Abstract
Background
Hepato-pancreato-biliary (HPB) surgery is a complex subspecialty drawing from varied training pools, and the need for competency is rapidly growing. However, no board certification process or standardized training metrics in HPB surgery exist in the Americas. This study aims to assess the attitudes of current trainees and HPB surgeons regarding the state of training, surgical practice and the HPB surgical job market in the Americas.
Study Design
A 20-question survey was distributed to members of Americas Hepato-Pancreato-Biliary Association (AHPBA) with a valid e-mail address who attended the 2014 AHPBA. Descriptive statistics were generated for both the aggregate survey responses and by training category.
Results
There were 176 responses with evenly distributed training tracks; surgical oncology (44, 28%), transplant (39, 24.8%) and HPB (38, 24.2%). The remaining tracks were HPB/Complex gastrointestinal (GI) and HPB/minimally invasive surgery (MIS) (29, 16% and 7, 4%). 51.2% of respondents thought a dedicated HPB surgery fellowship would be the best way to train HPB surgeons, and 68.1% felt the optimal training period would be a 2-year clinical fellowship with research opportunities. This corresponded to the 67.5% of the practicing HPB surgeons who said they would prefer to attend an HPB fellowship for 2 years as well. Overall, most respondents indicated their ideal job description was clinical practice with the ability to engage in clinical and/or outcomes research (52.3%).
Conclusions
This survey has demonstrated that HPB surgery has many training routes and practice patterns in the Americas. It highlights the need for specialized HPB surgical training and career education. This survey shows that there are many ways to train in HPB. A 2-year HPB fellowship was felt to be the best way to train to prepare for a clinically active HPB practice with clinical and outcomes research focus.
Introduction
Hepato-pancreato-biliary (HPB) surgery is a complex subspecialty drawing from many different training pools. The need for competent HPB surgeons is rapidly growing.1 Evidence exists to suggest that high-volume HPB centres confer better surgical outcomes.2–6 Unfortunately, such centres are not always uniformly distributed geographically in the Americas and can burden patients in remote areas with long commute times for treatment and follow-up care. As a consequence, secondary to local patient demand, up to 40% of complex HPB procedures in the United States are performed at community centres with lower volume by general (non-HPB) surgeons.7
Surgery residents are usually exposed to the HPB field as a part of their general surgery training. This exposure varies depending on training centre volume and expertise. The Accreditation Council for Graduate Medical Education (ACGME) case log data in the USA indicates that most surgical residents log 0–3 major HPB cases.8,9 Obviously, to perform complex HPB cases, additional training beyond general surgery residency is required. Up to 20 years ago, in United States, the two educational tracks that offered the aforementioned additional training were the Abdominal Transplant Surgery Fellowships via American Society of Transplant Surgeons (ASTS)10 and the Surgical Oncology Fellowships via Society of Surgical Oncology (SSO)11 accredited programmes. Overall, the HPB case requirements were minimal for both these educational tracks. Alternatively, additional HPB surgery training could be achieved via individual fellowship positions wherein surgeons would spend an additional 1–2 years gaining experience in the HPB field under the mentorship of senior staff that was preferentially performing these complex procedures. Significant variation in the number of cases and training methodology was seen among institutions. These fellowships initially had no governing body or minimal case requirements. Graduates relied on the recommendation of their mentors and on the strength of institutional reputation to give credence to their training.
In 1994, the Americas Hepato-Pancreato-Biliary Association (AHPBA) was created with the primary objective to facilitate collaboration and improvement of HPB surgery in North, Central and South America. Out of this organization, an association with the Fellowship Council (FC) was forged. The FC housed the majority of non-ACGME fellowships in North America. The AHPBA became a sponsoring society and developed criteria that were validated during the accreditation process by the FC. The AHPBA was the first of the sponsoring societies of the FC that offered a certificate to graduates of FC-accredited programmes. This certificate process was initiated in 2010. Presently there are 20 programmes in the US and six programmes in Canada that offer the HPB fellowship for general surgeons who have completed residency.12
Currently, there is no board certification process in HPB surgery. Training in HPB surgery is still offered in the three different tracks mentioned above in association with their parent organizations. The SSO accredited programme is now part of a board certified ‘Complex Surgical Oncology’ under the ACGME that is meant to provide broad exposure to surgical oncology. Each of these tracks offers advantages and disadvantages that were highlighted at a recent consensus conference of leaders in HPB Surgery education.13
This study was designed to address a gap in knowledge regarding the views on HPB training across different training tracks in the Americas. The AHPBA constituency represents HPB surgeons who have trained in different models including transplantation, surgical oncology and HPB. Therefore, this is the ideal group to query to address this information gap.
A survey was undertaken and distributed to all AHPBA members to understand current attitudes amongst HPB trainees and surgeons regarding their fellowship and practice.
Methods
A survey was distributed to members of the AHPBA with a valid electronic mail (e-mail) address and/or internet access. This included practicing HPB surgeons and those in training (residents and fellows) in North, South and Central America. Responses to the survey were anonymous. A survey of 20 questions was developed based upon contents discussed at the Bernard Langer Fellows and Residents Symposium at the AHPBA national meeting in February 2014, Miami, FL (Appendix A1). The questionnaire was initially validated amongst a small cohort of residents and fellows for content and clarity. The average time for completion was approximately 5 min. Subsequently, the survey was distributed to conference attendees and AHPBA members. Results were tabulated, and descriptive statistics were generated for the aggregate survey responses. Further stratification was performed based on ‘Current Status’ or ‘Specialty Track’. ‘Current Status’ included the categories Senior Practicing HPB Surgeon (>5 years of experience), Practicing HPB Surgeon (<5 years of experience), Current Fellow, Matched Incoming Fellow and HPB-Interested Resident. ‘Specialty Track’, which is a reference to type of clinical practice, included the categories of HPB Surgery alone, HPB/Complex GI Surgery, HPB/MIS (Minimally Invasive Surgery), Surgical Oncology and Transplant Surgery.
Results
Study population demographics
A total of 176 out of 1231 (14.3%) members of the AHPBA responded to the survey. Almost nine out of 10 (86.2%) were male. Most respondents were 31–50 years of age (n = 138, 78.8%) and were practicing HPB surgeons for more than 5 years (n = 85, 50.0%). The remaining respondents were in the early stages of their careers as current fellows, matched incoming fellows, or residents interested in HPB (n = 31, 18.2%). Training backgrounds were not evenly distributed. Surgical oncology training was most commonly reported (n = 44, 28%) followed by Transplant and HPB surgeons (n = 39, 24.8% and n = 38, 24.2%, respectively). Two other ‘Specialty Track’ categories included 29 (16%) respondents for HPB/Complex GI Surgery and 7 (4%) respondents for HPB/Minimally Invasive Surgery.
HPB surgery training
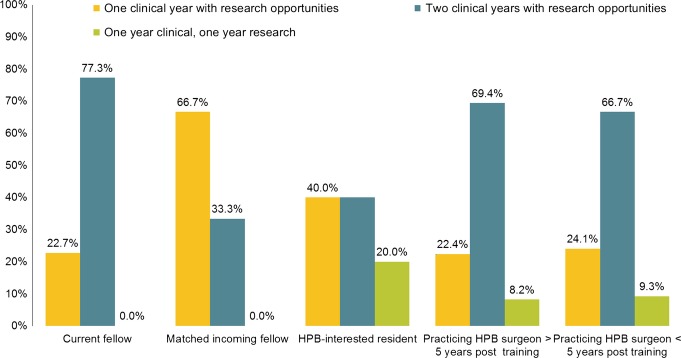
More than half of respondents thought a dedicated HPB surgery fellowship would be the best way to train HPB surgeons (n = 86, 51.2%). Current fellows thought this was the best training option as compared with other ‘Current Status’ types (Table1). In contrast, 19% (n = 33) of the respondents indicated that too many HPB surgeons were currently being trained. In terms of training duration, 68.1% (n = 115) felt that the optimal training period would be a 2-year clinical fellowship with research opportunities. This observation is in concert with the preference of 67.5% (n = 104) of the respondents to participate in a 2-year HPB fellowship, should they have to start their HPB training now. Current fellows preferred a 2-year pure-clinical model with research opportunities. Neither current fellows nor matched incoming fellows preferred a 1-year pure research and 1-year pure-clinical model (Fig.1).
Table 1.
Opinions of fellowship training modalities by survey respondent status type
| What do you think is the best way to train HPB surgeons? | ||||
|---|---|---|---|---|
| HPB surgery fellowship | Surgical oncology fellowship | Transplant surgery fellowship | Not applicable – we are training too many HPB surgeons already | |
| What is your current status? | N (%) | |||
| Current fellow | 15 (68.2) | 4 (18.2) | 1 (4.5) | 2 (9.1) |
| Matched incoming fellow | 2 (66.7) | 0 (0) | 0 (0) | 1 (33.3) |
| HPB-interested resident | 3 (50.0) | 1 (16.7) | 2 (33.3) | 0 (0) |
| Practicing HPB surgeon > 5 years post training | 36 (43.4) | 13 (15.7) | 15 (18.1) | 19 (22.9) |
| Practicing HPB surgeon <5 years post training | 30 (55.6) | 9 (16.7) | 5 (9.3) | 10 (18.5) |
| Total | 86 (51.2) | 27 (16.1) | 23 (13.7) | 32 (19.0) |
HPB, hepato-pancreato-biliary.
Figure 1.
Preference of hepato-pancreato-biliary (HPB) fellowship length and composition stratified by respondent status
HPB surgery practice
About half of the respondents indicated their ideal job description was clinical practice with the ability to engage in clinical and/or outcomes research (n = 81, 52.3%). Senior practicing HPB surgeons wanted to include more basic science in their research activities (50% versus 37.4% of all respondents). Finally, a career in a traditional academic setting would be the preferred practice environment for 60%, 59% and 45% of senior practicing HPB surgeons, junior Practicing HPB Surgeons and current fellows, respectively.
Operative capacity/capability
Pancreaticoduodenectomy (Whipple procedure)
Responders felt that 29 cases needed to be performed for one to gain enough experience to operate independently (range 2–75). Those in the HPB Surgery track and the transplant surgery track indicated the highest and lowest average number of pancreaticoduodenectomies performed, respectively (48 versus 26). The average number of Whipple's performed from respondents of from all training tracks during their training was 38 Respondents from all specialty tracks performed more Whipple procedures during training than they felt they needed to perform the procedure safely and independently (Fig.2; Table2).
Figure 2.
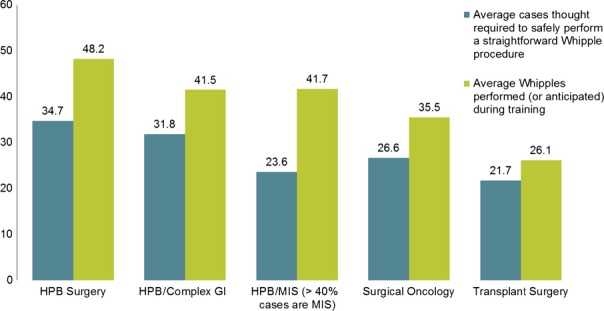
Comparison of average cases thought necessary to perform a Whipple safely to average Whipple cases performed, by survey respondent specialty track. HPB, hepato-pancreato-biliary; GI, gastrointestinal tract; MIS, minimally invasive surgery
Table 2.
Case training characteristics and opinions by survey respondent specialty track
| Answers by Specialty Track | HPB Surgery | HPB/Complex GI | HPB/MIS (>40% cases are MIS) | Surgical Oncology | Transplant Surgery |
|---|---|---|---|---|---|
| Pancreaticoduodenectomy required for independent performance | 34.7 | 31.8 | 23.6 | 26.6 | 21.7 |
| Pancreaticoduodenectomy performed in training | 48.2 | 41.5 | 41.7 | 35.5 | 26.1 |
| Hemi-liver resection required for independent performance | 35.3 | 28.0 | 20.0 | 22.2 | 24.2 |
| Hemi-liver resection performed in training | 73.3 | 24.7 | 18.3 | 33.9 | 45.2 |
HPB, hepato-pancreato-biliary; MIS, minimally invasive surgery; GI, gastrointestinal tract.
Hemi-liver resection
On average, respondents felt that 27.0 training cases were needed to perform a hemi-liver resection safely and independently (20–35). Those in the HPB Surgery track indicated the highest average number of training cases needed to be comfortable whereas the HPB/Minimally Invasive Surgery trained surgeons indicated the lowest (35.0 versus 20.0). Surgeons of the HPB Surgery, Surgical Oncology and Transplant Surgery tracks performed more hemi-liver resection procedures during their training than they felt they needed to perform the procedure safely and independently. In contrast, the HPB/Complex GI Surgery and HPB/MIS tracks did not (Fig.3; Table2).
Figure 3.
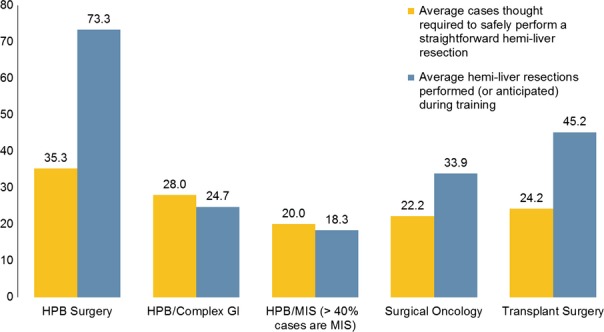
Comparison of average cases thought necessary to perform a hemi-liver resection safely to average hemi-liver resection cases performed, by survey respondent specialty track. HPB, hepato-pancreato-biliary; GI, gastrointestinal tract; MIS, minimally invasive surgery
Minimally invasive surgery
Surgeons were asked, on a scale from 1 (most uncomfortable) to 10 (most comfortable), how they felt performing a Whipple or a hemi-liver resection using minimally invasive approaches. Only HPB/MIS track respondents were comfortable in performing a minimally invasive Whipple (9.0 versus 3.0 overall, P = 0.004, Table3). In contrast, no statistically significant difference was identified among different training tracks with regards to comfort performing a minimally invasive hemi-liver resection (P = 0.101).
Table 3.
Hepato-pancreato-biliary (HPB) surgery comfort scores by survey respondent specialty track
| Specialty Track | Comfort Scale: 1-most uncomfortable 10 - most comfortable | ||
|---|---|---|---|
| How comfortable are you at performing a MIS Whipple | How comfortable are you performing a MIS hemi-liver resection | ||
| Mean (SD) | P value | ||
| HPB surgery | 2.2 (2.2) | 4.6 (2.3) | <0.001 |
| HPB/Complex GI | 3.6 (3.5) | 4.3 (2.8) | 0.282 |
| HPB/MIS (> 40% cases are MIS) | 8.6 (1.3) | 5.7 (1.7) | 0.004 |
| Surgical oncology | 3.2 (2.7) | 5.0 (3.1) | 0.005 |
| Transplant surgery | 3.7 (3.2) | 5.9 (3.0) | 0.012 |
| Total | 3.3 (3.0) | 5.1 (2.8) | <0.001 |
| P-value, between groups | <0.001 | 0.202 | |
MIS, minimally invasive surgery; GI, gastrointestinal tract.
Practicing HPB surgeons
Most practicing HPB surgeons felt the best way to train other HPB surgeons was through a dedicated HPB fellowship (48.2%) comprising of two clinical years with research opportunities (68.4%). Supporting this finding, 68.9% indicated they would have preferred to attend an HPB fellowship that was 2 years in length.
On average, practicing HPB surgeons felt 28.5 cases were needed to perform a Whipple procedure independently. Similarly, this group said 27.6 cases were needed to perform a hemi-liver resection procedure independently. In terms of the level of comfort with performing these procedures with MIS techniques, on a scale from 1 to 10, practicing HPB surgeons felt only slightly more comfortable than all other respondents (3.7 versus 3.3 overall) with a Whipple procedure, similar findings were seen with performing an MIS hemi-liver resection (5.5 versus 5.1 overall). When the practicing HPB surgeons group was stratified by length of time post-training, comfort with performing these procedures predictably increased with time, where surgeons who were more than 5 years post training indicated a 4.0 on the comfort scale with MIS Whipple's, versus their counterparts with less than 5 years of training who indicated a 3.2. This pattern was seen with MIS hemi-liver resections as well, where those >5 years post training indicated a 6.0 on the comfort scale versus surgeons with <5 years indicating a 4.8.
Finally, practicing HPB surgeons felt outcomes research was best achieved in high-volume centres (48.2%) and a clinical practice with the ability to do outcomes research was their ideal job scenario (50.4%), although this preference decreased with more time post-training (41.7% with >5 years versus 62.8% <5 years).
Discussion
At present, there is very little regulation regarding allotment of hospital privileging in respect with HPB Surgery in the Americas. It is critical to the future of the field that uniform expectations of experience and quality are established so that the HPB surgical community may set the standards to which it will be held. We must collectively decide the ‘learning curve’ for each one of the HPB procedures and these should be completed within training. This should allow the novice HPB surgeon to be able to perform the majority of the cases in an independent fashion. Emphasis must also be placed to decide what level of institutional volume is needed to quantify hospitals ‘centres of excellence’ in HPB surgery. In making these designations and establishing recommended training or privileging requirements, we protect our patients, our reimbursements and the future of our profession.
Given the historical existence of HPB surgery as a part of other general surgical disciplines, it is unrealistic to expect that a transition away from the more traditional routes to HPB such as SSO and ASTS fellowships will give way to a dedicated HPB track, such as the currently applied AHPBA training model. Moreover, each training track offers a different but important perspective towards HPB disease processes, and the collaboration amongst surgeons from all three training tracks presents unparalleled opportunities for surgical innovation and advancement. However, to preserve what has, therefore, been a symbiotic interdisciplinary relationship, surgeons from each of the three training tracks must collaborate to ensure the field moves forward in a sustainable manner. In the coming years, difficult questions will arise, such as what is the number of HPB-trained surgeons needed to meet the growing demand of an aging population. A recent study has shown that the majority of the US is underserved in respect to HPB surgical care.14Another question is what role surgical governing bodies should have in regulating hospital privileging for complex HPB procedures. Answers to these and many other relevant questions could be obtained perhaps only through a national needs analysis for HPB Surgery Fellowship with stakeholders that include: (i) HPB Surgery fellows (expressed and felt needs), (ii) HPB Surgery academic faculty (expressed, normative and comparative needs), (iii) General Surgery residents (expressed and felt needs), (iv) HPB Surgery non-academic practicing surgeons (normative and comparative needs), (v) HPB Surgery mid-level providers (normative and comparative needs), (vi) Health Care and Medical Education policy makers (normative and comparative needs) and most importantly, and (vii) patients (expressed and felt needs). However, the AHPBA's initial foray into answering these questions in a smaller scale took place in conjunction with the 2014 American College of Surgeons Clinical Congress at the first ever consensus conference on HPB training.13,15,16
As with any survey, this tool and the data it produced have limitations. First, there is the inherent bias that comes with a survey created by AHPBA members for AHPBA conference attendees. While the AHPBA conference is well attended by many surgeons from ASTS and SSO training backgrounds, the ones participating in the AHPBA meeting may be more open to HPB training pathways than their colleagues. Despite attempts to appropriately validate the survey, the authors overlooked the established surgeon perspective, so questions regarding ideal practice types and current job search status were difficult for practicing surgeons to answer. These questions may not have been worded in a way that established surgeons felt they could answer and, therefore, results stemming from these questions must be taken with this bias in mind. Finally, the response rate of the survey (176/1231, 14.3%) was suboptimal, and as the sample was not statistically calibrated, the survey was unable to yield statistically meaningful conclusions. Nevertheless, the observable trends in responses are intriguing and accomplish the intended goal, which was the initiation of a discussion.17
Despite the limitations, some very interesting data have arisen from this survey. For instance, the concordance of various respondent groups regarding the optimal length of training; while most AHPBA-accredited training programmes in North America are 1 year in length, the vast majority of current fellows, and two-thirds of practicing surgeons indicated that a 2-year clinical programme with research opportunities would be the optimal fellowship length. Very few respondents preferred the 2-year fellowship with one research and one clinical year. This is an interesting response. The authors feel that fellowship training has many components to it that are not measured by operative volume alone; for example, learning the business of HPB surgery practice and increasing research productivity. These elements may take longer than 1 year. With regards to a number of cases required to achieve procedural competence, all respondent groups indicated that they performed more Whipple procedures during training than they felt were necessary to become proficient, as detailed in Fig.2. Interestingly, those from training tracks who reported the highest HPB case volumes during training also indicated that more cases were necessary to achieve proficiency. A similar phenomenon was seen with regards to hemi-liver resections. Surgeons who identified with SSO, AHPBA, and ASTS tracks, all felt as if they performed in training as many hemi-hepatectomies as necessary for them to become proficient. Here again, the HPB track respondents, although they performed more hemi-hepatectomies than any other respondents, still felt that more cases were required to become proficient. This may be because HPB pathway fellowships are often 1 year, whereas SSO and ASTS are traditionally 2 years in length. Certainly, studies to establish the ideal learning curve for HPB cases are warranted, but this insight into surgeon perception can help inform future decisions. Not surprisingly, only the HPB/Minimally Invasive Surgery training group indicated a high level of comfort performing a minimally invasive Whipple. While the true role of a minimally invasive pancreaticoduodenectomy has yet to be readily accepted, further studies should be performed to truly understand the state of minimally invasive HPB surgery in North America today and how the HPB training programmes should explore the minimally invasive boundaries.
The disparity in comfort level across training tracks is shown in Table4. The authors feel that MIS liver surgery has been more prevalent in training programmes than an MIS pancreaticoduodenectomy. This may explain the relative comfort with the liver as compared with a pancreaticoduodenectomy.
Table 4.
Comfort in minimally invasive surgery hepato-pancreato-biliary (MIS HPB) surgery by training track
| On a scale of 1–10 (1-most uncomfortable to 10 - most comfortable) | ||
|---|---|---|
| How comfortable are you at performing a MIS Whipple | How comfortable are you at performing a minimally invasive hemi-liver resection | |
| Specialty Track | n (%) of those that were comfortable (a ‘6’ or more on the comfort scale) within each specialty track | |
| HPB surgery | 3/38 (7.9) | 13/36 (36.1) |
| HPB/Complex GI | 9/28 (32.1) | 9/29 (31.0) |
| HPB/MIS (>40% cases are MIS) | 7/7 (100.0) | 3/7 (42.9) |
| Surgical oncology | 8/44 (18.2) | 18/44 (40.9) |
| Transplant surgery | 9/37 (24.3) | 20/36 (55.6) |
GI, gastrointestinal tract.
n = number of respondents that were comfortable/total number of respondents in the Specialty track.
Finally, 51% of the respondents believed that HPB fellowship is the best way to teach HPB surgery, which means that close to half of the respondents believe that training for HPB surgery can be achieved by other means. This speaks to the importance of standardization among disciplines to ensure quality outcomes. Both, the nature of HPB surgery and the widely varied opinions and training backgrounds of the surgeons participating in AHPBA, mandate interdisciplinary cohesion and consensus. Without standardization, the authors feel that we risk the well-being of both our patients and our sub-specialty, by producing novice HPB surgeons that are inadequately trained, regardless of their training track of fellowship.
There are two aspects of this study that warrant further study: the response rate was relatively low. The authors plan a more global survey using these data as a baseline for comparison. This will be performed at the time of the IHPBA Congress in 2016. The hope is that this future study will allow some insight into the global perspective on training in HPB surgery.
Conclusions
HPB surgery is a rapidly evolving field with many different routes to train and many different practice patterns. This survey highlights some of the discrepancies in the perception of the case volume required to achieve comfort amongst different training backgrounds and clinical practices. Collaboration and consensus among the governing bodies training HPB surgeons are essential to the future of the field and the complex patients they serve. Establishment of minimum case volumes and the consensus conferences amongst the various governing bodies involved in HPB training is a good next step towards ensuring a promising future for the HPB surgery community in the Americas.
Conflicts of interest
None declared.
Appendix 1
- What is your gender?
- ○Female
- ○Male
- What is your age?
- ○21 to 25
- ○26 to 30
- ○31 to 35
- ○36 to 40
- ○41 to 45
- ○46 to 50
- ○51 to 55
- ○56 to 60
- ○61 to 65
- ○66 to 70
- ○71 to 75
- ○76 or older
- Excluding gallbladders, how many HPB cases do you do (or expect to do upon graduating) in one month?
- ○1–2
- ○2–5
- ○5–10
- ○>10
- What is your current status?
- ○1. Current fellow
- ○2. Matched incoming fellow
- ○3. HPB-interested resident
- ○4. Practicing HPB surgeon > 5 years out of training
- ○5. Practicing HPB surgeon <5 years out of training
- ○Other (please specify)
- Which specialty track best describes your training?
- ○1. HPB Surgery
- ○2. HPB/complex GI
- ○3. HPB/MIS (> 40% cases are MIS)
- ○4. Surgical Oncology
- ○5. Transplant surgery
- ○6. Multiple fellowships (please comment)
- Did you attend the Residents & Fellows' Symposium at the AHPBA meeting?
- ○Yes
- ○No
- If yes please comment on the following:
- What were the strengths of the symposium?
- What were the weaknesses?
- What topics would you like to see addressed in the future?
What other topics would you like included in future symposiums?
- What do you think is the best way to train HPB surgeons?
- ○1. HPB surgery fellowship
- ○2. Surgical oncology fellowship
- ○3. Transplant surgery fellowship
- ○4. Not applicable – we are training too many HPB surgeons already!
- What length of HPB fellowship do you feel provides optimal training?
- ○1. One clinical year with research opportunities
- ○2. Two clinical years with research opportunities
- ○3. One year clinical, one year research
- What length of HPB fellowship would you prefer to attend?
- ○1. One year
- ○2. Two years
- ○3. Don't care, just want to match
How many cases do you think are generally required to be able to safely perform a straightforward Whipple procedure independently?
How many Whipple's did you perform (or do you anticipate performing) during your training?
How many cases do you think are generally required to be able to safely perform a straightforward hemi-liver resection independently?
How many hemi-liver resections did you perform (or do you anticipate performing) during your training?
- On a scale of 1-10, how comfortable are you at performing hemi-liver resection minimally invasively (includes laparoscopic, robotic, hybrid or hand-assist)? (1 - Most uncomfortable to 10 - Most comfortable)
- ○1
- ○2
- ○3
- ○4
- ○5
- ○6
- ○7
- ○8
- ○9
- ○10
- On a scale of 1-10, how comfortable are you at performing whipple MIS (includes laparoscopic, robotic, hybrid or hand-assist)? (1 - Most uncomfortable to 10 - Most comfortable)
- ○1
- ○2
- ○3
- ○4
- ○5
- ○6
- ○7
- ○8
- ○9
- ○10
- The best outcomes are achieved in which of the following settings?
- ○1. Major academic centers
- ○2. High volume private centers
- ○3. Best surgeon has best outcomes – hospital type irrelevant
- ○4. Highest volume center has best outcomes – hospital type irrelevant
- If you are a current trainee, which best describes your current job search situation?
- ○1. Still training – too early to look
- ○2. Actively looking
- ○3. Interviewed at 1-3 placed
- ○4. Interviewed at > 3 places
- ○5. Reviewing contract
- ○6. Contract signed!
- ○7. n/a
- What type of practice do you have/are you interested in?
- ○1. Private practice
- ○2. Hybrid private practice with access to residents
- ○3. HMO or hospital-employed practice
- ○4. Traditional academic setting
- ○5. I will take a job wherever I can get one
- What type of job do you think you can get?
- ○1. Private practice
- ○2. Hybrid private practice with access to residents
- ○3. HMO or hospital-employed practice
- ○4. Traditional academic setting
- ○5. Again, I will take a job wherever I can get one
- Which best reflects your ideal job description?
- ○1. Pure clinical practice
- ○2. Clinical practice with clinical/outcomes research
- ○3. Clinical practice with basic science research
- ○4. Clinical practice with some combination of clinical & basic science research
References
- Scarborough JE, Pietrobon R, Bennett KM, Clary BM, Kuo PC, Tyler DS, et al. Workforce projections for hepato-pancreato-biliary surgery. J Am Coll Surg. 2008;206:678–684. doi: 10.1016/j.jamcollsurg.2007.11.016. [DOI] [PubMed] [Google Scholar]
- Balzano G, Zerbi A, Capretti G, Rocchetti S, Capitanio V, Di Carlo V. Effect of hospital volume on outcome of pancreaticoduodenectomy in Italy. Br J Surg. 2008;95:357–362. doi: 10.1002/bjs.5982. [DOI] [PubMed] [Google Scholar]
- de Wilde RF, Besselink MG, van der Tweel I, de Hingh IH, van Eijck CH, Dejong CH, et al. Impact of nationwide centralization of pancreaticoduodenectomy on hospital mortality. Br J Surg. 2012;99:404–410. doi: 10.1002/bjs.8664. [DOI] [PubMed] [Google Scholar]
- Colavita PD, Tsirline VB, Belyansky I, Swan RZ, Walters AL, Lincourt AE, et al. Regionalization and outcomes of hepato-pancreato-biliary cancer surgery in USA. J Gastrointest Surg. 2014;18:532–541. doi: 10.1007/s11605-014-2454-z. [DOI] [PubMed] [Google Scholar]
- Birkmeyer JD, Finlayson SR, Tosteson AN, Sharp SM, Warshaw AL, Fisher ES. Effect of hospital volume on in-hospital mortality with pancreaticoduodenectomy. Surgery. 1999;125:250–256. [PubMed] [Google Scholar]
- Chamberlain RS, Tichauer M, Klaassen Z, Paragi PR. Complex pancreatic surgery: safety and feasibility in the community setting. J Gastrointest Surg. 2011;15:184–190. doi: 10.1007/s11605-010-1305-9. [DOI] [PubMed] [Google Scholar]
- Swan RZ, Lau KN, Sindram D, Iannitti DA, Martinie JB. Pancreatic resection in a large tertiary care community-based hospital: building a successful pancreatic surgery program. Surg Oncol Clin N Am. 2011;20:487–500. doi: 10.1016/j.soc.2011.01.004. , viii. [DOI] [PubMed] [Google Scholar]
- Sachs TE, Ejaz A, Weiss M, Spolverato G, Ahuja N, Makary MA, et al. Assessing the experience in complex hepatopancreatobiliary surgery among graduating chief residents: is the operative experience enough? Surgery. 2014;156:385–393. doi: 10.1016/j.surg.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helling TS, Khandelwal A. The challenges of resident training in complex hepatic, pancreatic, and biliary procedures. J Gastrointest Surg. 2008;12:153–158. doi: 10.1007/s11605-007-0378-6. [DOI] [PubMed] [Google Scholar]
- American Society of Transplant Surgeons Accredited Abdominal Fellowship Training Programs. Available at http://asts.impakadvance.com/members_online/members/fellowship_directory.asp?sort=s (last accessed 1 February 2015)
- Surgical Oncology Fellowship Training Programs . Available at http://www.surgonc.org/training-fellows/fellows-education/surgical-oncology/program-list (last accessed 1 February 2015)
- Americas Hepato-Pancreato-Biliary Association HPB Fellowship Training Programs. Available at http://www.ahpba.org/assets/documents/2014_fellowships.pdf (last accessed 1 February 2015)
- 2014 Training in HPB Surgery Consensus Conference – Available at http://www.ahpba.org/ahpba-sponsored-consensus-conferences (last accessed 1 January 2015)
- Ali N, O'Rourke C, El-Hayek K, Chalikonda S, Jeyarajah DR, Walsh RM. Estimating the need for hepato-pancreatico-biliary surgeons in the USA. HPB. 2015;17:352–356. doi: 10.1111/hpb.12370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant J. Learning needs assessment: assessing the need. BMJ. 2002;324:156–159. doi: 10.1136/bmj.324.7330.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner SG, Connor S, Christophi C, Azodo IA, Kent T, Pier D, et al. Development of an international online learning platform for hepatopancreatobiliary surgical training: a needs assessment. HPB. 2014;16:1127–1132. doi: 10.1111/hpb.12289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebel M. Multivariate calibration of classifier scores into the probability space, Dissertation, Universität Dortmund, 2009.