Abstract
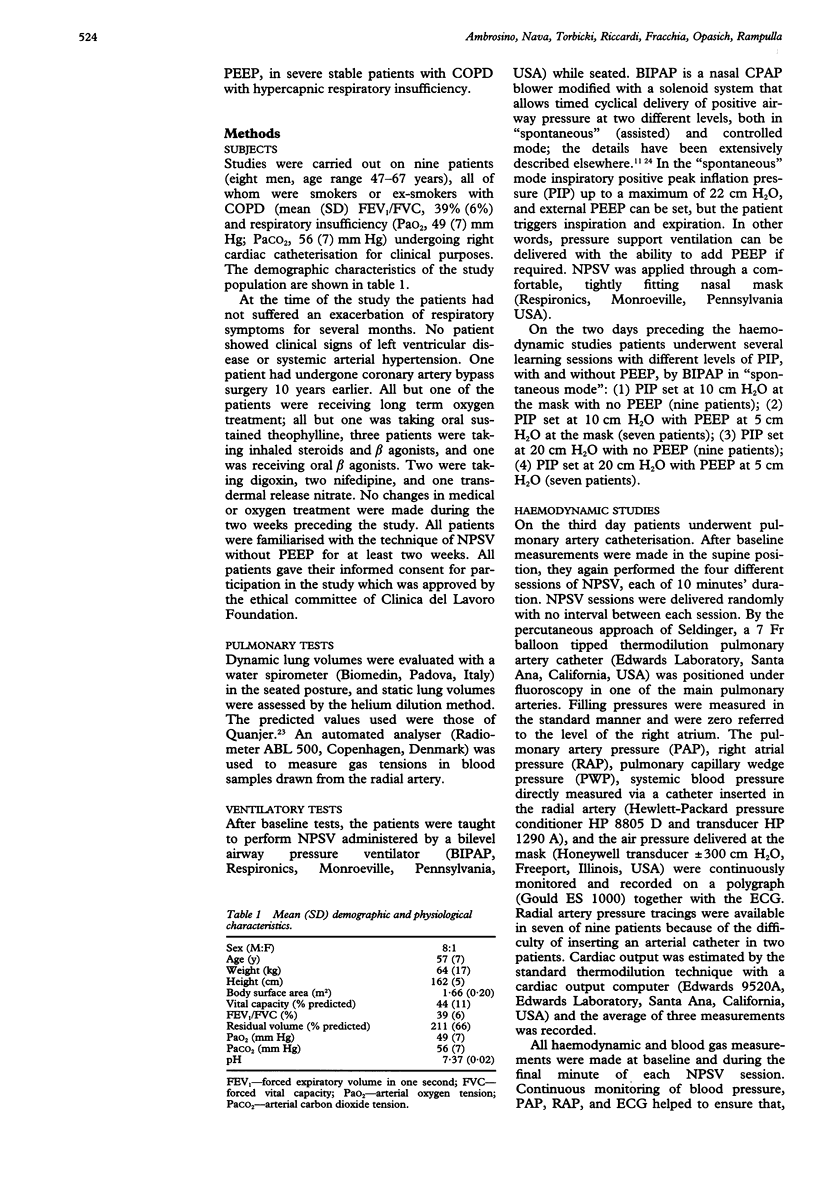
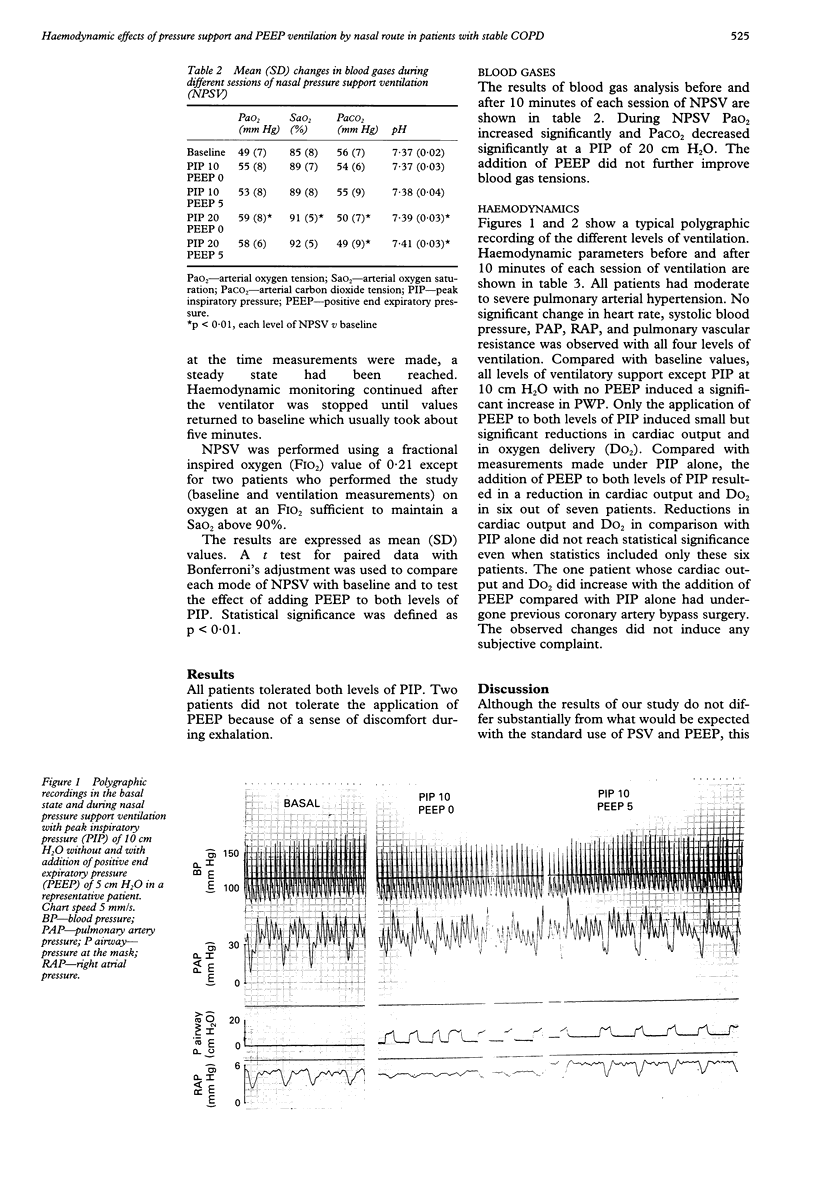
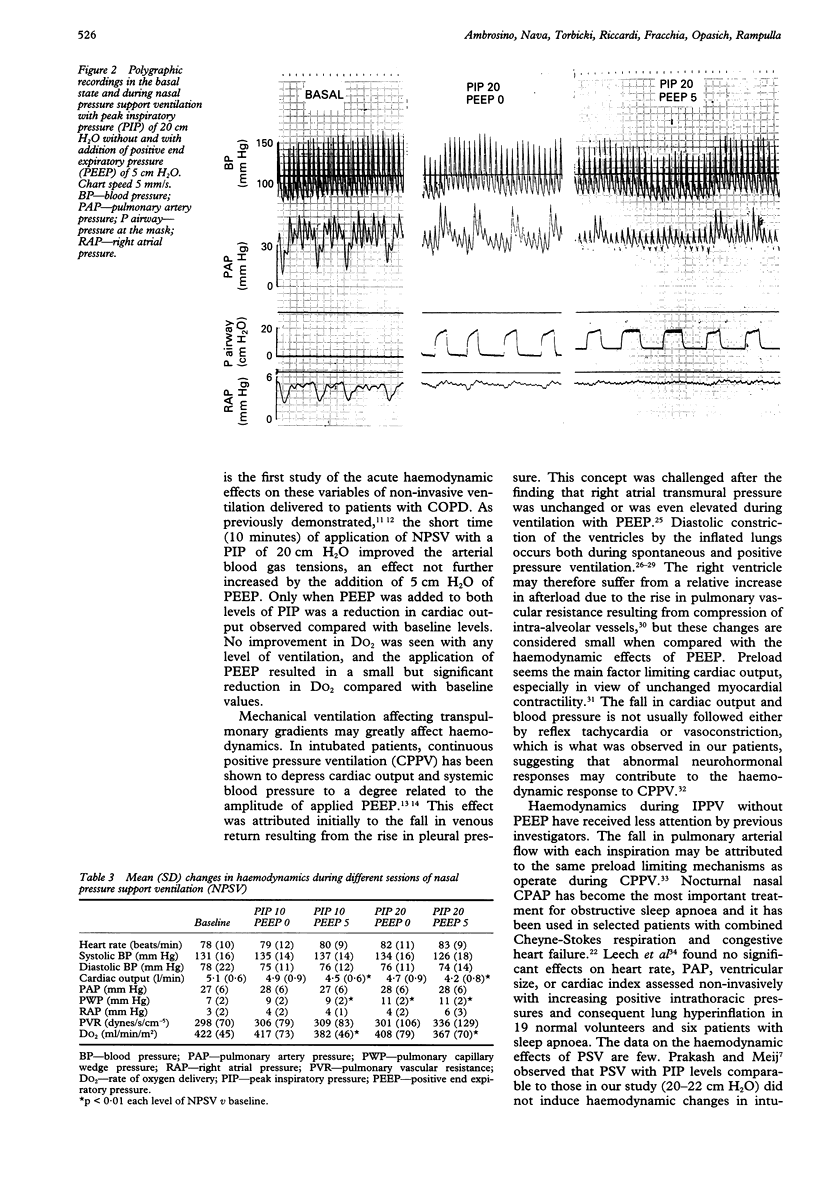
BACKGROUND--Intermittent positive pressure ventilation applied through a nasal mask has been shown to be useful in the treatment of chronic respiratory insufficiency. Pressure support ventilation is an assisted mode of ventilation which is being increasingly used. Invasive ventilation with intermittent positive pressure, with or without positive end expiratory pressure (PEEP), has been found to affect venous return and cardiac output. This study evaluated the acute haemodynamic support ventilation by nasal mask, with and without the application of PEEP, in patients with severe stable chronic obstructive pulmonary disease and hypercapnia. METHODS--Nine patients with severe stable chronic obstructive pulmonary disease performed sessions lasting 10 minutes each of pressure support ventilation by nasal mask while undergoing right heart catheterisation for clinical evaluation. In random order, four sessions of nasal pressure support ventilation were applied consisting of: (1) peak inspiratory pressure (PIP) 10 cm H2O, PEEP 0 cm H2O; (2) PIP 10 cm H2O, PEEP 5 cm H2O; (3) PIP 20 cm H2O, PEEP 0 cm H2O; (4) PIP 20 cm H2O, PEEP 5 cm H2O. RESULTS--Significant increases in arterial oxygen tension (Pao2) and saturation (Sao2) and significant reductions in arterial carbon dioxide tension (PaCO2) and changes in pH were observed with a PIP of 20 cm H2O. Statistical analysis showed that the addition of 5 cm H2O PEEP did not further improve arterial blood gas tensions. Comparison of baseline values with measurements performed after 10 minutes of each session of ventilation showed that all modes of ventilation except PIP 10 cm H2O without PEEP induced a small but significant increase in pulmonary capillary wedge pressure. In comparison with baseline values, a significant decrease in cardiac output and oxygen delivery was induced only by the addition of PEEP to both levels of PIP. CONCLUSIONS--In patients with severe stable chronic obstructive pulmonary disease and hypercapnia, pressure support ventilation with the addition of PEEP delivered by nasal mask may have short term acute haemodynamic effects in reducing oxygen delivery in spite of adequate levels of SaO2.
Full text
PDF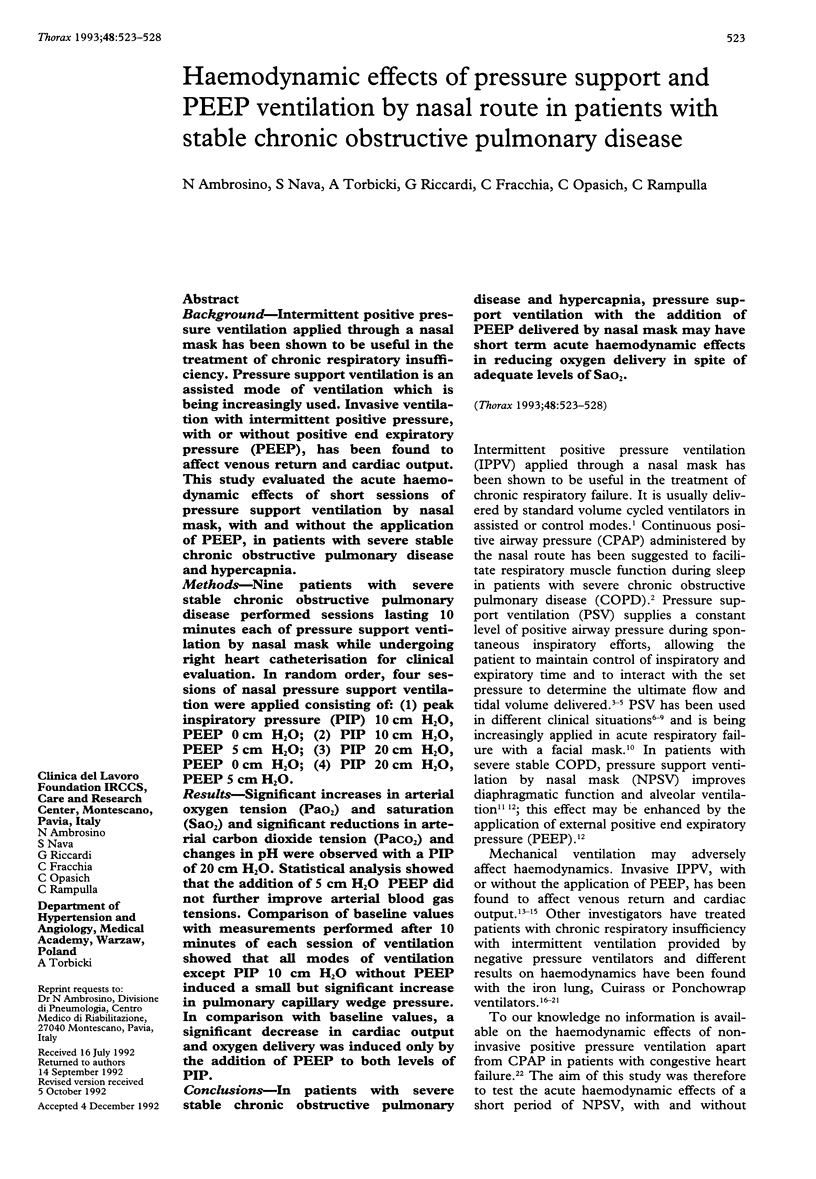
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ambrosino N., Cobelli F., Torbicki A., Opasich C., Pozzoli M., Fracchia C., Rampulla C. Hemodynamic effects of negative-pressure ventilation in patients with COPD. Chest. 1990 Apr;97(4):850–856. doi: 10.1378/chest.97.4.850. [DOI] [PubMed] [Google Scholar]
- Ambrosino N., Nava S., Bertone P., Fracchia C., Rampulla C. Physiologic evaluation of pressure support ventilation by nasal mask in patients with stable COPD. Chest. 1992 Feb;101(2):385–391. doi: 10.1378/chest.101.2.385. [DOI] [PubMed] [Google Scholar]
- BECK G. J., SEANOR H. E., BARACH A. L., GATES D. Effects of pressure breathing on venous pressure; a comparative study of positive pressure applied to the upper respiratory passageway and negative pressure to the body of normal individuals. Am J Med Sci. 1952 Aug;224(2):169–174. doi: 10.1097/00000441-195208000-00007. [DOI] [PubMed] [Google Scholar]
- Biondi J. W., Schulman D. S., Soufer R., Matthay R. A., Hines R. L., Kay H. R., Barash P. G. The effect of incremental positive end-expiratory pressure on right ventricular hemodynamics and ejection fraction. Anesth Analg. 1988 Feb;67(2):144–151. [PubMed] [Google Scholar]
- Bradley T. D., Holloway R. M., McLaughlin P. R., Ross B. L., Walters J., Liu P. P. Cardiac output response to continuous positive airway pressure in congestive heart failure. Am Rev Respir Dis. 1992 Feb;145(2 Pt 1):377–382. doi: 10.1164/ajrccm/145.2_Pt_1.377. [DOI] [PubMed] [Google Scholar]
- Branthwaite M. A. Assisted ventilation 6. Non-invasive and domiciliary ventilation: positive pressure techniques. Thorax. 1991 Mar;46(3):208–212. doi: 10.1136/thx.46.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braschi A., Iotti G. Partial ventilatory support in 1989. Intensive Care Med. 1989;15(8):488–490. doi: 10.1007/BF00273557. [DOI] [PubMed] [Google Scholar]
- Brochard L., Harf A., Lorino H., Lemaire F. Inspiratory pressure support prevents diaphragmatic fatigue during weaning from mechanical ventilation. Am Rev Respir Dis. 1989 Feb;139(2):513–521. doi: 10.1164/ajrccm/139.2.513. [DOI] [PubMed] [Google Scholar]
- Brochard L., Isabey D., Piquet J., Amaro P., Mancebo J., Messadi A. A., Brun-Buisson C., Rauss A., Lemaire F., Harf A. Reversal of acute exacerbations of chronic obstructive lung disease by inspiratory assistance with a face mask. N Engl J Med. 1990 Nov 29;323(22):1523–1530. doi: 10.1056/NEJM199011293232204. [DOI] [PubMed] [Google Scholar]
- Brochard L., Pluskwa F., Lemaire F. Improved efficacy of spontaneous breathing with inspiratory pressure support. Am Rev Respir Dis. 1987 Aug;136(2):411–415. doi: 10.1164/ajrccm/136.2.411. [DOI] [PubMed] [Google Scholar]
- Cassidy S. S., Robertson C. H., Jr, Pierce A. K., Johnson R. L., Jr Cardiovascular effects of positive end-expiratory pressure in dogs. J Appl Physiol Respir Environ Exerc Physiol. 1978 May;44(5):743–750. doi: 10.1152/jappl.1978.44.5.743. [DOI] [PubMed] [Google Scholar]
- Cook T. I., Trimble C., Smith D. E., Rehman I., Trummer M. J. Intermittent positive pressure and extrathoracic assisted breathing in hypovolemia. Comparative hemodynamic effects. Arch Surg. 1971 Jun;102(6):586–588. doi: 10.1001/archsurg.1971.01350060050014. [DOI] [PubMed] [Google Scholar]
- Kharasch E. D., Yeo K. T., Kenny M. A., Buffington C. W. Atrial natriuretic factor may mediate the renal effects of PEEP ventilation. Anesthesiology. 1988 Dec;69(6):862–869. doi: 10.1097/00000542-198812000-00010. [DOI] [PubMed] [Google Scholar]
- Kinnear W., Petch M., Taylor G., Shneerson J. Assisted ventilation using cuirass respirators. Eur Respir J. 1988 Mar;1(3):198–203. [PubMed] [Google Scholar]
- Leech J. A., Ascah K. J. Hemodynamic effects of nasal CPAP examined by Doppler echocardiography. Chest. 1991 Feb;99(2):323–326. doi: 10.1378/chest.99.2.323. [DOI] [PubMed] [Google Scholar]
- MacIntyre N. R. Respiratory function during pressure support ventilation. Chest. 1986 May;89(5):677–683. doi: 10.1378/chest.89.5.677. [DOI] [PubMed] [Google Scholar]
- MacIntyre N., Nishimura M., Usada Y., Tokioka H., Takezawa J., Shimada Y. The Nagoya conference on system design and patient-ventilator interactions during pressure support ventilation. Chest. 1990 Jun;97(6):1463–1466. doi: 10.1378/chest.97.6.1463. [DOI] [PubMed] [Google Scholar]
- Marini J. J., O'Quin R., Culver B. H., Butler J. Estimation of transmural cardiac pressures during ventilation with PEEP. J Appl Physiol Respir Environ Exerc Physiol. 1982 Aug;53(2):384–391. doi: 10.1152/jappl.1982.53.2.384. [DOI] [PubMed] [Google Scholar]
- Marini J. J., Smith T. C., Lamb V. J. External work output and force generation during synchronized intermittent mechanical ventilation. Effect of machine assistance on breathing effort. Am Rev Respir Dis. 1988 Nov;138(5):1169–1179. doi: 10.1164/ajrccm/138.5.1169. [DOI] [PubMed] [Google Scholar]
- Martin D. J., Grimbert F. A., Baconnier P., Benchetrit G. Effect of acute hypoxia on lung transvascular filtration in anaesthetized dogs. Bull Eur Physiopathol Respir. 1983 Jan-Feb;19(1):7–11. [PubMed] [Google Scholar]
- Nava S., Ambrosino N., Rubini F., Fracchia C., Rampulla C., Torri G., Calderini E. Effect of nasal pressure support ventilation and external PEEP on diaphragmatic activity in patients with severe stable COPD. Chest. 1993 Jan;103(1):143–150. doi: 10.1378/chest.103.1.143. [DOI] [PubMed] [Google Scholar]
- Nava S., Ambrosino N., Zocchi L., Rampulla C. Diaphragmatic rest during negative pressure ventilation by pneumowrap. Assessment in normal and COPD patients. Chest. 1990 Oct;98(4):857–865. doi: 10.1378/chest.98.4.857. [DOI] [PubMed] [Google Scholar]
- Petrof B. J., Kimoff R. J., Levy R. D., Cosio M. G., Gottfried S. B. Nasal continuous positive airway pressure facilitates respiratory muscle function during sleep in severe chronic obstructive pulmonary disease. Am Rev Respir Dis. 1991 May;143(5 Pt 1):928–935. doi: 10.1164/ajrccm/143.5_Pt_1.928. [DOI] [PubMed] [Google Scholar]
- Pinsky M. R., Desmet J. M., Vincent J. L. Effect of positive end-expiratory pressure on right ventricular function in humans. Am Rev Respir Dis. 1992 Sep;146(3):681–687. doi: 10.1164/ajrccm/146.3.681. [DOI] [PubMed] [Google Scholar]
- Prakash O., Meij S. Cardiopulmonary response to inspiratory pressure support during spontaneous ventilation vs conventional ventilation. Chest. 1985 Sep;88(3):403–408. doi: 10.1378/chest.88.3.403. [DOI] [PubMed] [Google Scholar]
- Qvist J., Pontoppidan H., Wilson R. S., Lowenstein E., Laver M. B. Hemodynamic responses to mechanical ventilation with PEEP: the effect of hypervolemia. Anesthesiology. 1975 Jan;42(1):45–55. doi: 10.1097/00000542-197501000-00009. [DOI] [PubMed] [Google Scholar]
- Robotham J. L., Badke F. R., Kindred M. K., Beaton M. K. Regional left ventricular performance during normal and obstructed spontaneous respiration. J Appl Physiol Respir Environ Exerc Physiol. 1983 Aug;55(2):569–577. doi: 10.1152/jappl.1983.55.2.569. [DOI] [PubMed] [Google Scholar]
- Robotham J. L., Lixfeld W., Holland L., MacGregor D., Bromberger-Barnea B., Permutt S., Rabson J. L. The effects of positive end-expiratory pressure on right and left ventricular performance. Am Rev Respir Dis. 1980 Apr;121(4):677–683. doi: 10.1164/arrd.1980.121.4.677. [DOI] [PubMed] [Google Scholar]
- Scharf S. M., Brown R., Saunders N., Green L. H. Hemodynamic effects of positive-pressure inflation. J Appl Physiol Respir Environ Exerc Physiol. 1980 Jul;49(1):124–131. doi: 10.1152/jappl.1980.49.1.124. [DOI] [PubMed] [Google Scholar]
- Skaburskis M., Helal R., Zidulka A. Hemodynamic effects of external continuous negative pressure ventilation compared with those of continuous positive pressure ventilation in dogs with acute lung injury. Am Rev Respir Dis. 1987 Oct;136(4):886–891. doi: 10.1164/ajrccm/136.4.886. [DOI] [PubMed] [Google Scholar]
- Suter P. M., Fairley B., Isenberg M. D. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med. 1975 Feb 6;292(6):284–289. doi: 10.1056/NEJM197502062920604. [DOI] [PubMed] [Google Scholar]
- WHITTENBERGER J. L., McGREGOR M., BERGLUND E., BORST H. G. Influence of state of inflation of the lung on pulmonary vascular resistance. J Appl Physiol. 1960 Sep;15:878–882. doi: 10.1152/jappl.1960.15.5.878. [DOI] [PubMed] [Google Scholar]
- Wallis T. W., Robotham J. L., Compean R., Kindred M. K. Mechanical heart-lung interaction with positive end-expiratory pressure. J Appl Physiol Respir Environ Exerc Physiol. 1983 Apr;54(4):1039–1047. doi: 10.1152/jappl.1983.54.4.1039. [DOI] [PubMed] [Google Scholar]


