Abstract
Background
Whether postoperative subsyndromal delirium (SSD) is a separate syndrome from delirium and has clinical relevance is not well understood.
Objectives
We sought to investigate SSD in older surgical patients and to determine its prognostic significance.
Methods
We performed a prospective cohort study of patients aged ≥65 years of age scheduled for noncardiac surgery. Postoperative delirium was determined using the Confusion Assessment Method. SSD was defined as the presence of at least one out of a possible 10 symptoms of delirium, as defined by the Confusion Assessment Method, but not meeting criteria for delirium.
Results
The number of features of SSD on the first postoperative day was associated with the subsequent development of delirium on the next day, after controlling for other risk factors. Compared to a patient with no SSD features, a patient with one SSD feature was 1.07 times more likely to have delirium on the next day (95% CI 0.42, 2.53), 2 features – 3.32 times more likely (95% CI 1.42. 7.57), and ≥ 2 features - 8.37 times more likely (95% CI 4.98, 14.53). Furthermore, there was a significant relationship between the number of features of SSD and increased length of hospital stay, and worsened functional status at one month after surgery.
Conclusions
SSD is prevalent in at risk surgical patients and has prognostic significance. Only one symptom of SSD was sufficient to cause a significant increase in hospital length of stay and further decline in functional status. These results suggest that monitoring for SSD is indicated in at risk patients.
Keywords: Subsyndromal, delirium, surgery, postoperative
INTRODUCTION
Previous work has characterized subsyndromal delirium (SSD) as an alteration in level of consciousness and cognition with severity and number of symptoms in between that of patients without delirium and those who meet DSM-IV criteria for delirium (1, 2). However, the definition of SSD is not uniformly agreed upon. Some researchers have defined SSD as having at least two or more a priori selected core symptoms (2–4) while others have focused on specific attentional and cognitive impairments (5) or have used specific cut-off points on diagnostic scales for delirium (6, 7). Research to date has been predominately in nonsurgical hospitalized elderly or those in long-term care, with few studies in postoperative patients. Furthermore, controversy exists as to whether the difference between SSD and delirium is a quantitative or qualitative one (2) and it is unclear whether SSD represents a “pre-delirious” or prodromal state heralding the potential onset of the full-fledged disorder, the residual symptoms of a resolving delirium and thus part of a continuum of symptoms, or a distinct clinical syndrome.
Because of limited data in the postoperative patients, the goals of this study were: 1) to determine if patients who did not meet criteria for delirium but had features of delirium progressed to full delirium, and 2) to determine whether SSD was associated with certain clinical outcomes, such as hospital length of stay, and post-discharge cognitive and physical functioning. We hypothesized that SSD was prevalent and had prognostic importance in predicting important clinical outcomes such as length of hospital stay and functional deterioration.
MATERIALS & METHODS
Study patients
Patients were all subjects 65 years of age or older admitted to a tertiary care academic teaching hospital undergoing major noncardiac surgery requiring anesthesia. Additional inclusion criteria included the anticipated hospital length of stay to be at least 2 days in duration, and fluency in English. A convenient sampling was used in that patients were recruited for surgical procedures conducted from Mondays to Wednesdays, to allow the postoperative follow up to be conducted during a regular work-week. Prior known dementia was not an exclusion criterion but patients were excluded if they did not comprehend the study procedures. Patients recruited between 2001–2012 were included in this report. Written informed consent from all patients was obtained preoperatively. The study was approved by the institutional review board. The study was part of a larger study to evaluate the pathophysiology of postoperative delirium. A subset of 215 patients in this study was included in a previously published study that did not consider SSD (8).
Measurements
At study enrollment, a research assistant collected demographic and clinical data. Activities of daily living and instrumental activities of daily living were assessed preoperatively, typically within one week of the planned surgery. Cognitive status was also measured before surgery, using a battery of tests including the Semantic Verbal Fluency Test, word list, Digit Symbol Test, and the Telephone Interview of Cognitive Status. The Telephone Interview of Cognitive Status is an 11-item screening test that was originally developed to assess cognitive function in patients with Alzheimer’s dementia who were unable to be evaluated in person (9). It has been compared to the Mini Mental State exam and found to have scores that correspond closely, allowing for a standardized comparator (10). Cognitive status was assessed again daily for the first two postoperative days. Patients were assessed preoperatively and daily after surgery for delirium using the Confusion Assessment Method. The Confusion Assessment Method has been validated as a diagnostic tool for delirium based on four core features, including acute onset and fluctuating course, inattention, disorganized thinking, and altered level of consciousness (11). Delirium requires the presence of the first two features plus either feature 3 (disorganized thinking), or features 4 (altered level of consciousness). In those who did not meet criteria for delirium, SSD was defined as the presence of at least one out of a possible 10 symptoms of delirium, as defined by the detailed Confusion Assessment Method inventory (acute onset, inattention, fluctuation, disorganized thinking, altered level of consciousness, disorientation, memory impairment, perceptual disturbances, psychomotor agitation or retardation, altered sleep-wake cycle). The subtypes of delirium (hypoactive vs. hyperactive) were defined per the CAM manual. If a patient demonstrated increased level of motor activity during he interview such as restlessness, picking at bedclothes, tapping fingers or making frequent sudden changes in position, that patient was considered as having hyperactivity. In contrast, if a patient had an unusually decreased level of motor activity such as sluggishness, starring into space, staying in one position for a long time, or moving very slowly, that patient is considered to have hypoactivity. All measurements were performed by trained study assistants. For analytic purpose, patients were categorized as having delirium, no delirium but have features of SSD, and no delirium or SSD at all.
At 30 days after surgery, patients were contacted by phone to evaluate cognitive status by Telephone Interview of Cognitive Status, and self reported activities of daily living and instrumental activities of daily living.
Statistical analysis
Chi-squared and analysis of variance (ANOVA) tests were used to analyze bivariate associations between cognitive status and patient characteristics (Table 2). Logistic regression with backwards variable selection was used to analyze the relationship between the number of SSD features on postoperative day one and subsequent delirium on day two while adjusting for covariates (Table 3). Similarly, for hospital length of stay, linear regression analysis using backwards variable selection was used to determine its relationship with the number of features of SSD while adjusting for co-variates. Chi-squared tests were used to assess the relationship between change in activities of daily living and instrumental activities of daily living functionality and postoperative cognitive status (Table 5).
Table 2.
Patient characteristics by cognitive status on the first postoperative day.
| SSD & Delirium- free n = 264 |
SSD n = 172 |
Delirium n = 195 |
P Value | |
|---|---|---|---|---|
| Mean Age* (SD) | 72.4 (5.9) | 73.7 (5.8) | 74.6 (6.3) | <.001 |
| Gender (Male %)* | 158 (60%) | 82 (48%) | 74 (38%) | <.001 |
| Race (White %) | 233 (88%) | 155 (91%) | 161 (83%) | .055 |
| Charlson Score (SD) | 1.5 (1.8) | 1.5 (1.7) | 1.5 (1.7) | .865 |
| CNS disorders (Yes %)* | 121 (46 %) | 88 (51%) | 114 (58%) | .028 |
| Baseline Cognitive Status (SD) * | 33.3 (3.3) | 32.2 (4.1) | 31.0 (4.5) | <.001 |
| Preoperative use of Narcotics (%) | 66 (25%) | 58 (34%) | 69 (35%) | .031 |
| Preoperative use of benzodiazepine (%) | 31 (12%) | 28 (17%) | 28 (15%) | .459 |
| Surgery duration* (SD) | 4.50 (1.75) | 5.00 (2.76) | 5.30 (3.35) | .012 |
| Baseline Preoperative Functional Status* | ||||
| ADL (% Yes) | 56 (21%) | 55 (32%) | 70 (36%) | .001 |
| IADL (% Yes) | 91 (35%) | 76 (44%) | 95 (49%) | .006 |
| Type of Surgery* | ||||
| Orthopedic/spine | 117 (52%) | 75 (49%) | 113 (62%) | .038 |
| Type of Anesthesia* | ||||
| General (compared to Regional) | 183 (69%) | 125 (73%) | 137 (70%) | .784 |
Percentages calculated by conditioning on cognitive status (column %). P values calculated by ANOVA (Age, Charlson Score, surgery duration) or Chi Squared (Gender, Race, CNS Disorders, Preoperative use of narcotics, Preoperative use of benzodiazepine, Baseline ADL, Baseline IADL, Type of Surgery, Type of Anesthesia) tests.
ADL = activities of daily living, CNS = central nervous system disorder, IADL = instrumental activities of daily living, SD = standard deviation
Table 3.
Logistic regression results assessing the association of symptoms of delirium on postoperative day 1 with subsequent delirium on postoperative day 2.
| P value | Mean Stay (95% CI) | Estimate (95% CI) | |
|---|---|---|---|
| Number of SSD Features | |||
| 0 features (ref) (n=256) | --- | 5.25 (4.55, 5.94) | |
| 1 feature (n=64) | .146 | 6.36 (5.01, 7.71) | -- |
| 2 features (n=49) | <.001 | 8.76 (7.18, 10.33) | |
| >2 features (n=231) | <.001 | 7.33 (6.61, 8.04) | |
| Charlson Score | .037 | - | .275 (.016, .534) |
| Length of Surgery (hours) | <.001 | .943 (.774, 1.11) | |
Logistic regression was used with diagnosis of delirium on day 2 as the response variable and number of subsyndromal delirium features on day 1 as the explanatory variable (0 features is the reference group).
The features refer to the presence of at least one out of a possible 10 symptoms of delirium, as defined by the CAM (acute onset, inattention, fluctuation, disorganized thinking, altered level of consciousness, disorientation, memory impairment, perceptual disturbances, psychomotor agitation or retardation, altered sleep wake cycle).
Table 5.
Activities of daily living – comparison of preoperative assessment to 30 days after surgery assessment in patients of various postoperative cognitive levels
| Change in activities of daily living (preoperative to 30 days postoperatively) | |||
|---|---|---|---|
| ADL | Deterioration n = 111 |
No Change n = 156 |
Improvement n = 29 |
| SSD & delirium free | 30 (25.2%) | 79 (66.4%) | 10 (8.4%) |
| SSD (at least one feature) | 32 (36.8%) | 46 (52.9%) | 9 (10.3%) |
| Delirium (Yes) | 49 (54.4%) | 31 (34.4%) | 10 (11.1%) |
| Change in instrumental activities of daily living (preoperative to 30 days postoperatively) | |||
|---|---|---|---|
| IADL | Deterioration n = 130 |
No Change n = 126 |
Improvement n = 37 |
| SSD & delirium free | 35 (29.4%) | 69 (58.0%) | 15 (12.6%) |
| SSD (at least one feature) | 44 (51.1%) | 32 (37.2%) | 10 (11.6%) |
| Delirium (Yes) | 51 (58.0%) | 25 (28.4%) | 12 (13.6%) |
P-Value <.001
RESULTS
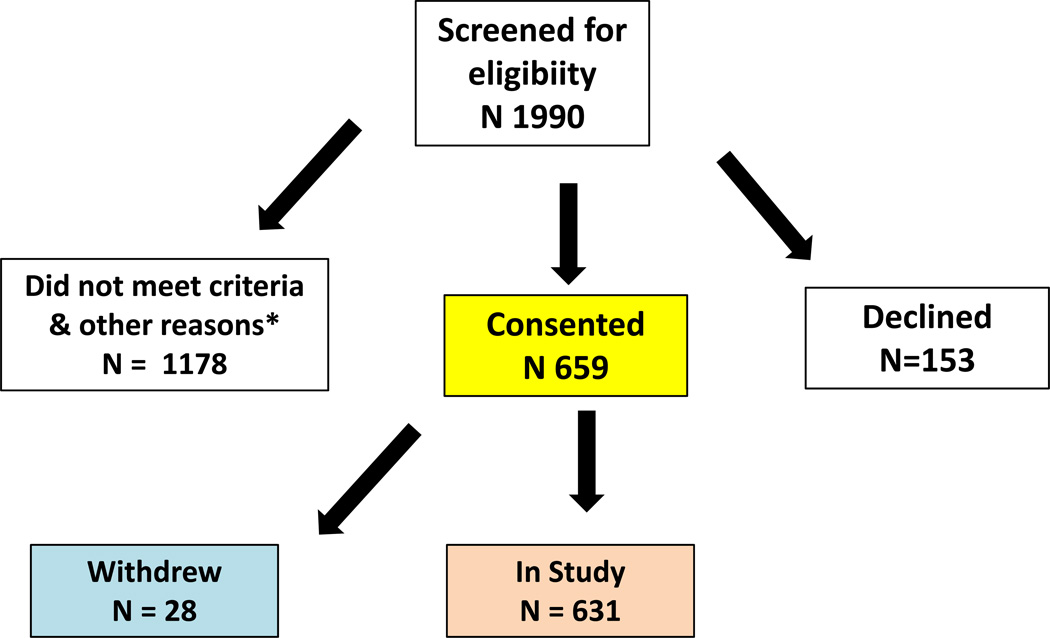
631 patients with delirium assessments were included in this study. The recruitment scheme is shown in figure 1. On the first postoperative day, 172 patients (27%) had features of SSD, and 195 (31%) had delirium. On the second postoperative day, 603 patients were evaluated because 25 patients were discharged early, 2 patients refused testing and one was not available for testing. Overall, there were 144 patients (24%) with SSD, and 183 (30%) had delirium on the second postoperative day (Table 1). The most commonly observed symptoms of delirium in patients with SSD were altered level of consciousness (56.4% on hospital day one, 54.2% on hospital day two), psychomotor retardation (37.8% on hospital day one, 36.1% on hospital day two), and altered sleep-wake cycle (37.9% on hospital day one, 29.9% on hospital day two). We also determined the prevalence of hyperactive vs. hypoactive delirium subtypes. Overall, the proportion of patients with hyperactivity was not significantly different in patients with delirium compared to those with SSD (52/195=26.7% vs. 47/172=27.3%, P=0.91). In contrast, the proportion of patients with hypoactivity was significantly higher in patients with delirium vs. those with SSD (160/195=82.1% vs. 75/172=43.6%), P<0.001).
Figure 1.
Our study used a convenient sampling method. Only patients scheduled for surgery on Mondays to Wednesdays were recruited to allow postoperative follow up to be completed in a regular work week. The asterisk represents patients who were not recruited because of non-English speaking, not undergoing general anesthesia, did not have time to recruit, surgery cancellation, etc.
Table 1.
Patients who are SSD and delirium free, with CAM diagnosed delirium, and subsyndromal delirium are summarized by postoperative day.
| Postoperative Day 1 | Postoperative Day 2 | |
|---|---|---|
| SSD and delirium free | 264 (42%) | 274 (46%) |
| Subsyndromal delirium | 172 (27%) | 144 (24%) |
| Delirium | 195 (31%) | 183 (30%) |
The number and % in brackets in each cell represent the number of patients who had each of the condition described. The results were stratified by the first and second postoperative day. Note that the patients were classified as the “worse” mental state. The subsyndromal delirium (SSD) and delirium free group never developed either SSD or delirium, the SSD group only had SSD, and the delirium group had delirium.
The patient characteristics between the three cognitive status groups - those who were SSD- and delirium-free, SSD, and delirium, are shown in Table 2. Overall significant differences in age, gender, a history of central nervous system disorders, baseline cognitive status, preoperative use of narcotics, surgery duration, preoperative activities of daily living and instrumental activities of daily living, and type of surgery were found between the three different cognitive status groups. The sub-types of central nervous system disorders are shown in table 4. The most prevalent neurological disorders at baseline was a history of or current depression, history of delirium, or a history of cerebrovascular disease. There were no differences between the three groups in race or Charlson co-morbidity scores. Because this was an observational cohort study, the anesthetic and surgical management was not controlled. Overall, there is no significant difference in the types of anesthetics administered (general vs. regional) among the patients with delirium, SSD or SSD- and delirium-free (table 2). For patients who received a general anesthetic, typically a balanced anesthetic comprising of volatile and intravenous agents were administered.
Table 4.
Sub-types of central nervous system disorders during preoperative evaluation
| Delirium & SSD Free | SSD | Delirium | P-Value | |
|---|---|---|---|---|
| History of stroke | 9 (3.4%) | 12 (7.0%) | 6 (3.1%) | .139 |
| History of TIA | 16 (6.1%) | 8 (4.7%) | 7 (3.6%) | .491 |
| Current Depression (%) | 31 (12.5%) | 28 (16.9%) | 28 (14.6%) | .459 |
| Seizure Disorders (%) | 2 (0.8%) | 5 (3.1%) | 5 (2.6%) | .156 |
| History of Delirium (%) | 41 (16.9%) | 36 (22.2%) | 49 (26.2%) | .064 |
| History of Dementia (%) | 3 (1.2%) | 2 (1.2%) | 7 (3.7%) | .155 |
| History of Depression (%) | 76 (31.4%) | 51 (31.5%) | 78 (41.5%) | .057 |
| Other CNS Disease (%) | 9 (8.3%) | 8 (9.9%) | 16 (14.0%) | .455 |
Other CNS Disease includes other miscellaneous conditions such as Parkinson’s disease, multiple sclerosis, migraine, restless leg syndrome, etc.
Results of a logistic regression analysis using backwards variable selection with the variables in Table 2 as candidates revealed that, among patients who did not meet criteria for delirium on day 1, the number of features of SSD on day 1, age, Charlson score, length of surgery and surgery type were significantly related to subsequent development of delirium. Specifically, increases in age, Charlson score, length of surgery and surgery type were associated with an increased risk of delirium on day 2. Compared to a patient having no SSD features, a patient with one SSD feature was 1.07 (95% CI 0.42, 2.53) times more likely to have delirium on the next day, 2 features - 3.32 (95% CI 1.42, 7.57) times more likely, and more than two features - 8.37 (95% CI 4.98, 14.53) times more likely to have delirium (Table 3).
When hospital length of stay was evaluated, results of a linear regression analysis using backwards variable selection with the variables in Table 2 as candidates revealed that the number of features of SSD, Charlson score, and length of surgery were significantly associated with hospital length of stay. Specifically, increases in Charlson score and length of surgery were associated with an increase in hospital length of stay. Patients who were SSD- and delirium free had an average length of hospital stay of 5.25 days (95% CI 4.55, 5.94), and this increased to 6.36 days (95% CI 5.01, 7.71) with one feature of delirium, 8.76 days (95% CI 7.18, 10.33) with two features, and 7.33 days (95 CI 6.61, 8.04) with more than two features. In comparison, the average hospital length of stay for patients with delirium on day one was 8.1 ± 7.4 days.
In terms of post-discharge functional outcomes which included the measurements of activities of daily living and instrumental activities of daily living at 30 days after surgery, patients with either postoperative delirium or SSD had an increased likelihood of becoming further dependent in one or more categories in activities of daily living or instrumental activities of daily living compared to patients who were free of SSD and delirium (Table 5). In contrast, cognitive status as assessed by Telephone Interview of Cognitive Status at 30 days after surgery was not significantly different between the three groups.
DISCUSSION
We prospectively examined a cohort of older patients undergoing noncardiac surgery requiring general anesthesia. One third of these patients developed delirium on postoperative day one, while over a quarter had SSD. This pattern remained relatively unchanged on the second postoperative day. A novel finding in our study is that patients with SSD who had a greater number of symptoms were more likely to progress to full delirium on the next day. Furthermore, patients with SSD had increased length of hospital stay after adjusting for covariates and developed new dependency activities of daily living and instrumental activities of daily living at 30 days follow up.
Comparison with previous studies
Our finding that patients with SSD were more likely to progress to delirium is supported by previous investigations examining the number of delirium core symptoms and progression to delirium. In a study of long term care residents, Cole et al. reported that the presence of delirium core symptoms at baseline assessment predicts incident delirium (12). These results also further support the concept of a continuum of illness rather than a categorical classification of delirium (4, 7). Moreover, our finding of approximately one quarter of patients having SSD is similar to that reported in medical patients. A recent systematic analysis suggested that SSD is a delirium spectrum disorder though findings were limited by significant heterogeneity between studies. The investigators estimated that there was a 23% prevalence and 13% incidence of SSD, and suggested that these percentages may be larger with more specific and frequent observations of mental status (4). However, depending on the criteria for defining SSD, the incidence does vary from one study to another (13).
In our study, the most commonly occurring SSD symptoms were altered level of consciousness, psychomotor retardation, and altered sleep-wake cycle, similar to previous work by Marquis and his co-investigators (14). Trzepacz and colleagues, in a recent study, pooled data derived from Delirium Rating Scale-Revised-98 (DRS-98) scores from a cohort of delirious adults and nondelirious controls in an attempt to clarify the phenomenology of SSD in order to identify core features of SSD. They found that SSD in general resembled delirium, and identified 3 core domains that differentiated it from nondelirium: attentional deficits, circadian abnormalities, and affective lability (15). Therefore, although there is some overlap in SSD symptomatology between our study and that of Trzepacz’s, such as in the area of sleep-wake cycle disturbance, there are differences in the core SSD symptoms between medical and surgical patients.
One additional novel finding in our study is that the prevalence of hypoactivity was higher in patients with delirium compared to those with SSD. The potential clinical implication of this finding is that delirium is likely underestimated in the clinical setting without a structured evaluation since the hypoactive form of delirium is less visible than the hyperactive form.
The other important finding in our study is the prognostic significance of postoperative SSD. Our study showed that there was a graded increase with respect to the number of SSD symptoms and the subsequent development of delirium. This finding is somewhat analogous to previous reports that SSD appears to be correlated with outcomes intermediate between that of patients who do not have delirium and those who are diagnosed as delirious (2, 3), though one study did not find a significant difference in outcomes such as hospital length of stay or need for post-hospital institutionalization for subjects with SSD and full delirium (7). These latter findings along with results from the current study suggest that even sub-threshold cases of delirium may have considerable influence on important clinical outcomes. In our study, a symptom burden as little as one feature of delirium significantly predicted a longer length of hospital stay. This highlights the importance of attending to all symptoms of delirium, not just specific core domains as suggested by recent research. Furthermore, we showed that the presence of SSD was associated with new dependence on activities of daily living and instrumental activities of daily living at 30 days after surgery, suggesting that patients who did not meet criteria of delirium but have features of SSD should be followed up with subsequent visits and evaluation. An alternative explanation of the post-discharge functional outcome may simply represent the associations between delirium and these outcomes. For example, our results showed that patients with SSD were likely to develop delirium and delirium was associated with worse functional outcomes, so these findings could represent the fact that patients with SSD became delirious and then had worse outcomes.
If SSD is prognostically important, can patients be identified by certain risk characteristics? In our study, the three groups differed in some demographic variables. Of note, older age, a history of central nervous system disease and poorer baseline functional status predictably were associated with subsyndromal and full delirium. This result is similar to that previously reported that risk factors for SSD appear to be similar to that for delirium, and patients most likely to develop full delirium have been found to have more severe and numerous risk factors for delirium (2, 4). Interestingly, females were more likely than males to have symptoms of delirium. This finding is likely secondary to the fact that in our cohort, more women than men underwent orthopedic surgery which was independently associated with an increased rate of postoperative delirium. Taken together, results from our current study combined with those from previous studies support the hypothesis that SSD is likely part of a continuum of delirium symptoms.
To date, the etiology of postoperative delirium and SSD is not clearly delineated. In a large study of patients undergoing hip fracture surgery, Brauer et al. reported that only 7% of episodes were assigned a definite cause (16). The American Geriatric Society recently published a comprehensive document on clinical guideline for the management of postoperative delirium (17) based on extensive literature review and expert panel consensus. Of the eight strong recommendations that were published, none of which identified a specific role of anesthetics or medications on the risk of postoperative delirium. Rather, non-pharmacologic multi-component therapy and optimizing postoperative pain management were two of the main areas that have been identified as key areas to target to reduce postoperative delirium. Thus, there is a critical need for more studies that are properly powered to determine the etiology of postoperative delirium and SSD.
Potential limitations
There are a few potential limitations of our study. First, we focused on the early postoperative period and measured delirium only on the first two postoperative days. Therefore, later cases of delirium would not have been captured. In addition, we did not include a tool to measure the severity of delirium, which should be considered in future studies of delirium and SSD. In our current study, we did not find any difference in cognitive status as measured by Telephone Interview of Cognitive Status at 30 days after surgery between patients with SSD vs. those without. It is possible that the absence of a difference in cognitive status at 30 days is that there truly is no difference, i.e., that individuals recovered cognitive function. Future studies with more sensitive and comprehensive measurement of cognitive status may be necessary to discern the relationship between postoperative SSD and subsequent cognitive status. Finally, we did not include patients undergoing outpatient operations requiring general anesthesia because of the difficulty in obtaining postoperative follow up. Given the large proportion of outpatient operations in most contemporary health care practice, future studies should include patients undergoing outpatient surgery.
Summary
Postoperative SSD was common in a cohort of older patients undergoing surgery. Moreover, the greater the symptom burden in the subsyndromal state, the higher the likelihood of subsequent delirium. Perhaps the most striking finding of this investigation was that just one symptom of SSD was sufficient to cause a significant increase in hospital length of stay and further decline in functional status. These results suggest that careful, regular screening is important to recognize such symptoms and mount appropriate interventions.
Table 6.
Instrumental activities of daily living – comparison of preoperative assessment to 30 days after surgery assessment in patients with subsyndromal delirium vs. those with delirium
| Change in instrumental activities of daily living (preoperative to 30 days postoperatively) | ||
|---|---|---|
| Deterioration | No Change | Improvement |
| 113 (44.3%) | 129 (43.3%) | 38 (12.7%) |
| Number of subsyndromal delirium features - Count (Row %) | |||
|---|---|---|---|
| Deterioration | No Change | Improvement | |
| 0 | 40 (31.2%) | 72 (56.3%) | 16 (12.5%) |
| 1 | 18 (51.4%) | 12 (34.3%) | 5 (14.3%) |
| 2 | 12 (48.0%) | 10 (40.0%) | 3 (12.0%) |
| 3+ | 63 (56.3%) | 35 (31.3%) | 14 (12.5%) |
| Delirium - Count (Row %) | |||
|---|---|---|---|
| Deterioration | No Change | Improvement | |
| No | 79 (38.5%) | 101 (49.3%) | 25 (12.2%) |
| Yes | 51 (58.0%) | 25 (28.4%) | 12 (13.6%) |
P = .005
P = .003
When comparing the instrumental activities of daily living (IADL) from before surgery to that measured at 30 days after surgery, patients with one or more features of SSD were more likely to have deterioration in IADL, defined as new dependency in one or more activities of IADL, when compared to those with no delirium or no subsyndromal delirium.
Acknowledgments
This project was supported in part by the National Institute of Aging, National Institutes of Health, Bethesda, MD, Grant # NIH 1RO1AG031795-05 (Leung).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
All authors attest that there are no conflicts of interest and all contribute to components of study design, data collection, data analysis and write-up of the manuscript
REFERENCES
- 1.Lipowski Z. Delirium (acute confusional states) JAMA. 1987;258:1789–1792. [PubMed] [Google Scholar]
- 2.Levkoff SELB, Cleary PD, Wetle T, Evans DA, Rowe JW, Lipsitiz LA. Subsyndromal Delirium. Am J Geriatric Psychiatry. 1996;4(4):320–329. doi: 10.1097/00019442-199622440-00006. [DOI] [PubMed] [Google Scholar]
- 3.Cole M, McCusker J, Dendukuri N, Han L. The prognostic significance of subsyndromal delirium in elderly medical inpatients. Journal of the American Geriatrics Society. 2003;51(6):754–760. doi: 10.1046/j.1365-2389.2003.51255.x. Epub 2003/05/22. [DOI] [PubMed] [Google Scholar]
- 4.Cole MG, Ciampi A, Belzile E, Dubuc-Sarrasin M. Subsyndromal delirium in older people: a systematic review of frequency, risk factors, course and outcomes. International journal of geriatric psychiatry. 2013;28(8):771–780. doi: 10.1002/gps.3891. Epub 2012/11/06. [DOI] [PubMed] [Google Scholar]
- 5.Lowery DP, Wesnes K, Brewster N, Ballard C. Subtle deficits of attention after surgery: quantifying indicators of sub syndrome delirium. International journal of geriatric psychiatry. 2010;25(10):945–952. doi: 10.1002/gps.2430. Epub 2010/01/08. [DOI] [PubMed] [Google Scholar]
- 6.Marcantonio E, Ta T, Duthie E, Resnick NM. Delirium severity and psychomotor types: their relationship with outcomes after hip fracture repair. Journal of the American Geriatrics Society. 2002;50(5):850–857. doi: 10.1046/j.1532-5415.2002.50210.x. [DOI] [PubMed] [Google Scholar]
- 7.Ouimet S, Riker R, Bergeron N, Cossette M, Kavanagh B, Skrobik Y. Subsyndromal delirium in the ICU: evidence for a disease spectrum. Intensive care medicine. 2007;33(6):1007–1013. doi: 10.1007/s00134-007-0618-y. Epub 2007/04/04. [DOI] [PubMed] [Google Scholar]
- 8.Vaurio LE, Sands LP, Wang Y, Mullen EA, Leung JM. Postoperative delirium: the importance of pain and pain management. Anesthesia and analgesia. 2006;102(4):1267–1273. doi: 10.1213/01.ane.0000199156.59226.af. Epub 2006/03/23. [DOI] [PubMed] [Google Scholar]
- 9.Desmond D, Tatemichi TK, Hanzawa L. The Telephone Interview for Cognitive Status (TICS): Reliabiility and validity in a stroke sample. International journal of geriatric psychiatry. 1994;9(10):803–807. [Google Scholar]
- 10.Fong TG, Fearing MA, Jones RN, Shi P, Marcantonio ER, Rudolph JL, et al. Telephone interview for cognitive status: Creating a crosswalk with the Mini-Mental State Examination. Alzheimer's & dementia : the journal of the Alzheimer's Association. 2009;5(6):492–497. doi: 10.1016/j.jalz.2009.02.007. Epub 2009/08/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Inouye S, van Dyke C, Alessi C, Balkin S, Siegal A, Horwitz R. Clarifying confusion: the confusion assessment method. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 12.Cole MG, McCusker J, Voyer P, Monette J, Champoux N, Ciampi A, et al. Symptoms of delirium predict incident delirium in older long-term care residents. Int Psychogeriatr. 2013;25(6):887–894. doi: 10.1017/S1041610213000215. Epub 2013/03/02. [DOI] [PubMed] [Google Scholar]
- 13.Meagher D, O'Regan N, Ryan D, Connolly W, Boland E, O'Caoimhe R, et al. Frequency of delirium and subsyndromal delirium in an adult acute hospital population. Br J Psychiatry. 2014;205(6):478–485. doi: 10.1192/bjp.bp.113.139865. Epub 2014/11/02. [DOI] [PubMed] [Google Scholar]
- 14.Marquis F, Ouimet S, Riker R, Cossette M, Skrobik Y. Individual delirium symptoms: do they matter? Critical care medicine. 2007;35(11):2533–2537. doi: 10.1097/01.ccm.0000284506.43390.f3. Epub 2007/12/18. [DOI] [PubMed] [Google Scholar]
- 15.Trzepacz PT, Franco JG, Meagher DJ, Lee Y, Kim JL, Kishi Y, et al. Phenotype of subsyndromal delirium using pooled multicultural Delirium Rating Scale--Revised-98 data. Journal of psychosomatic research. 2012;73(1):10–17. doi: 10.1016/j.jpsychores.2012.04.010. Epub 2012/06/14. [DOI] [PubMed] [Google Scholar]
- 16.Brauer C, Morrison RS, Silberzweig SB, Siu AL. The cause of delirium in patients with hip fracture. Archives of internal medicine. 2000;160(12):1856–1860. doi: 10.1001/archinte.160.12.1856. [DOI] [PubMed] [Google Scholar]
- 17.Inouye S, Robinson T, Blaum C, Busby-Whitehead J, Boustani M, Chalian A, et al. American Geriatrics Society abstracted clinical practice guideline for postoperative delirium in older adults. Journal of the American Geriatrics Society. 2015;63(1):142–150. doi: 10.1111/jgs.13281. Epub 2014/12/17. [DOI] [PMC free article] [PubMed] [Google Scholar]