Abstract
Objective:
In some medical circumstances, pediatric patients may need premedication for transferring to the operating room. In these situations, using intravenous premedication is preferred. We assessed the efficacy and safety of intravenous midazolam, intravenous ketamine, and combination of both to reduce the anxiety and improve behavior in children undergoing general anesthesia.
Methods:
In a double-blind randomized clinical trial, 90 pediatric patients aged 6 months to 6 years with American Society of Anesthesiologist grade I or II were enrolled. Before anesthesia, children were randomly divided into three groups to receive intravenous midazolam 0.1 mg/kg, or intravenous ketamine 1 mg/kg, or combination of half doses of both. Behavior types and sedation scores were recorded before premedication, after premedication, before anesthesia, and after anesthesia in the postanesthesia care unit. Anesthesia time, recovery duration, blood pressure, and heart rate were also recorded. For comparing distribution of behavior types and sedation scores among three groups, we used Kruskal–Wallis test, and for comparing mean and standard deviation of blood pressure and heart rates, we used analysis of variance.
Findings:
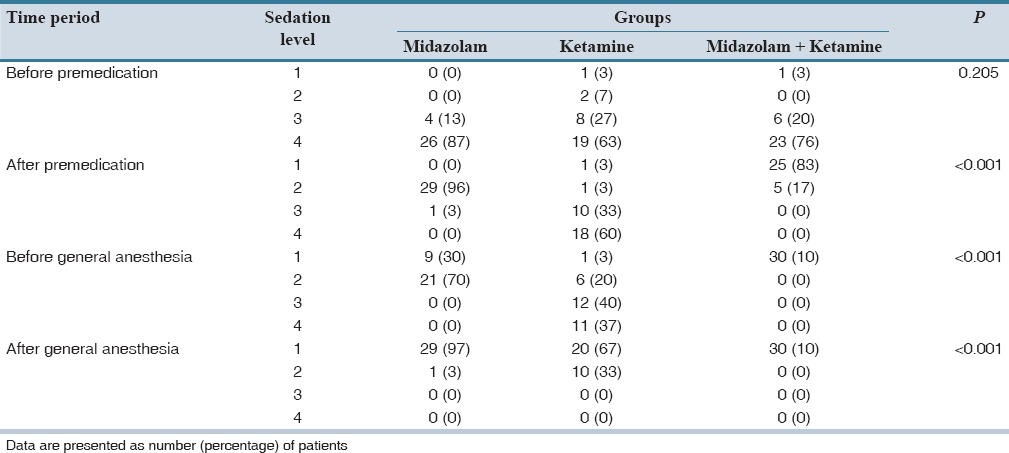
After premedication, children's behavior was significantly better in the combination group (P < 0.001). After anesthesia, behavior type was same among three groups (P = 0.421). Sedation scores among three groups were also different after premedication and the combination group was significantly more sedated than the other two groups (P < 0.001).
Conclusion:
Combination of 0.05 mg/kg of intravenous midazolam and 0.5 mg/kg of intravenous ketamine as premedication produced more deep sedation and more desirable behavior in children compared with each midazolam 0.1 mg/kg or ketamine 1 mg/kg.
Keywords: Ketamine, Midazolam, pediatric, premedication
INTRODUCTION
About 70% of children before anesthesia show a lot of stress and anxiety.[1] This stress and anxiety not only can disturb course of anesthesia but also can produce complications such as emergence delirium, psychiatric disorders, increased infection, increased postoperative pain, and therefore, increase duration of stay in postanesthesia care unit (PACU).[2,3,4,5] Therefore preparation of children before anesthesia is necessary, which take place as psychological and pharmacological intervention. Different kinds of medical products have been used for premedication such as anticholinergic drugs, opioids, barbiturates, benzodiazepines, and ketamine.[6,7,8] Midazolam is a water-soluble, short-acting benzodiazepine with rapid onset, short duration of action. It is an anxiolytic and sedative agent with minimal side effects.[9] Midazolam in comparison with placebo was superior for premedication in presence of children parents.[10] Ketamine is a phencyclidine derivative which acts on the n-methyl d-aspartate receptors and causes central dissociation of the cerebral cortex while providing amnesia and analgesia and applied for premedication in different studies.[11,12] In the literature, there are studies comparing the effects of midazolam and ketamine or their combination for premedication, which in most of them, the route of premedication was orally because of no availability for intravenous line before anesthesia. One study which performed during 2005 on 60 pediatric patients, in one group oral midazolam, 0.5 mg/kg was prescribed, and in other group midazolam 0.25 mg/kg plus ketamine 4 mg/kg were administered orally before anesthesia. Combination group had more desired effects for sedation and analgesia than midazolam group.[13] In another study which compared the effects of midazolam, ketamine, and combination of them as oral premedication, ketamine group, and combination group were superior to midazolam, but these two groups did not have any superiority to each other.[14] Paradoxical reactions to intravenous midazolam are restlessness, violent behavior, physical assault, act of self-injury, and need for restraints, and may occur after premedication especially with higher doses.[15] In another study, combination of intravenous form of midazolam and ketamine was superior to meperidine plus midazolam in cancer patients.[16] Until now, few studies were done with intravenous form of ketamine and midazolam as premedication. However, sometimes inpatient pediatrics patients with previous existing intravenous line need to prepare for operating room, while intravenous premedication is superior in this situation. Then in this study, we decided to compare the efficacy and safety of intravenous midazolam (0.1 mg/kg), intravenous ketamine (1 mg/kg), and combination of both (0.05 mg/kg and 0.5 mg/kg), respectively, to reduce the stress and anxiety in children undergoing inpatient general anesthesia and surgery. The first endpoint of the study was comparing of the child behavior after receiving the premedication and the second aims were about sedation degree, stability of the vital signs, anesthesia time, and recovery duration.
METHODS
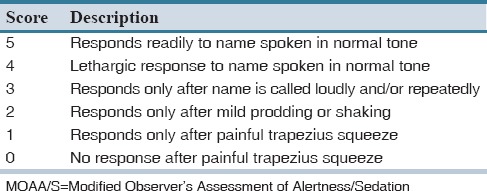
In a double-blind randomized clinical trial, after obtaining approval of Ethics and Research Committee and written informed consent by the parents’ child, 95 patients who were scheduled for elective abdominal surgery in Al-Zahra Medical Center (Isfahan, Iran) from January 2013 to December 2013 were enrolled in the study. Inclusion criteria were: Age between 6 months and 6 years, American Society of Anesthesiologist grades I and II, and elective abdominal surgery under general anesthesia. Exclusion criteria were refusal of the parents and patients, intraoperative complications including bleeding, respiratory depression, and allergy to study drugs. Patients were randomly allocated into one of three study groups. All study drugs were prepared by premedication room physician in solutions contained 1 mg/ml midazolam, or 10 mg/ml ketamine, or 0.5 mg/ml midazolam plus 5 mg/ml ketamine according to patients study group codes. Ten min before the operation, each child received 0.1 ml/kg of the study drug, intravenously, according to the code that was given to the patient. All the codes remained closed until the study was finished. None of researchers did know about patient groups until the study was finished and the codes were opened. Premedication was performed in the presence of parent's child. Child behavior was recorded according to 4-points behavior score of the child [Table 1].[17] Also sedation level was recorded according to the Modified Observer's Assessment of Alertness/Sedation Scale (MOAA/S) [Table 2].[17] Behavior score and MOAA/S were recorded in three groups in 4 times: Before premedication, after premedication, before induction of anesthesia, and in the PACU.[17] Blood pressure, saturation of oxygen, and heart rate were recorded after premedication, before induction of anesthesia and 5 min after induction of anesthesia and intubation. Anesthesia was induced with 2 mcg/kg fentanyl, 5 mg/kg sodium thiopental, and 0.6 mg/kg atracurium, and then tracheal intubation was done. Maintenance of anesthesia was performed with 50% oxygen in air and 1.2% minimum alveolar concentration of isoflurane. At the end of anesthesia, the residual effect of muscle relaxants was reversed by applying 0.02 mg/kg of atropine and 0.05 mg/kg of neostigmine. Patient was extubated following full consciousness. Extubation time was defined as the time from discontinuation of inhalation drug to extubation of trachea and recorded in the questionnaire. Recovery from anesthesia was recorded as the duration from arriving to the PACU to the time taken to reach a modified Aldrete score 7/8 for discharge from PACU.[18]
Table 1.
Behavior scores
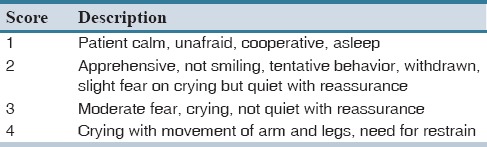
Table 2.
MOAA/S scale
The sample size of our study was selected according to anxiety behavior data in Ghai et al. study,[7] using 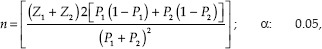 β: 39.52%, P1: 39.52%, and P2: 18.32%. All analyses were carried out using the Statistical Package for Social Sciences Software version 20 (Version 20, SPSS Inc., Chicago, IL). Data were expressed as mean ± standard deviation (SD) or number (percent). For comparing distribution of behavior types and sedation scores among three groups, we used Kruskal–Wallis test, and for comparing mean and SD of blood pressure and heart rates, we used analysis of variance. Behavioral types were scored from 1 to 4, and considered satisfied when it was 1 or 2. Sedation was scored from 1 to 6, and it was considered satisfactory if it was from 1 to 4. We considered P < 0.05 as statistically significant.
β: 39.52%, P1: 39.52%, and P2: 18.32%. All analyses were carried out using the Statistical Package for Social Sciences Software version 20 (Version 20, SPSS Inc., Chicago, IL). Data were expressed as mean ± standard deviation (SD) or number (percent). For comparing distribution of behavior types and sedation scores among three groups, we used Kruskal–Wallis test, and for comparing mean and SD of blood pressure and heart rates, we used analysis of variance. Behavioral types were scored from 1 to 4, and considered satisfied when it was 1 or 2. Sedation was scored from 1 to 6, and it was considered satisfactory if it was from 1 to 4. We considered P < 0.05 as statistically significant.
RESULTS
A total of 95 children were recruited in the study. Five children were excluded. There were no significant differences in the demographic data, surgical duration, and distribution of surgical procedures in the three groups [Table 3]. Mean heart rate and systolic blood pressure values were summarized in Figures 1 and 2. In ketamine group, heart rate was significantly increased compared to midazolam and ketamine + midazolam groups. There were no significant differences among three groups regarding behavioral types, before premedication. After premedication, children's behavior type was significantly better in the combination group (P < 0.001). After anesthesia, behavior types were the same among three groups [Table 4]. Sedation scores before premedication were 5 and 6 for all children except for four children who had scores 3 and 4. Sedation among the groups was also significantly different after premedication and the combination group was significantly better sedated than the two other groups (P < 0.001) [Table 5]. There were no significant differences for extubation time and recovery time among three groups [Table 3].
Table 3.
Demographic data, duration of surgery, recovery time and anesthetic drug doses of study groups
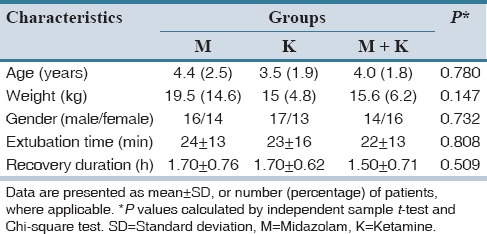
Figure 1.
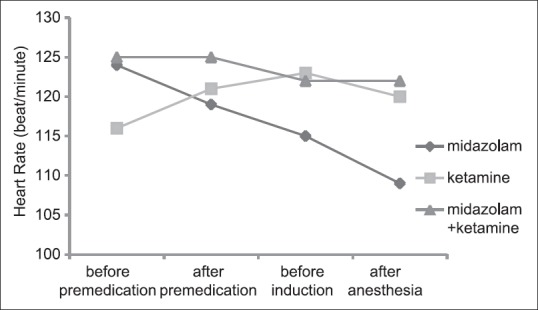
Comparison of the means of heart rate among three study groups in different times
Figure 2.
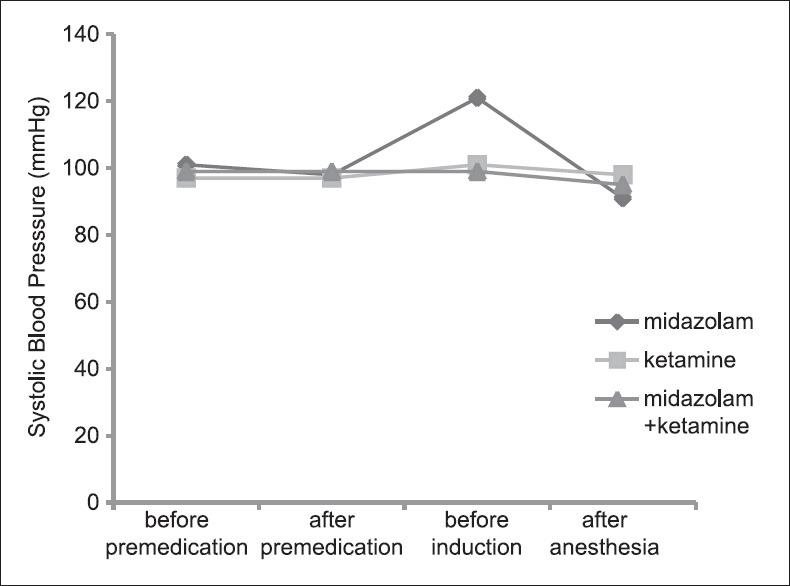
Comparison of the means of systolic blood pressure among three study groups in different times
Table 4.
Frequency distribution of behavioral types in three groups at different times of the study
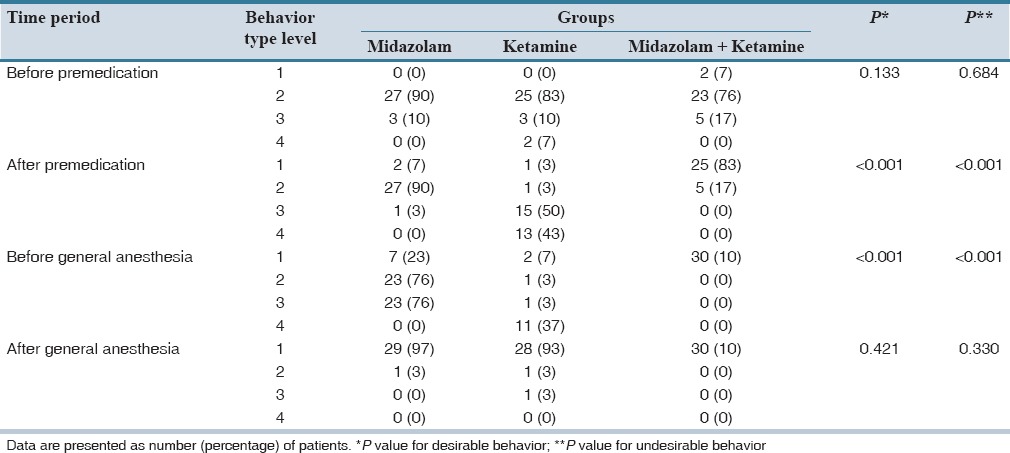
Table 5.
Frequency distribution of sedation scores in three groups at different times of the study
DISCUSSION
Surgery and anesthesia can cause considerable emotional stress on children and their parents. The preoperative anxiety in children can lead to postoperative medical, psychological, and physiological abnormality such as; eating problems, bad dreams, enuresis, increased fear of doctors, and hospital. Premedication should be performed in all pediatric patients, in order to decrease preoperative anxiety, allow smooth induction, and prevent postoperative psychological insult and behavioral changes.[19,20] We assessed the efficacy and safety of midazolam 0.1 mg/kg, ketamine 1 mg/kg, and combination of half doses of midazolam and ketamine intravenously to reduce the stress and anxiety in children undergoing surgical procedures. According to our study, intravenous premedication with combination of half doses of midazolam and ketamine makes earlier and more effective sedation than midazolam or ketamine alone in full dose premedication. Children behavior type was proper in combination group than each group separately. In previous studies both midazolam and ketamine were used as premedication in different situation. Most of these studies were about oral and intranasal form of these two drugs. Both midazolam and ketamine have untoward side effects in higher doses. Nowadays combination of them was enthusiastic for researcher.[21] These studies had controversial results. In one study in 2005 effectiveness of oral midazolam (0.5 mg/kg) and oral ketamine (50 mg) on sedation, separation of children from parents and acceptance for mask ventilation by children were evaluated and midazolam was superior to ketamine with lower side effects.[22] In Darlong et al. study efficacy of oral midazolam (0.25 mg/kg), oral ketamine (3 mg/kg), and combination of them were studied on sedation degree, children behavior type, and separation of children from parents.[23] In combination group, desirable sedation scores after 10 and 20 min were significantly specific than other group. Children separation behavior type score was not significant among groups. This finding of Darlong et al. study was not coordinate with our study.[23] Another study which was performed in 2011 by Banerjee et al. sedative effect of oral midazolam, ketamine, and combination of them was evaluated. Again after 20 min of prescription of premedication, sedation degree was superior in combination group, and after 30 min sedation degree in midazolam group was comparable with combination group.[24] In another study which was conducted by Ghai et al. there were no significant differences between two groups: Oral midazolam and midazolam plus ketamine.[7] In this study, Group M received 0.5 mg/kg oral midazolam and Group MK received 0.25 mg/kg oral midazolam with 2.5 mg/kg oral ketamine. Both groups provided equally effective anxiolytics and separation characteristics. However, the combination group provided more children in an awake, calm, and quiet state who could be separated easily from parents.[7] In the study which was done by Mostafa and Morsy premedication for bone marrow biopsy were done with dexmedetomidine, midazolam, and ketamine intranasal and dexmedetomidine had faster sedation score and better parents separation score than two other groups and midazolam and dexmedetomidine has better sedation score than ketamine.[19]
The study which was done by Ozcan et al. showed that low dose of midazolam and ketamine as premedication was not effective for reducing anxiety in children who received caudal block under sevoflurane anesthesia.[25]
As shown in Figure 1, heart rate increased in ketamine group. This finding is coordinate with the other study about sympathomimetic effect of ketamine.[26] Although the mechanism for this increasing of heart rate is not well-known, but it may be due to the effect of the ketamine on heart muscle.[27] According to Figure 1, midazolam decreased heart rate. This finding is not in accordance with benzodiazepines pharmacology, because benzodiazepines with reducing systemic vascular resistance causes increase in heart rate. This discrepancy may be the result of producing sedation in children and then decreasing heart rate. Linares Segovia et al. compared the efficacy of intranasal dexmedetomidine with oral midazolam to reduce preoperative anxiety in pediatric patients. In this study, there were no decreases in heart rate and blood pressure in oral midazolam group.[20] This finding is also different from findings of our study. In our study, recovery time was not significant among group. This finding also is different with Darlong et al. study which had prolonged recovery time in ketamine group.[23]
In this study, we found that combination of 0.05 mg/kg of intravenous midazolam and 0.5 mg/kg of intravenous ketamine as premedication produced more deep sedation and more desirable behavior in children compared with each midazolam 0.1 mg/kg or ketamine 1 mg/kg.
AUTHORS’ CONTRIBUTION
Sajedi designed study, Habibi gathered data, Sajedi and Habibi participated in statistical analysis and calculations and drafted the manuscript and Sajedi supervised the study and revised the manuscript.
Financial support and sponsorship
Research Department, Isfahan University of Medical Sciences, Isfahan, Iran.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kain ZN, Mayes LC, O’Connor TZ, Cicchetti DV. Preoperative anxiety in children. Predictors and outcomes. Arch Pediatr Adolesc Med. 1996;150:1238–45. doi: 10.1001/archpedi.1996.02170370016002. [DOI] [PubMed] [Google Scholar]
- 2.Kain ZN, Caldwell-Andrews AA, Maranets I, McClain B, Gaal D, Mayes LC, et al. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth Analg. 2004;99:1648–54. doi: 10.1213/01.ANE.0000136471.36680.97. [DOI] [PubMed] [Google Scholar]
- 3.Ader R, Cohen N, Felten D. Psychoneuroimmunology: Interactions between the nervous system and the immune system. Lancet. 1995;345:99–103. doi: 10.1016/s0140-6736(95)90066-7. [DOI] [PubMed] [Google Scholar]
- 4.Deshpande S, Platt MP, Aynsley-Green A. Patterns of the metabolic and endocrine stress response to surgery and medical illness in infancy and childhood. Crit Care Med. 1993;21(9 Suppl):S359–61. doi: 10.1097/00003246-199309001-00036. [DOI] [PubMed] [Google Scholar]
- 5.Kain ZN, Mayes LC, Caldwell-Andrews AA, Karas DE, McClain BC. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics. 2006;118:651–8. doi: 10.1542/peds.2005-2920. [DOI] [PubMed] [Google Scholar]
- 6.Funk W, Jakob W, Riedl T, Taeger K. Oral preanaesthetic medication for children: Double-blind randomized study of a combination of midazolam and ketamine vs midazolam or ketamine alone. Br J Anaesth. 2000;84:335–40. doi: 10.1093/oxfordjournals.bja.a013435. [DOI] [PubMed] [Google Scholar]
- 7.Ghai B, Grandhe RP, Kumar A, Chari P. Comparative evaluation of midazolam and ketamine with midazolam alone as oral premedication. Paediatr Anaesth. 2005;15:554–9. doi: 10.1111/j.1460-9592.2004.01523.x. [DOI] [PubMed] [Google Scholar]
- 8.Machata AM, Willschke H, Kabon B, Kettner SC, Marhofer P. Propofol-based sedation regimen for infants and children undergoing ambulatory magnetic resonance imaging. Br J Anaesth. 2008;101:239–43. doi: 10.1093/bja/aen153. [DOI] [PubMed] [Google Scholar]
- 9.Kain ZN, Mayes LC, Bell C, Weisman S, Hofstadter MB, Rimar S. Premedication in the United States: A status report. Anesth Analg. 1997;84:427–32. doi: 10.1097/00000539-199702000-00035. [DOI] [PubMed] [Google Scholar]
- 10.Kain ZN, Mayes LC, Wang SM, Caramico LA, Hofstadter MB. Parental presence during induction of anesthesia versus sedative premedication: Which intervention is more effective? Anesthesiology. 1998;89:1147–56. doi: 10.1097/00000542-199811000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Gutstein HB, Johnson KL, Heard MB, Gregory GA. Oral ketamine preanesthetic medication in children. Anesthesiology. 1992;76:28–33. doi: 10.1097/00000542-199201000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Tobias JD, Phipps S, Smith B, Mulhern RK. Oral ketamine premedication to alleviate the distress of invasive procedures in pediatric oncology patients. Pediatrics. 1992;90:537–41. [PubMed] [Google Scholar]
- 13.Rabie M. Combination of oral ketamin and midazolam versus midazolam alone as a premedication in children undergoing tonsilectomy. Alex J Anesth Intensive Care. 2005;8:58–64. [Google Scholar]
- 14.Gharde P, Chauhan S, Kiran U. Evaluation of efficacy of intranasal midazolam, ketamine and their mixture as premedication and its relation with bispectral index in children with tetralogy of fallot undergoing intracardiac repair. Ann Card Anaesth. 2006;9:25–30. [PubMed] [Google Scholar]
- 15.Golparvar M, Saghaei M, Sajedi P, Razavi SS. Paradoxical reaction following intravenous midazolam premedication in pediatric patients – A randomized placebo controlled trial of ketamine for rapid tranquilization. Paediatr Anaesth. 2004;14:924–30. doi: 10.1111/j.1460-9592.2004.01349.x. [DOI] [PubMed] [Google Scholar]
- 16.Marx CM, Stein J, Tyler MK, Nieder ML, Shurin SB, Blumer JL. Ketamine-midazolam versus meperidine-midazolam for painful procedures in pediatric oncology patients. J Clin Oncol. 1997;15:94–102. doi: 10.1200/JCO.1997.15.1.94. [DOI] [PubMed] [Google Scholar]
- 17.Yuen VM, Hui TW, Irwin MG, Yuen MK. A comparison of intranasal dexmedetomidine and oral midazolam for premedication in pediatric anesthesia: A double-blinded randomized controlled trial. Anesth Analg. 2008;106:1715–21. doi: 10.1213/ane.0b013e31816c8929. [DOI] [PubMed] [Google Scholar]
- 18.Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970;49:924–34. [PubMed] [Google Scholar]
- 19.Mostafa MG, Morsy KM. Premedication with intranasal dexmedetomidine, midazolam and ketamine for children undergoing bone marrow biopsy and aspirate. Egypt J Anaesth. 2013;29:131–5. [Google Scholar]
- 20.Linares Segovia B, García Cuevas MA, Ramírez Casillas IL, Guerrero Romero JF, Botello Buenrostro I, Monroy Torres R, et al. Pre-anesthetic medication with intranasal dexmedetomidine and oral midazolam as an anxiolytic. A clinical trial. An Pediatr (Barc) 2014;81:226–31. doi: 10.1016/j.anpedi.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 21.Ghai B, Grandhe RP, Kumar A, Chari P. Comparative evaluation of midazolam and ketamine with midazolam alone as oral premedication. Paediatr Anaesth. 2005;15:554–9. doi: 10.1111/j.1460-9592.2004.01523.x. [DOI] [PubMed] [Google Scholar]
- 22.Horiuchi T, Kawaguchi M, Kurehara K, Kawaraguchi Y, Sasaoka N, Furuya H. Evaluation of relatively low dose of oral transmucosal ketamine premedication in children: A comparison with oral midazolam. Paediatr Anaesth. 2005;15:643–7. doi: 10.1111/j.1460-9592.2004.01513.x. [DOI] [PubMed] [Google Scholar]
- 23.Darlong V, Shende D, Subramanyam MS, Sunder R, Naik A. Oral ketamine or midazolam or low dose combination for premedication in children. Anaesth Intensive Care. 2004;32:246–9. doi: 10.1177/0310057X0403200214. [DOI] [PubMed] [Google Scholar]
- 24.Banerjee B, Bose A, Pahari S, Dan AK. A comparative study of paediatric oral premedication: Midazolam, ketamine and low dose combination of midazolam and ketamine. J Indian Med Assoc. 2011;109:386–8. [PubMed] [Google Scholar]
- 25.Ozcan A, Kaya AG, Ozcan N, Karaaslan GM, Er E, Baltaci B, et al. Effects of ketamine and midazolam on emergence agitation after sevoflurane anaesthesia in children receiving caudal block: A randomized trial. Rev Bras Anestesiol. 2014;64:377–81. doi: 10.1016/j.bjan.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 26.Haas DA, Harper DG. Ketamine: A review of its pharmacologic properties and use in ambulatory anesthesia. Anesth Prog. 1992;39:61–8. [PMC free article] [PubMed] [Google Scholar]
- 27.Barrigon S, De Miguel B, Tamargo J, Tejerina T. The mechanism of the positive inotropic action of ketamine on isolated atria of the rat. Br J Pharmacol. 1982;76:85–93. doi: 10.1111/j.1476-5381.1982.tb09193.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


