Abstract
Neurotoxicity is an infrequent adverse reaction to iodinated contrast agents. Contrast induced neurotoxicity following coronary angiogram is very rare. Renal disease is a risk factor for contrast induced neurotoxicity. We report a case of contrast induced neurotoxicity following coronary angiogram and intervention using Iohexol (Omnipaque 350) in an end stage renal disease patient on peritoneal dialysis who had prior exposure to iodinated contrast without any adverse reaction. Hemodialysis had to be initiated for rapid removal of the contrast agent with subsequent complete resolution of neurological deficits. This case highlights the need for interventionalists to be aware of an important adverse reaction to iodinated contrast agents, especially in individuals with renal dysfunction, and that neurotoxicity is a possibility even with prior uneventful exposures. The role and timing of hemodialysis in contrast induced neurotoxicity in patients with chronic kidney disease and in those without chronic kidney disease needs further deliberation.
Keywords: Coronary angiogram, End stage renal disease, Hemodialysis, Iodinated contrast agent, Neurotoxicity
Core tip: Contrast induced neurotoxicity following coronary angiogram is very rare. Interventionalists should be aware of this rare complication especially in patients with end stage renal disease (ESRD). Iodinated contrast media can be effectively removed from the blood by dialysis. Hemodialysis is a better modality for rapid removal of contrast agent compared to peritoneal dialysis. Hemodialysis should be considered in life-threatening adverse reactions when supportive care alone is not sufficient. More studies are needed to further delineate the role and timing of hemodialysis following coronary angiogram and the optimal dosage of contrast media in ESRD patients to prevent this infrequent but potentially life threatening adverse reaction.
INTRODUCTION
Iodinated contrast agents are an important tool in medical practice. It is estimated that nearly 75 million doses are administered worldwide every year[1]. Modern iodinated contrast agents are mostly nonionic and low osmolar (2-3 times the osmolality of serum) or iso-osmolar (same osmolality of serum). They are safe and adverse reactions, when occur, are mild and self-limiting but serious and life threatening reactions can occur occasionally[2]. Here we describe a case of contrast induced neurotoxicity (CIN) following coronary angiogram in a patient with end stage renal disease (ESRD).
CASE REPORT
A 44-year-old African American female with coronary artery disease, hypertension, severe functional mitral regurgitation, ESRD on peritoneal dialysis, status post failed renal transplant on slow taper of immunosuppressants and diabetes mellitus type 2, was admitted for unstable angina. A month prior to this presentation patient had undergone a diagnostic right and left heart catheterization revealing 70% stenosis of first obtuse marginal branch and 80% stenosis of mid right coronary artery. Seventy ml of Iohexol (Omnipaque 350), a low-osmolar nonionic contrast media, had been used during the procedure. A coronary angiogram with percutaneous coronary intervention was planned. Three days prior to the cardiac intervention, a computerized tomography (CT) of abdomen and pelvis with and without contrast was performed for evaluation of hematuria. Seventy milliliter of Iodixanol (Visipaque 320), an iso-osmolar nonionic contrast media, was used. Patient tolerated this without any untoward events. Three days later patient underwent coronary angiogram and percutaneous intervention with drug eluting stent to first obtuse marginal branch of left circumflex and right coronary artery. Around 190 mL of Iohexol (Omnipaque 350) was used during the procedure. Patient tolerated the procedure without any immediate complications but within few hours developed headache with left sided weakness. A non-contrast head CT, four hours after the coronary intervention, showed extensive intravascular contrast with cortical staining, primarily over the right cerebral hemisphere and left cerebral hemisphere watershed territories (Figure 1). No other acute abnormalities were noted. Subarachnoid hemorrhage was considered unlikely and the clinical picture was considered likely secondary to contrast induced neurotoxicity. Supportive care and manual peritoneal dialysis exchanges were initiated. During this process, patient became more encephalopathic with subsequent seizure like activity. Antiepileptic medications, lorazepam and levetiracetam, were given to control seizures. Patient was transitioned to hemodialysis for rapid removal of contrast agent. A magnetic resonance imaging (MRI) of the brain taken 24 h after the coronary intervention showed hyperintense cortical signal on T2, fluid attenuated inversion recovery (FLAIR) and diffusion weighted images throughout the right greater than left cerebral hemisphere (Figure 2). No definite restricted diffusion was observed. There was mild mass effect without hemorrhage or herniation. An electro encephalogram was negative for seizure activity. These findings were considered consistent with contrast induced neurotoxicity (CIN). Supportive care and hemodialysis were continued for the next three days with gradual improvement and complete resolution of neurological abnormalities. Patient was transitioned back to peritoneal dialysis and discharged from the hospital in stable condition. Repeat imaging was not performed prior to discharge.
Figure 1.
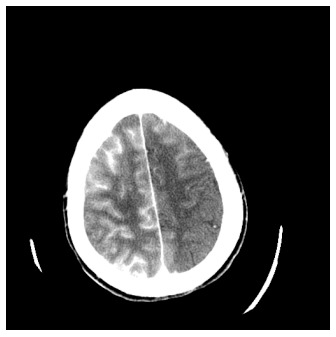
Non-contrast head computerized tomography showing extensive intravascular contrast with cortical staining, primarily over the right cerebral hemisphere.
Figure 2.
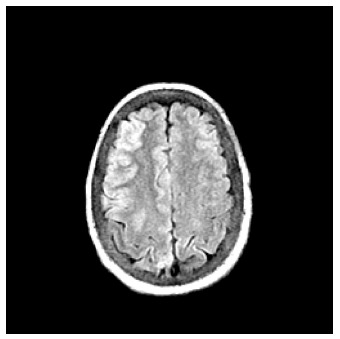
Magnetic resonance imaging fluid attenuated inversion recovery image showing hyperintense cortical signal of the cerebral hemispheres.
DISCUSSION
CIN is an infrequent adverse reaction to iodinated contrast agents. Intraarterial and neurointerventional procedures are more commonly associated with CIN[3]. CIN following coronary angiogram is very rare and the reported incidence is 0.06%[4]. This adverse reaction following coronary angiogram using Iohexol has been noted before[5]. All types of iodinated contrast agents irrespective of their ionic state or osmolality can cause CIN[3]. Neurological deficits are either focal or global. The exact etiology of CIN is unclear. Prior and subsequent exposure may not cause the same complication[4]. It is considered to be an idiosyncratic reaction to the contrast agent. An intact blood brain barrier is impermeable to contrast agents under normal conditions. Direct chemotoxic effects and hyperosmolality result in increased permeability of blood brain barrier and resultant cerebral edema, and also the possibility of increased hydrostatic pressure transmitted during neurointerventional procedures and subsequent changes in cerebral autoregulation predisposing to contrast extravasation has also been postulated[4,6]. Symptoms range from headache to seizures, hemiparesis, ophthalmoplegia, transient global amnesia, and transient cortical blindness. Neurological deficits are mostly transient but could also be persistent, especially with ophthalmic involvement[3,4]. Symptoms appear within 2 to 12 h of contrast injection and usually resolve in 24 to 72 h[7]. Imaging studies are recommended to rule out thromboembolic or hemorrhagic complications. Unenhanced CT images may be normal or show combination of poorly localized cortical and or subcortical enhancement, cerebral edema, and hyperdensity in the subarachnoid space similar to subarachnoid hemorrhage. MRI imaging may demonstrate hyperintense areas on T2, FLAIR, and diffusion weighted images[5]. Risk factors for CIN include renal disease, hypertension, and route, number of administration, and duration of exposure[3,7]. Larger dose of contrast is considered a risk factor but CIN has been reported even with very small doses[4]. Kocabay et al[3] recommend a maximum of 170 mL contrast agent for coronary angiograms to prevent CIN but none of the patients in their case series had ESRD. Our patient had ESRD and had prior exposure to iodinated contrast agents including Omnipaque 350 and to Visipaque 320 without any adverse events supporting the concept of CIN being an idiosyncratic reaction. In our case, for the culprit coronary angioplasty procedure, 190 mL of Omnipaque 350 had been utilized. General consensuses for preventive measures include adequate hydration prior to contrast exposure and using lowest possible contrast dose. Treatment is mostly supportive and hydration. Contrast media can be effectively removed from the blood by dialysis[8].
Contrast induced neurotoxicity following coronary angiogram is very rare. Interventionalists should be aware of this rare complication especially in patients with ESRD. Iodinated contrast media can be effectively removed by dialysis. Hemodialysis is a better modality for rapid removal of contrast agent compared to peritoneal dialysis. Hemodialysis should be considered in life-threatening adverse reactions when supportive care alone is not sufficient. More studies are needed to further delineate the role and timing of hemodialysis following coronary angiogram, and the optimal dosage of contrast media in ESRD patients to prevent this infrequent but potentially life threatening adverse reaction to iodinated contrast agents.
COMMENTS
Case characteristics
A 44-year-old female with coronary artery disease and end-stage renal disease on peritoneal dialysis underwent coronary angiogram and intervention for unstable angina.
Clinical diagnosis
Status post coronary angiogram and intervention, patient developed acute encephalopathy with no focal neurological deficits.
Differential diagnosis
Cerebrovascular accident, contrast neurotoxicity.
Imaging diagnosis
A non-contrast computerized tomography of the head showed extensive intravascular contrast with cortical staining, primarily over the right cerebral hemisphere. A magnetic resonance imaging showed hyperintense cortical signal of the cerebral hemispheres.
Treatment
Hemodialysis and supportive care.
Related reports
Contrast induced neurotoxicity is very rare following coronary angiogram. Correct diagnosis will avoid erroneous treatment for cerebrovascular accident.
Term explanation
Contrast induced neurotoxicity (CIN) is an infrequent adverse reaction to iodinated contrast agents. End stage renal disease (ESRD) is a risk factor for the development of CIN.
Experiences and lessons
Contrast induced neurotoxicity is very rare following coronary angiogram. Prior exposures to iodinated contrast agents may not have resulted in any adverse reaction supporting CIN to be an idiosyncratic reaction. Hemodialysis is an effective tool in contrast removal and management of CIN, especially in ESRD patients.
Peer-review
Very good case report about contrast induced neurotoxicity. It is very well written, summarized but completed.
Footnotes
Institutional review board statement: This case report was exempt from the Institutional Review Board standards at East Carolina University.
Informed consent statement: The patient involved in this study gave informed consent authorizing use and disclosure of protected health information.
Conflict-of-interest statement: All the authors have no conflicts of interests to declare.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: May 8, 2015
First decision: July 10, 2015
Article in press: September 8, 2015
P- Reviewer: Anis S, Cesar D, Desai DJ, Jiang B S- Editor: Ji FF L- Editor: A E- Editor: Wang CH
References
- 1.Pasternak JJ, Williamson EE. Clinical pharmacology, uses, and adverse reactions of iodinated contrast agents: a primer for the non-radiologist. Mayo Clin Proc. 2012;87:390–402. doi: 10.1016/j.mayocp.2012.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh J, Daftary A. Iodinated contrast media and their adverse reactions. J Nucl Med Technol. 2008;36:69–74; quiz 76-77. doi: 10.2967/jnmt.107.047621. [DOI] [PubMed] [Google Scholar]
- 3.Kocabay G, Karabay CY, Kalayci A, Akgun T, Guler A, Oduncu V, Tanboga IH, Izgi A, Kirma C. Contrast-induced neurotoxicity after coronary angiography. Herz. 2014;39:522–527. doi: 10.1007/s00059-013-3871-6. [DOI] [PubMed] [Google Scholar]
- 4.Leong S, Fanning NF. Persistent neurological deficit from iodinated contrast encephalopathy following intracranial aneurysm coiling. A case report and review of the literature. Interv Neuroradiol. 2012;18:33–41. doi: 10.1177/159101991201800105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sawaya RA, Hammoud R, Arnaout S, Alam S. Contrast-induced encephalopathy following coronary angioplasty with iohexol. South Med J. 2007;100:1054–1055. doi: 10.1097/SMJ.0b013e3181540086. [DOI] [PubMed] [Google Scholar]
- 6.Yu J, Dangas G. Commentary: New insights into the risk factors of contrast-induced encephalopathy. J Endovasc Ther. 2011;18:545–546. doi: 10.1583/11-3476C.1. [DOI] [PubMed] [Google Scholar]
- 7.Law S, Panichpisal K, Demede M, John S, Marmur JD, Nath J, Baird AE. Contrast-Induced Neurotoxicity following Cardiac Catheterization. Case Rep Med. 2012;2012:267860. doi: 10.1155/2012/267860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deray G. Dialysis and iodinated contrast media. Kidney Int Suppl. 2006;69:S25–S29. doi: 10.1038/sj.ki.5000371. [DOI] [PubMed] [Google Scholar]


