Abstract
Purpose
Perianal lesions are common in Crohn disease, but their clinical course is unpredictable. Nevertheless, predicting the clinical course after surgery for perianal Crohn disease (PCD) is important because repeated operations may decrease patient's quality of life. The aim of this study was to predict the risk of reoperation in patients with PCD.
Methods
From September 1994 to February 2010, 377 patients with PCD were recruited in twelve major tertiary university-affiliated hospitals and two specialized colorectal hospitals in Korea. Data on the patient's demographics, clinical features, and surgical outcomes were analyzed.
Results
Among 377 patients, 227 patients were ultimately included in the study. Among the 227 patients, 64 patients underwent at least one reoperation. The median period of reoperation following the first perianal surgery was 94 months. Overall 3-year, 5-year, and 10-year cumulative rates of reoperation-free individuals were 68.8%, 61.2%, and 50.5%, respectively. In multivariate analysis (Cox-regression hazard model), reoperation was significantly correlated with an age of onset less than 20 years (hazard ratio [HR], 1.93; 95% confidence interval [CI], 1.07-3.48; P = 0.03), history of abdominal surgery (HR, 1.99; 95% CI, 1.08-3.64; P = 0.03), and the type of surgery. Among types of surgery, fistulotomy or fistulectomy was associated with a decreased incidence of reoperation in comparison with incision and drainage (HR, 0.19; 95% CI, 0.09-0.42; P < 0.001).
Conclusion
Young age of onset and a history of abdominal surgery were associated with a high risk of reoperation for PCD, and the risk of reoperation were relatively low in fistulotomy or fistulectomy procedures.
Keywords: Perianal Crohn disease, Recurrence, Surgery
INTRODUCTION
Crohn disease (CD) is an idiopathic chronic inflammatory bowel disease, characterized by various and unpredictable clinical courses. Recently, according to local epidemiologic studies, the incidence of CD has been increasing in Korea [1,2]. Perianal involvement in CD, which includes skin tags, hemorrhoids, anal fissures or ulcers, perianal abscesses, perianal fistulas, and anorectal strictures, is a common and troublesome complication because it can seriously decrease a patient's quality of life. The reported incidence of perianal involvement in CD varies widely from approximately 10% to 80% [3,4,5]. Perianal complications can develop at anytime during the course of the disease, and in approximately 10%-17% of patients, perianal problems precede the diagnosis of CD [6,7]. Various surgical procedures from minimal intervention, such as incision and drainage, to a proctectomy are required, depending on the disease's severity and type.
CD is characterized by transmural bowel involvement, anywhere from the mouth to the anus, which can lead to the development of a fistula, particularly in the perianal area. A perianal Crohn fistula should be considered as a distinct disease phenotype, different from luminal fistulizing CD, because it is associated with colonic involvement of CD instead of small bowel involvement [8]. Moreover, the general clinical course of CD with perianal disease seems to be more aggressive. If a fistula is present at the initial diagnosis, the disease is likely to progress more rapidly from inflammatory to stricturing or penetrating complications. Because of these potential complications, more advanced medical therapies, such as immunosuppressive agents, anti-tumor necrosis factor (anti-TNF) treatment, or surgical interventions, may be required [9,10,11].
To date, many clinical studies have attempted to predict the risk factors for intestinal resection or recurrence after primary surgery in patients with CD. Unfortunately, the results have been inconsistent, and most of the clinical and epidemiological studies have been based on Western populations, despite an increasing incidence of CD in Asian countries, including Korea. In addition, the amount of available data on the risk factors of reoperation after perianal surgery for CD is relatively small compared to the available data on the risk factors of reoperation after abdominal surgery for CD patients. Considering that the incidence of perianal CD (PCD) requiring surgery ranges from 25% to 30% [12,13], predicting the clinical course after surgery for PCD is very important. Reoperations may increase the risk of sphincter injury, which can subsequently devastate the patient's quality of life. Thus, the aim of this study was to predict the risk factors for reoperation in Korean patients with PCD.
METHODS
Patient inclusion
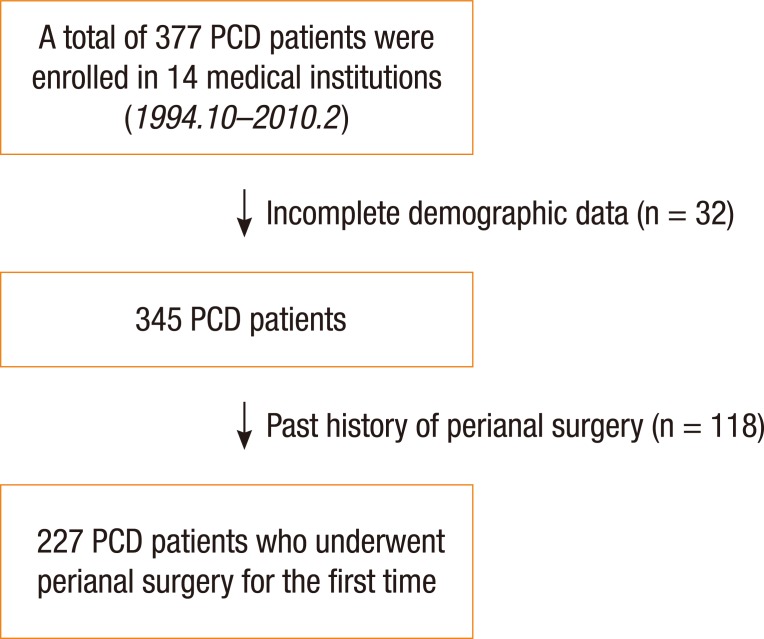
From September 1994 to February 2010, 377 patients with perianal CD were recruited at 12 major tertiary university-affiliated hospitals and 2 colorectal-specializing hospitals in Korea and were considered for inclusion in this study. Age at diagnosis, disease behavior, and location were categorized according to the Montreal classification. Data on the patients' demographics, clinical features, and surgical outcomes were analyzed to evaluate the risk factors for reoperation for PCD. The factors included in this study protocol were decided at a meeting of the 'inflammatory bowel disease (IBD) Study Group of The Korean Society of Coloproctology, which was held before data collection started. The data were initially collected for the 377 patients, 32 cases were excluded because of incomplete demographic data, and then among the remaining 345 patients, 118 patients with a history of anal surgery for perianal disease were excluded (Fig. 1). Therefore, 227 patients who underwent perianal surgery for PCD for the first time were included in this study. During the follow-up period after the first operation, the rate of reoperation was investigated, and the data were analyzed to determine the risk factors for reoperation.
Fig. 1. Flow chart for patient inclusion.
Statistical analysis
We used the SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA) for our statistical analyses. The Kaplan-Meier method was used to estimate the cumulative reoperation rate after primary perianal surgery. In the univariate analyses, the log rank test was used to determine differences in the distributions. In the multivariate analyses, factors that seemed to have a significant impact on the time to event-free survival (log rank P < 0.1) were entered into a Cox proportional hazards model to test for independent significance of their effects, while simultaneously adjusting for multiple factors. Significance was accepted at a P-value of less than 0.05 for all tests.
RESULTS
Baseline characteristics (Table 1)
Table 1. Baseline characteristics of the patients (n = 227).
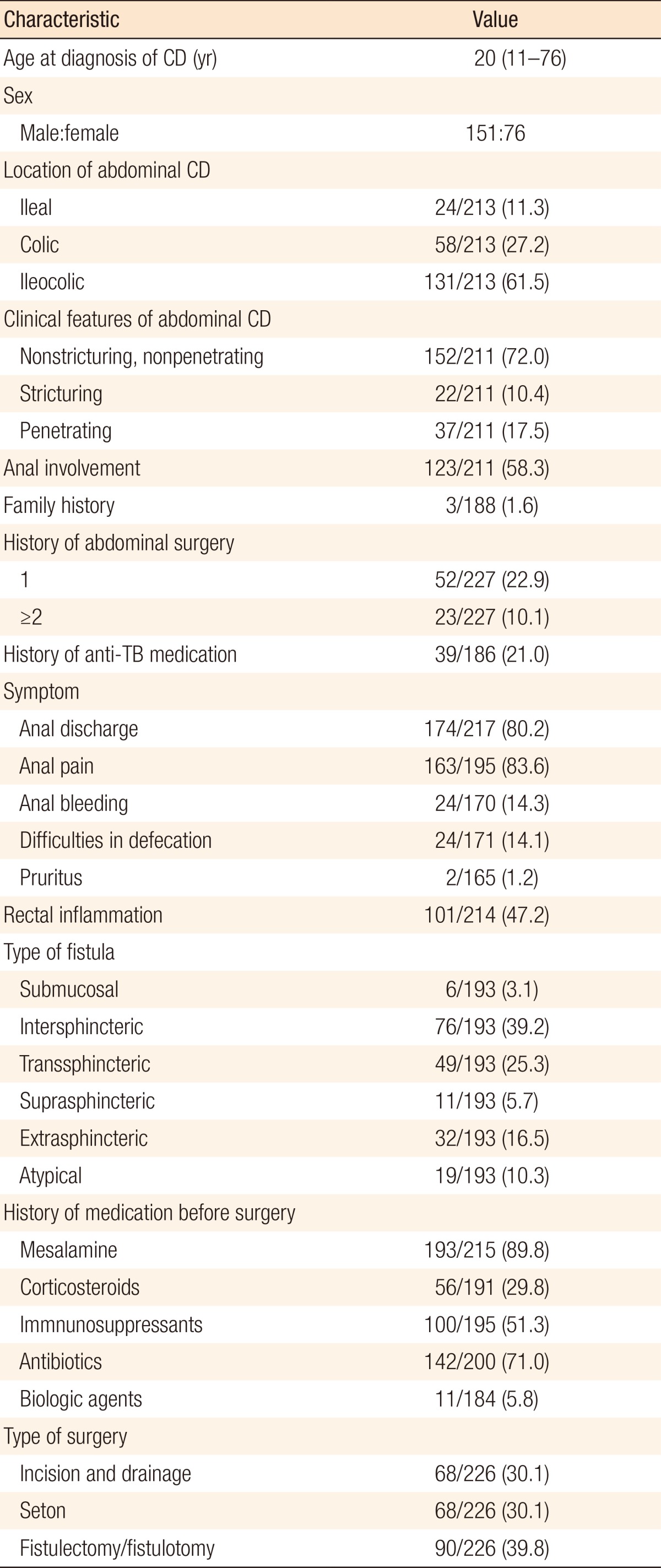
Values are presented as median (range) or number (%).
CD, Crohn disease; TB, tuberculosis.
The median age at the diagnosis of CD was 20 years old (range, 11-76 years), and males were more common than females (male: female = 1.99:1). Family history of the disease was confirmed in only 1.6% of the patients. At the time of diagnosis, ileocolic type (61.5%), and the nonstricturing and the nonpenetrating types were the most common (72.0%) when classified according to the disease distribution and clinical behavior. Seventy-five of the 227 patients (33%) underwent abdominal surgery before anal surgery. The most common type of fistula was an intersphincteric fistula (39.2%), followed by a transsphincteric fistula (25.3%).
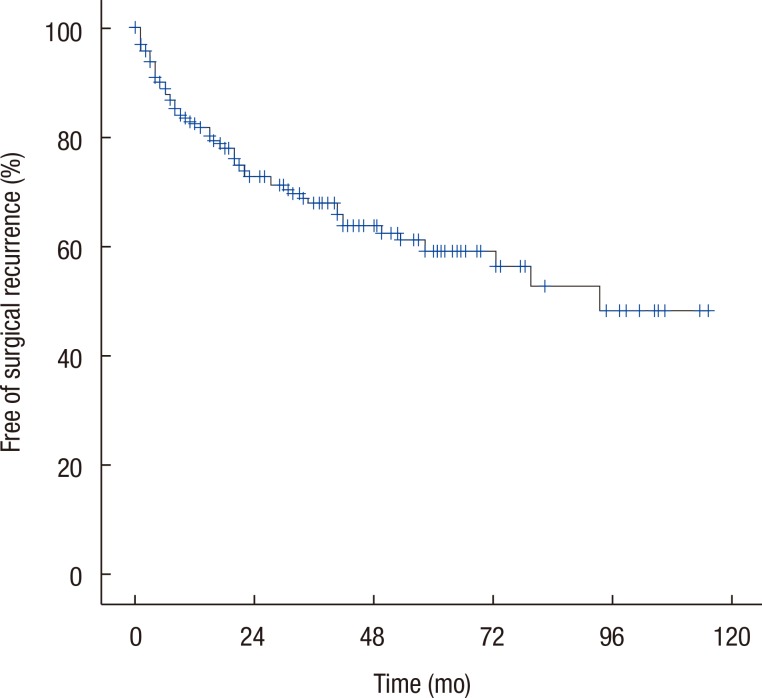
During the follow-up period (median, 41 months; range, 3-131 months), 64 patients underwent at least one reoperation (28.2%). The median time to reoperation following perianal surgery was 94 months. The overall 3-year, 5-year, and 10-year cumulative free-of-reoperation rates were 68.8%, 61.2%, and 50.5%, respectively (Fig. 2).
Fig. 2. Kaplan-Meier curve demonstrating the free of surgical recurrence rate as a function of time after perianal surgery for perianal Crohn disease.
Univariate and multivariate analyses
In the univariate analysis, the following factors were statistically significant: age at onset less than 20 years, defecation difficulty, a history of mesalamine medication, and the type of fistula surgery (log rank P < 0.05). A history of abdominal surgery was marginally significant (P < 0.06) (Table 2). These factors were subsequently entered into a Cox proportional hazards model to test if they had significant independent effects.
Table 2. Univariate analysis.
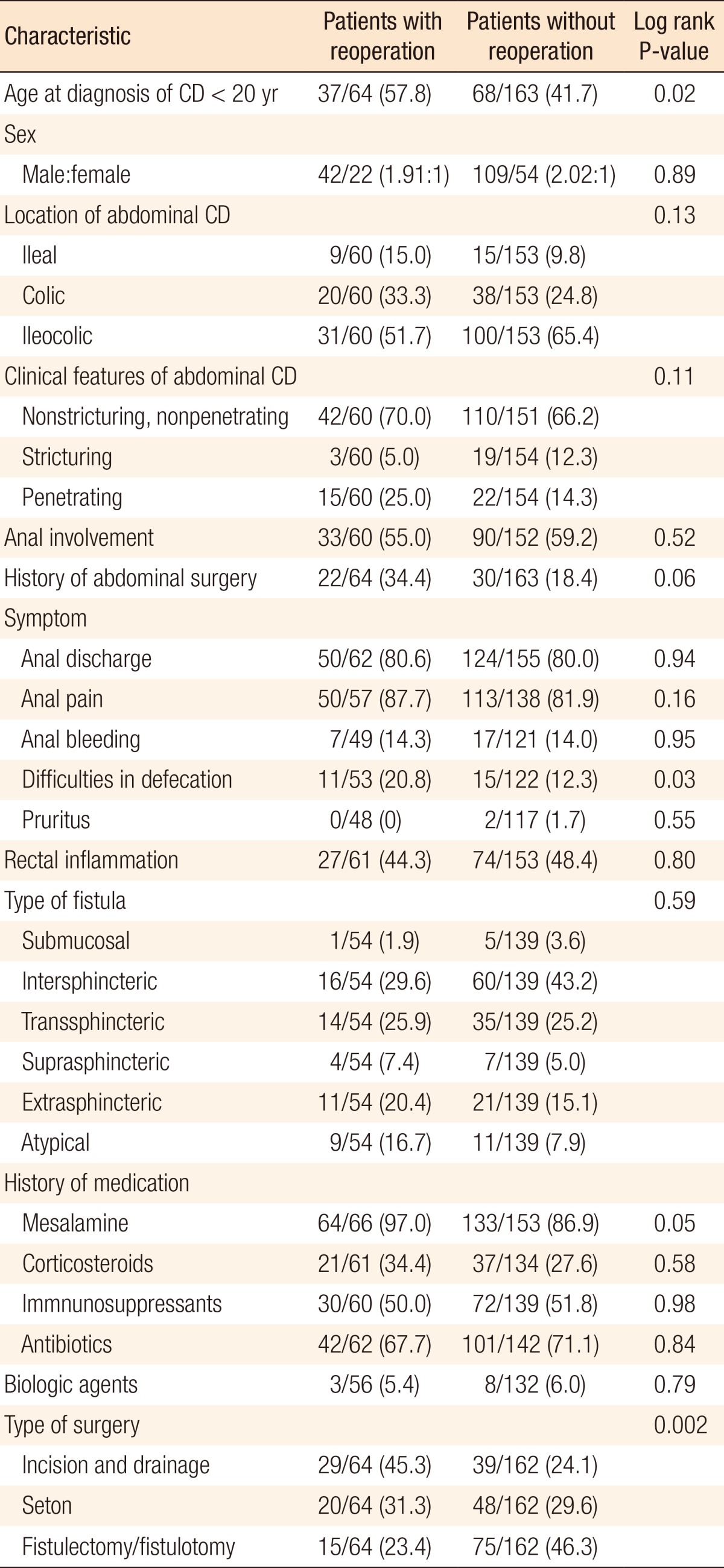
Values are presented as number (%).
CD, Crohn disease.
In the multivariate analysis, reoperation was significantly correlated with an onset age less than 20 years (hazards ratio [HR], 1.93; 95% confidence interval [CI], 1.07-3.48; P = 0.03), a history of abdominal surgery (HR, 1.99; 95% CI, 1.08-3.64; P = 0.03), and the type of surgery. Among the types of surgery, compared with incision and drainage, the fistulotomy and the fistulectomy were associated with a decreased incidence of reoperation (HR, 0.19; 95% CI, 0.09-0.42; P < 0.001) (Table 3).
Table 3. Multivariate analysis.
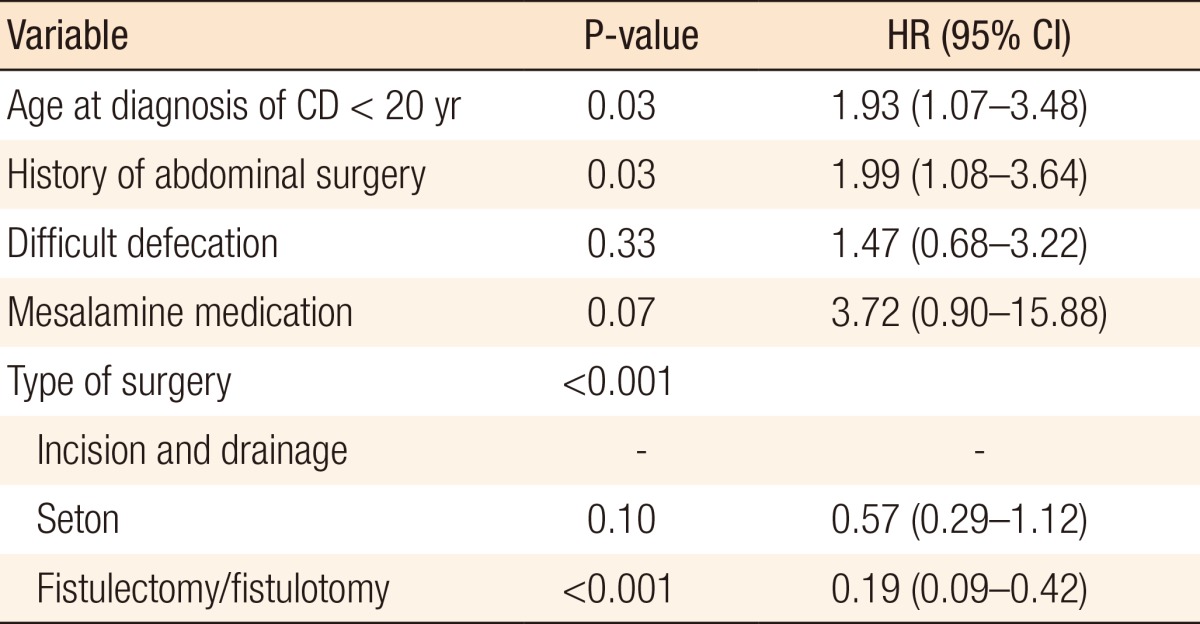
CI, confidence interval; HR, hazard ratio; CD, Crohn disease.
DISCUSSION
We know that perianal complications are common in patients with CD; however, the reported incidence of PCD varies widely. In the literature, the incidence rate ranges from approximately 13% to 27% in population-based studies and from 35% to 45% in studies from tertiary referral centers [4,5,7]. Some surgical groups have reported incidence rates as high as 78% [3]. According to the data from Korea, the incidence of perianal CD is about 37% to 50% [14,15,16]. This wide variation in incidence rates may be due to selection bias. To minimize such errors, we attempted to include patients from various hospitals in our medical referral system, such as colorectal-specializing hospitals and secondary and tertiary referral hospitals. This is the first multicenter study analyzing the risk factors for reoperation in patients with PCD in Korea.
Although PCD is a surgical challenge, surgical intervention is indispensible for some patients with PCD, such as those with symptomatic perianal abscesses, perianal fistulas, or anal stricture. The primary goals of surgery in patients with PCD are to cure the perianal disease and to preserve continence. Therefore, knowledge of the appropriate indicators of surgery and an ability to predict the postoperative clinical course are very important because repeated operations may increase the risk of sphincter injury, which can have a subsequent devastating effect on the quality of life.
Despite a multitude of clinical studies, possible risk factors for recurrence in PCD remain poorly defined. According to previous studies on abdominal CD, a variety of factors are suspected of being associated with the risk of repeat surgical treatment, including the female sex, perianal disease, upper gastrointestinal bowel involvement, and penetrating or stricture disease. The only factor to be confirmed is smoking [17,18,19,20,21]. Patients with CD who smoke have been reported to have a 2.5-fold increased risk of surgical recurrence [18]. In a multicenter study conducted by the 'Korean Study Group for IBD', young age, stricturing behavior, intra-abdominal abscess, emergency surgery, and delayed diagnosis after surgery were identified as possible risk factors for repeat abdominal surgery in luminal CD patients [22]. However, clinical studies concerning the risk factors for reoperation in PCD patients are rare.
An early age at diagnosis is known to be associated with more complicated CD. Some studies have suggested that a younger age at diagnosis (<20 years) is associated with greater small bowel involvement, more stricturing disease, and a higher frequency of surgery [23]. According to our results, young onset age is not only associated with a more complicated clinical course and a more frequent need for surgical intervention but also seems to be associated with poor surgical outcome after perianal surgery for PCD. Therefore, one should be cautious in pursuing perianal surgery in PCD. Moreover, considering that perianal problems predate the diagnosis of CD in approximately 10%-17%, one should be careful in addressing complicated perianal diseases, particularly those of young patients.
In our study, the CD patients who had previously undergone abdominal surgery showed higher incidences of reoperation after perianal surgery. Some reports have suggested that PCD is a risk factor for abdominal CD reoperation [17,18]; therefore, an interesting finding is that the history of abdominal surgery for CD can be inversely associated with an increased risk of reoperation for PCD. Regueiro et al [20]. reported, in their randomized controlled study, that administration of anti-TNF after an intestinal resection effectively prevented the recurrence of CD. We wonder if administration of anti-TNF after intestinal resection will be effective in preventing perianal operations as well as abdominal reoperations.
Although conservative treatment is generally recommended for patients with CD perianal fistulas, patients with simple perianal fistulas without proctitis may be treated with a fistulotomy or a fistulectomy, with reported healing rates of up to 85% [24,25]. In our study, we found that a fistulotomy and a fistulectomy were associated with a decreased incidence of reoperation in comparison with incision and drainage. However, we should be careful in interpreting these results because surgical procedures are individualized depending on the severity and the complexity of the perianal disease. For example, in a case with more infiltrative abscesses or complex fistulas, aggressive treatment such as a fistulotomy or a fistulectomy is not indicated. In fact, our study was intended to evaluate the clinical course of PCD, not to compare the effectiveness of each surgical procedure.
Our study has some limitations. First, missing data caused by incomplete follow-up made the interpretation of the results difficult and confusing. In some items, such as clinical symptoms, disease location, and family history, the rates of missing data were more than 10%. This study was retrospective, and data were collected from multiple hospitals; therefore, further review of the collected data was not possible. Second, although smoking was reported to be one of the most important factors that could affect the prognosis for CD, smoking habits were not investigated in our study. Third, whether medications such as immunosuppressive or anti-TNF agents had been administered before or after surgery and how long those medications had been used was unclear. In particular, postoperative anti-TNF was a promising treatment in some reports concerning small bowel CD [20]; therefore, a large-scale, controlled study should be completed to evaluate its postoperative effectiveness in treating patients with PCD. Unfortunately, our results did not show a significant difference in reoperation rates between patients treated and those not treated with anti-TNF. However, the number of patients who used anti-TNF was very small (5.8%) in our study because biologic agents were not widely available in Korea during our study period.
In conclusion, we found that a young onset age (<20 years) and a history of abdominal surgery were associated with a high risk of reoperation for perianal CD. In addition, the risk of reoperation was relatively low in the patients who had undergone a fistulotomy or a fistulectomy.
ACKNOWLEDGMENTS
The authors thank the members of the Korean IBD Study Group for their contribution in data acquisition. This multicenter study was funded by the Korean Society of Coloproctology.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Shin DH, Sinn DH, Kim YH, Kim JY, Chang DK, Kim EJ, et al. Increasing incidence of inflammatory bowel disease among young men in Korea between 2003 and 2008. Dig Dis Sci. 2011;56:1154–1159. doi: 10.1007/s10620-010-1403-2. [DOI] [PubMed] [Google Scholar]
- 2.Yang SK, Yun S, Kim JH, Park JY, Kim HY, Kim YH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008;14:542–549. doi: 10.1002/ibd.20310. [DOI] [PubMed] [Google Scholar]
- 3.Harper PH, Fazio VW, Lavery IC, Jagelman DG, Weakley FL, Farmer RG, et al. The long-term outcome in Crohn's disease. Dis Colon Rectum. 1987;30:174–179. doi: 10.1007/BF02554332. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz DA, Loftus EV, Jr, Tremaine WJ, Panaccione R, Harmsen WS, Zinsmeister AR, et al. The natural history of fistulizing Crohn's disease in Olmsted County, Minnesota. Gastroenterology. 2002;122:875–880. doi: 10.1053/gast.2002.32362. [DOI] [PubMed] [Google Scholar]
- 5.Hellers G, Bergstrand O, Ewerth S, Holmstrom B. Occurrence and outcome after primary treatment of anal fistulae in Crohn's disease. Gut. 1980;21:525–527. doi: 10.1136/gut.21.6.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nielsen OH, Rogler G, Hahnloser D, Thomsen OO. Diagnosis and management of fistulizing Crohn's disease. Nat Clin Pract Gastroenterol Hepatol. 2009;6:92–106. doi: 10.1038/ncpgasthep1340. [DOI] [PubMed] [Google Scholar]
- 7.Eglinton TW, Barclay ML, Gearry RB, Frizelle FA. The spectrum of perianal Crohn's disease in a population-based cohort. Dis Colon Rectum. 2012;55:773–777. doi: 10.1097/DCR.0b013e31825228b0. [DOI] [PubMed] [Google Scholar]
- 8.Tang LY, Rawsthorne P, Bernstein CN. Are perineal and luminal fistulas associated in Crohn's disease? A population-based study. Clin Gastroenterol Hepatol. 2006;4:1130–1134. doi: 10.1016/j.cgh.2006.06.021. [DOI] [PubMed] [Google Scholar]
- 9.Lapidus A, Bernell O, Hellers G, Lofberg R. Clinical course of colorectal Crohn's disease: a 35-year follow-up study of 507 patients. Gastroenterology. 1998;114:1151–1160. doi: 10.1016/s0016-5085(98)70420-2. [DOI] [PubMed] [Google Scholar]
- 10.Beaugerie L, Seksik P, Nion-Larmurier I, Gendre JP, Cosnes J. Predictors of Crohn's disease. Gastroenterology. 2006;130:650–656. doi: 10.1053/j.gastro.2005.12.019. [DOI] [PubMed] [Google Scholar]
- 11.Tarrant KM, Barclay ML, Frampton CM, Gearry RB. Perianal disease predicts changes in Crohn's disease phenotype-results of a population-based study of inflammatory bowel disease phenotype. Am J Gastroenterol. 2008;103:3082–3093. doi: 10.1111/j.1572-0241.2008.02212.x. [DOI] [PubMed] [Google Scholar]
- 12.Williams DR, Coller JA, Corman ML, Nugent FW, Veidenheimer MC. Anal complications in Crohn's disease. Dis Colon Rectum. 1981;24:22–24. doi: 10.1007/BF02603444. [DOI] [PubMed] [Google Scholar]
- 13.Fichera A, Michelassi F. Surgical treatment of Crohn's disease. J Gastrointest Surg. 2007;11:791–803. doi: 10.1007/s11605-006-0068-9. [DOI] [PubMed] [Google Scholar]
- 14.Ye BD, Yang SK, Cho YK, Park SH, Yang DH, Yoon SM, et al. Clinical features and long-term prognosis of Crohn's disease in Korea. Scand J Gastroenterol. 2010;45:1178–1185. doi: 10.3109/00365521.2010.497936. [DOI] [PubMed] [Google Scholar]
- 15.Kim HD, Kim CG, Kim JW, Kim SG, Kim BG, Kim JS, et al. Clinical features and therapeutic responses of perianal lesions in Crohn's disease. Korean J Gastroenterol. 2003;42:128–133. [PubMed] [Google Scholar]
- 16.Kim JY, Yang SK, Byeon JS, Myung SJ, Choe JW, Jo JY, et al. The incidence and natural history of perianal fistulas in Korean patients with Crohn's disease. Intest Res. 2006;4:22–31. [Google Scholar]
- 17.Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn's disease. Ann Surg. 2000;231:38–45. doi: 10.1097/00000658-200001000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reese GE, Nanidis T, Borysiewicz C, Yamamoto T, Orchard T, Tekkis PP. The effect of smoking after surgery for Crohn's disease: a meta-analysis of observational studies. Int J Colorectal Dis. 2008;23:1213–1221. doi: 10.1007/s00384-008-0542-9. [DOI] [PubMed] [Google Scholar]
- 19.Simillis C, Yamamoto T, Reese GE, Umegae S, Matsumoto K, Darzi AW, et al. A meta-analysis comparing incidence of recurrence and indication for reoperation after surgery for perforating versus nonperforating Crohn's disease. Am J Gastroenterol. 2008;103:196–205. doi: 10.1111/j.1572-0241.2007.01548.x. [DOI] [PubMed] [Google Scholar]
- 20.Regueiro M, Schraut W, Baidoo L, Kip KE, Sepulveda AR, Pesci M, et al. Infliximab prevents Crohn's disease recurrence after ileal resection. Gastroenterology. 2009;136:441–450.e1. doi: 10.1053/j.gastro.2008.10.051. [DOI] [PubMed] [Google Scholar]
- 21.Gao X, Yang RP, Chen MH, Xiao YL, He Y, Chen BL, et al. Risk factors for surgery and postoperative recurrence: analysis of a south China cohort with Crohn's disease. Scand J Gastroenterol. 2012;47:1181–1191. doi: 10.3109/00365521.2012.668931. [DOI] [PubMed] [Google Scholar]
- 22.Lee KY, Yu CS, Lee KY, Cho YB, Park KJ, Choi GS, et al. Risk factors for repeat abdominal surgery in korean patients with Crohn's disease: a multi-center study of a Korean inflammatory bowel disease study group. J Korean Soc Coloproctol. 2012;28:188–194. doi: 10.3393/jksc.2012.28.4.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Polito JM, 2nd, Childs B, Mellits ED, Tokayer AZ, Harris ML, Bayless TM. Crohn's disease: influence of age at diagnosis on site and clinical type of disease. Gastroenterology. 1996;111:580–586. doi: 10.1053/gast.1996.v111.pm8780560. [DOI] [PubMed] [Google Scholar]
- 24.Williams JG, Farrands PA, Williams AB, Taylor BA, Lunniss PJ, Sagar PM, et al. The treatment of anal fistula: ACPGBI position statement. Colorectal Dis. 2007;9(Suppl 4):18–50. doi: 10.1111/j.1463-1318.2007.01372.x. [DOI] [PubMed] [Google Scholar]
- 25.Sangwan YP, Schoetz DJ, Jr, Murray JJ, Roberts PL, Coller JA. Perianal Crohn's disease: results of local surgical treatment. Dis Colon Rectum. 1996;39:529–535. doi: 10.1007/BF02058706. [DOI] [PubMed] [Google Scholar]