Abstract
AIM: To perform a systematic review and meta-analysis comparing operative vs non-operative treatment of displaced proximal humerus fractures in elderly patients.
METHODS: A systematic literature search was performed using EMBASE and MEDLINE through the OVID interface, CINAHL, the Cochrane Central Register of Controlled Trials (CENTRAL), Proquest, Web of Science, SAE digital library, and Transportation Research Board’s TRID database. Searches of conference proceedings were also conducted. All available randomized controlled trials comparing operative vs non-operative management of displaced three- and four-part proximal humerus fractures in elderly patients were included. The primary outcomes measures included physical function, pain, health related quality of life, mortality, and the re-operation rate.
RESULTS: Six randomized controlled trials (n = 287) were included. There was no statistically significant difference in function (MD = 1.72, 95%CI: -2.90-6.34, P = 0.47), as measured by the Constant score, between the operative and the non-operative treatment groups. There was no statistically significance difference in secondary outcomes of health related quality of life (standardized MD = 0.27, 95%CI: -0.05-0.59, P = 0.09), and mortality (relative risk 1.29, 95%CI: 0.50- 3.35, P = 0.60). Operative treatment had a statistically significant higher re-operation rate (relative risk 4.09, 95%CI: 1.50-11.15, P = 0.006), and statistically significant decreased pain (MD = 1.26, 95%CI: 0.02- 2.49, P = 0.05).
CONCLUSION: There is moderate quality evidence to suggest that there is no difference in functional outcomes between the two treatments. Further high quality randomized controlled trials are required to determine if certain subgroup populations benefit from surgical management.
Keywords: Proximal humerus fracture, Outcomes, Operative treatment, Non-operative treatment, Meta-analysis
Core tip: Our systematic review and meta-analysis found a lack of high quality evidence to determine the effects of operative vs non-operative treatment on patient-important outcomes among elderly patients with three- or four-part proximal humeral fractures. There is moderate quality evidence to suggest that there is no difference in functional outcomes between the two treatments.
INTRODUCTION
Proximal humerus fractures are the third most common fragility fracture and they are associated with a substantial burden of disability and impaired quality of life. Optimal treatment in elderly patients remains controversial, and an evidence-based approach is critical to improve patient outcomes and allocate limited health care resources[1-4].
Fracture treatment depends on the type of fracture, the degree of fragment displacement, and fracture stability[5]. Most proximal humeral fractures are nondisplaced or minimally displaced and are usually treated successfully non-operatively, but the optimum treatment becomes less clear in more complex, displaced fracture patterns[6,7]. Three- and four-part fractures account for 13% of proximal humerus fractures, and are regarded as the most challenging to treat[7]. Surgical interventions are associated with good functional outcomes in young adults, but provide varying results and high complication rates in the elderly population[8]. There is little evidence to support that surgical treatment of three- and four-part fractures in elderly patients is more effective than non-operative treatment[9].
Previous systematic reviews have attempted to compare operative and non-operative management of these fractures, but were limited to specific surgical techniques or did not include recently published relevant trials[10-12]. More importantly, most reviews do not use statistical techniques to appropriately pool the heterogeneous proximal humerus fracture literature. Substantial diversity in treatment options and the quality of comparative trials is well known in the management of these fractures, and failure to account for this heterogeneity may lead to incorrect conclusions or biased effect size estimates. In addition, further efforts to systematically assess the individual studies included in pooled analysis are necessary to protect the validity of conclusions and facilitate interpretation of the statistical results. To date, no previous proximal humerus fracture reviews have incorporated the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) to summarize evidence[13].
This systematic review and meta-analysis aimed to overcome the limitations of previous pooled analyses and determine whether operative treatment of displaced three- and four-part proximal humerus fractures in elderly patients improves physical function, pain, health related quality of life, mortality, complications and re-operation rate in comparison to non-operative treatment.
MATERIALS AND METHODS
This review was conducted according to the Cochrane Handbook and is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines[14,15].
Eligibility criteria for study selection
All randomized controlled trials that compared at least one operative intervention to a non-operative intervention for management of three- or four-part fractures of the proximal humerus in elderly patients were eligible for inclusion in this review. We excluded retrospective and prospective observational studies, case-reports, case-series, and reviews and studies including nondisplaced fractures or two part fractures. There was no restriction on the type of surgical technique or the non-operative treatment. We did not apply language or publication restrictions[16].
Identification of studies
The following electronic databases were searched for articles published up to February 20th, 2014: EMBASE and MEDLINE through the OVID interface, CINAHL, the Cochrane Central Register of Controlled Trials (CENTRAL), Proquest, Web of Science, SAE digital library, and Transportation Research Board’s TRID database. Combination of keywords and MeSH terms related to proximal humeral fractures were used and no language restrictions were applied (Appendix 1). The WHO International Clinical Trials Registry Platform Search Portal and Current Controlled Trials were searched to identify current and ongoing trials.
We also searched conference proceedings archives for the Canadian Orthopaedic Association, American Academy of Orthopaedic Surgeons, and Orthopaedic Trauma Association for the past seven years. We further conducted hand searches of the major orthopaedic journals in the Journal of Bone and Joint Surgery (American and British volumes) and Journal of Shoulder and Elbow Surgery for the same time frame. Reference list of eligible articles were searched to identify any relevant trials.
Assessment of eligibility and methodological quality
Two reviewers conducted title and abstract screening independently and disagreements were resolved by consensus through discussion between the two reviewers. Both reviewers also independently assessed the studies for final eligibility based on full text screening.
The two reviewers independently assessed the studies for risk of bias using the Cochrane Collaboration’s Risk of Bias Tool[14]. Developed by Cochrane, this quality assessment tool is designed to report the adequacy of patient allocation, allocation concealment, blinding, clarity of outcome data, the potential for selective outcome reporting, and any other sources of bias for each study included in a systematic review. One reviewer used the GRADE system to assess each outcome measure identified in this review and a second reviewer verified the assessments. When used in the context of a systematic review, the GRADE system is designed to rank the overall quality of included studies for a given outcome from “strong” to “weak” evidence[13]. Data from randomized controlled trials is inherently considered high quality or “strong”. Five limitations that can downgrade the quality include study limitations, inconsistency of results, indirectness of evidence, imprecision, and publication bias[13]. Moderate, low or very low quality evidence can be upgraded if there is a large magnitude of effect, a dose-response gradient, or if all plausible biases would not undermine the conclusions[13]. Rater differences in the assessment were discussed and resolved by consensus.
Data abstraction
A data abstraction form was developed and piloted. The following data was abstracted from each included trial: funding source, diagnostic classification system, mean age, gender, sample size, intervention methods, study duration, length of follow-up, physical function, pain, health related quality of life, mortality, and complication and re-operation rates. Outcome measurements within the first 6 mo after the intervention were considered short term and measurements beyond 12 mo were considered long term. One reviewer independently completed data abstraction for each of the included trials and the second reviewer verified the data abstraction.
Statistical analysis
Inter-observer differences for study eligibility and risk of bias assessment were measured using Cohen’s kappa statistic[17,18]. The following criteria for the kappa values were set a priori: 0.40 to 0.59 reflects fair agreement, 0.60 to 0.75 reflects good agreement, and 0.75 and higher reflects excellent agreement[14,19].
Function, pain, and health related quality of life were summarized using mean differences (MDs) or standardized mean differences when different instruments were used, and were weighted according to the inverse variance method[20,21]. Missing SDs were derived from CIs and P values[22,23]. Mortality and re-operation rate were summarized using risk ratios calculated using the Mantel-Haenszel method[14]. All comparisons were made for surgical fixation vs non-operative management; therefore, positive pooled estimates represent higher outcomes in the operative group. All tests for statistical significance were two tailed, and a P value of 0.05 or less was considered significant.
Heterogeneity was measured using the I2 statistic[14]. Surgical technique was defined as an a priori subgroup hypothesis to explain potential heterogeneity. Sensitivity analyses were conducted to test the effect of excluding outdated surgical methods, and to compare open reduction and internal fixation (ORIF) trials or hemi-arthroplasty trials alone. Publication bias was assessed by generating a funnel plot for studies measuring long-term function[14]. Outcomes were pooled using the fixed-effects model and if heterogeneity exceeded 40%, the random-effects model was used. Funnel plot and forest plots were generated using Review Manger 5.2.
RESULTS
Study selection
Our literature search identified 6473 titles for consideration for inclusion in this review. Agreement between reviewers for title and abstract eligibility was excellent (kappa= 1.0). Fourteen full-text articles were assessed for eligibility. Six randomized controlled trials (n = 287) met the eligibility criteria and are included in this review (Figure 1).
Figure 1.
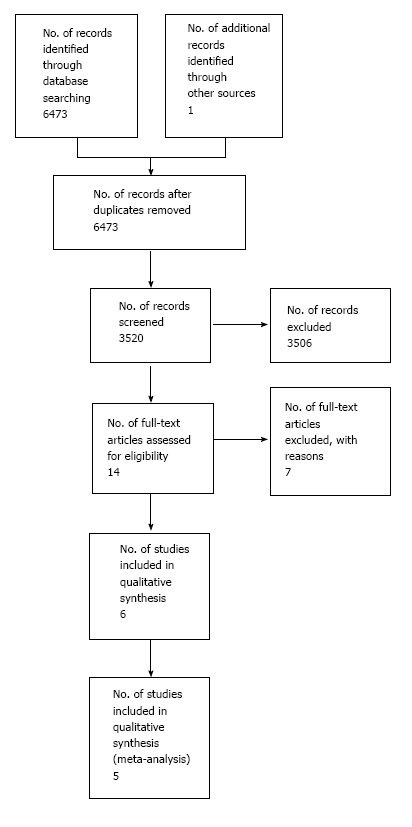
Study flowchart.
Study characteristics
All included trials were published between 1984 and 2012 (Table 1)[24-29]. All of the trials were conducted in Europe across four countries (Sweden, Norway, the Netherlands, and the United Kingdom). Three of the studies were government funded, one study was funded by industry, and two studies did not disclose a funding source.
Table 1.
Characteristics chart of included studies
| Ref. | Year | Country | Funding | Size | Age (mean) | Male (%) | Fracture classification system | Fracture type | Operative intervention | Non-operative intervention | Short term follow-up (mo) | Long term follow-up (mo) |
| Boons et al[24] | 2012 | The Netherlands | Industry funding | 50 | 79.9 | 2 | Neer | 3 or 4 part fractures | Hemiar- throplasty | Immobilization of the shoulder | 3 | 12 |
| Fjalestad et al[9,25] | 2010 | Norway | Government funding | 50 | 72.71 | 12 | OTA | 3 or 4 part fractures | ORIF with locking plate | Immobilization in a modified Velpeau bandage | 3 | 12 |
| Olerud et al[26] | 2011 | Sweden | Government funding | 55 | 76.71 | 14.5 | Neer | 4 part fractures | Hemiar- throplasty | Immobilization by slings | 4 | 12 |
| Olerud et al[27] | 2011 | Sweden | Government funding | 59 | 73.91 | 18.6 | Neer | 3 part fractures | ORIF-locking plate | Immobilization by slings | 4 | 12 |
| Stableforth[28] | 1984 | England | Not reported | 32 | 67.91 | 21.9 | Neer | 4 part fractures | Neer prosthesis | Closed manipulation | Not applicable | Not applicable |
| Zyto et al[29] | 1997 | Sweden | Not reported | 40 | 74 | 12.5 | Neer | 3 or 4 part fractures | ORIF-tension band technique | Immobilization by sling | No short term follow-up | 50 |
Average weighted mean of the two arms. ORIF: Open reduction and internal fixation.
Trial sample sizes ranged from 32 to 60 patients. All trials included patients over the age of 52 years and the mean ages ranged from 67.9 to 79.9 years. Fracture type was either classified by Neer’s classification (five trials), or OTA (one trial). The operative treatments included: Hemi-arthroplasty, ORIF with locking plate and cerclage wires, ORIF with a locking plate, and ORIF with tension band technique and Neer’s prosthesis. Non-operative treatment consisted of immobilization of the shoulder in all trials. Five trials reported short term and long term physical function measured by the Constant score (n = 228). Three trials reported health related quality of life, all six trials reported complications (mortality and re-operation), and pain was reported as a component of the Constant score in four trials and as a Visual Analog Scale in one trial.
Risk of bias
Four of the included trials had inadequate or unclear random sequence generation and allocation concealment was inadequate or unclear in two studies (Figure 2). Blinding of patients and outcome assessor bias was high in all studies. Agreement between the two reviewers for the risk of bias assessment was good (kappa = 0.635). The funnel plot is fairly symmetric; however, due to the low number of yielded studies, it is inefficient to clearly assess publication bias (Figure 3).
Figure 2.
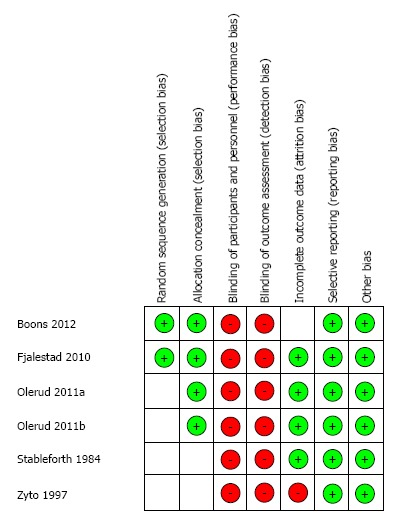
Risk of bias summary.
Figure 3.
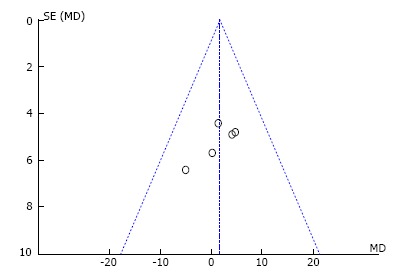
Funnel plot.
Functional outcome
Short term physical function was measured by the Constant score in three of the included trials (n = 156). The pooled estimate did not demonstrate any difference (MD = -2.79, 95%CI: -8.66 to 3.09, P = 0.35, I2 = 42%). Long term physical function measured by the Constant score was measured in five of the included trials (n = 228). The pooled estimate did not demonstrate any difference (MD = 1.63, 95%CI: 2.90, to 6.34, P = 0.47, I2 = 0%) (Figure 4A). The findings were robust to sensitivity analysis that tested the effect of excluding outdated surgical techniques (MD = 2.78, 95%CI: -2.20 to 7.75, P = 0.27, I2 = 0%), and they were robust in subgroup analyses that included either ORIF trials alone (MD = 3.25, 95%CI: -4.61 to 11.11, P = 0.42, I2 = 0%), or hemi-arthroplasty trials alone (MD = 2.46, 95%CI: -3.96 to 8.88, P = 0.45, I2 = 0%).
Figure 4.
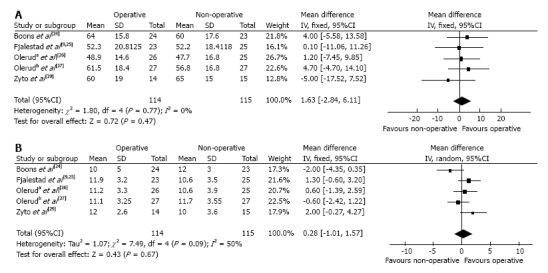
Pooled estimate of physical function according to the Constant score at a minimum of one year follow-up (A) and pain according to the Constant score component at a minimum of one year follow-up (B).
Pain
Pain was measured as an individual outcome in one of the studies using the Visual Analog Scale and, was measured as a component of the Constant score in five studies. The short term pooled estimate for the Constant pain score did not demonstrate any difference (MD = 0.77, 95%CI: -0.63 to 2.16, P = 0.28, I2 = 42%). The long-term pooled estimate was statistically significant and pain was lower in the operative group (MD = 1.26, 95%CI: 0.02 to 2.49, P = 0.05, I2 = 51%) (Figure 4B). However, pain was not statistically significant when sensitivity analysis was conducted that tested the effect of excluding outdated surgical techniques (MD = 1.10, 95%CI: -0.39 to 2.59, P = 0.15, I2 = 61%), and no difference was found in subgroup analyses that included either ORIF trials alone (MD = 0.37, 95%CI: –1.49 to 2.23, P = 0.70, I2 = 51%), or hemi-arthroplasty trials alone (MD = 1.84, 95%CI: -0.51 to 4.19, P = 0.08, I2 = 67%).
Health related quality of life
Health related quality of life was reported in three of the included trials (two studies used the EQ-5D and one study used the 15D instrument). The short and long term pooled estimates did not demonstrate any difference (SMD = 0.26, 95%CI: -0.06-0.57, P = 0.11, I2 = 0% and SMD = 0.27, 95%CI: -0.05-0.59, P = 0.09, I2 = 0%, respectively).
Complications and re-operations
The pooled estimate of mortality did not demonstrate any difference [relative risk (RR) 1.29, 95%CI: 0.50 to 3.35, P = 0.60, I2 = 0%] (Figure 5A). The re-operation rate was reported in five studies and was significantly higher in the operative group (RR 4.09, 95%CI: 1.50-11.15, P = 0.006, I2 = 0%) (Figure 5B). The rates of infection (RR 4.43, 95%CI: 0.78-25.18, P = 0.08, I2 = 0%), avascular necrosis (RR 0.63, 95%CI: 0.35-1.14, P = 0.13, I2 = 0%), nonunion (RR 0.45, 95%CI: 0.14-1.43, P = 0.18, I2 = 0%), and post-traumatic osteoarthritis (RR 0.60, 95%CI: 0.22-1.64, P = 0.32, I2 = 36%) did not differ significantly between the operative and non-operative treatment groups (Table 2).
Figure 5.
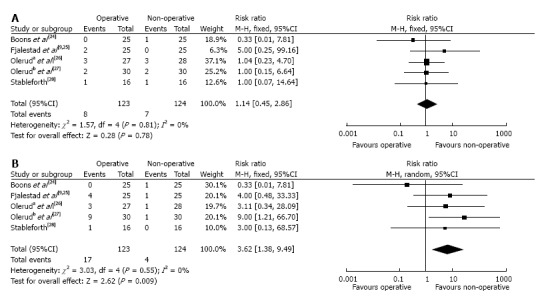
Pooled estimate of mortality rate (A) and re-operation rate (B).
Table 2.
Complications chart
|
Operative |
Non-operative |
|||||||||
| Ref. | Infection | Avascular necrosis | Nonunion | Nerve injury | Post-traumatic osteoarthritis | Infection | Avascular necrosis | Nonunion | Nerve injury | Post-traumatic osteoarthritis |
| Boons et al[24] | 0 | 0 | 0 | NR | NR | 0 | 2 | 3 | NR | NR |
| Fjalestad et al[9,25] | 0 | 8 | 0 | 7 | NR | 0 | 13 | 2 | 6 | NR |
| Olerud et al[26] | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 0 | 5 |
| Olerud et al[27] | 2 | 3 | 1 | 0 | 3 | 0 | 2 | 1 | 1 | 2 |
| Stableforth[28] | 1 | NR | NR | NR | NR | 0 | NR | NR | NR | NR |
| Zyto et al[29] | 2 | 1 | 1 | NR | 2 | 0 | 0 | 0 | NR | 2 |
| Total | 5 | 12 | 2 | 7 | 5 | 0 | 20 | 7 | 7 | 9 |
NR: Not reported.
GRADE quality assessment
Physical function as measured by the Constant score, long term health related quality of life, and mortality were deemed to be of moderate quality by the GRADE quality system due to the risks of bias associated with the trial design and conduct (Table 3). This finding indicates that further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Long term pain and re-operation received a low quality score which indicates that further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Table 3.
Grading of Recommendations Assessment, Development, and Evaluation summary findings: Operative vs non-operative treatment in proximal humeral fractures
| Outcomes | No. of Participants (studies) | Quality of the evidence (GRADE) | Relative effect (95%CI) |
Anticipated absolute effects |
|
| Follow up | Risk difference between non-operative and operative1 (95%CI) | ||||
| Physical Function by Constant score - long term | 229 (5 studies) | Moderate due to risk of bias | The mean physical function by constant score-long term in the intervention group was 1.63 higher (2.84 lower to 6.11 higher) | ||
| Health Related Quality of Life - long term | 154 (3 studies) | Moderate due to risk of bias | The mean health related quality of life - long term in the intervention group was 0.23 standard deviations higher (0.09 lower to 0.54 higher) | ||
| Constant pain - long term | 229 (5 studies) | Low due to risk of bias, inconsistency | The mean Constant pain - long term in the intervention group was 0.28 higher (1.01 lower to 1.57 higher) | ||
| Mortality rate | 247 (5 studies) | Moderate due to risk of bias | RR 1.14 (0.45 to 2.86) | Study population | |
| 56 per 1000 | 8 more per 1000 (from 31 fewer to 105 more) | ||||
| Moderate | |||||
| 63 per 1000 | 9 more per 1000 (from 35 fewer to 117 more) | ||||
| Re-operation Rate | 247 (5 studies) | Low due to risk of bias, imprecision | RR 3.62 (1.38 to 9.49) | Study population | |
| 32 per 1000 | 85 more per 1000 (from 12 more to 274 more) | ||||
| Moderate | |||||
| 36 per 1000 | 94 more per 1000 (from 14 more to 306 more) | ||||
The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95%CI). RR: Risk ratio; GRADE Working Group grades of evidence: High quality: Further research is very unlikely to change our confidence in the estimate of effect; Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate; Very low quality: We are very uncertain about the estimate.
Sensitivity analyses
Two of the included trials used older implants that are no longer commonly used in clinical practice[28,29]. To ensure the stability of our pooled results, we conducted a sensitivity analysis that excluded data from these two studies, but found that there was no change in our meta-analysis conclusions as described above.
DISCUSSION
This systematic review and meta-analysis compared operative treatment vs non-operative treatment of three- and four-part proximal humeral fractures in elderly patients. According to the GRADE system, the evaluation of physical function constituted moderate quality evidence. We did not find a significant difference in physical function between the operative and non-operative treatment for both the short term and long term follow-up periods. The outcome of pain was limited by low quality of evidence, although we found a significant difference in the long term period in favor of the operative group. Health related quality of life was ranked as moderate quality of evidence and there was no statistically significant difference in the short and long term health related quality of life between the two treatment groups. Mortality comparison was of moderate quality evidence and showed no statistically significant difference. Re-operation rate was limited by low quality of evidence and we found a statistically significant difference in the re-operation rate in favour of the non-operative group.
Strengths and limitations
Overall, the results of this study must be interpreted in the context of the primary studies’ design. This meta-analysis included randomized controlled trials with methodological limitations and consequently a high risk of bias. These limitations include small sample sizes, inadequate blinding, and poor reporting of randomization technique. Blinding is not always possible in trials comparing surgical vs non-operative management. Strategies to mitigate this limitation could have been implemented including blinded adjudication of outcomes and a blinded analysis and interpretation of the data. In an attempt to further minimize bias, we did not include observational studies in this review. Their inclusion may have increased the overall sample size, but may have also introduced a higher level of bias due to their non-randomized designs.
The six trials included in this review did not report on all relevant outcomes. For example, the trials did not report on the cost-effectiveness of operative vs non-operative management, which is an important consideration. Pain was also poorly reported, with only one study reporting pain as an individual outcome measure as opposed to a component of the Constant score.
The trials were conducted in four different countries within Europe which may limit the generalizability of the findings beyond this region. It is also important to recognize that differences in surgical practice, technique, and management exist across the trials which may skew the overall results due to expertise bias. In addition, two of the included trials used older implants that are no longer commonly used in clinical practice[28,29]; however, our sensitivity analyses showed that the results remained robust with the inclusion of these two trials.
Despite these limitations, our meta-analysis is strengthened by its systematic approach, pre-defined and broad eligibility criteria, our duplicated data abstraction methods, and the use of the GRADE quality assessment system. The GRADE system was developed by a widely representative group of international guideline developers to offer a comprehensive grading system that can separate decisions regarding the quality of evidence from the strength of recommendations; where high quality evidence does not always result in strong recommendations. Additional advantages of GRADE over other systems include explicit evaluation of the importance of outcomes of alternative management strategies; explicit, comprehensive criteria for downgrading and upgrading quality of evidence ratings; a transparent process of moving from evidence to recommendations; the acknowledgement of values and preferences of the population under study and/or for which guidelines are being developed; clear, pragmatic interpretations of strong vs weak recommendations for clinicians, patients, and policy makers; and is useful for systematic reviews, health technology, and guideline assessments.
There is a lack of high quality evidence to determine the effects of operative vs non-operative treatment on patient-important outcomes among elderly patients with three- or four-part proximal humeral fractures. There is moderate quality evidence to suggest that there is no difference in functional outcomes between the two treatments. Further high quality trials are warranted to determine if operative treatment in elderly patients with three- and four-part fractures is the optimal method of managing these complex fractures.
COMMENTS
Background
Proximal humerus fractures are associated with a substantial burden of disability and impaired quality of life. Most proximal humeral fractures are nondisplaced or minimally displaced and are usually treated successfully non-operatively, but the optimum treatment becomes less clear in more complex, displaced fracture patterns.
Research frontiers
Optimal treatment of displaced proximal humerus fractures in elderly patients remains controversial, and an evidence-based approach is critical to improve patient outcomes and allocate limited health care resources.
Innovations and breakthroughs
In the present study, the authors investigated the outcomes of operative vs non-operative treatment of displaced proximal humerus fractures in elderly patient by pooling results from six randomized controlled trials. This is the first report of a meta-analysis comparing the effects of operative vs non-operative treatment on patient-important outcomes among elderly patients with three- or four-part proximal humeral fractures.
Applications
There is moderate quality evidence to suggest that there is no difference in functional outcomes between operative vs non-operative treatment of displaced proximal humerus fractures in elderly patients.
Peer-review
Very well put together paper and review.
Footnotes
P- Reviewer: Kwasnicki RM, Shafi M S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
Supported by In part by a Canada Research Chair to Dr. Bhandari; in part by the Canadian Institutes of Health Research and Vancouver Coastal Health Research Institute to Dr. Slobogean.
Conflict-of-interest statement: The authors certify that they, or a member of their immediate families, have no funding or commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article
Data sharing statement: No additional data are available.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: March 2, 2015
First decision: June 18, 2015
Article in press: September 28, 2015
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72:365–371. doi: 10.1080/000164701753542023. [DOI] [PubMed] [Google Scholar]
- 3.Huttunen TT, Launonen AP, Pihlajamäki H, Kannus P, Mattila VM. Trends in the surgical treatment of proximal humeral fractures - a nationwide 23-year study in Finland. BMC Musculoskelet Disord. 2012;13:261. doi: 10.1186/1471-2474-13-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87–92. doi: 10.1097/01.blo.0000194672.79634.78. [DOI] [PubMed] [Google Scholar]
- 5.Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 6.Burkhart KJ, Dietz SO, Bastian L, Thelen U, Hoffmann R, Müller LP. The treatment of proximal humeral fracture in adults. Dtsch Arztebl Int. 2013;110:591–597. doi: 10.3238/arztebl.2013.0591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fakler JK, Hogan C, Heyde CE, John T. Current concepts in the treatment of proximal humeral fractures. Orthopedics. 2008;31:42–51. doi: 10.3928/01477447-20080101-13. [DOI] [PubMed] [Google Scholar]
- 8.Robinson CM, Page RS, Hill RM, Sanders DL, Court-Brown CM, Wakefield AE. Primary hemiarthroplasty for treatment of proximal humeral fractures. J Bone Joint Surg Am. 2003;85-A:1215–1223. doi: 10.2106/00004623-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Fjalestad T, Hole MO, Hovden IA, Blucher J, Stromsoe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma. 2012;26:98–106. doi: 10.1097/BOT.0b013e31821c2e15. [DOI] [PubMed] [Google Scholar]
- 10.Handoll HH, Ollivere BJ, Rollins KE. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2012;12:CD000434. doi: 10.1002/14651858.CD000434.pub3. [DOI] [PubMed] [Google Scholar]
- 11.Li Y, Zhao L, Zhu L, Li J, Chen A. Internal fixation versus nonoperative treatment for displaced 3-part or 4-part proximal humeral fractures in elderly patients: a meta-analysis of randomized controlled trials. PLoS One. 2013;8:e75464. doi: 10.1371/journal.pone.0075464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Misra A, Kapur R, Maffulli N. Complex proximal humeral fractures in adults--a systematic review of management. Injury. 2001;32:363–372. doi: 10.1016/s0020-1383(00)00242-4. [DOI] [PubMed] [Google Scholar]
- 13.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 14.Higgins JPT, Greene S. Cochrane handbook for systematic reviews of interventions. USA: The Cochrane Collaboration; 2011. [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D, Pham B, Lawson ML, Klassen TP. The inclusion of reports of randomised trials published in languages other than English in systematic reviews. Health Technol Assess. 2003;7:1–90. doi: 10.3310/hta7410. [DOI] [PubMed] [Google Scholar]
- 17.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 18.Sackett D, Haynes R, Guyatt G, Tugwell P. Clinical epidemiology: A basic science for clinicians. 2nd ed. Boston: Little Brown; 1991. [Google Scholar]
- 19.Orwin RG. Evaluating coding decisions. In: Cooper H, Hedges LV, editors. The Handbook of Research Synthesis. New York: Russell Sage Foundation; 1994. pp. 139–162. [Google Scholar]
- 20.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 21.Puhan MA, Soesilo I, Guyatt GH, Schünemann HJ. Combining scores from different patient reported outcome measures in meta-analyses: when is it justified? Health Qual Life Outcomes. 2006;4:94. doi: 10.1186/1477-7525-4-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. J Clin Epidemiol. 2006;59:7–10. doi: 10.1016/j.jclinepi.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 23.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boons HW, Goosen JH, van Grinsven S, van Susante JL, van Loon CJ. Hemiarthroplasty for humeral four-part fractures for patients 65 years and older: a randomized controlled trial. Clin Orthop Relat Res. 2012;470:3483–3491. doi: 10.1007/s11999-012-2531-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fjalestad T, Hole MØ, Jørgensen JJ, Strømsøe K, Kristiansen IS. Health and cost consequences of surgical versus conservative treatment for a comminuted proximal humeral fracture in elderly patients. Injury. 2010;41:599–605. doi: 10.1016/j.injury.2009.10.056. [DOI] [PubMed] [Google Scholar]
- 26.Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Hemiarthroplasty versus nonoperative treatment of displaced 4-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011;20:1025–1033. doi: 10.1016/j.jse.2011.04.016. [DOI] [PubMed] [Google Scholar]
- 27.Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011;20:747–755. doi: 10.1016/j.jse.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 28.Stableforth PG. Four-part fractures of the neck of the humerus. J Bone Joint Surg Br. 1984;66:104–108. doi: 10.1302/0301-620X.66B1.6693466. [DOI] [PubMed] [Google Scholar]
- 29.Zyto K, Ahrengart L, Sperber A, Törnkvist H. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br. 1997;79:412–417. doi: 10.1302/0301-620x.79b3.7419. [DOI] [PubMed] [Google Scholar]


