Abstract
Objectives
We compared diagnostic accuracy of conventional troponin/traditional coronary artery disease (CAD) assessment and highly sensitive troponin (hsTn) I/advanced CAD assessment for acute coronary syndrome (ACS) during the index hospitalization.
Background
HsTn I and advanced assessment of CAD using coronary computed tomography angiography (CTA) are promising candidates to improve the accuracy of emergency department (ED) evaluation of patients with suspected ACS.
Methods
We performed an observational cohort study in patients with suspected ACS enrolled in the ROMICAT II trial and randomized to coronary CTA who also had hsTn I measurement at the time of the ED presentation. We assessed coronary CTA for traditional (no CAD, non-obstructive CAD, ≥50% stenosis) and advanced features of CAD (≥50% stenosis, high-risk plaque features: positive remodeling, low <30 Hounsfield Units plaque, napkin ring sign, spotty calcium).
Results
Of 160 patients (mean age: 53±8 years, 40% women) 10.6% were diagnosed with ACS. The ACS rate in patients with HsTn I below the limit of detection (n=9, 5.6%), intermediate (n=139, 86.9%), and above the 99th percentile (n=12, 7.5%) was 0%, 8.6%, and 58.3%, respectively. Absence of ≥50% stenosis and high-risk plaque ruled out ACS in patients with intermediate hsTn I (n=87, 54.4%; ACS rate 0%), while patients with both ≥50% stenosis and high-risk plaque were at high risk (n=13, 8.1%; ACS rate 69.2%) and patients with either ≥50% stenosis or high-risk plaque were at intermediate risk for ACS (n=39, 24.4%; ACS rate 7.7%). HsTn I/advanced coronary CTA assessment significantly improved the diagnostic accuracy for ACS as compared to conventional troponin/traditional coronary CTA (AUC 0.84, 95%CI 0.80-0.88 vs. 0.74, 95%CI 0.70-0.78; p<0.001).
Conclusions
HsTn I at the time of presentation followed by early advanced coronary CTA assessment improves the risk stratification and diagnostic accuracy for ACS as compared to conventional troponin and traditional coronary CTA assessment. (Multicenter Study to Rule Out Myocardial Infarction/Ischemia by Cardiac Computed Tomography [ROMICAT-II]; NCT01084239)
Keywords: highly-sensitive troponin, coronary CT angiography, coronary plaque, acute coronary syndrome, risk stratification, emergency department
Introduction
Highly sensitive troponin (hsTn) assays and coronary computed tomography angiography (CTA) are promising candidates to improve diagnostic accuracy in patients undergoing evaluation for suspected acute coronary syndrome (ACS) in the emergency department (ED).(1-7) Multiple studies have shown that HsTn assays have increased sensitivity for the detection of ACS and decreased time to assay positivity compared to conventional troponin.(1-4) These assay characteristics suggest a potential for faster and more efficient evaluation of patients presenting to the ED with symptoms suggestive of ACS. Several recent studies suggested that even a single very low measurement of hsTn at the time of ED presentation can rule out MI safely.(8-10) Further, increasing levels of hsTn are associated with coronary artery disease (CAD) and myocardial perfusion defects, and have prognostic value beyond the acute care episode.(11, 12) Three large randomized trials have demonstrated that coronary CTA as compared to standard of care, including serial conventional troponin and functional testing to provoke myocardial ischemia, decreased the time to diagnosis and allowed for earlier discharge from the ED.(5-7) Recent data suggest that detection of high-risk coronary plaque features [defined as positive remodeling, low <30 Hounsfield Units (HU) plaque, napkin ring sign, or spotty calcium) is independent and incremental to significant coronary stenosis for diagnosis of ACS.(13) The exclusion of high-risk plaque may help to decrease downstream testing (e.g. additional stress testing and invasive coronary angiography). The increase in downstream testing was observed in studies using the traditional assessment of coronary CTA for stenosis.(14-16)
Hence, there are expectations that a combination of advanced coronary CTA with hsTn may increase accuracy in the management of patients presenting to the ED with suspected ACS. We designed an observational cohort study nested in the ROMICAT II trial. We determined whether combined assessment of HsTn I and advanced coronary CTA for high-risk plaque improves accuracy of ACS risk classification as compared to conventional troponins and traditional coronary CTA assessment for stenosis.
Methods
Patient population
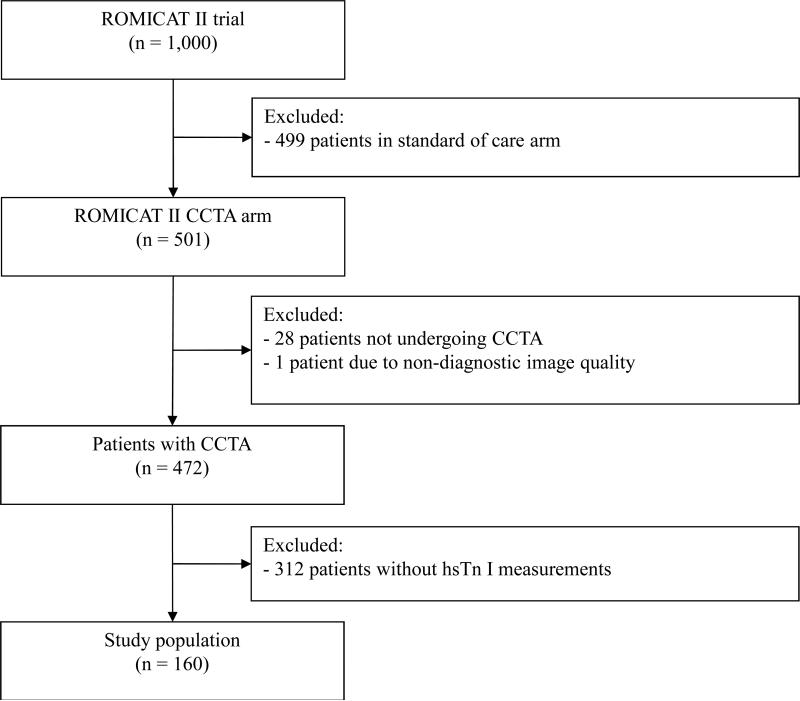
The Rule Out Myocardial Infarction/Ischemia Using Computer Assisted Tomography (ROMICAT) II trial randomized patients presenting to the ED with suggestive of ACS but without ischemic electrocardiographic changes and with negative conventional troponins (see supplemental Table 1 for the conventional troponin assays used in the study).(7) This ancillary study was designed as a nested observational cohort study in patients who were randomized to coronary CTA and consented to blood sampling for hsTn I at the time of ED presentation (Figure 1). All study participants provided written consent for participation in ROMICAT II. The local institutional review boards approved the study. A detailed description of the patient population, including the inclusion and exclusion criteria, was reported previously.(7)
Figure 1. Study population enrollment, exclusion and inclusion.
CONSORT diagram shows the inclusion and exclusion of patients resulting in the final study population of 160 patients.
Blood samples and hsTn I testing
Blood was collected into tubes containing ethylenediamintetraacetic acid at baseline and immediately processed and frozen at −80 degrees centigrade until the completion of the study. The samples were obtained at the time of presentation. Additional 2nd sample was obtained at 90-115 minutes in 140 patients and 3rd sample was obtained at 210-300 minutes in 105 patients. The blood was then analyzed in a blinded fashion using a preclinical highly sensitive method for detecting troponin I (hsVista, Siemens Diagnostics, Newark, DE).(1) The limit of detection and 99th percentile values for hsTn I were 0.5 pg/L and 49 pg/L, respectively.(17) We categorized patients into three groups: below the limit of detection (LOD) for the assay (below LOD group), between the LOD and the 99th percentile (intermediate group), and above the 99th percentile (> 99th percentile group).
Coronary CTA analysis
Coronary CTA images were acquired using 64-row or newer scanner generations using either retrospectively ECG-gated or prospectively ECG-triggered protocols.(7) Three readers with at least 5 years of experience in coronary CTA and level III training performed the analysis on a dedicated cardiac workstation (TeraRecon, Foster City, CA). The coronary CTA analysis was performed on a per coronary segment basis using the model of the Society of Cardiovascular Computed Tomography.(18)
The traditional assessment of coronary CTA was performed in all evaluable coronary segments. Each segment was assessed for the presence of coronary stenosis and plaque. The severity of stenosis was categorized as: 0% = no stenosis, 1-49% = non-obstructive CAD, ≥50% = significant CAD.
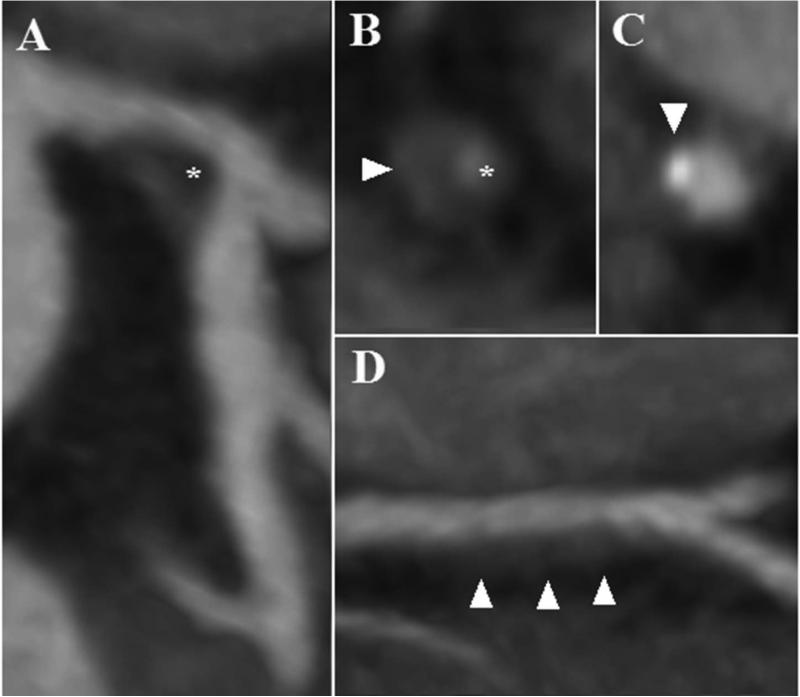
The advanced assessment for high-risk coronary plaque was performed in all coronary segments with plaque. High-risk plaque was defined as the presence of at least one of the following features: positive remodeling (remodeling index >1.1), presence of plaque with low CT attenuation of <30 HU plaque, napkin ring sign and spotty calcium (Figure 2).(13)
Figure 2. High-risk plaque features as detected by coronary CTA.
Panel A – low CT attenuation <30 HU plaque (asterisk) in the distal left main coronary artery. Panel B – cross-sectional view of the vessel with non-calcified plaque demonstrating napkin ring sign with the central low HU area next to the lumen (asterisk) surrounded by a peripheral rim of higher CT attenuation (arrowhead). Panel C – cross-sectional view of a partially calcified plaque with a spotty calcification (arrowhead). Panel D – non-calcified plaque with positive remodeling (arrowheads).
Definition and adjudication of acute coronary syndrome
The primary outcome was ACS during the index hospitalization. Acute coronary syndrome was defined as acute myocardial infarction or unstable angina pectoris according to the American College of Cardiology/American Heart Association Guidelines.(19) This endpoint was predefined and adjudicated by an external, independent clinical end-points committee (Supplemental Material).(7) The measurements of conventional cardiac troponin at each site were available for adjudication (supplemental Table 1 summarizes cut off values for each site). The results of hsTn I and advanced coronary CTA analysis were blinded to the investigators performing the adjudication.
Statistical methods
All statistical analyses were performed using Stata 13.1 (StataCorp LP, College Station, Texas). Continuous data are presented as mean±standard deviation and categorical variables were presented as numbers and percentages. Comparisons between groups were performed with the use of an independent sample t-test and ANOVA for continuous variables, and the Fisher's exact test for categorical variables. For sensitivity, specificity, positive and negative predictive value, 95% confidence intervals (CI) were calculated using exact binomial confidence intervals. For the traditional coronary CTA assessment the test was considered positive if there was any ≥50% stenosis or plaque. For the combined hsTn I and advanced coronary CTA assessment, the test was considered positive if at least one of the three factors was present: hsTn I result was above the 99th percentile at the time of presentation, ≥50% stenosis or high-risk plaque present on coronary CTA. Areas under the receiver operating characteristics curve (AUC) were compared using the DeLong algorithm.(20) The net reclassification index was calculated using method described by Pencina et al.(21) For all analyses, a 2-tailed p value <0.05 was required to reject the null hypothesis.
Results
Patient population
Of 501 patients randomized to coronary CTA in the ROMICAT II trial, 472 underwent coronary CTA and had diagnostic image quality. Of those, 160 agreed to participate in blood collection and were included in the nested observational cohort study (Figure 1). The baseline characteristics of the study population are summarized in Table 1. The mean age was 52.7±7.6 years. ACS during the index hospitalization was diagnosed in 19 (10.6%) patients (myocardial infarction n=2, unstable angina pectoris n=17). There were no significant differences in baseline demographics, risk factors and outcomes between patients who agreed to blood collection and the overall cohort of patients randomized to coronary CTA in the ROMICAT II trial (Supplemental Table 2).
Table 1.
Baseline patient characteristics
| Total (n=160) | hsTn I below the limit of detection (n=9) | hsTn I intermediate (n=139) | hsTn I above the 99th percentile (n=12) | p value | |
|---|---|---|---|---|---|
| Mean age (years) | 52.7 ± 7.6 | 47.4 ± 5.7 | 53.0 ± 7.5 | 53.8 ± 8.7 | 0.091 |
| Female gender (%) | 64 (40.0) | 7 (77.8) | 56 (40.3) | 1 (8.3) | 0.004 |
| Cardiovascular risk factors (%) | |||||
| Hypertension | 83 (51.9) | 1 (11.1) | 74 (53.2) | 8 (66.7) | 0.024 |
| Diabetes mellitus | 21 (13.1) | 0 (0) | 20 (14.4) | 1 (8.3) | 0.752 |
| Dyslipidemia | 71 (44.4) | 2 (22.2) | 63 (45.3) | 6 (50.0) | 0.409 |
| Former or current smoker | 85 (53.1) | 6 (66.7) | 71 (51.1) | 8 (66.7) | 0.434 |
| Family history of premature CAD | 50 (31.3) | 3 (33.3) | 43 (30.9) | 4 (33.3) | 1.000 |
| Acute coronary syndrome (%) | |||||
| Myocardial infarction | 2 (1.3) | 0 (0) | 0 (0) | 2 (16.7) | 0.008 |
| Unstable angina pectoris | 17 (10.6) | 0 (0) | 12 (8.6) | 5 (41.7) | 0.007 |
CAD = coronary artery disease, hsTn = highly-sensitive troponin
Conventional troponin and traditional coronary CTA and ACS
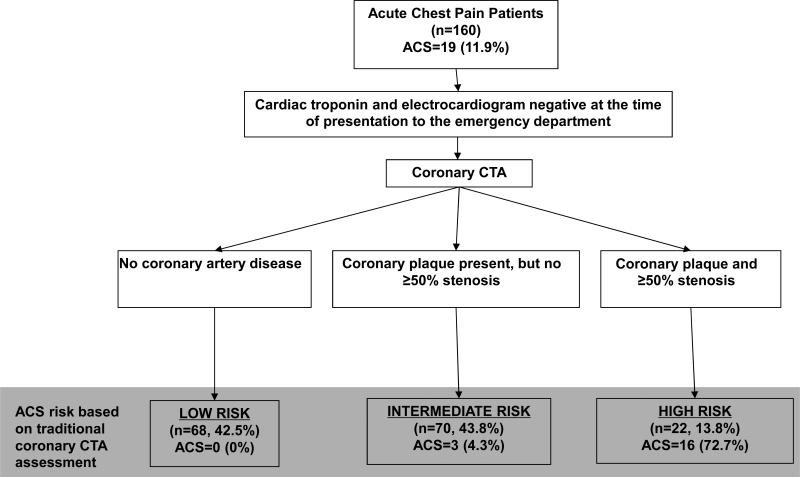
By the ROMICAT II protocol conventional troponin at the time of presentation to the ED was normal. Based on traditional coronary CTA assessment 42.5% of patients (n=68/160) had no CAD, 43.8% (n=70/160) had non-obstructive CAD, and 13.8% (n=22/160) had significant CAD (Table 2). Reflecting clinical practice, patients with normal conventional troponin at the time of presentation and no CAD on coronary CTA were stratified as low risk (ACS rate: 0%) and patients who had ≥50% stenosis on coronary CTA were stratified as high risk for ACS (ACS rate: 72.7%). However, nearly half of the patients remained at intermediate risk having non-obstructive CAD (ACS rate: 4.3%) (Figure 3).
Table 2.
Coronary CTA characteristics of CAD and high-risk coronary plaque stratified by the levels of hsTn I.
| Total (n=160) | hsTn I below the limit of detection (n= 9) | hsTn I intermediate (n=139) | hsTn I above the 99th percentile (n=12) | p value | |
|---|---|---|---|---|---|
| Traditional CAD assessment (%) | |||||
| No CAD (0% stenosis) | 68 (42.5) | 6 (66.7) | 60 (43.2) | 2 (16.7) | 0.066 |
| Non-obstructive CAD (1-49% stenosis) | 70 (43.8) | 3 (33.3) | 65 (46.5) | 2 (16.7) | 0.106 |
| Significant CAD (≥50% stenosis) | 22 (13.8) | 0 (0) | 14 (10.1) | 8 (66.7) | <0.001 |
| Advanced assessment of coronary CTA (%) | |||||
| Any high-risk plaque | 61 (38.1) | 0 (0) | 51 (36.7) | 10 (83.3) | <0.001 |
| Positive remodeling | 26 (16.3) | 0 (0.0) | 20 (14.4) | 6 (50.0) | 0.006 |
| Low <30 HU plaque | 20 (12.5) | 0 (0.0) | 15 (10.8) | 5 (41.7) | 0.010 |
| Napkin-ring sign | 14 (8.8) | 0 (0) | 10 (7.2) | 4 (33.3) | 0.022 |
| Spotty calcium | 56 (35.0) | 0 (0.0) | 46 (33.1) | 10 (83.3) | <0.001 |
CAD = coronary artery disease, hsTn = highly-sensitive troponin, HU = Hounsfield units
Figure 3. Traditional coronary CTA assessment and ACS in the ROMICAT II trial.
Flow diagram depicts the risk stratification based on the conventional troponin followed by the traditional assessment of coronary CTA for the presence of coronary atherosclerotic plaque and ≥50% stenosis.
Association of HsTn I and ACS
In contrast to conventional troponins, hsTn I permitted immediate risk stratification at the time of ED presentation. Overall, 9 patients (5.6%) had hsTn I below the LOD and 12 (7.5%) had hsTn I above the 99th percentile. The majority of patients had intermediate hsTn I levels (n=139, 86.9%) (Table 1). The prevalence of ACS was 0% (n=0/9) when hsTn I was below the LOD, 8.6% (n=12/139) in the intermediate hsTn I group and 58.3% (n=7/12) in patients with hsTn I above the 99th percentile. All events in the intermediate group were adjudicated as unstable angina pectoris. Hence, using hsTn I, ACS could be ruled out safely in a small group of patients, obviating the need for subsequent coronary CTA.
The addition of the 2nd and 3rd hsTn I did not allow for improvement of risk stratification (data not shown).
Association of high-risk plaque and ACS
At least one high-risk plaque feature was present in all patients with ACS. Conversely, only 30.7% of patients without ACS had high-risk plaque. The prevalence of ACS in the coronary CTA strata of no high-risk plaque and no ≥50% stenosis, either high-risk plaque or ≥50% stenosis, and both high-risk plaque and ≥50% stenosis was 0%, 7.7%, and 69.2%, respectively. Among patients with hsTn I above the 99th percentile, 66.7% of patients had ≥50% stenosis and 88.3% of patients had high-risk plaque.
Association of CAD and high-risk plaque with hsTn I
Association between the hsTn I strata and presence, extent and composition of CAD are shown in Table 2. Significant associations were observed for all high-risk plaque features and for significant CAD (≥50% stenosis) (p<0.01 for each parameter), but not for non-obstructive CAD, indicating that further characterization of non-obstructive CAD for high-risk plaque features is meaningful. None of the patients with hsTn I below the LOD had ≥50% stenosis or high-risk plaque on coronary CTA, while 33.3% of patients had non-obstructive CAD.
CAD characteristics and hsTn I levels in patients with intermediated hsTn I
In a sub-analysis, we compared CAD characteristics and hsTn I levels in patients with intermediated levels of hsTn (Table 3). Patients with ACS had higher prevalence of ≥50% stenosis and high-risk plaque. The levels of hsTn I were not different between those with and without ACS.
Table 3.
Coronary CTA characteristics and hsTn I levels of patients with intermediate hsTn I stratified according to the diagnosis of acute coronary syndrome
| Total (n=139) | No ACS (n=127) | ACS (n=12) | p value | |
|---|---|---|---|---|
| Traditional CAD assessment (%) | ||||
| No CAD (0% stenosis) | 60 (43.2) | 60 (47.2) | 0 (0.0) | 0.001 |
| Non-obstructive CAD (1-49% stenosis) | 65 (46.8) | 62 (48.8) | 3 (25.0) | 0.139 |
| Significant CAD (≥50% stenosis) | 14 (10.1) | 5 (3.9) | 9 (75.0) | <0.001 |
| Advanced assessment of coronary CTA (%) | ||||
| Any high-risk plaque | 51 (36.7) | 39 (30.7) | 12 (100.0) | <0.001 |
| Positive remodeling | 20 (14.4) | 11 (8.7) | 9 (75.0) | <0.001 |
| Low <30 HU plaque | 15 (10.8) | 9 (7.1) | 6 (50.0) | <0.001 |
| Napkin-ring sign | 10 (7.2) | 5 (3.9) | 5 (41.7) | <0.001 |
| Spotty calcium | 46 (33.1) | 34 (26.8) | 12 (100.0) | <0.001 |
| HsTn I (ng/L) | 2.4 (1.3-4.7) | 2.3 (1.4-4.6) | 3.5 (1.1-6.1) | 0.696 |
CAD = coronary artery disease, hsTn = highly-sensitive troponin, HU = Hounsfield units, ACS = acute coronary syndrome
Comparison of the diagnostic accuracy of conventional troponin and traditional coronary CTA versus hsTnI and advanced coronary CTA
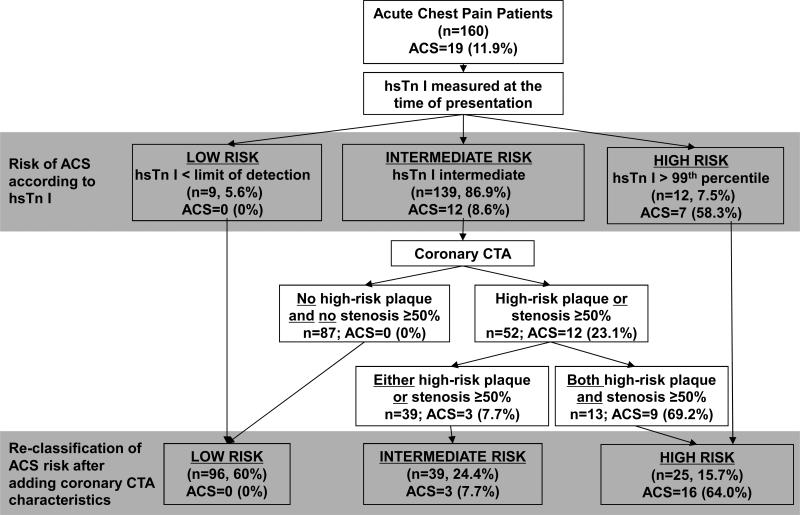
A first hsTn I at the time of presentation followed by early coronary CTA with advanced assessment for high-risk plaque improved the accuracy of risk stratification as compared to conventional troponin and traditional CTA assessment (Figure 4).
Figure 4. Combined HsTn I and advanced coronary CTA assessment and ACS in the ROMICAT II trial.
Flow diagram depicts the improvement of ACS risk stratification using hsTn I at the time of ED presentation. Further improvement of the risk stratification can be achieved with advanced assessment of coronary CTA for high-risk plaque.
Based on the first hsTn I, coronary CTA would not be needed in 13.1% of patients (n=21): 9 patients (5.6%) with hsTn I below the LOD (ACS rate: 0%) and 12 patients (7.5%) with hsTn I above the 99th percentile (ACS rate: 58.3%). In the remaining 139 patients with intermediate hsTn I, the absence of both high-risk plaque and ≥50% stenosis on coronary CTA excluded ACS in 87 patients (no CAD in 60 patients, non-obstructive CAD in 27 patients). Among the remaining 52 patients, those with either high-risk plaque or ≥50% stenosis represented an intermediate risk group (n=39; ACS rate: 7.7%), and those who had both high-risk plaque and ≥50% stenosis (n=13; ACS rate: 69.2%) represented a high-risk group. Hence, coronary CTA allowed for reclassification of the majority (72%, n=100/139) of patients in the intermediate hsTn I group for ACS risk (Table 4). In 19 patients with ACS, 9 patients were upgraded to high risk for ACS, and no patient was downgraded to low risk for ACS when using advanced coronary CTA results for reclassification. The net gain in reclassification proportion for patients with ACS was 0.47 (CI 95% 0.16-0.78; p=0.003). The net gain in reclassification proportion for subjects who did not have ACS was 0.59 (CI 95%: 0.46-0.72; p<0.001); 87 out of 141 patients were reclassified downward and 4 out of 141 were reclassified upward. The net reclassification index was thus calculated at 1.06 (CI 95%: 0.73-1.40; p <0.001).
Table 4.
Re-classification of ACS risk based on hsTn I at the time of presentation followed by advanced coronary CTA assessment including high risk plaque
| Re-classification of ACS risk by advanced coronary CTA assessment | |||||
|---|---|---|---|---|---|
| Low risk | Intermediate risk | High risk | Total | ||
| Risk of ACS based on hsTn I at the time of presentation | Low risk | 9 | 0 | 0 | 9 |
| Intermediate risk | 87 | 39 | 13 | 139 | |
| High risk | 0 | 0 | 12 | 12 | |
| Total | 96 | 39 | 25 | 160 | |
ACS = acute coronary syndrome, hsTn = highly-sensitive troponin, CTA = computed tomography angiography
The strategy of combined hsTn I and coronary CTA with assessment for high-risk plaque as compared to conventional troponin combined with traditional coronary CTA increased the number of patients in whom ACS could be ruled out from 68 (42.5%) to 96 (60%) and the number of patients at high risk for ACS from 22 (13.8%) to 25 (15.7%), while the group at intermediate risk decreased from 70 (43.8%) to 39 (24.4%) patients. Overall, the additional information provided by hsTn I and high-risk plaque increased the number of patients categorized into low or high-risk category from 82 (51.3%) to 121 (75.6%).
The sensitivity and negative predictive value of combined hsTn I and advanced coronary CTA assessment for ACS were maintained at 100% (similar to conventional troponin and traditional coronary CTA assessment) while the specificity improved from 48.2 to 68.1% (Table 5). The combined assessment of hsTnI and advanced coronary CTA for high-risk plaque (AUC 0.84, 95% CI 0.80-0.88) significantly improved the diagnostic performance for ACS as compared to traditional coronary CTA (AUC 0.74, 95% 0.70-0.78; p<0.001).
Table 5.
Diagnostic accuracy for ACS of conventional troponin and traditional coronary CTA assessment versus hsTn I and advanced coronary CTA
| Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | AUC (95% CI) | |
|---|---|---|---|---|---|
| Conventional troponin and traditional CTA | 100.0% (82.4-100.0) | 48.2% (39.7-56.8) | 20.7% (12.9-30.4) | 100.0% (94.7-100.0) | 0.74 (0.70-0.78) |
| HsTn I and advanced CTA | 100.0% (82.4-100.0) | 68.1% (59.7-75.7) | 29.7% (18.9-42.4) | 100.0% (96.2-100.0) | 0.84 (0.80-0.88) |
PPV – positive predictive value, NPV – negative predictive value, AUC – area under the curve, 95% CI – 95% confidence interval, ACS – acute coronary syndrome, hsTn – highly-sensitive troponin
Discussion
We demonstrated that hsTn I at the time of the ED presentation followed by early coronary CTA with assessment for stenosis and high-risk plaque improved the diagnostic accuracy for ACS in patients with suspected ACS as compared to conventional troponin and traditional coronary CTA assessment. This was based on 1) the ability of the first hsTn I at the time of presentation to stratify 13.1% into high or low risk ACS groups, 2) the reclassification of 71.9% of those with intermediate hsTn I by using additional information from the coronary CTA assessment, thereby decreasing the fraction of patients remaining at intermediate risk for ACS from 43.8% to 24.4%, 3) the improvement in specificity for ACS in those with intermediate hsTn I levels through assessment of high risk plaque (from 48.2 to 68.1%) while sensitivity and negative predictive value for ACS were maintained at 100%. Overall, hsTn I at the time of ED presentation followed by early coronary CTA with assessment for stenosis and high-risk plaque significantly improved discriminatory ability for ACS (AUC: 0.74 to 0.84; p<0.001).
HsTn assays in the assessment of patients with acute chest pain
HsTn assays increase the sensitivity for the detection of smaller amounts of myocardial injury and also decrease the time to assay positivity (1-4) There is growing evidence that hsTn below the LOD measured at the time of presentation has a negative predictive value of >99% for myocardial infarction, suggesting that it could serve as an early triage tool.(1-4, 8-10) The triage effectiveness of hsTn using the LOD threshold can be affected by the prevalence of hsTn below the LOD in a population. Prior studies suggest that between 10 and 15% of patients with suspected ACS have hsTn I below the LOD.(1-4, 10) We found a slightly lower fraction of 6%, which likely represents the extremely high analytical sensitivity of this pre-commercial hsTn I method. None of the patients with hsTn I below the LOD had myocardial infarction or unstable angina pectoris suggesting that these patients do not need to undergo coronary CTA and a direct discharge from the ED can be considered. While a small number of subjects, the importance of this finding cannot be underestimated. Further improvement in efficiency of ACS diagnosis may be possible by combining hsTn and clinical risk assessment, and by measuring short-term dynamic changes of hsTn.(8-10, 22) This may lead to further decrease in the number of patients requiring additional testing, including imaging. In addition, reduced need for coronary CTA imaging can be achieved in patients with hsTn I above the 99th percentile at the time of presentation who are at high risk for ACS.
However, the major diagnostic challenge is the large group of patients with intermediate levels of hsTn. In a recent study, these patients had non-negligible rates of ACS (8.3%) during the index hospitalization and also significantly higher rate of myocardial infarction in the first 30 days after ED discharge versus patients with hsTn T below the LOD (3.08 vs. 0.17%).(23) Our results confirm these observations (ACS rate: 8.6%) and suggest that patients with intermediate hsTn I at the time of presentation require further evaluation and cannot be safely discharged home.
Serial measurements of hsTn I improved the detection and exclusion of ACS in previous studies.(22, 24) In our study, the addition of 2nd and 3rd hsTn I measurement at approximately 3 and 6 hours after the presentations did not improve ACS risk classification. However, serial hsTn measurements were not available in all patients, potentially including bias to our observations. Further studies will be needed to explore whether serial hsTn measurements can help in the management of patients, especially in patients with CAD and intermediate stenosis on coronary CTA.
Incremental value of advanced coronary CTA assessment
We demonstrated the incremental value of coronary CTA to accurately stratify patients with intermediate hsTn I, who are at intermediate risk of ACS. We reclassified 71.9% of patients with intermediate hsTn I using coronary CTA and decreased the fraction of patients remaining at intermediate risk for ACS after both assessments from 43.8% to 24.4%. This also improved specificity for ACS from 48.2 to 68.1% as compared to traditional coronary CTA and was achieved, because the presence of high-risk plaque and ≥50% stenosis carried a very high-risk of ACS (9 out of 13 patients) in the group with intermediate hsTn I. We demonstrated that patients with non-obstructive CAD, but no high-risk plaque did not develop ACS and hence, the fraction of low risk patients increased from 42.5% to 60%, while maintaining sensitivity and negative predictive value for ACS at 100%. These findings resulted in a significant improvement in the discriminatory ability for ACS (AUC: 0.74 to 0.84; P>0.001).
The patients with intermediate hsTn I and either high-risk plaque or ≥50% stenosis remained at intermediate risk of ACS (3 out of 39 patients). All 3 patients with ACS had high-risk plaque, but none had ≥50% stenosis. These findings are consistent with invasive angiographic studies demonstrating a minority of patients (12-14%) who develop ACS in the absence of hemodynamically significant stenosis.(25, 26)
Implications for management of acute chest pain patients
Although this is an observational study, the results carry important implications for patient management. We found a small but important number of patients with hsTn I below the LOD at the time of ED might be rapidly triaged home without further testing. Further studies are warranted to determine whether the fraction of patients to be potentially immediately discharged without coronary CTA can be improved by including risk factors and clinical characteristics of chest pain and whether this fraction is stable across different hsTn assays. After coronary CTA, 60% of patients, including those with hsTn I below the LOD and those with intermediated hsTn I, but no ≥50% coronary stenosis and no high-risk plaque on coronary CTA, could be candidates for immediate discharge. Patients with hsTn I above the 99th percentile at the time of presentation are at high risk for ACS and appropriate guideline recommended therapies, such as dual antiplatelet therapy, high-dose statin, anticoagulation, and early invasive strategy could be considered without coronary CTA. Similar guideline directed ACS therapies could be considered after coronary CTA demonstrates both coronary stenosis and high-risk plaque in patients with intermediate hsTn I as they have high-risk of ACS. After the first hsTn I and early coronary CTA, about one quarter of patients remain at intermediate risk for ACS, for whom observation could be considered, including serial troponin measurements, aspirin, statin and a stress test.
Limitations
The measurements of hsTn I were available only in a subpopulation of patients in ROMICAT II trial. This limited our sample size and could introduce a bias. However, the baseline characteristics of patients with hsTn I measurements were not significantly different from the entire population of patients in the coronary CTA arm of the ROMICAT II trial. We only used one hsTn assay. The LOD, sensitivity and specificity of hsTn assays vary and thus could affect the performance of the test. Our results might not be generalizable to other hsTn assays. The strategy of hsTn I at the time of presentation with early coronary CTA was not predefined in the ROMICAT II trial and no actual ED disposition decisions were made based on these results. As such, our data should be interpreted with caution and are mostly hypothesis generating. The interpretation of coronary CTA images was performed in the setting of a core lab, by experienced readers and with unlimited time for interpretation. Further prospective investigations will be required to determine whether clinical coronary CTA readers can reproduce the results and whether coronary CTA assessment of high-risk plaque features can be implemented into clinical workflow. Unstable angina pectoris is a clinical diagnosis supported by more objective evidence on advanced cardiac testing and remains a challenge for clinicians and in the setting of clinical trials. However, in the ROMICAT II trial, an independent clinical end-points committee provided a rigorous high-quality adjudication of potential unstable angina pectoris according to predefined criteria.
Conclusions
Combined hsTn I at the time of presentation followed by early coronary CTA with the assessment for both stenosis and high-risk plaque improved the diagnostic accuracy for ACS as compared to conventional troponin and traditional assessment of coronary CTA. This has the potential to improve risk stratification of ED patients presenting with symptoms suggestive of ACS.
Supplementary Material
Clinical Perspectives.
Competency in Patient Care and Procedural Skills
Our results provide new insights into the accuracy of a management strategy for patients presenting to the ED with suspected ACS. Combined hsTn I at the time of presentation followed by early coronary CTA with the assessment for both stenosis and high-risk plaque improved the diagnostic accuracy for ACS as compared to conventional troponin and traditional assessment of coronary CTA for stenosis. The education of referring providers will be critical to assure that the results of hsTn and advanced coronary CTA are appropriately interpreted and incorporated in the clinical decision-making.
Translational Outlook
This was an observational study and no actual clinical decisions were made based on the results of hsTn I and advanced coronary CTA assessment. The use of combined hsTn I and advanced assessment of coronary CTA should be tested in a clinical trial, in which clinical decisions and care will be guided by the test results.
Acknowledgments
Disclosures: ROMICAT II Support NIH U01HL092040 and U01HL092022, ACRIN
Ferencik: Research Grant/Significant: American Heart Association Fellow to Faculty Award 13FTF16450001
Truong: Research Grant/Significant: NIH/NHLBI K23HL098370 and L30HL093896, St. Jude Medical, American College of Radiology Imaging Network, and Duke Clinical Research
Peacock: Research Grant/Significant: Abbott, Alere, Banyan, Cardiorentis, Portola, Roche, The Medicine's Company; Ownership Interest/Significant: Comprehensive Research Associates LLC, Emergencies in Medicine LLC; Consultant/Advisory Board/Modest: BG Medicine, Beckman, Boehringer-Ingelheim, Instrument Labs, Prevencio, The Medicine's Company, ZS Pharma; Consultant/Advisory Board/Significant: Alere, Cardiorentis, Janssen
Nagurney: Research Grant/Significant: Alere/Biosite, Brahms Ltd/Thermo-Fisher, Nanosphere; Consultant/Advisory/Significant: Board CardioDx
Januzzi: Research Grant/Significant: Siemens, Thermo Fisher, Singulex; Consultant/Advisory Board/Significant: Critical Diagnostics, Sphingotec, Roche
Hoffmann: Research Grant/Significant: NIH U01HL092040, U01HL092022, Siemens Medical Solutions, Heart Flow Inc; Consultant/Advisory Board/Significant: Heart Flow
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclaimer: The content of this manuscript is solely the responsibility of the authors and does not necessarily reflect the views of the National Institutes of Health or the Department of Health and Human Services
References
- 1.Apple FS, Collinson PO, IFCC Task Force on Clinical Applications of Cardiac Biomarkers Analytical characteristics of high-sensitivity cardiac troponin assays. Clin. Chem. 2012;58:54–61. doi: 10.1373/clinchem.2011.165795. [DOI] [PubMed] [Google Scholar]
- 2.Reichlin T, Hochholzer W, Bassetti S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361:858–867. doi: 10.1056/NEJMoa0900428. [DOI] [PubMed] [Google Scholar]
- 3.Keller T, Zeller T, Peetz D, et al. Sensitive troponin I assay in early diagnosis of acute myocardial infarction. N Engl J Med. 2009;361:868–877. doi: 10.1056/NEJMoa0903515. [DOI] [PubMed] [Google Scholar]
- 4.Giannitsis E, Kurz K, Hallermayer K, Jarausch J, Jaffe AS, Katus HA. Analytical validation of a high-sensitivity cardiac troponin T assay. Clin. Chem. 2010;56:254–261. doi: 10.1373/clinchem.2009.132654. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein JA, Chinnaiyan KM, Abidov A, et al. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) Trial. J Am Coll Cardiol. 2011;58:1414–1422. doi: 10.1016/j.jacc.2011.03.068. [DOI] [PubMed] [Google Scholar]
- 6.Litt HI, Gatsonis C, Snyder B, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med. 2012;366:1393–1403. doi: 10.1056/NEJMoa1201163. [DOI] [PubMed] [Google Scholar]
- 7.Hoffmann U, Truong QA, Schoenfeld DA, et al. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012;367:299–308. doi: 10.1056/NEJMoa1201161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Body R, Carley S, McDowell G, et al. Rapid exclusion of acute myocardial infarction in patients with undetectable troponin using a high-sensitivity assay. J Am Coll Cardiol. 2011;58:1332–1339. doi: 10.1016/j.jacc.2011.06.026. [DOI] [PubMed] [Google Scholar]
- 9.Reichlin T, Schindler C, Drexler B, et al. One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Arch Intern Med. 2012;172:1211–1218. doi: 10.1001/archinternmed.2012.3698. [DOI] [PubMed] [Google Scholar]
- 10.Rubini Giménez M, Hoeller R, Reichlin T, et al. Rapid rule out of acute myocardial infarction using undetectable levels of high-sensitivity cardiac troponin. Int. J. Cardiol. 2013;168:3896–3901. doi: 10.1016/j.ijcard.2013.06.049. [DOI] [PubMed] [Google Scholar]
- 11.Schlett CL, Truong QA, Ahmed W, et al. High-sensitivity troponin T and C-reactive protein to identify patients without cardiac structural and functional abnormalities as assessed by cardiac CT and SPECT imaging: can biomarkers predict cardiac health? Int J Cardiovasc Imaging. 2013;29:865–873. doi: 10.1007/s10554-012-0164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Lemos JA, Drazner MH, Omland T, et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA. 2010;304:2503–2512. doi: 10.1001/jama.2010.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Puchner SB, Liu T, Mayrhofer T, et al. High-risk plaque detected on coronary CT angiography predicts acute coronary syndromes independent of significant stenosis in acute chest pain: results from the ROMICAT-II trial. J Am Coll Cardiol. 2014;64:684–692. doi: 10.1016/j.jacc.2014.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ladapo JA, Jaffer FA, Hoffmann U, et al. Clinical outcomes and cost-effectiveness of coronary computed tomography angiography in the evaluation of patients with chest pain. J Am Coll Cardiol. 2009;54:2409–2422. doi: 10.1016/j.jacc.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 15.Shreibati JB, Baker LC, Hlatky MA. Association of coronary CT angiography or stress testing with subsequent utilization and spending among Medicare beneficiaries. JAMA. 2011;306:2128–2136. doi: 10.1001/jama.2011.1652. [DOI] [PubMed] [Google Scholar]
- 16.Hulten E, Pickett C, Bittencourt MS, et al. Outcomes after coronary computed tomography angiography in the emergency department: a systematic review and meta-analysis of randomized, controlled trials. J Am Coll Cardiol. 2013;61:880–892. doi: 10.1016/j.jacc.2012.11.061. [DOI] [PubMed] [Google Scholar]
- 17.Januzzi JL, Sharma U, Zakroysky P, et al. Sensitive troponin assays in patients with suspected acute coronary syndrome: Results from the multicenter rule out myocardial infarction using computer assisted tomography II trial. Am Heart J. 2015;169:572–578.e1. doi: 10.1016/j.ahj.2014.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raff GL, Abidov A, Achenbach S, et al. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr. 2009;3:122–136. doi: 10.1016/j.jcct.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Anderson JL, Adams CD, Antman EM, et al. 2011 ACCF/AHA Focused Update Incorporated Into the ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;123:e426–e579. doi: 10.1161/CIR.0b013e318212bb8b. [DOI] [PubMed] [Google Scholar]
- 20.Delong ER, Delong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- 21.Pencina MJ, D'Agostino RB, D'Agostino RB, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72. doi: 10.1002/sim.2929. discussion 207–12. [DOI] [PubMed] [Google Scholar]
- 22.Wildi K, Reichlin T, Twerenbold R, et al. Serial changes in high-sensitivity cardiac troponin I in the early diagnosis of acute myocardial infarction. Int. J. Cardiol. 2013;168:4103–4110. doi: 10.1016/j.ijcard.2013.07.078. [DOI] [PubMed] [Google Scholar]
- 23.Bandstein N, Ljung R, Johansson M, Holzmann MJ. Undetectable high-sensitivity cardiac troponin T level in the emergency department and risk of myocardial infarction. J Am Coll Cardiol. 2014;63:2569–2578. doi: 10.1016/j.jacc.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 24.Keller T, Zeller T, Ojeda F, et al. Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA. 2011;306:2684–2693. doi: 10.1001/jama.2011.1896. [DOI] [PubMed] [Google Scholar]
- 25.Diver DJ, Bier JD, Ferreira PE, et al. Clinical and arteriographic characterization of patients with unstable angina without critical coronary arterial narrowing (from the TIMI-IIIA Trial). Am J Cardiol. 1994;74:531–537. doi: 10.1016/0002-9149(94)90739-0. [DOI] [PubMed] [Google Scholar]
- 26.Roe MT, Harrington RA, Prosper DM, et al. Clinical and Therapeutic Profile of Patients Presenting With Acute Coronary Syndromes Who Do Not Have Significant Coronary Artery Disease. Circulation. 2000;102:1101–1106. doi: 10.1161/01.cir.102.10.1101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.