Abstract
Irregular hypoechoic masses in the breast do not always indicate malignancies. Many benign breast diseases present with irregular hypoechoic masses that can mimic carcinoma on ultrasonography. Some of these diseases such as inflammation and trauma-related breast lesions could be suspected from a patient's symptoms and personal history. Careful ultrasonographic examination and biopsy could help to differentiate these from malignancies.
Keywords: Breast, Ultrasonography, Neoplasm
INTRODUCTION
Ultrasonography (US) is an essential tool for evaluating breast masses. In the Breast Imaging Reporting and Data System (BI-RADS) and lexicon for US established by the American College of Radiology, breast lesions are classified as benign category 2, likely benign category 3, suspicious for malignancy category 4 (a-c), and highly suggestive of malignancy category 5. This classification is based on the sonographic features of breast lesions including shape, margin, orientation, echo pattern, and posterior features (1).
Irregular hypoechoic masses on breast ultrasound are usually considered suspicious lesions. If the lesions combine other features of malignancy such as spiculated margin, nonparallel orientation and posterior shadowing, they are considered moderate and highly suspicious for malignancy (BI-RADS categories 4b and 4c) or highly suggestive of malignancy (BI-RADS category 5). However, lesions with benign features such as a circumscribed margin are classified as low suspicion (BI-RADS category 4a) (2). BI-RADS category 4 lesions are known to have a broad range of malignancy rates (3-94%). There are various histopathologic results for US BI-RADS category 4 lesions (3, 4). Taskin et al. (3) found that the benign histopathologic diagnoses of these lesions on US were fibroadenoma (38%), sclerosing adenosis (18%), fibrocystic changes (FCCs) (14%), mastitis-inflammation (9.5%), intraductal papillomas (5.5%), focal fibroses (5%), atypical ductal hyperplasias (2.5%), fat necroses (2.5%), phyllodes tumors (1%), tubular adenomas (0.5%), epidermal inclusion cysts (0.5%), and others (3.5%).
In this review article, we classify benign breast lesions that show irregular hypoechoic masses on US into 4 groups: iatrogenic or trauma-related breast lesions (foreign body reaction, fat necrosis, fibrotic scar), inflammations (abscess, idiopathic granulomatous lobular mastitis [IGLM], diabetic mastopathy [DMP]), proliferative diseases (sclerosing adenosis, apocrine metaplasia, FCC), and benign breast tumors (intraductal papilloma, fibroadenoma, tubular adenoma).
Iatrogenic or Trauma-Related Breast Lesions
Foreign Body Reaction
Numerous foreign bodies are introduced into the human organism during surgery or trauma as well as after exposure to some chemical substances. They may cause an inflammatory reaction such as granuloma (5). Reported foreign matter has included suture materials, carbon particles used for localization, gunpowder, and injected foreign materials such as silicone or paraffin (5,6).
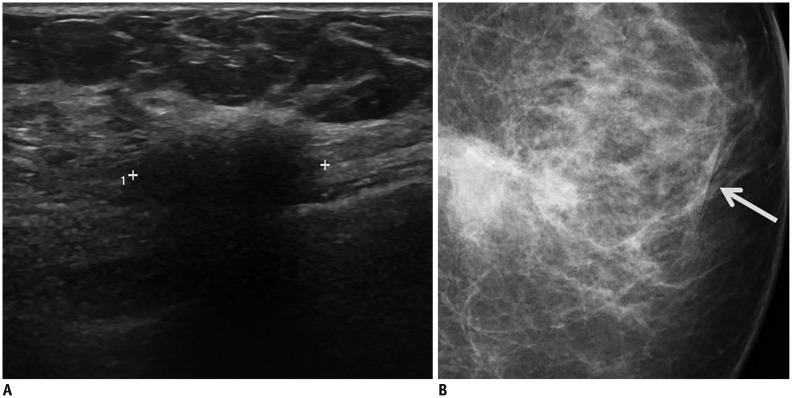
On mammography, foreign body reactions can be seen as calcifications or microcalcifications but can also be seen as a mass that simulates malignancy because of its ill-defined or partially circumscribed margin (6,7). At US, the lesion can show an irregular spiculated hypoechoic mass (Fig. 1). Magnetic resonance images (MRI) can show varying signal intensity depending on materials, and some cases reported that the lesions showed hypointense signal intensity on all spin-echo images caused by fibrosis (5).
Fig. 1. Foreign body reaction in 61-year-old woman with history of breast augmentation and removal (material: unknown).
A. Transverse ultrasonography image shows irregular spiculated hypoechoic mass with posterior shadowing. B. Left craniocaudal mammogram shows irregular obscured hyperdense mass with overlying skin thickening (arrow) in left breast lower inner quadrant.
Fat Necrosis
Fat necrosis usually results from surgery or radiation therapy, but some cases result from accidental trauma. When it develops, the lesion appears as a hemorrhage in fat, and it becomes demarcated, forming a distinct yellow-gray mass with or without some reddish portion after several weeks. Cystic degeneration makes a cavity containing oily fluid secondary to the necrotic fat (8). Because of the variability in the inflammatory process, fat necrosis can have differing imaging features, so that it is difficult to differentiate from malignancy.
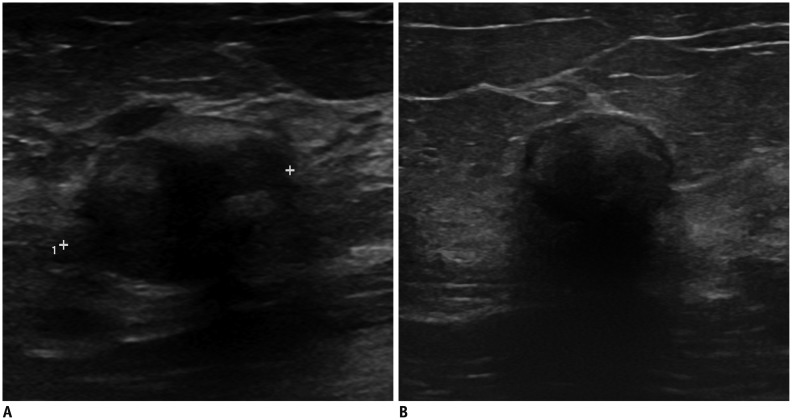
The sonographic features of fat necrosis vary in terms of pathologic reaction and degree of fibrosis. Fat necrosis may present as a solid mass, a complex mass with mural nodules, a complex mass with echogenic bands, an anechoic mass with posterior acoustic enhancement, an anechoic mass with shadowing, or an isoechoic mass. The margin of fat necrosis ranges from well circumscribed to indistinct or spiculated (Fig. 2) (9,10). On mammography, fat necrosis may show an oil cyst with coarse calcifications, focal asymmetries, spiculated masses or microcalcifications depending on the amount of fibrosis (11). Before the biopsy for the diagnosis, careful history collections and mammographic findings are helpful.
Fig. 2. Fat necrosis in 39-year-old woman without trauma history.
A. Transverse ultrasonography (US) shows irregular hypoechoic mass in her left breast. Lesion measured 2.24 cm in diameter. Pathologically, necrosis was confirmed by US-guided core needle biopsy. B. Follow-up US image after 3 years demonstrates decrease in lesion size to 1.67 cm with increased posterior acoustic shadowing.
Fibrotic Scars
Fibrotic scar usually occurs after breast surgery or breast trauma. According to the histopathology, postsurical scars, which are considered the general term for fibrotic scars, range from early inflammatory reactions with histiocytes and lymphocytes to proliferative connective tissue (12).
The lesion usually shows architectural distortion with variable density on mammography. When irregular hypoechoic lesion and architectural distortion on US with previous surgical history are perceived, it is not difficult to diagnose the lesion as fibrotic scar (Fig. 3). However, in the case of unknown personal history, it could be a suspicious lesion that mimics malignancy. Sometimes, a linear hypoechoic line with extension to the skin layer can be an indicator of fibrotic scar with past surgical history. Enhancement patterns of the lesion are diverse depending on the interval between surgery and MRI examination (13).
Fig. 3. 43-year-old woman with fibrotic scar.
Initially, she had left breast lesion that was confirmed as fibrocystic change with stromal fibrosis on excisional biopsy (not shown). A. After 5 years of excisional biopsy, lesion shows irregular hypoechoic mass with posterior acoustic shadowing on transverse ultrasonography. Fibrotic nodule with dystrophic calcification was proven from repeated biopsy. B. Transverse ultrasonography image after 7 years shows decreased size of the lesion.
Inflammations
Abscess
Because abscess is usually associated with typical clinical features such as palpable mass with a focal area of pain, erythema and induration, which usually results from mastitis, clinical features and past medical history can be helpful for diagnosis (14). There are two types of mastitis: puerperal (lactation-related) and periductal (nonlactational). Puerperal mastitis occurs in maternal age with a history of pregnancy or lactation. Pathogens are transmitted through the disrupted nipple, and subsequent milk stasis is thought to be the cause. In contrast, periductal mastitis can be found in perimenopausal women who smoke or have nipple rings (15). It is known that the direct effect of toxic metabolism from smoking can damage the subareolar ductal epithelium.
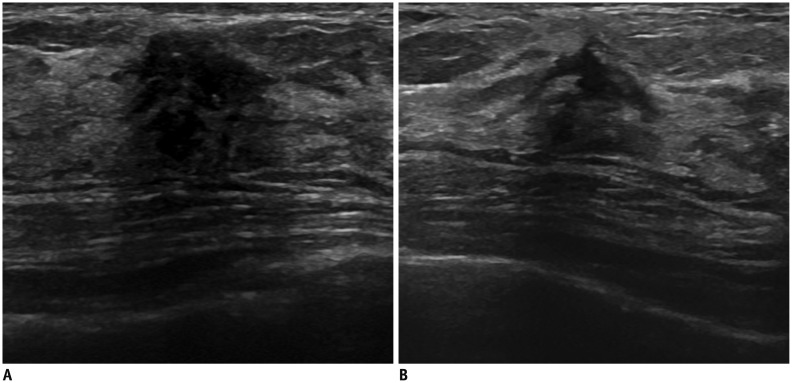
On US, the typical finding of abscess is a markedly hypoechoic or anechoic mass with a thick echogenic rim (16). Internal heterogeneous echogenicity can be shown depending on the inflammatory process with necrotic debris. However, with the varying degrees of inflammation, the lesion can show a poorly defined irregularly shaped hypoechoic mass without a definitive anechoic-fluid-filled lesion in the early inflammatory phase, which can mimic breast malignancy (Fig. 4) (14,17). Nguyen et al. (17) suggest that surrounding interstitial fluid and the hypoechoic wall can be a point of differential diagnosis between a breast abscess and cancer. On mammography, abscess may present as an irregular hyperdense mass with indistinct or spiculated margins that arouses suspicion (16).
Fig. 4. Right breast abscess in 36-year-old woman.
A. Transverse ultrasonography (US) image shows irregular hypoechoic mass with inner mixed echogenicity in her right breast. B. Increased vascularity is seen on color Doppler US. Acute and chronic inflammation were confirmed by US-guided core needle biopsy. C. After 13 months, transverse US image reveals abscess with fistula formation.
Idiopathic Granulomatous Lobular Mastitis
Idiopathic granulomatous lobular mastitis, also called chronic granulomatous mastitis or granulomatous lobulitis, is a rare benign inflammatory disease of the breast that mimics cancer both clinically and radiologically. Kessler and Wolloch found that it was characterized by granulomas with the presence of epitheloid and multinucleated giant cells that were limited to the mammary lobules with microabscesses without obvious etiology (18). A previous study reported that IGLM is an autoimmune process and is related to a recent history of pregnancy, lactation, and use of an oral contraceptive (19).
On US, IGLM shows not only an irregular hypoechoic mass with indistinct margin but also areas of mixed echogenicity with parenchymal deformity (Fig. 5). Clustered multiple lesions or contiguous tubular hypoechoic lesions (fingerlike) can also be found (20). The most common mammographic findings of IGLM are an ill-defined mass and asymmetric density (19). Gautier et al. (21) reported that the most common MR finding of IGLM is a segmental or regional area of non-mass enhancement, and all lesions show rapid enhancement with heterogeneous kinetics.
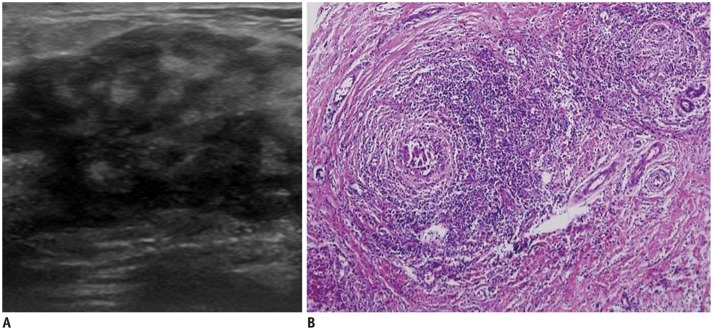
Fig. 5. 5. Granulomatous lobular mastitis in 38-year-old woman presenting as painful mass in left breast.
A. Transverse ultrasonography image shows irregular hypoechoic lesion. B. Photomicrograph (hematoxylin and eosin stain, × 100) demonstrates granulomatous inflammation that is centered on lobules with lymphocytes, plasma cells, epithelioid histiocytes, and multinucleated giant cells.
Diabetic Mastopathy
Diabetic mastopathy is a rare disease with a self-limiting fibroinflammatory process of the breast composed of dense stromal keloid-like fibrosis with or without lymphocytic infiltration and interlobular epithelioid fibroblasts in histology (22). Because this condition has been described in type 1 and long-standing type 2 diabetes mellitus, clinical history is very important. Clinical features including hard, irregular, movable breast masses without pain are typical. The lesions can be multiple and bilateral (23).
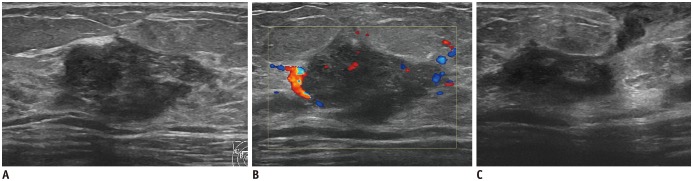
On mammography, the lesion usually shows localized increased density in the glandular tissue. An irregular hypoechoic mass with intense posterior acoustic shadowing can be typically seen on US and can mimic breast malignancy (Fig. 6). DMP usually shows nonspecific parenchymal enhancement rather than an irregular enhancing mass on MRI (24). Because the number and size of DMP usually increases as the patient's age increases, it is supported that repetitive fine needle aspiration cytology or core biopsy be performed on new lesions to ensure that they are not malignant lesions. Open excisional biopsy is not recommended if clinical and radiological features suggest DMP (25).
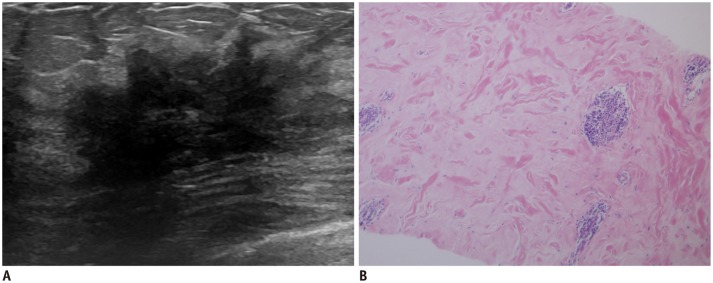
Fig. 6. Diabetic mastopathy in 44-year-old woman with long-standing type 2 diabetes mellitus.
A. Initial transverse ultrasonography image shows irregular spiculated hypoechoic masses with marked posterior shadowing in right breast. B. Photomicrography (hematoxylin and eosin stain, × 100) demonstrates band-like keloid fibrosis with periductal inflammation. After 2 years, lesions remain unchanged on follow-up image (not shown).
Proliferative Diseases
Sclerosing Adenosis
Sclerosing adenosis is a benign proliferative disease that is frequently seen in perimenopausal women. The lesion consists of acinar, myoepithelial, and connective tissue changes at the terminal ductal lobular unit (26). Both clinically and radiologically, sclerosing adenosis can be confused with invasive carcinoma because it presents a firm mass and other overlapping findings with those of malignancy. Histologically, the lesion can be confused with malignancy because of its fibrosis and elastosis, and sclerosing adenosis may coexist with carcinoma in situ or invasive carcinoma. Westenend and Liem (27) reported that some cases that were diagnosed as sclerosing adenosis by core needle biopsy demonstrated malignancy on surgical excision.
There is a wide range of radiological findings for sclerosing adenosis in both mammography and US (Fig. 7). The contours of mass lesions vary from circumscribed to irregular and even spiculated forms. Contour irregularity of these lesions is associated with stromal sclerosis and fibrosis. Architectural distortion can be seen. The most frequent microcalcification patterns are amorphous or pleomorphic punctate clusters and scattered amorphous punctate calcifications (26). A common ultrasonographic finding of sclerosing adenosis is an oval circumscribed hypoechoic mass with posterior acoustic enhancement (28). However, the lesion can also show suspicious findings including partial indistinct margin, heterogeneity and antiparallel orientation on US.
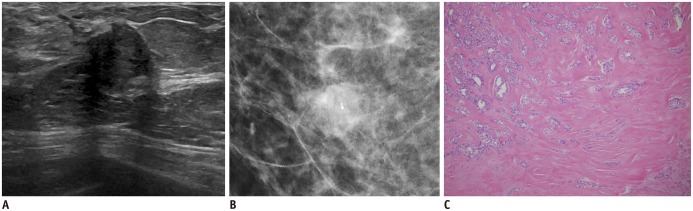
Fig. 7. Sclerosing adenosis in 60-year-old woman.
A. Transeverse ultrasonography image shows nonparallel irregular hypoechoic mass. B. Craniocaudal mammogram shows irregular obscured hyperdense mass in her right breast. C. Lesion was proven to be sclerosing adenosis on pathologic exam, showing lobulocentric and swirling architecture of proliferating acini with maintenance of normal epithelial and myoepithelial cells (hematoxylin and eosin stain, × 100).
Apocrine Metaplasia
Apocrine metaplasia is a benign epithelial alteration primarily in the lobular portion of the terminal ductal lobular unit (29). In pathologic specimens of apocrine metaplasia, the columnar-type secretory epithelium has granular, eosinophilic cytoplasm and is lined along the dilated acini. Apocrine metaplasia occurs frequently in conjunction with other benign breast diseases, including FCC, papilloma, fibroadenoma, and hamartoma (30).
The mammographic finding of apocrine metaplasia is a micro- or macro-lobulated mass with equal to low density relative to breast parenchyma owing to its prominent cystic composition (31). On US, the lesion typically shows clustered multiple anechoic cysts that form a lobulated mass with intervening hyperechoic lines that suggest septations and that also show partial posterior acoustic enhancement (Fig. 8).
Fig. 8. 40-year-old woman with apocrine metaplasia.
A. Transverse ultrasonography image shows irregular hypoechoic mass with angular margin in her right breast. B. Apocrine metaplasia was reveled from core biopsy (hematoxylin and eosin stain, × 400).
Fibrocystic Change
Fibrocystic change is the most common benign breast condition; 1 out of every 2 women may develop this condition in her lifetime (32). FCC is a clinical diagnostic term that encompasses a wide spectrum of histologies such as stromal fibrosis, cysts, adenosis, apocrine metaplasia, and epithelial proliferation to varying degrees (33). There are two types of FCC on histopathology, non-proliferative type without malignant potential and proliferative type that can be combined with atypical ductal or lobular hyperplasia. The etiology of FCC is not well-known, but estrogen supplements and phase of menstrual cycle have been thought to be related.
On US, FCCs may show cystic lesions that can be simple, complicated, or clustered cysts or clustered microcysts. Solid masses, complex cystic and solid lesions, and irregular discrete masses with irregular shadowing can be seen with scattered echogenic foci that represent calcifications (Fig. 9) (20,34). There is a broad spectrum of mammographic findings of FCC that ranges from circumscribed mass to indistinct mass with calcifications (34).
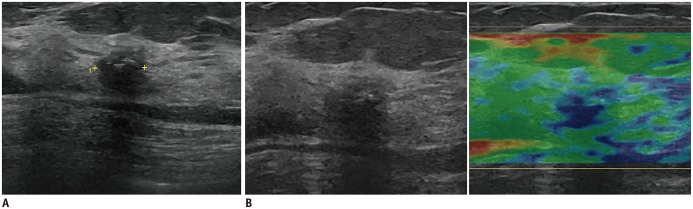
Fig. 9. Fibrocystic change in 47-year-old woman.
A. Irregular microlobulating hypoechoic mass with posterior shadowing was seen in her left breast on transverse ultrasonography. Inner hyperechoic foci in this lesion suggest calcifications. B. On elastography, lesion demonstrates elasticity score 2.
Benign Breast Tumors
Fibroadenoma
Fibroadenoma is a benign fibroepithelial tumor that develops in the lobules at the ends of mammary gland ducts and is composed of the epithelium and stroma (35). At clinical examination and on histopathologic analysis, fibroadenomas are the breast tumors that are most commonly found in adolescent girls and young women, possibly because of estrogen stimulation (36). Histopathologic features of fibroadenomas include the concurrent proliferation of stromal and glandular elements.
On mammography, fibroadenoma shows well-defined round, oval, or lobulated masses with some calcifications ranging from small peripheral dots to popcorn-shaped features. If the calcified fibroadenoma is typically benign, additional work-up such as US imaging or biopsy is not necessary. On US, fibroadenoma usually shows a well-circumscribed oval mass, either hypoechoic or isoechoic, that is typically parallel in orientation (37). However, Fornage et al. (38) reported that one-quarter of fibroadenomas showed an irregular hypoechoic mass that aroused suspicion (Fig. 10). Posterior shadow or enhancement on gray-scale image and peripheral feeding vessels on color Doppler US can be seen (37,38).
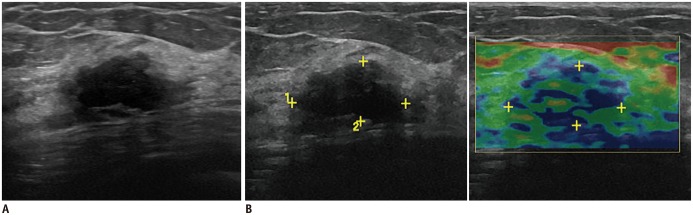
Fig. 10. Fibroadenoma in 45-year-old woman.
A. Transverse ultrasonography image shows irregular hypoechoic mass with mild posterior shadowing in right breast. B. Elastogram demonstrates elasticity score 2. Dense collagenous fibroadenoma was proven by excision biopsy.
Intraductal Papilloma
Intraductal papillomas are usually benign breast tumors that are epithelial proliferations of the lactiferous ducts (39). There are two types of intraductal papillomas, central and peripheral. The central types arise within the subareolar region and are solitary palpable masses in perimenopausal women, whereas the peripheral types are multiple peripheral masses within the terminal ductal lobular unit that develop in young women (39,40). The most common cause of unilateral, single-pore, spontaneous ductal discharge is papilloma (41,42).
The usual appearance of an intraductal papilloma on mammography is a well-defined, round solitary subareolar mass with a radiolucent halo. Occasionally, in one-fourth of all cases, the lesion is associated with a coarse calcification or microcalcification (39). Ductography can help to define the sites, numbers, and extent of presumed papillomas. Because papilloma secretes fluid profusely, a dilated duct downstream is often noted (42). On US, two patterns indicate intraductal papilloma. The most common is an intraductal mass with duct dilatation, and the other is a solid mass, sometimes with a cystic component but without visible duct dilatation (Fig. 11) (40).
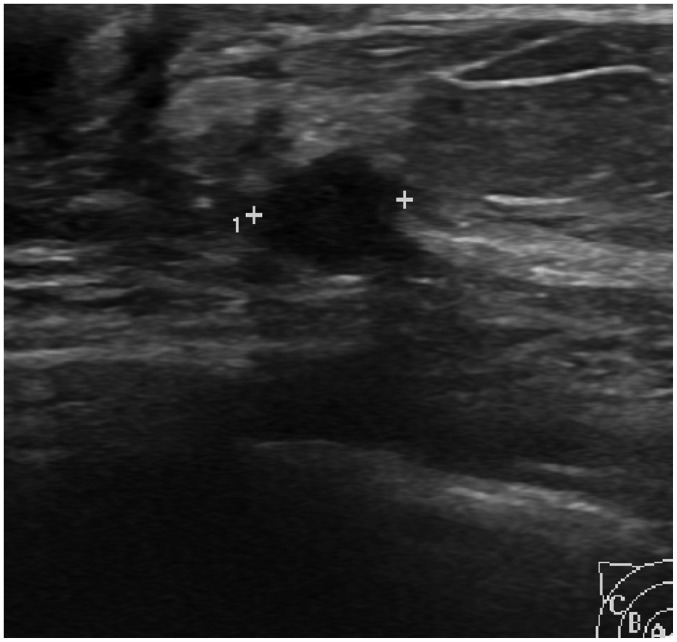
Fig. 11. Intraductal papilloma in 44-year-old woman.
Transverse ultrasonography image demonstrates irregular hypoechoic mass in right breast.
Tubular Adenoma
Tubular adenoma is a rare benign breast lesion that is often found in young women. It is known to be related to fibroadenoma because there are lesions that histologically fall within a spectrum between fibroadenoma and tubular adenoma. Tubular adenoma is distinguished by homogeneously tightly packed tubular or acinar epithelial components with sparse connective tissue, whereas fibroadenoma has abundant stroma and an epithelial component consisting of large ducts (43).
The imaging appearance of tubular adenomas of the breast has been rarely described. At mammography, dense, punctate, or irregular microcalcifications that are tightly grouped within a mass may be a distinctive feature of tubular adenomas. Noncalcified tubular adenomas are similar to noncalcified fibroadenomas on US (Fig. 12) (44).
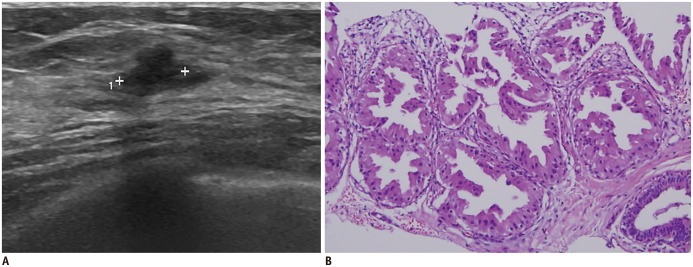
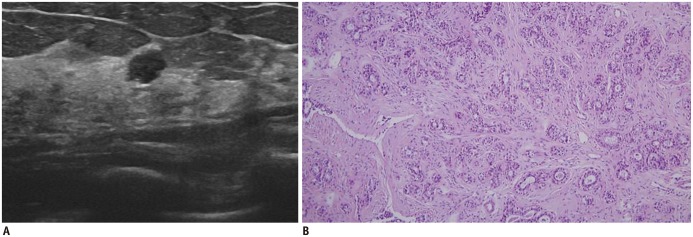
Fig. 12. Tubular adenoma in 43-year-old woman.
A. Transverse ultrasonography image shows irregular hypoechoic mass in her right breast. B. On histologic examination, closely packed small tubules are seen with lining of epithelial cells surrounded by myoepithelial layer (hematoxylin and eosin stain, × 100).
CONCLUSION
Irregular hypoechoic breast masses on US are usually considered suspicious BI-RADS category 4, but BI-RADS category 4 lesions are known to have a broad range of malignant rates (3-94%), and these lesions on US vary significantly on histopathological examinations. Recently, sono-elastography has received attention as a helpful tool for differentiating between benign and malignant breast lesions. In assessing BI-RADS category 4a lesions, soft elasticity can decrease the suspicion and downgrade the lesions to category 3 so that unnecessary biopsies can be reduced (45).
Irregular hypoechoic breast masses on US do not always indicate malignancies; various benign diseases could show irregular hypoechoic masses and other disease-specific findings during differential diagnosis. In some sophisticated cases, careful ultrasonographic examination and additional work-up with US-guided core needle biopsy could help to differentiate the lesions from malignancies.
Footnotes
This study was supported by Wonkwang University in 2014.
References
- 1.Mendelson EB, Böhm-Vélez M, Berg WA, et al. ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. Reston, VA: American College of Radiology; 2013. ACR BIRADS® Ultrasound. [Google Scholar]
- 2.Raza S, Goldkamp AL, Chikarmane SA, Birdwell RL. US of breast masses categorized as BI-RADS 3, 4, and 5: pictorial review of factors influencing clinical management. Radiographics. 2010;30:1199–1213. doi: 10.1148/rg.305095144. [DOI] [PubMed] [Google Scholar]
- 3.Taskin F, Koseoglu K, Ozbas S, Erkus M, Karaman C. Sonographic features of histopathologically benign solid breast lesions that have been classified as BI-RADS 4 on sonography. J Clin Ultrasound. 2012;40:261–265. doi: 10.1002/jcu.21923. [DOI] [PubMed] [Google Scholar]
- 4.Raza S, Chikarmane SA, Neilsen SS, Zorn LM, Birdwell RL. BI-RADS 3, 4, and 5 lesions: value of US in management--follow-up and outcome. Radiology. 2008;248:773–781. doi: 10.1148/radiol.2483071786. [DOI] [PubMed] [Google Scholar]
- 5.Han BK, Choe YH, Ko YH, Nam SJ, Yang JH. Foreign body granulomas of the breast presenting as bilateral spiculated masses. Korean J Radiol. 2001;2:113–116. doi: 10.3348/kjr.2001.2.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tez S, Sen M, Yenidünya S, Tez M. Foreign body granuloma: a mimic of breast carcinoma. Bratisl Lek Listy. 2009;110:366–367. [PubMed] [Google Scholar]
- 7.Wakabayashi M, Reid JD, Bhattacharjee M. Foreign body granuloma caused by prior gunshot wound mimicking malignant breast mass. AJR Am J Roentgenol. 1999;173:321–322. doi: 10.2214/ajr.173.2.10430127. [DOI] [PubMed] [Google Scholar]
- 8.Taboada JL, Stephens TW, Krishnamurthy S, Brandt KR, Whitman GJ. The many faces of fat necrosis in the breast. AJR Am J Roentgenol. 2009;192:815–825. doi: 10.2214/AJR.08.1250. [DOI] [PubMed] [Google Scholar]
- 9.Crystal P, Bukhanov K. Sonographic findings of palpable isoechoic breast fat necrosis: look for skin integrity. J Ultrasound Med. 2005;24:105–107. doi: 10.7863/jum.2005.24.1.105. [DOI] [PubMed] [Google Scholar]
- 10.Soo MS, Kornguth PJ, Hertzberg BS. Fat necrosis in the breast: sonographic features. Radiology. 1998;206:261–269. doi: 10.1148/radiology.206.1.9423681. [DOI] [PubMed] [Google Scholar]
- 11.Chala LF, de Barros N, de Camargo Moraes P, Endo E, Kim SJ, Pincerato KM, et al. Fat necrosis of the breast: mammographic, sonographic, computed tomography, and magnetic resonance imaging findings. Curr Probl Diagn Radiol. 2004;33:106–126. doi: 10.1067/j.cpradiol.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Franquet T, De Miguel C, Cozcolluela R, Donoso L. Spiculated lesions of the breast: mammographic-pathologic correlation. Radiographics. 1993;13:841–852. doi: 10.1148/radiographics.13.4.8356272. [DOI] [PubMed] [Google Scholar]
- 13.Shaheen R, Schimmelpenninck CA, Stoddart L, Raymond H, Slanetz PJ. Spectrum of diseases presenting as architectural distortion on mammography: multimodality radiologic imaging with pathologic correlation. Semin Ultrasound CT MR. 2011;32:351–362. doi: 10.1053/j.sult.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 14.An YY, Kim SH, Cha ES, Kim HS, Kang BJ, Park CS, et al. Diffuse infiltrative lesion of the breast: clinical and radiologic features. Korean J Radiol. 2011;12:113–121. doi: 10.3348/kjr.2011.12.1.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dixon JM, Ravisekar O, Chetty U, Anderson TJ. Periductal mastitis and duct ectasia: different conditions with different aetiologies. Br J Surg. 1996;83:820–822. doi: 10.1002/bjs.1800830630. [DOI] [PubMed] [Google Scholar]
- 16.Nicholson BT, Harvey JA, Cohen MA. Nipple-areolar complex: normal anatomy and benign and malignant processes. Radiographics. 2009;29:509–523. doi: 10.1148/rg.292085128. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen SL, Doyle AJ, Symmans PJ. Interstitial fluid and hypoechoic wall: two sonographic signs of breast abscess. J Clin Ultrasound. 2000;28:319–324. doi: 10.1002/1097-0096(200009)28:7<319::aid-jcu1>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 18.Taylor GB, Paviour SD, Musaad S, Jones WO, Holland DJ. A clinicopathological review of 34 cases of inflammatory breast disease showing an association between corynebacteria infection and granulomatous mastitis. Pathology. 2003;35:109–119. [PubMed] [Google Scholar]
- 19.Gurleyik G, Aktekin A, Aker F, Karagulle H, Saglamc A. Medical and surgical treatment of idiopathic granulomatous lobular mastitis: a benign inflammatory disease mimicking invasive carcinoma. J Breast Cancer. 2012;15:119–123. doi: 10.4048/jbc.2012.15.1.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho SH, Park SH. Mimickers of breast malignancy on breast sonography. J Ultrasound Med. 2013;32:2029–2036. doi: 10.7863/ultra.32.11.2029. [DOI] [PubMed] [Google Scholar]
- 21.Gautier N, Lalonde L, Tran-Thanh D, El Khoury M, David J, Labelle M, et al. Chronic granulomatous mastitis: imaging, pathology and management. Eur J Radiol. 2013;82:e165–e175. doi: 10.1016/j.ejrad.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 22.Logan WW, Hoffman NY. Diabetic fibrous breast disease. Radiology. 1989;172:667–670. doi: 10.1148/radiology.172.3.2672091. [DOI] [PubMed] [Google Scholar]
- 23.Camuto PM, Zetrenne E, Ponn T. Diabetic mastopathy: a report of 5 cases and a review of the literature. Arch Surg. 2000;135:1190–1193. doi: 10.1001/archsurg.135.10.1190. [DOI] [PubMed] [Google Scholar]
- 24.Francisco C, Júlio C, Fontes AL, Silveira Reis I, Fernandes R, Valadares S, et al. Diabetic mastopathy: a case report. Clin Imaging. 2012;36:829–832. doi: 10.1016/j.clinimag.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 25.Mak CW, Chou CK, Chen SY, Lee PS, Chang JM. Case report: diabetic mastopathy. Br J Radiol. 2003;76:192–194. doi: 10.1259/bjr/51145312. [DOI] [PubMed] [Google Scholar]
- 26.Tas¸kin F, Köseoğlu K, Unsal A, Erkus¸ M, Ozbas¸ S, Karaman C. Sclerosing adenosis of the breast: radiologic appearance and efficiency of core needle biopsy. Diagn Interv Radiol. 2011;17:311–316. doi: 10.4261/1305-3825.DIR.3785-10.2. [DOI] [PubMed] [Google Scholar]
- 27.Westenend PJ, Liem SJ. Core biopsy of nodular adenosis of the breast can lead to underdiagnosis. AJR Am J Roentgenol. 2001;176:1596. doi: 10.2214/ajr.176.6.1761596. [DOI] [PubMed] [Google Scholar]
- 28.Liberman L. Clinical management issues in percutaneous core breast biopsy. Radiol Clin North Am. 2000;38:791–807. doi: 10.1016/s0033-8389(05)70201-3. [DOI] [PubMed] [Google Scholar]
- 29.Wellings SR, Alpers CE. Apocrine cystic metaplasia: subgross pathology and prevalence in cancer-associated versus random autopsy breasts. Hum Pathol. 1987;18:381–386. doi: 10.1016/s0046-8177(87)80169-7. [DOI] [PubMed] [Google Scholar]
- 30.Bussolati G, Cattani MG, Gugliotta P, Patriarca E, Eusebi V. Morphologic and functional aspects of apocrine metaplasia in dysplastic and neoplastic breast tissue. Ann N Y Acad Sci. 1986;464:262–274. doi: 10.1111/j.1749-6632.1986.tb16008.x. [DOI] [PubMed] [Google Scholar]
- 31.Warner JK, Kumar D, Berg WA. Apocrine metaplasia: mammographic and sonographic appearances. AJR Am J Roentgenol. 1998;170:1375–1379. doi: 10.2214/ajr.170.5.9574619. [DOI] [PubMed] [Google Scholar]
- 32.Drukker BH. Fibrocystic change of the breast. Clin Obstet Gynecol. 1994;37:903–915. doi: 10.1097/00003081-199412000-00017. [DOI] [PubMed] [Google Scholar]
- 33.Love SM, Gelman RS, Silen W. Sounding board. Fibrocystic "disease" of the breast--a nondisease? N Engl J Med. 1982;307:1010–1014. doi: 10.1056/NEJM198210143071611. [DOI] [PubMed] [Google Scholar]
- 34.Chen JH, Nalcioglu O, Su MY. Fibrocystic change of the breast presenting as a focal lesion mimicking breast cancer in MR imaging. J Magn Reson Imaging. 2008;28:1499–1505. doi: 10.1002/jmri.21455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Foster ME, Garrahan N, Williams S. Fibroadenoma of the breast: a clinical and pathological study. J R Coll Surg Edinb. 1988;33:16–19. [PubMed] [Google Scholar]
- 36.Masciadri N, Ferranti C. Benign breast lesions: ultrasound. J Ultrasound. 2011;14:55–65. doi: 10.1016/j.jus.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goel NB, Knight TE, Pandey S, Riddick-Young M, de Paredes ES, Trivedi A. Fibrous lesions of the breast: imaging-pathologic correlation. Radiographics. 2005;25:1547–1559. doi: 10.1148/rg.256045183. [DOI] [PubMed] [Google Scholar]
- 38.Fornage BD, Lorigan JG, Andry E. Fibroadenoma of the breast: sonographic appearance. Radiology. 1989;172:671–675. doi: 10.1148/radiology.172.3.2549564. [DOI] [PubMed] [Google Scholar]
- 39.Tarallo V, Canepari E, Bortolotto C. Intraductal papilloma of the breast: a case report. J Ultrasound. 2012;15:99–101. doi: 10.1016/j.jus.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brookes MJ, Bourke AG. Radiological appearances of papillary breast lesions. Clin Radiol. 2008;63:1265–1273. doi: 10.1016/j.crad.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 41.Chang JM, Cho N, Moon WK, Park JS, Chung SY, Jang M. Does ultrasound-guided directional vacuum-assisted removal help eliminate abnormal nipple discharge in patients with benign intraductal single mass? Korean J Radiol. 2009;10:575–580. doi: 10.3348/kjr.2009.10.6.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Slawson SH, Johnson BA. Ductography: how to and what if? Radiographics. 2001;21:133–150. doi: 10.1148/radiographics.21.1.g01ja15133. [DOI] [PubMed] [Google Scholar]
- 43.Moross T, Lang AP, Mahoney L. Tubular adenoma of breast. Arch Pathol Lab Med. 1983;107:84–86. [PubMed] [Google Scholar]
- 44.Soo MS, Dash N, Bentley R, Lee LH, Nathan G. Tubular adenomas of the breast: imaging findings with histologic correlation. AJR Am J Roentgenol. 2000;174:757–761. doi: 10.2214/ajr.174.3.1740757. [DOI] [PubMed] [Google Scholar]
- 45.Lee SH, Chang JM, Cho N, Koo HR, Yi A, Kim SJ, et al. Practice guideline for the performance of breast ultrasound elastography. Ultrasonography. 2014;33:3–10. doi: 10.14366/usg.13012. [DOI] [PMC free article] [PubMed] [Google Scholar]