Abstract
Background:
Nephrotic syndrome is a disorder that leads to hyperlipidemia. L-carnitine and genistein can effect on lipid metabolism and the syndrome. In the present study, we have delved into the separate and the twin-effects of L-carnitine and genistein on the gene expressions of HMG-COA reductase and LDL receptor in experimental nephrotic syndrome.
Methods:
In this controlled experimental study, 50 male Sprague–Dawley rats were randomly divided into five groups: NC (normal-control), PC (patient-control), LC (L-carnitine), G (genistein), LCG (L-carnitine-genistein). Adriamycin was used for inducing nephrotic syndrome and the spot urine samples and urine protein-to-creatinine ratio were measured. Hepatocytic RNA was extracted and real-time PCR was used for HMG-COA Reductase and LDL receptor gene Expression measurement.
Results:
The final weight of the patients groups were lower than the NC group (P=0.001), and weight gain of the NC group was higher than the other groups (P<0.001). The proteinuria and urine protein-to-creatinine ratio showed significant differences between PC group and LC, G and LCG groups at week 7 (P<0.001). The expression of HMGCOA Reductase mRNA down regulated in LC, G and LCG groups in comparison with PC group (P<0.001). ΔCT of LDLr mRNA showed significant differences between the PC group and the other patient groups (P<0.001).
Conclusion:
This study shows a significant decreasing (P<0.001) and non-significant increasing trend in HMG-COA Reductase and LDLr gene expression, respectively, and synergistic effect of L-carnitine and genistein on these genes in experimental nephrotic syndrome.
Keywords: Gene, Genistein, L-carnitine, LDL Receptor, Nephrotic syndrome
Introduction
The nephrotic syndrome is a kind of disorder arising from extreme protein leakage from the bloodstream into the urine because of renal damage (1). Hyperlipidemia is a disorder, which happens alongside this disease (2). The common dyslipidemias in nephrotic syndrome are Hypercholesterolemia, increases of low-density lipoprotein-cholesterol (LDL-C) and very low-density lipoprotein-cholesterol (VLDL-C). Consequently, these disorders in lipid metabolism result in higher risk of cardiovascular diseases that shows the importance of lipid metabolism control in this disease. Among the substances that have the capacity to control cardiovascular diseases through changes in lipid metabolism, phyto-estrogens have an important role. Food phyto-estrogens are a subgroup of flavonoids that have beneficial effects on human health. This group comprises of several subgroups of non-steroid estrogens including isoflavones and lignans having been widely distributed among plants (3). Isoflavones (genistein and diadzein) are the most significant groups to have been widely undergone study. However, these isoflavones exist only in soybeans and several other legumes (3). The beneficial effects of dietary soy protein on the serum lipid concentrations have been shown in many studies on animal and on human cells (4–7). However, it is not exactly clear yet that these effects be mediated through the isoflavones such as genistein or not.
Carnitine is bio-synthesized by two amino acids [lysine and methionine] (8), and is necessary for transporting fatty acids from cytosols to mitochondria (9). Recently, many studies have focused on the role of carnitine in lipid metabolism. It has been proven that L-carnitine (a chemical structure of carnitine) is able to bring down the levels of triglycerides within rats’ tissues and plasma (10) but the mechanisms of its effects are not obvious yet.
Hydroxy Methyl Glutharyl-CoA Reductase (HMG-CoA) is the enzyme involved in synthesizing cholesterol and Low Density Lipoprotein Receptor (LDLr), which would be the LDL-C lipo-protein receptor in the liver: they are effective in the metabolic regulation of lipid and the liver cholesterol (11). Genistein gives rise to some level of LDLr gene expression (12, 13) while reducing the HMG-COA Reductase gene expressivity (13, 14). However, rare studies have ever been conducted as for the effect of L-carnitine on HMG-COA Reductase and LDLr; their resultant outcome is mostly paradoxical (15). The conducted investigations over the issue of the twin effect of genistein and L-carnitine on these two mentioned gene expression are extremely limited. We investigated the twin effect of genistein and L-carnitine to know if any joint pathway or synergistic effects in the pathways do exist or not.
Lack of a comprehensive study regarding this issue has caused the design of the present study with the aim of delving into the single separate and/or twin effects of genistein and L-carnitine on the HMG-COA Reductase and LDLr gene expression among the rats afflicted by the experiential nephrotic syndrome.
Material and Methods
Animals and experimental diets
Male Sprague–Dawley rats at 8–12 weeks of age were housed individually in a room with controlled temperature (20–22 °C), humidity (55– 65%) and lighting (from 0700 to 1900 h) and fed assigned experimental diet (AIN 93 M diet) (Table 1) (16). After 7 days of acclimatization, the rats were randomly divided into five groups consisting of 10 animals each with similar mean body weights (300±50 g) by randomized block design method: normal control (NC), patient control (PC), L-carnitine (LC), genistein (G), L-carnitinegenistein (LCG).
Table 1.
Composition of experimental diet (AIN-93 modified diet for rodents)
| Ingredient | g/kg diet |
|---|---|
| Cornstarch | 465.692 |
| Casein (>85% protein) | 140.000 |
| extrinized cornstarch (90–94% tetrasaccharides)1 | 155.000 |
| Sucrose | 100.000 |
| Soybean oil (no additives) | 40.000 |
| Fiber2 | 50.000 |
| Mineral mix | 35.000 |
| Vitamin mix | 10.000 |
| L-Cystine | 1.800 |
| Choline bitartrate (41.1% choline)3 | 2.500 |
| Tert-butylhydroquinone | 0.008 |
| u/kg diet | |
| Total energy4 kcal | 3601.0 |
| protein% | 14.1 |
| CHO% | 75.9 |
| fat% | 10.0 |
Dyetrose (Dyets, Bethlehem, PA) and Lo-Dex 10 (American Maize, Hammond, IN) meet these specifications. An equivalent product may also be used./
Solka-Floc®,200 FCC (FS&.D, St. Louis, MO) or its equivalent is recommended./
Based on the molecular weight of the free base./
The estimate of caloric content was based on the standard physiological fuel values for protein, fat, and carbohydrate of 4, 9 and 4, respectively.
Chemical reagents and Intervention
All groups received their own experimental diets during the study (8 weeks). We used carboxymethyl cellulose (CMC, Sigma Chemical Co.) as a solvent for genistein and L-carnitine. In addition, CMC was used for gavage feeding of control groups. NC group received 50 mg/kg body weight CMC by gavage for 8 weeks; PC group received CMC for 8 weeks while receiving single dose of 7.5 mg/kg body weight Adriamycin (Doxorubicin, Pharmacia Italia SPA Co.)-an antibiotic/antineoplastics drug with nephrotoxic side effect- through tail vein at the end of week 2 to induce nephrotic syndrome (17), hereafter, we keep on gavage-feeding of rats with 50 mg/kg body weight CMC for 6 weeks. LC, G and LCG groups were similar to PC except receiving 50 mg/kg body weight L-carnitine (99%, Karen Pharma & Food Supplement Co.), 50 mg/kg body weight genistein (99%, LC-laboratories Co.) and 50 mg/kg body weight L-carnitine plus 50 mg/kg body weight genistein, respectively, that were dissolved in CMC instead of CMC.
Animals were maintained ad libitum on assigned experimental diet and water during the experiment and Dietary intake and body weight were recorded every day and weekly, respectively.
This study was approved by the review board of animal ethics Tehran University of Medical Sciences and we followed the institute’s guidelines in the care and use of laboratory animals.
Sample preparation
During the study, urine samples were collected (spot urine method) at the end of weeks 2, 3 and 7 and measured urine total protein and protein-to-creatinine ratio from spot urine samples. Pyrogallol-Red/Colorimetric End Point method and Taussky et al. (18) & Owen et al. (19), modified method were used for measuring of protein and creatinine, respectively. After 8 weeks, the animals were sacrificed after overnight fasting by bleeding from the abdominal aorta under diethyl ether anesthesia. Blood was collected from abdominal aorta and livers were surgically excised. The blood was allowed to coagulate and centrifuged at 1,100 rpm for 15 minutes, and serum was stored at −20 °C until albumin analysis (salt fractionation method). Liver tissues were collected and immediately frozen in liquid nitrogen, and stored at −80 °C until analysis.
RNA Extraction from Liver and cDNA Synthesis
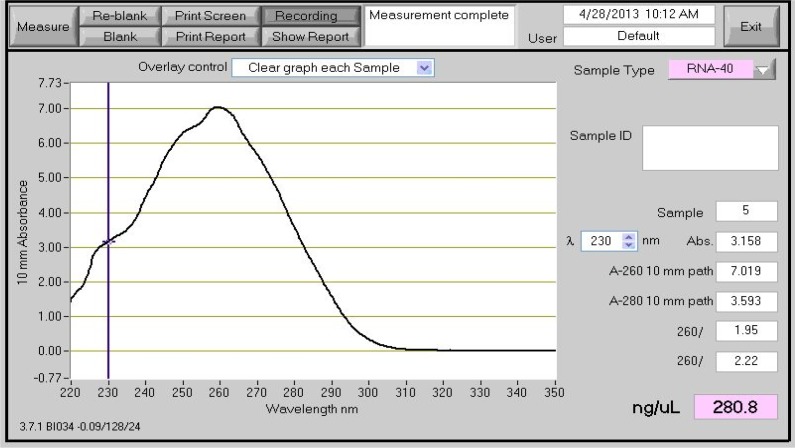
Cytoplasmic RNA was extracted and purified using RNeasy Plus Mini Kit (Qiagen, Valencia, Calif., USA) according to the manufacturer’s protocol. Quantity and purity of extracted RNA was checked by NanoDrop spectrophotometer (NanoDrop Technologies, Wilmington, Del., USA). A ratio of A 260/280 between 1.9–2.1 was taken into account as pure RNA (Fig. 1). Single-strand cDNA was synthesized using QuantiTect Reverse Transcription Kit (Qiagen).
Fig. 1:
NanoDrop spectrophotometer of the extracted RNA
Real-time PCR for Gene Expression
PCR primers for HMG-COA Reductase and LDLr genes and 18-S gene (as housekeeping) were designed by Primer express 3 software (Applied Biosystem, Foster city, CA, USA) and purchased from Metabion (Table 2).
Table 2.
Primer sequences for real-time PCR
| Gene | Sequence | Length | TM | CG% |
|---|---|---|---|---|
| HMG-COA Reductase | Forward 5′-GTGGGAACGGTGACACT TA-3′ | 19 | 49.47 | 53 |
| Reverse 5′-CTTCAAATTTTGGGCACTCA-3′ | 20 | 49.14 | 40 | |
| LDLr | Forward 5′-CTGGCGGTAGACTGGATC-3′ | 18 | 50.97 | 61 |
| Reverse 5′-CAATCTGTCCAGTACATGAAGC-3′ | 22 | 52.39 | 45 | |
| 18-S | Forward 5′-CCATCCAAT CGGTAGTAGC-3′ | 19 | 49.61 | 53 |
| Reverse 5′-GTAACCCGT TGAACCCCATT-3′ | 20 | 50.05 | 50 |
PCR reactions were briefly as follows (20, 21); PCR proceeded in special optical tubes in 48- reaction plates (MicroAmp Optical, ABI) with 20 μl reaction mixture containing 10μl Power SYBR® Green PCR Master Mix (Applied Biosystem, Foster city, CA, USA), 7μl DEPC treated water, 0.5μl forward primer, 0.5μl reverse primer and 2μl cDNA as template. The wells were sealed with optical adhesive film (Applied Biosystem, Foster city, CA, USA), and the plate was centrifuged for a few seconds at high speed. Amplification conditions were performed using the standard two-step run protocol; step 1:10s at 95 °C, step 2: 40 cycles of 15s at 95 °C plus 1s at 60 °C.
After completion of amplification cycles, melt curve was generated to verify if a single gene product had been amplified. For each gene, mRNA expression level was normalized to the level of 18-S. The fold changes of genes expression were computed using the comparative Ct (2–ΔΔCt) method.
Statistical analysis
Statistical analysis was done using SPSS 18.0 for windows (Chicago, IL, USA). Normality of all data was checked by Kolmogorov-Smirnov test and histogram. Data was expressed as mean ± SD. Comparison of quantitative variables between different groups were evaluated by one-way ANOVA, followed by post hoc Scheffé test. P-value < 0.05 was considered statistically significant.
Results
Body weight and food intake
As shown in Table 3, there were not any statistically significant differences between groups in initial weight, but final weight and weight gain of the patient groups was significantly less than the NC group (P<0.05). The PC group did not show any statistically significant differences compared with LC, G and LCG groups in all these variables (Table 3).
Table 3.
Body weight and food intake in rat fed experimental diets for 8 weeks
| Variable | NC group | PC group | LC group | G group | LCG group | P valuea |
|---|---|---|---|---|---|---|
| Initial weight (g) | 296.50±25.50 | 291.50±28.19 | 294.77±23.62 | 303.22±34.23 | 312.00±26.25 | 0.501 |
| Final weight (g) | 355.30±18.43 | 283.30±34.13b | 277.88±48.73b | 283.44±47.47b | 263.14±67.88b | 0.001 |
| Weight gain (g/day) | 1.04±0.45 | −0.14±0.50b | −0.36±0.83b | −0.34±0.58b | −0.87±0.77b | 0.00 |
| Food intake (g/day) | 20.36±0.73 | 16.73±0.49b | 16.36±1.16b | 15.33±1.10b | 15.16±0.40b | 0.00 |
| Protein Intake (g/day) | 2.55±0.09 | 2.10±0.06b | 2.05±0.14b | 1.92±0.14b | 1.90±.05b | 0.00 |
| Energy intake (Kcal/day) | 73.34±2.65 | 60.25±1.77 b | 58.93±4.20 b | 55.21±3.98 b | 54.61±1.45 b | 0.00 |
Values are means±SD./
One-way ANOVA between groups./
Values for PC, LC, G and LCG groups are significantly different compared with NC group by post hoc Scheffé test at P<0.05.
Serum albumin, Proteinuria and protein-to-creatinine ratio
There were not any statistical significant difference between groups in proteinuria and urine protein-to-creatinine ratio at week 2, but the differences were significant between PC group and LC, G and LCG groups at week 7 (Table 4).
Table 4.
Proteinuria and protein-to-creatinine in experimental groups at weeks 2, 3 and 7 and serum albumin
| Variable | NC group | PC group | LC group | G group | LCG group | P valuea |
|---|---|---|---|---|---|---|
| Week 2: Proteinuria (mg/dl) | 107.70±4.92 | 111.85±5.92 | 102.00±48.74 | 105.11±28.94 | 98.00±9.38 | 0.877 |
| Week 3: Proteinuria (mg/dl) | 107.50±6.36 | 671.14±180.28b | 273.00±99.73c | 384.66±237.18b | 210.25±131.77c | 0.00 |
| Week 7: Proteinuria (mg/dl) | 103.90±22.65 | 1864.00±298.27b | 328.50±27.87c | 680.88±348.82bc | 400.25±120.13c | 0.00 |
| Week 2: Urine protein-to-creatinine ratio | 2.96±1.26 | 3.96±0.71 | 1.85±0.28 | 3.74±1.82 | 3.67±1.47 | 0.104 |
| Week 3: Urine protein-to-creatinine ratio | 3.39±1.12 | 29.98±7.41b | 18.70±30.71 | 14.38±7.92 | 5.88±.3.71c | 0.001 |
| Week 7: Urine protein-to-creatinine ratio | 3.87±1.30 | 71.48±17.20b | 22.97±3.19c | 38.11±19.59bc | 20.67±21.28c | 0.00 |
| Serum albumin | 3.63±0.25 | 1.32±0.34b | 2.73±0.23bc | 1.47±0.63b | 2.86±1.35c | 0.00 |
Values are means±SD.
One-way ANOVA between groups.
Values for PC, LC, G and LCG groups are significantly different compared with NC group by post hoc Scheffé test at P<0.05.
Values for LC, G and LCG groups are significantly different compared with PC group by post hoc Scheffé test at P<0.05.
HMG-COA Reductase and LDLr Expression in hepatocyte-Extracted mRNA
Expression of HMG-COA Reductase mRNA between the LC, G, LCG groups and the PC group had statistically significant differences (P<0.001, Table 5). L-carnitine and genistein could down-regulate HMG-COA Reductase and twin-effects of them had a synergistic effect, however the differences between the LC, G, LCG groups were not statistically significant. As to the relative gene expression of LDLr, significant differences were not observed between the groups, but there were statistically significant differences between LC, G, LCG groups and PC group in ΔCT (P<0.001, Table 5).
Table 5.
ΔCT and mean of HMG-COA Reductase and LDLr gene expression in hepatocytes
| Variable | NC group | PC group | LC group | G group | LCG group | P valuea |
|---|---|---|---|---|---|---|
| Δ-CT of HMG-COA Reductase | 14.52±1.72 | 13.29±0.48 | 13.32±1.94 | 13.14±1.96 | 12.68±2.38 | 0.371 |
| Mean of gene expression of HMG-COA Reductase | 1.41±1.32 | 2.66±0.88 | 0.78±0.61c | 0.24±0.20bc | 0.23±0.15bc | 0.000 |
| Δ-CT of LDLr | −0.16±0.48 | 3.31±1.88b | −0.33±0.66c | −0.82±1.24c | −1.14±2.21c | 0.000 |
| Mean of gene expression of LDLr | 1.24±0.83 | 0.19±0.08b | 0.89±0.67 | 1.09±0.49 | 0.74±0.34 | 0.035 |
Data are reported as means ± SD. ΔCT = CT of target gene – CT of 18S.
One-way ANOVA between groups./
Values for PC, LC, G and LCG groups are significantly different compared with NC group by post hoc Scheffé test at P<0.05./
Values for LC, G and LCG groups are significantly different compared with PC group by post hoc Scheffé test at P<0.05.
Discussion
Over the separate effects of genistein and L-carnitine, we have studied their cumulative twin effects, as well, in Sprague-Dawley rats. As shown in Table 3, the final weight in addition to the weight gain have been lower and negative in all patient groups in comparison with the NC group; the reasonable cause for this phenomenon has been rats’ affliction by the nephrotic syndrome which has consequently followed by reductions in food and energy intakes among these groups. In spite of receiving less protein in the patient groups as compared with the NC group, the proteinuria and the urine protein-to-creatinine ratio have been higher in the patient groups versus the NC group, as brought out in Table 4: this indicates their having been caught by the nephrotic syndrome and the protein tissue lysis leading to higher weight loss among these groups, although such increase amongst a number of patient groups has not been statistically significant.
Genistein Effect on LDLr and HMG-COA Reductase Gene Expression
Insulin and glucagon are key controllers for the matter of biosynthesizing cholesterol and triglyceride within the liver: they exert their biological controlling influence through some changes in the level of activity and/or expressing gene levels involved in the synthesizing and/or absorbing cholesterol; the same influence can also be exerted by means of synthesizing fatty acids. Such genes transcription controlling would be accomplished through the means of a family of transcription factors by the name of SREBP (22). Genistein possesses the capability to increase the glucagon to insulin ratio (23), thus giving rise to some increase not only in the level of SREBP-2 expression, but also in its activity (24). SREBP-2 would preferably hook on to those promoters of the number of genes involved in absorbing and biosynthesizing cholesterol [including HMG-CoA Reductase and (LDLr) LDL recipient] (11). In fact, the category of isoflavones present in soy protein can activate SREBP-2 so that, as a result, the serum cholesterol clearance could well increase (25). When the cholesterol level comes down in the cells belonging to animals fed with soy protein, the mature nuclear SREBP-2 form content increases by up to the level of 119% in comparison with the rats dieted on casein (26) which in itself would lead to some increase in the level of LDLr gene expression (27). Borradaile et al. have also conducted a study on the human liver cells (HepG2) to show that genistein causes increase in the levels of LDLr mRNA by 3 to 6 times; this means that they increase the absorption and the lysis of marked LDLs statistically significantly (13). All the same, it should not be far from notice that such effects might actually be independent of the insulin to glucagon ratio (28).
The isoflavones’ effect, especially that of genistein, on HMG-COA Reductase turns out to be paradoxical. There are a number of studies indicating that genistein could give rise to increase in LDLr gene expression to be followed by HMG-COA Reductase gene expression within the human DLD-1 cancerous colon cells (12, 29).
Our own investigation has shown that genistein causes some reduction in HMG-COA Reductase gene expression: this is in contrast with the PC group. Such reduction was even greater than that of the L-carnitine recipient group, despite the fact that the said difference did not prove statistically significant (Table 5). Moreover, the LDLr expression in the group receiving genistein was actually higher as compared with the PC group, and even: as contrasted with L-carnitine; however, these differences were not statistically significant, though the Δ-CT difference in between the G group and the PC group turned out to be statistically significant (Table 5).
L-carnitine Effect on LDLr and HMG-COA Reductase Gene Expression
Dyslipidemia is generally common among patients with renal ailments, specifically among those afflicted by the nephrotic syndrome. Nearly 40 percent of those patients undergoing haemodialysis are gripped by some sort of dyslipidemia: the majority of them are afflicted by hyperlipidemia type IV and plasma HDL-C reduced levels (30). The progressing and advancement of dyslipidemia among such patients are themselves under the influence of a number of various parameters such as carnitine shortage, leading to actual disorders in the process of lipid metabolism (31, 32). The carnitine can significantly bring down the levels of rats’ tissues and plasma triglyceride (33). Still, and overall systematic review would indicate that carnitine has no statistically significant effects on triglyceride, cholesterol, and their probable derivatives (34). The carnitine supplement has turned out to be effective in adjusting the lipid profile among those patients whose level of triglyceride has been above the 200 mg/dl or the HDL-C level has actually been below 35 mg/dl (35).
In the present study, L-carnitine could well have caused some statistically significant decrease in HMG-COA Reductase gene expressivity in comparison with the PC group in spite of the fact that such reducing effect has not been up to the group receiving genistein. In addition, the LDLr expression because of receiving L-carnitine went on the increase in comparison with the PC group: although such an increase was not statistically significant, the difference in Δ-CT did prove significant (Table 5).
Very limited studies are available regarding the effect of carnitine on the gene expressions of the two genes of HMG-COA Reductase and LDLr. Evaluation has been made in Mondola’s et al. investigation into the effect of carnitine on cholesterol metabolism and HMG-COA Reductase activity in rats’ liver cells where it has been shown that L-carnitine could well rein in the HMG-COA Reductase activity and also increase the bonding of LDL on two the liver cells (15).
The Twin Effect of Genistein and Carnitine on LDLr and HMG-COA Reductase Gene Expression
In our study, the synergistic effect of genistein and L-carnitine on the expressivity of both genes have actually been observed, although this effect turned out to be statistically significant nearly as far as comparison was made in between HMG-COA Reductase vs. the PC group. Δ-CT gene LDLr, too, showed of itself some significant synergistic effect (Table 5). Similar studies concerning the twin effect of genistein and carnitine on these two genes’ expression are skimpy to such a degree that their availability would prove difficult.
Conclusion
A 6-week gavaging with L-carnitine and genistein increased the HMG-COA Reductase and LDLr gene expression and had synergistic effects in rats with nephrotic syndrome; however, the changes were statistically significant only for HMG-COA reductase. It seems genistein is more effective on these gene expressions in comparison with L-carnitine. These finding could warrant future studies to determine the therapeutic effects of these supplements on nephrotic syndrome and lipid metabolism management.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
We thank the technical assistance of Ms. Derakhshanian and Ms. Zareie. The authors acknowledge the financial support of Vice Chancellor for Research and Technology of Tehran University of Medical Sciences. In addition, we thank the staff members of Cellular and Molecular Nutrition laboratory and Animal house of public health school for their valuable cooperation during this study. The authors declare that there is no conflict of interests.
References
- 1. Bergstain JM. (2000). Nephrotic syndrome. In: Nelson textbook of pediatrics. Eds, Behrman RE, Kliegman RM, Jenson HB. 16th ed, W B Saunders Company; Philadephia, P.: 1801. [Google Scholar]
- 2. Sulowicz W, Stompor T. (2003). LDL-apheresis and immunoadsorption: novel methods in the treatment of renal diseases refractory to conventional therapy. Nephrol Dial Transplant, 18: v59–v62. [DOI] [PubMed] [Google Scholar]
- 3. Setchell KD, Cassidy A. (1999). Dietary isoflavones: biological effects and relevance to human health. J Nutr, 129: 758S– 767S. [DOI] [PubMed] [Google Scholar]
- 4. Sirtori CR, Even R, Lovati MR. (1993). Soybean protein diet and plasma cholesterol: from therapy to molecular mechanisms. Ann NY Acad Sci, 676: 188–201. [DOI] [PubMed] [Google Scholar]
- 5. Tovar AR, Murguía F, Cruz C, Hernández-Pando R, Aguilar-Salinas CA, Pedraza-Chavarri J, et al. (2002). A soy protein diet alters hepatic lipid metabolism gene expression and reduces serum lipids and renal fibrogenic cytokines in rats with chronic nephritic syndrome. J Nutr, 132: 2562–9. [DOI] [PubMed] [Google Scholar]
- 6. Tovar-Palacio C, Potter SM, Hafermann JC, Shay NF. (1998). Intake of soy protein and soy protein extracts influences lipid metabolism and hepatic gene expression in gerbils. J Nutr, 128: 839–42. [DOI] [PubMed] [Google Scholar]
- 7. Rosell MS, Appleby PN, Spencer EA, Key TJ. (2004). Soy intake and blood cholesterol concentrations: a cross-sectional study of 1033 pre- and postmenopausal women in the Oxford arm of the European Prospective Investigation into Cancer and Nutrition. Am J Clin Nutr, 80: 1391–6. [DOI] [PubMed] [Google Scholar]
- 8. Steiber A, Kerner J, Hoppel C. (2004). Carnitine: a nutritional, biosynthetic, and functional perspective. Mol Aspects Med, 25 ( 5–6): 455–73. [DOI] [PubMed] [Google Scholar]
- 9. Liedtke AJ, Nellis SH, Whitesell LF, Mahar CQ. (1982). Metabolic and mechanical effects using L- and D-carnitine in working swine hearts. Heart Circulat Physiol, 243 ( 5): H691–H697. [DOI] [PubMed] [Google Scholar]
- 10. Karanth J, Jeevaratnam K. (2009). Effect of dietary lipid, carnitine and exercise on lipid profile in rat blood, liver and muscle. Indian J Exp Biol, 47 ( 9): 748–753. [PubMed] [Google Scholar]
- 11. Amemiya-Kudo M, Shimano H, Hasty AH, Yahagi N, Yoshikawa T, Matsuzaka T, et al. (2002). Transcriptional activities of nuclear SREBP-1a,-1c, and -2 to different target promoters of lipogenic and cholesterogenic genes. J Lipid Res, 43: 1220–35. [PubMed] [Google Scholar]
- 12. Notarnicola M, Messa C, Orlando A, D’Attoma B, Tutino V, Rivizzigno R, Caruso MG. (2008). Effect of genistein on cholesterol metabolism-related genes in a colon cancer cell line. Genes Nutr, April; 3( 1): 35– 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Borradaile NM, de Dreu LE, Wilcox LJ, Edwards JY, Huff MW. (2002). Soya phytoestrogens, genistein and daidzein, decrease apolipoprotein B secretion from HepG2 cells through multiple mechanisms. Biochem J, 366 ( Pt 2): 531–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Marsh TG, Straub RK, Villalobos F, Hong MY. (2011). Soy protein supports cardiovascular health by downregulating hydroxymethylglutaryl-coenzyme A reductase and sterol regulatory element-binding protein-2 and increasing antioxidant enzyme activity in rats with dextran sodium sulfate-induced mild systemic inflammation. Nutr Res, 31( 12): 922–8. [DOI] [PubMed] [Google Scholar]
- 15. Mondola P, Santillo M, De Mercato R, Santangelo F. (1992). The effect of L-carnitine on cholesterol metabolism in rat (Rattus bubalus) hepatocyte cells. Int J Biochem, 24( 7): 1047–50. [DOI] [PubMed] [Google Scholar]
- 16. Reeves PG. (1997). Symposium: Animal56 Diets for Nutritional and Toxicological Research, pp: 24– 28. [Google Scholar]
- 17. Javanbakht MH, Sadria R, Djalali M, Derakhshanian H, Hosseinzadeh P, Zarei M, Azizi G, Sedaghat R, Mirshafiey A. (2014). Soy protein and genistein improves renal antioxidant status in experimental nephrotic syndrome. Nefrologia, 34( 4): 483–90. [DOI] [PubMed] [Google Scholar]
- 18. Taussky HH. (1961). Creatinine and Creatine in Urine and Serum. In standard Methods of Clinical Chemistry (Vol. 3), Ed, Seligson D. Acad. Press, New York: , p.:99. [Google Scholar]
- 19. Owen JA, Iggo B, Scandrett FJ, Stewart CP. (1954). The determination of creatinine in plasma or serum and in urine: a critical examination. Biochem J. pp.: 58, 426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mottaghi A, Salehi E, Keshvarz A, Sezavar H, Saboor-Yaraghi AA. (2012). The influence of vitamin A supplementation on Foxp3 and TGF-β gene expression in atherosclerotic patients. J Nutrigenet Nutrigenomics, 5( 6): 314–26. [DOI] [PubMed] [Google Scholar]
- 21. Mottaghi A, Salehi E, Sezavar H, Keshavarz SA, Eshraghian MR, Rezaei N, Rejali L, Saboor-Yaraghi AA. (2012). The in vitro effect of oxidized LDL and PHA on proliferation and gene expression of regulatory T cells in patients with atherosclerosis. Iran J Allergy Asthma Immunol, 11( 3): 217–23. [PubMed] [Google Scholar]
- 22. Brown MS, Goldstein JL. (1997). The SREBP pathway: regulation of cholesterol metabolism by proteolysis of a membrane-bound transcription factor. Cell, 89: 331–40. [DOI] [PubMed] [Google Scholar]
- 23. Ae Park S, Choi MS, Cho SY, Seo JS, Jung UJ, Kim MJ, Sung MK, Park YB, Lee MK. (2006). Genistein and daidzein modulate hepatic glucose and lipid regulating enzyme activities in C57BL/KsJ-db/db mice. Life Sci, 15; 79( 12): 1207– 13. [DOI] [PubMed] [Google Scholar]
- 24. Yang JY, Lee SJ, Park HW, Cha YS. (2006). Effect of genistein with carnitine administration on lipid parameters and obesity in C57Bl/6J mice fed a high-fat diet. J Med Food, 9( 4): 459–67. [DOI] [PubMed] [Google Scholar]
- 25. Mullen E, Brown RM, Osborne TF, Shay NF. (2004). Soy isoflavones affect sterol regulatory element binding proteins (SREBPs) and SREBP-regulated genes in HepG2 cells. J Nutr, 134: 2942–7. [DOI] [PubMed] [Google Scholar]
- 26. Tovar A, Manzano N, Torres N. (2005). Regulación del metabolismo del colesterol y ácidos grasos en el síndrome nefrótico experimental por las Proteínas que se Unen a los Elementos Regulatorios de Esteroles (SREBP’s): efecto de la soya. Gaceta Med Mex, 141: 27–35. [PubMed] [Google Scholar]
- 27. Ascencio C, Torres N, Isoard-Acosta F, Gómez-Pérez FJ, Hernández Pando R, Tovar AR. (2004). Soy protein affects serum insulin and hepatic SREBP-1 mRNA and reduces fatty liver in rats. J Nutr, 134: 522–9. [DOI] [PubMed] [Google Scholar]
- 28. Shukla A, Brandsch C, Bettzieche A, Hirche F, Stangl GI, Eder K. (2007). Isoflavone-poor soy protein alters the lipid metabolism of rats by SREBP-mediated down-regulation of hepatic genes. J Nutr Biochem, 18( 5): 313–21. [DOI] [PubMed] [Google Scholar]
- 29. Caruso MG, Messa C, Orlando A, D’Attoma B, Notarnicola M. (2008). Early induction of LDL receptor gene expression by genistein in DLD-1 colon cancer cell line. Fitoterapia, 79(7–8): 524–8. 10.1016/j.fitote.2008.05.003. Epub 2008Jun 22. PubMed PMID: . [DOI] [PubMed] [Google Scholar]
- 30. Tsimihodimos V, Dounousi E, Siamopoulos K C. (2008). Dyslipidemia in chronic kidney disease: an approach to pathogenesis and treatment. Am J Nephrol, 28 ( 6): 958–973. [DOI] [PubMed] [Google Scholar]
- 31. Vaziri ND, Moradi H. (2006). Mechanisms of dyslipidemia of chronic renal failure. Hemodialysis Int, 10 ( 1): 1–7. [DOI] [PubMed] [Google Scholar]
- 32. Bellinghieri G, Santoro D, Calvani M, Mallamace A, Savica V. (2003). Carnitine and hemodialysis. Am J Kidney Dis, 41(3), supplement; pp. S112– S126. [DOI] [PubMed] [Google Scholar]
- 33. Karanth J, Jeevaratnam K. (2009). Effect of dietary lipid, carnitine and exercise on lipid profile in rat blood, liver and muscle. Indian J Exp Biol, 47( 9): 748–753. [PubMed] [Google Scholar]
- 34. Hurot J M, Cucherat M, Haugh M, Fouque D. (2002). Effects of L-carnitine supplementation in maintenance hemodialysis patients: a systematic review. J Am Soc Nephrol, 13( 3): 708–714. [DOI] [PubMed] [Google Scholar]
- 35. Reuter SE, Faull R J, Evans AM. (2008). L-carnitine supplementation in the dialysis population: are Australian patients missing out? Nephrology, 13( 1): 3–16. [DOI] [PubMed] [Google Scholar]