1.00 | Reference | 1.00 | Reference | ||
| Victim of crime | 0.75 | [0.26, 2.15] | .59 | 0.15 | [0.04, 0.66] | .01 |
| N | 213 | |||||
Note. BMI = body mass index; OR = odds ratio; CI = confidence interval.
Single includes widowed, separated, and divorced participants.
Table 4.
Neighborhood Participation, Physical Activity, and BMI.
| Normal BMI vs. obese
|
Normal BMI vs. overweight
|
|||||
|---|---|---|---|---|---|---|
| Variables | OR | 95% CI | p value | OR | 95% CI | p value |
| Demographic | ||||||
| Age | 0.38 | [0.17, 0.87] | .02 | 1.27 | [0.58, 2.75] | .55 |
| Race | ||||||
| White | 1.00 | Reference | 1.00 | Reference | ||
| Black | 2.82 | [1.16, 6.85] | .02 | 1.45 | [0.64, 3.10] | .37 |
| Gender | ||||||
| Male | 1.00 | Reference | 1.00 | Reference | ||
| Female | 1.28 | [0.50, 3.25] | .61 | 0.96 | [0.43, 2.21] | .98 |
| Social/economic | ||||||
| Marital status | ||||||
| Singlea | 0.34 | [0.27, 1.57] | .34 | 0.55 | [0.24, 1.27] | .16 |
| Married | 1.00 | Reference | 1.00 | Reference | ||
| Education | ||||||
| <High school | 3.26 | [0.72, 14.84] | .13 | 1.13 | [0.32, 3.99] | .85 |
| High school graduate | 2.93 | [0.80, 10.73] | .10 | 0.72 | [0.26, 1.95] | .51 |
| College/associate degree | 7.04 | [1.83, 27.12] | <.01 | 1.16 | [0.39, 3.49] | .78 |
| Bachelor’s and above | 1.00 | Reference | 1.00 | Reference | ||
| Neighborhood participation | ||||||
| Beautification/garden | 0.23 | [0.09, 0.58] | <.01 | 0.43 | [0.19, 0.99] | .04 |
| Health behavior | ||||||
| No physical activity | 2.70 | [0.81, 7.51] | .03 | 0.31 | [0.11, 0.88] | .03 |
| Low physical Activity | 2.09 | [0.64, 6.85] | .01 | 0.28 | [0.09, 0.89] | .03 |
| Average physical Activity | 2.57 | [0.80, 8.27] | .11 | 0.67 | [0.23, 1.87] | .44 |
| High physical activity | 1.00 | Reference | 1.00 | Reference | ||
| N | 213 | |||||
Note. BMI = body mass index; OR = odds ratio; CI = confidence interval.
Single includes widowed, separated, and divorced participants.
Results
Our study population consisted of 217 individuals ranging in age from 65 to 91 years of age. There were a total of 112 White and 107 Black survey participants. The average age was similar for Whites and Blacks at 74.26 and 74.18 years, respectively. Among White older adults, 70% were females compared with 30% males, and among Blacks, 73% were females versus 23% males. Seven percent of White older adults did not complete high school or a GED compared with 27% of Blacks. Of those with the highest levels of education, 22% of Whites held a bachelor’s degree or higher, while 15% of blacks had an equivalent level of education. Only 32% of Whites were married or in a committed relationship compared with 40% of Blacks. There were no significant differences between White and Black older adults on the previous demographic variables. Although BMI was higher among Black older adults, mean scores for BMI were not significantly different between Whites (28.39) and Blacks (29.80). Black older adults reported higher levels of moderate physical activity; however, the levels between Black and White older adults were not significantly different (3.25 days vs. 3.06 days, respectively).
Table 2 summarizes our analysis of neighborhood environment and BMI among older adults. In this analysis, we compared obese and overweight with normal weight older adults in association with parks, libraries, grocery stores, and neighborhood crime index. Obese older adults were 63% less likely to have a park within their neighborhood than normal weight older adults (p = .04). For overweight older adults, we found that they were 74% less likely to live in area with high crime. Increasing age among older adults was related to a 64% lower odds of obesity versus normal BMI (p = .02). Because of the significant association between crime and BMI, we conducted further analysis of this neighborhood association. Results are shown in Table 3.
Figure 1 shows the relationship between the neighborhood average BMI and crime index. The map also shows the proximity of neighborhood parks and green spaces. The availability of grocery stores and libraries were not significantly associated with average neighborhood BMI; therefore, they were eliminated from the final version of the map.
Table 3 shows the individual’s perception of neighborhood crime and personal experience on BMI. Our results show that older adults who perceive their neighborhood crime as very high are 12 times more likely to be overweight (p = .04); however, they are 85% less likely to report being the victim of a crime within the last 2 years when compared with normal weight older adults (p = .01). Results were not significant between normal weight and obese older adults. Furthermore, increasing age among older adults was related to a 57% lower odds of obesity (p = .03).
Our final model examined associations between physical activity, neighborhood participation, and BMI. As expected, when compared with normal BMI, obese older adults were two to three times more likely to report no or low physical activity when asked how many days per week they engage in moderate physical activity (p = .03, p = .01). These older adults were also 80% less likely to participate in neighborhood activities such as gardening. These results also extend to overweight older adults. When compared with normal weight older adults, overweight older adults were 57% less likely to participate in neighborhood activities.
Discussion
We found among older adults that perception of the environment and actual neighborhood factors may similarly affect BMI. Obese older adults had less access to parks and grocery stores in their community but were more likely to have a library nearby. Perception of neighborhood crime is also associated with BMI. Although obese and overweight older adults are less likely to live in a high crime neighborhood, they are more likely to perceive the crime rate as higher and they are less likely to be a victim of a crime. This perception may influence obese older adults’ social behavior. Our results confirm obese older adults are less likely to participate in neighborhood activities, such as, gardening and neighborhood beautification. This lack of participation may lessen the opportunity for physical activity among older adults. Individuals who are involved in neighborhood activities are more likely to meet their neighbors and establish relationships. Previous studies have shown that knowing one’s neighbors can decrease vulnerability to health risks (Eilers et al., 2007). It also may be associated with low to no physical activity (Sullivan et al, 2014; VanDyck et al, 2013). Because older adults perceive their neighborhood as less safe, they are less likely to participate in social activities (Gallagher, 2010; Centers for Disease Control and Prevention, 1999). The limitations of this study are that the data are cross-sectional and the study population contains only Black and White urban residents. The study could be strengthened by examining additional races or ethnicities in other urban centers. However, because of the characteristics of this geographic area, the number of participants of other races or ethnicities was too small to analyze. Although these findings give insight into the relationship between neighborhood environment and BMI, it still raises questions that should be explored. Future research should assess what creates perceptions of crime and whether this perception substantially changes an individual’s health behaviors or BMI status. It is reasonable to assume that fear is caused by objective measures such as actual neighborhood crime rates, but it appears that other influences such as perception of neighborhood crime or history of victimization may play a greater role.
Conclusion
This study supports the conceptual framework for understanding social inequalities in health and aging proposed by House (2005). This framework, based on a stress and adaptation model from social epidemiology, theorizes that socioeconomic position and race/ethnicity shape individuals’ exposure to and experience of virtually all known psychosocial and environmental risk factors. These risk factors explain the size and persistence of social disparities in health. A growing body of literature suggests that social context matters in health outcomes (Ellaway, Macintyre, & Kearns, 2001; Kruger, Reischl, & Gee, 2007); however, only recent studies have examined these effects among older adults. And fewer studies separately compare obese and overweight with normal weight. This study adds to existing literature by examining differential effects of neighborhood environment among older adults. We were able to show that actual neighborhood factors and perception of the environment may have similar influences on BMI among urban older adults. Findings suggest that providing parks or other open spaces and changing perceptions on crime in the neighborhood may decrease the odds of obesity in older adults. Understanding specific neighborhood influences on health will enable us to improve the lives of older adults, many of whom are aging in place (Kochera, Straight, & Guterbock, 2005), and is crucial in addressing growing populations of urban older adults.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was developed from a pilot grant from the Michigan Center for Urban African-American Aging Research. The Speak to Your Health Survey was supported by the Centers for Disease Control and Prevention (CDC) grant U48/DP000055 through the Prevention Research Center of Michigan.
Biographies
Arlesia L. Mathis is an assistant professor of health policy and management in the Institute of Public Health at Florida A&M University. She earned her PhD in public health specializing in health policies and programs at University of South Florida College of Public Health in 2005. Her research interests focus on health disparities, minority health, and public health systems and services research. She has authored articles in the areas of primary care, public health systems and services, and population health disparities.
Ronica N. Rooks is an associate professor in the Department of Health and Behavioral Sciences at the University of Colorado–Denver. She earned her PhD in sociology at University of Maryland at College Park in 1999, with postdoctoral training in geriatric epidemiology in 1999–2001 and health disparities in 2001–2003. Her research interests focus on social-ecological explanations for racial and ethnic disparities in cardiovascular diseases (CVD). She has (co)authored articles in Social Science & Medicine, Race & Social Problems, Journal of Aging and Health, and Journal of Gerontology: Social Sciences.
Rima H. Tawk is an assistant professor in the Institute of Public Health at Florida A&M University. She earned her PhD in health policy and administration at the University of Illinois at Chicago (UIC) along with postdoctoral training in health economics and outcomes research at UIC. Her research interests focus on cancer outcomes research and predictive modeling.
Daniel J. Kruger is a research assistant professor in the Prevention Research Center at the University of Michigan School of Public Health. He earned his PhD in applied social psychology at Loyola University in Chicago, with postdoctoral training in psychosocial epidemiology at University of Michigan. His research interests focus on applied community health, mortality patterns, economic and consumer behavior, and risk taking. He has authored more than 80 peer-review articles in public health and social psychology.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Adams D. Flint still tops nation for violent crime but officials see signs of hope. MLive. 2013 Sep 13; Retrieved from http://www.mlive.com/news/flint/index.ssf/2013/09/flint_still_tops_in_nation_for.html.
- Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, Leitzmann MF. Overweight, obesity and mortality in a large prospective cohort of persons 50 to 71 years old. New England Journal of Medicine. 2006;355:763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- Administration on Aging. Aging statistics. 2013 Retrieved from http://www.aoa.gov/Aging_Statistics/
- Bracy NL, Millstein RA, Carlson JA, Conway TL, Sallis JF, Saelens BE, King AC. Is the relationship between the built environment and physical activity moderated by perceptions of crime and safety? International Journal of Behavioral Nutrition and Physical Activity. 2014;11(1):11–24. doi: 10.1186/1479-5868-11-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Neighborhood safety and the prevalence on physical inactivity—Selected states, 1996. MMWR Morbidity and Mortality Weekly Report. 1999;48(7):143–146. [PubMed] [Google Scholar]
- Dale C, Bowling A, Adamson J, Kuper H, Amuzu A, Ebrahim S, Nüesch E. Predictors of patterns of change in health-related quality of life in older women over 70 years: Evidence from a prospective cohort study. Age and Ageing. 2013;42:312–318. doi: 10.1093/ageing/aft029. [DOI] [PubMed] [Google Scholar]
- Diez-Roux A. Investigating neighborhood and area effects on health. American Journal of Public Health. 2001;91:1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eilers MK, Lucey P, Stein SS. Promoting social capital for the elderly. Nursing Economics. 2007;25:304–307. [PubMed] [Google Scholar]
- Ellaway A, Macintyre S, Kearns A. Perceptions of place and health in socially contrasting neighbourhoods. Urban Studies. 2001;38:2299–2316. [Google Scholar]
- Fakhouri THI, Ogden C, Carroll M, Kit BK, Flegal KM. NCHS Data Brief. National Center for Health Statistics; 2012. Prevalence of obesity among older adults in the United States, 2007–2010; pp. 1–7. [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key indicators of well-being. Federal interagency forum on aging-related statistics. Washington, DC: U.S. Government Printing Office; 2012. Jun, [Google Scholar]
- Ferrer R, Cruz I, Bruge S, Bayles B, Castilla M. Measuring capability for health diet and physical activity. Annuals of Family Medicine. 2014;12:46–56. doi: 10.1370/afm.1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories. Journal of the American Medical Association. 2013;309:71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher N. Neighborhood factors relevant for walking in older, urban, African-American adults. Journal of Aging and Physical Activity. 2010;18:99–115. doi: 10.1123/japa.18.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geographic Products Branch U.S. Census Bureau. Census tracts. Census Tracts. 2012 Retrieved from http://www.census.gov/geo/maps-data/data/tiger-line.html.
- Glass TA, Balfour JL. Neighborhoods, aging, and functional limitations. In: Kawachi I, Berkman LF, editors. Neighborhoods and health. Oxford, UK: Oxford University Press; 2003. pp. 303–334. [Google Scholar]
- Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlie key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- Harris TB, Launer LJ, Madans J, Feldman JJ. Cohort study of effect of being overweight and change in weight on risk of coronary health disease in old age. British Medical Journal. 1997;314:1791–1794. doi: 10.1136/bmj.314.7097.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS. Continuity and change in the social stratification of aging and health over the life course: Evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans’ changing lives study) Journal of Gerontology. 2005;60B:15–26. doi: 10.1093/geronb/60.special_issue_2.s15. [DOI] [PubMed] [Google Scholar]
- Janssen I, Katzmarzyk P, Ross R. Body mass index is inversely related to mortality in older people after adjustment for waist circumference. Journal of the American Geriatrics Society. 2005;53:2112–2118. doi: 10.1111/j.1532-5415.2005.00505.x. [DOI] [PubMed] [Google Scholar]
- King AC, Sallis JF, Frank LD, Saelens BE, Cain K, Conway TL, Kerr J. Aging in neighborhoods differing in walkability and income: Associations with physical activity and obesity in older adults. Social Science & Medicine. 2011;73:1525–1533. doi: 10.1016/j.socscimed.2011.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochera A, Straight A, Guterbock T. Beyond 50.05—A report to the nation on livable communities: Creating environments for successful aging. Washington, DC: AARP Policy Institute; 2005. [Google Scholar]
- Kruger DJ, Hamacher L, Struger-Fritsch D, Shirey L, Renda E, Zimmerman Marc A. Facilitating the development of a county health coverage plan with data from a community-based health survey. Journal of Public Health Policy. 2010;31:199–211. doi: 10.1057/jphp.2010.8. [DOI] [PubMed] [Google Scholar]
- Kruger DJ, Reischl T, Gee G. Neighborhood social conditions mediate the association between physical deterioration and mental health. American Journal of Community Psychology. 2007;40:261–271. doi: 10.1007/s10464-007-9139-7. [DOI] [PubMed] [Google Scholar]
- Larson NI, Story MT, Nelson MC. Neighborhood environments disparities in access to health foods in the U.S. American Journal of Preventive Medicine. 2009;36:74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- National Heart, Lung and Blood Institute. Aim for a healthy weight. n.d Retrieved from http://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmi-m.htm.
- Population Issues. Migration and urbanization. 1999 Retrieved from https://www.unfpa.org/6billion/populationissues/migration.htm.
- Ralf B, Jockel K, Trautner C, Spraul M, Berger M. Effect of age on excess mortality in obesity. Journal of the American Medical Association. 1999;281:1498–1504. doi: 10.1001/jama.281.16.1498. [DOI] [PubMed] [Google Scholar]
- Shepard RJ. Exercise and aging: Extending independence in older adults. Geriatrics. 1993;48(5):61–64. [PubMed] [Google Scholar]
- So ES, Yoo KS. Waist circumference cutoff points for central obesity in the Korean elderly population. Journal of Applied Gerontology. 2015;34:102–117. doi: 10.1177/0733464812464428. [DOI] [PubMed] [Google Scholar]
- Stenholm S, Sainio P, Rantanen T, Koskinen S, Jula A, Heliövaara M, Aromaa A. High body mass index and physical impairments as predictors of walking limitation 22 years later in adult Finns. Journal of Gerontology. 2007;62A:859–865. doi: 10.1093/gerona/62.8.859. [DOI] [PubMed] [Google Scholar]
- Sugiyama T, Cerin E, Owen N, Oyeyemi AL, Conway TL, Van Dyck D, Sallis JF. Perceived neighbourhood environmental attributes associated with adults’ recreational walking: IPEN adult study in 12 countries. Health & Place. 2014;28:22–30. doi: 10.1016/j.healthplace.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan SM, Brashear MM, Broyles ST, Rung AL. Neighborhood environments and obesity among African-American, and non-Hispanic White adults in the united states: Results from the national survey of American life. Preventive Medicine. 2014;61:1–5. doi: 10.1016/j.ypmed.2013.12.023. [DOI] [PubMed] [Google Scholar]
- Van Dyck D, Sallis JF, Cardon G, Deforche B, Adams MA, Geremia C, De Bourdeaudhuij I. Associations of neighborhood characteristics with active park use: An observational study in two cities in the USA and Belgium. International Journal of Health Geographics. 2013;12(26):1–9. doi: 10.1186/1476-072X-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent GK, Velkoff VA. Current Population Reports, P25-1138. Washington, DC: U.S. Census Bureau; 2010. The next four decades: The older population in the United States: 2010 to 2050. [Google Scholar]
- Weiss L, Ompad D, Galea S, Vlahov D. Defining neighborhood boundaries for urban health research. American Journal of Preventive Medicine. 2007;32:S154–S159. doi: 10.1016/j.amepre.2007.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]