Abstract
Objective:
There is few data regarding the correlation between serum Vitamin D level and unfavorable intensive care unit (ICU) outcome in postsurgical patients. In this study, correlation between serum 25(OH)D level and length of ICU stay and in-hospital mortality has been evaluated in critically ill surgical patients.
Methods:
Serum 25(OH)D has been evaluated in 70 surgical, critically ill patients. Demographic, laboratory, and clinical data of the patients were collected. Correlation between serum 25(OH) D level and duration of ICU stay and hospital mortality was evaluated using two-factor analysis of covariance. Multivariable Cox-regression analysis was used for adjusting the effect of season of blood sampling and type of surgery on the main variables. For all the analyses, P values less than or equal to 0.05 were considered as statistically significant.
Findings:
Serum 25(OH)D deficiency was identified in 52 (74.3%) of the patients. Patients with serum Vitamin D levels < 30 ng/ml had longer length of ICU stay than those with serum Vitamin D levels ≥ 30 ng/ml (7.8 ± 5.1 vs. 4.05 ± 2.12 days, P = 0.003). Although hospital mortality was more common in Vitamin D deficient patients than sufficient ones (25% in deficient group versus 22.2% in sufficient group), there was no significant difference regarding hospital mortality rate between the groups.
Conclusion:
Statistically significant association was found between low 25(OH)D level and increased length of ICU stay in critically ill surgical patients. It could be explained by favorable effects of Vitamin D on immune system functions, reducing tissue dysfunction, and risk of organ failure and overall complications. However, there was no correlation between serum Vitamin D level and patients’ in-hospital mortality. Further, well-designed prospective clinical studies with adequate sample size are needed to evaluate correlation between serum Vitamin D level and mortality in critically ill patients.
Keywords: Critically ill patients, intensive care unit stay, mortality, surgical, Vitamin D
INTRODUCTION
Vitamin D deficiency is common around the world and it is estimated that 1 billion peoples are living with inadequate Vitamin D.[1,2] Although the main known physiologic function of Vitamin D is the regulation of calcium and phosphorus homeostasis, it has been shown that Vitamin D plays a major role in the extraskeletal metabolic processes such as glucose metabolism, immunomodulation, renin-angiotensin system regulation, cell growth, membrane stabilizing, angiogenesis, anti-proliferation, and apoptosis.[2,3,4,5]
Vitamin D insufficiency has been reported in more than 80% of critically ill patients, hospitalized in intensive care unit (ICU).
Unexpectedly, up to 17% of this population had undetectable serum level of 25(OH)D.[6,7,8]
Decrease in the serum Vitamin D level during ICU stay can be explained by the lack of exposure to sunlight and insufficient replacement of this vitamin through parental or enteral metabolic support.[9] Several studies have evaluated the relationship between serum Vitamin D level and clinical outcome in critically ill patients. In some of the surveys, it has been shown that low serum level of 25(OH)D was associated with adverse clinical outcome such as prolonged length of ICU stay, organ dysfunction, acquiring nosocomial infections, acute kidney injury (AKI), increased health care costs, and mortality.[8,10,11,12] While in other studies, the correlation between the serum Vitamin D level and worse outcome has not been detected in this population.[13,14,15]
However, in most of the studies, patient care setting (medical, surgical, or trauma) and also type and severity of baseline diseases have not been considered in the final analysis. Surgical patients are more vulnerable to postoperative sudden cardiovascular events and infections that both of them may be aggravated by Vitamin D deficiency.[16,17]
There is few data regarding the correlation between serum Vitamin D level and unfavorable ICU outcome in postsurgical patients. In this study, correlation between serum 25(OH)D level and length of ICU stay and in-hospital mortality has been evaluated in surgical, critically ill patients.
METHODS
This prospective, cross-sectional, descriptive study was performed during 1-year period from early March 2014 to February 2015 at ICU of the Imam Khomeini Hospital affiliated to Tehran University of Medical Sciences, Tehran, Iran. The Institutional Review Board and the Medical Ethics Committee of the Hospital approved the study and all the patients or their family members signed and approved a written informed consent form.
During the study period, 70 surgical patients admitted to the ICU were recruited. Baseline patients’ demographic data, including sex, age, weight, body mass index (BMI), baseline diseases, and type of surgery, were collected from the patients’ medical records. Severity of patients’ clinical condition at ICU admission was evaluated based on the acute physiology and chronic health evaluation and simplified acute physiologic score criteria.
The patients’ laboratory parameters, including serum electrolytes (Na+, K+, Mg+2, and Ca+2), renal function tests (serum creatinine and urea), liver enzymes (alanine aminotransferase, aspartate aminotransferase, and alkaline phosphatase), and liver function indexes (serum albumin and bilirubin, international normalized ratio) also were recorded at the time of recruitment.
From each included patient, 5 ml of venous blood sample was collected at the time of ICU admission. The blood were centrifuged and separated serum samples were stored at −80°C up to the time of measurement of serum 25(OH)D level.
Serum 25(OH)D level was measured by ELISA (Immunodiagnostic Systems, Louvain-la-Neuve, Belgium). Calibration, control, and samples were diluted with biotin-labeled 25(OH)D. The diluted samples were incubated in microtiter wells, which were coated with highly specific sheep 25(OH)D antibody for 2 h at room temperature before aspiration and washing. Enzyme-labeled avidin was added and binded selectively to complexed biotin; then color was developed using a chromogenic substrate. The absorbance of the stopped reaction microtiter were read in a microtiter plate reader; color intensity developed being inversely proportional to the concentration of 25(OH)D. Serum 25(OH)D level <30 ng/ml was considered as Vitamin D deficiency.[2,18]
All the statistical analyses were performed by the SPSS (Statistical Package for the Social Sciences) version 18 software (IBM Corp., Armonk, NY, USA). The Kolmogorov–Smirnov test was used to assess the normal distribution of continuous variables. The data were expressed as a mean ± standard deviation. Categorical variables were reported as percentages. Association between serum 25(OH)D category and the main endpoints of study (duration of ICU stay and in-hospital mortality) was evaluated using two-factor analysis of covariance. Multivariable Cox-regression analysis was used for adjusting the effect of season of blood sampling and type of surgery on the main variables. For all the analyses, P values <0.05 were considered as statistical significant.
RESULTS
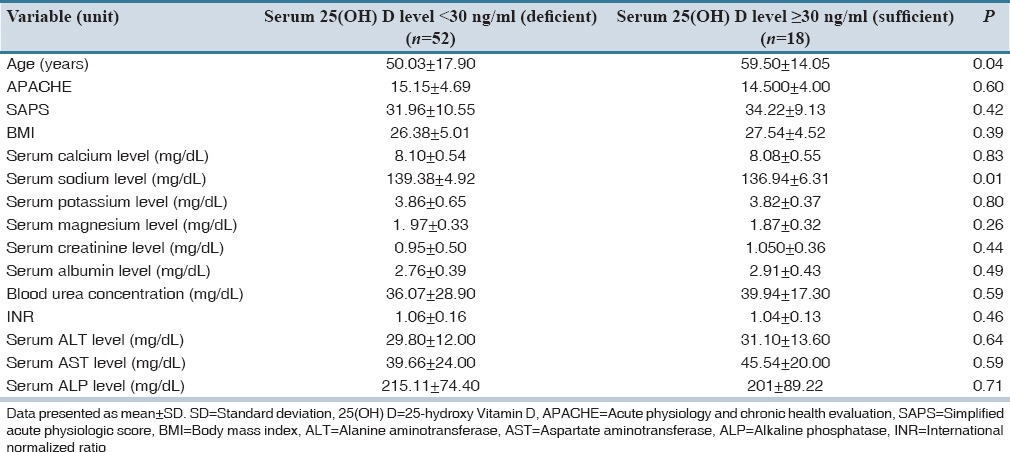
Of the 70 patients who were enrolled in this study, 31 (44.3%) were male and 39 (55.7%) were female. Serum 25(OH)D deficiency was identified in 52 (74.3%) patients. The characteristics of the study population regarding serum 25(OH)D level is shown in Table 1. Except for age, there was no significant difference in the baseline characteristics of patients with and without vitamin D deficiency. Vitamin D deficient patients were younger than sufficient ones (P = 0.04).
Table 1.
Characteristics of the patients regarding serum 25(OH) D levels
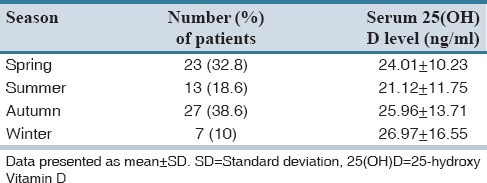
The patients’ serum 25(OH)D levels regarding season of the ICU admission were shown in Table 2. There was a nonsignificant difference between the patients’ serum 25(OH)D levels regarding the seasons of sampling (P = 0.39).
Table 2.
Season of admission of the patients and serum 25(OH) D levels
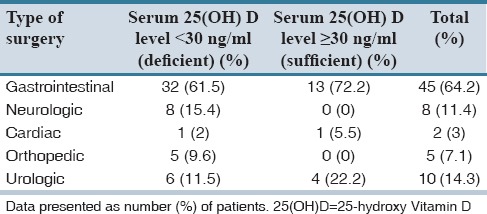
Regarding baseline disease, 17.1% of patients had a history of hypertension, 8.5% suffered from ischemic heart disease, and 52.8% had gastrointestinal diseases. Gastrointestinal surgery was the most common surgery type (61.5%) in the patients. Serum 25(OH)D level regarding the type of the surgery has been shown in Table 3. Considering the possible effect of different types of major surgeries with different stress-inducing properties on serum Vitamin D status, association between serum 25(OH)D level and type of surgery was evaluated. No difference in serum 25(OH)D level based on the type of surgery was detected (P = 0.41). Patients with serum Vitamin D levels <30 ng/ml had longer length of ICU stay than those with serum Vitamin D levels ≥30 ng/ml (7.8 ± 5.1 vs. 4.05 ± 2.12 days, P = 0.003).
Table 3.
Serum 25(OH) D levels of the patients based on the type of surgery
Following Cox-regression analysis, it was found that serum 25(OH)D status at the time of ICU admission can be a potential predictor for length of ICU stay following adjustment for age, sex, BMI, season, and type of surgery in critically ill surgical patients (P = 0.05).
Although hospital mortality was more common in Vitamin D deficient patients than sufficient ones (25% in deficient group vs. 22.2% in sufficient group), there was no significant difference regarding hospital mortality rate between the groups.
DISCUSSION
Vitamin D deficiency is common among critically ill medical and surgical patients. There is no uniform definition for Vitamin D deficiency in these populations. In general population, serum 25(OH)D level is defined as the best indicator of body's Vitamin D status, since it has longer half-life, more stability in the systemic circulation, and more positive correlation with calcium absorption in comparison with 1,25(OH)2D.[19,20]
There is no definite cut-off level for 25(OH)D that predict beneficial outcome in critically ill patients. In the previous studies, unfavorable outcome was associated with serum 25(OH)D level of 12 to 20 ng/ml in critically ill medical patients.[15,21,22] In critically ill surgical patients, serum 25(OH)D level more than 26 ng/ml showed beneficial effects.[8]
In analysis of the data from 32 studies published between 1966 and 2013, serum 25(OH)D concentration >30 ng/ml was associated with lower all-cause mortality in critically ill patients compared with concentration ≤30 ng/ml.[18]
In our study, serum 25(OH)D level <30 ng/ml was considered as a deficient cut-off in surgical patients.
There are some concerns regarding the accuracy of serum 25(OH)D level as the best indicator of Vitamin D status in critically ill patients. Liver and renal dysfunction, low serum albumin, and Vitamin D binding protein levels that are common in these patients may lead to falsely high serum 25(OH)D level.[23,24] However, the previous studies have shown association between low serum 25(OH)D and adverse clinical outcomes, including systemic inflammatory response syndrome, nosocomial bloodstream and respiratory tract infections, AKI and metabolic dysfunction as well as longer length of ICU stay, and all-cause mortality in critically ill patients.[25,26,27]
In this study, 74.3% of the Iranian critically ill surgical patients had Vitamin D deficiency. In a large multicentric study, in a general population of Iran, moderate to severe Vitamin D deficiency was detected in 75.1% and 72.1% of women and men, respectively.[28] Inadequate sun exposure, lack of Vitamin D food fortification program, clothing habits (especially among women), polymorphism in Vitamin D receptor, and low daily calcium intake introduced as predisposing factors of Vitamin D deficiency in middle-east countries.[29,30]
Although mechanisms of adverse ICU outcome resulting from hypovitaminosis D in critically ill patients have not been well-defined, several suggestions, including pleiotropic effects of Vitamin D on immunity, mucosal and endothelial functions, and different metabolic effects of Vitamin D have been reported.[2]
Due to seasonal variations in sunlight, blood sampling in winter and spring is associated with lower 25(OH)D levels compared with summer and fall seasons.[10,13] In our patients, we did not observe any correlation between serum Vitamin D level and seasonality. This finding might be expected since serum Vitamin D level in critically ill patients is less affected by seasonal changes due to immobility and restricted sun exposure, even before the ICU admission.
In this study, Vitamin D deficiency was associated with younger age. Similar finding was reported in another study in critically ill patients and can be related to the impact of common Vitamin D supplementation in an elderly population in recent years.[15]
Vitamin D deficiency was associated with increased length of ICU stay in our surgical critically ill patients. This is in line with other studies that showed the correlation between serum level of Vitamin D and length of ICU stay.[6,31] In Higgins et al. study, low serum levels of 25(OH)D was associated with increased time of ICU stay.[6] Also, in Zittermann et al. study, length of ICU stay was significantly higher in Vitamin D deficient cardiac surgery patients compared with adequate ones.[31] McKinney et al. reported similar results in medical critically ill patients.[32] Correlation between severity of Vitamin D deficiency and length of ICU stay has been reported by Matthews et al.[8] Contrary to the above studies, in Amrein et al., Venkatram et al. and Aygencel et al. studies, the correlation between Vitamin D insufficiency and length of ICU stay was not detected.[13,14,15]
The second endpoint of our study was evaluating the correlation between serum 25(OH)D level and the in-hospital mortality. Although mortality was more common in Vitamin D deficient critically ill surgical patients than those were sufficient, we did not find a significant correlation between hypovitaminosis D and in-hospital mortality. Similar to this study, in Flynn et al. prospective survey, no difference in mortality rate was reported between Vitamin D sufficient and deficient surgical critically ill patients.[17] In another study, Lucidarme et al. showed that mortality rate was unchanged by low serum Vitamin D level in critically ill patients.[33] Although, Aygencel et al. detected a correlation between mortality and Vitamin D insufficiency primarily in univariate analysis, Vitamin D insufficiency was not defined as an independent risk factor for mortality in the later multivariate analysis.[14]
In contrast to the previous studies, Zhang et al. in a meta-analysis of 7 cohort studies suggested that Vitamin D deficiency is associated with an increased risk of hospital mortality.[34] In addition, higher Vitamin D concentration was associated with a linear reduction of in-hospital mortality in Turan et al. study.[16] Venkatram et al. in a retrospective study, in a medical ICU, found a significant correlation between Vitamin D deficiency and mortality, but there was no correlation between Vitamin D insufficiency and hospital mortality. In that study, Vitamin D deficiency and insufficiency were defined as serum 25(OH)D level <20 ng/ml and 20 to 29 ng/ml, respectively.[15]
Following a single-center, retrospective, observational study in 655 surgical and nonsurgical critically ill patients, Amrein et al. reported the lowest in-hospital mortality at serum 25(OH)D levels between 20 and 40 ng/ml. They also proposed serum 25(OH)D level of 15 ng/ml as the cut-off point for in-hospital mortality.[13] Ralph et al. did not observe any association between low level of serum 25(OH)D at admission and increased risk of mortality in critically ill medical patients, but interestingly, patients with supraphysiologic serum Vitamin D levels at ICU admission had higher mortality rate.[35] Association between high serum 25(OH)D levels (>100 nmol/ml or >40 ng/ml) and adverse clinical outcome has been reported in a recent study of postcardiac surgery patients.[31] In the second recent study, as a 9 years follow-up, a reverse J-shaped correlation between serum 25(OH)D level and mortality has been shown and serum Vitamin D level more than 120 nmol/ml (or > 48 ng/ml) was associated with higher rate of mortality.[36]
No association between low serum levels of Vitamin D and in-hospital mortality in our study may be due to small number of the included patients, different cut-off point values for Vitamin D, deficiency in previous studies (most of the studies that supported correlation between serum 25(OH)D level and mortality used the concentrations below 20 ng/ml), and supraphysiologic serum 25(OH)D level in 72% of the patients in “sufficient” group (13 of 18 patients). The “J-shaped effect theory” should be considered in interpreting mortality rate in the Vitamin D sufficient group.
In our study, critically ill surgical patients were enrolled and so the heterogeneity among medical, surgical, and traumatic critically ill patients that mentioned in the several previous studies was considered. All the patients’ blood samples were collected at a definite time, at 5–7 a.m., in 1st-day of ICU admission. Also, the effects of potential confounders, including BMI and seasonal variation, were adjusted in the data analysis.
However, some limitations should be considered in our study. The major limitation was small sample size of the study. It was a single-center study and, therefore, the results could not be generalized. Serum Vitamin D levels were assessed only at the time of ICU admission in our patients. Serial Vitamin D assay may result in more reliable judgment about body's Vitamin D status. It was not possible to measure serum Vitamin D binding protein in our patients. Concentration of this protein can affect serum Vitamin D level, especially in critically ill patients with malnutrition.
Vitamin D deficiency is common in critically ill surgical patients. Statistically significant association was found between low 25(OH)D level and increased length of ICU stay in critically ill surgical patients. However, there was no correlation between serum Vitamin D level and patients’ in-hospital mortality. Further, well-designed, prospective clinical studies with adequate sample size are needed to evaluate the correlation between serum Vitamin D level and mortality in critically ill patients.
AUTHORS’ CONTRIBUTION
Alizadeh N: Data gathering and preparation of the article draft. Khalili H: Designing the study, data analysis and final proof of the article. Mohammadi M: Patients’ selection and clinical assessment of the patients. Abdollahi A: laboratory measurements.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This study was the result of a Ph.D. student's thesis and supported by a Vice-Chancellor for the Research of Tehran University of Medical Sciences. The authors expressed sincere gratitude to all the nursing staff of the general ICU of Imam Khomeini Hospital for their kindly support.
REFERENCES
- 1.Holick MF, Chen TC. Vitamin D deficiency: A worldwide problem with health consequences. Am J Clin Nutr. 2008;87:1080S–6S. doi: 10.1093/ajcn/87.4.1080S. [DOI] [PubMed] [Google Scholar]
- 2.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 3.Deluca HF, Cantorna MT. Vitamin D: Its role and uses in immunology. FASEB J. 2001;15:2579–85. doi: 10.1096/fj.01-0433rev. [DOI] [PubMed] [Google Scholar]
- 4.Gysemans CA, Cardozo AK, Callewaert H, Giulietti A, Hulshagen L, Bouillon R, et al. 1,25-Dihydroxyvitamin D3 modulates expression of chemokines and cytokines in pancreatic islets: Implications for prevention of diabetes in nonobese diabetic mice. Endocrinology. 2005;146:1956–64. doi: 10.1210/en.2004-1322. [DOI] [PubMed] [Google Scholar]
- 5.Liu PT, Stenger S, Tang DH, Modlin RL. Cutting edge: Vitamin D-mediated human antimicrobial activity against Mycobacterium tuberculosis is dependent on the induction of cathelicidin. J Immunol. 2007;179:2060–3. doi: 10.4049/jimmunol.179.4.2060. [DOI] [PubMed] [Google Scholar]
- 6.Higgins DM, Wischmeyer PE, Queensland KM, Sillau SH, Sufit AJ, Heyland DK. Relationship of vitamin D deficiency to clinical outcomes in critically ill patients. JPEN J Parenter Enteral Nutr. 2012;36:713–20. doi: 10.1177/0148607112444449. [DOI] [PubMed] [Google Scholar]
- 7.Lee P, Eisman JA, Center JR. Vitamin D deficiency in critically ill patients. N Engl J Med. 2009;360:1912–4. doi: 10.1056/NEJMc0809996. [DOI] [PubMed] [Google Scholar]
- 8.Matthews LR, Ahmed Y, Wilson KL, Griggs DD, Danner OK. Worsening severity of Vitamin D deficiency is associated with increased length of stay, surgical intensive care unit cost, and mortality rate in surgical intensive care unit patients. Am J Surg. 2012;204:37–43. doi: 10.1016/j.amjsurg.2011.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mata-Granados JM, Vargas-Vasserot J, Ferreiro-Vera C, Luque de Castro MD, Pavón RG, Quesada Gómez JM. Evaluation of Vitamin D endocrine system (VDES) status and response to treatment of patients in intensive care units (ICUs) using an on-line SPE-LC-MS/MS method. J Steroid Biochem Mol Biol. 2010;121:452–5. doi: 10.1016/j.jsbmb.2010.03.078. [DOI] [PubMed] [Google Scholar]
- 10.Braun A, Chang D, Mahadevappa K, Gibbons FK, Liu Y, Giovannucci E, et al. Association of low serum 25-hydroxyvitamin D levels and mortality in the critically ill. Crit Care Med. 2011;39:671–7. doi: 10.1097/CCM.0b013e318206ccdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Braun AB, Litonjua AA, Moromizato T, Gibbons FK, Giovannucci E, Christopher KB. Association of low serum 25-hydroxyvitamin D levels and acute kidney injury in the critically ill. Crit Care Med. 2012;40:3170–9. doi: 10.1097/CCM.0b013e318260c928. [DOI] [PubMed] [Google Scholar]
- 12.Arnson Y, Gringauz I, Itzhaky D, Amital H. Vitamin D deficiency is associated with poor outcomes and increased mortality in severely ill patients. QJM. 2012;105:633–9. doi: 10.1093/qjmed/hcs014. [DOI] [PubMed] [Google Scholar]
- 13.Amrein K, Zajic P, Schnedl C, Waltensdorfer A, Fruhwald S, Holl A, et al. Vitamin D status and its association with season, hospital and sepsis mortality in critical illness. Crit Care. 2014;18:R47. doi: 10.1186/cc13790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aygencel G, Turkoglu M, Tuncel AF, Candir BA, Bildaci YD, Pasaoglu H. Is Vitamin D insufficiency associated with mortality of critically ill patients? Crit Care Res Pract. 2013;2013:856747. doi: 10.1155/2013/856747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Venkatram S, Chilimuri S, Adrish M, Salako A, Patel M, Diaz-Fuentes G. Vitamin D deficiency is associated with mortality in the medical intensive care unit. Crit Care. 2011;15:R292. doi: 10.1186/cc10585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Turan A, Hesler BD, You J, Saager L, Grady M, Komatsu R, et al. The association of serum Vitamin D concentration with serious complications after noncardiac surgery. Anesth Analg. 2014;119:603–12. doi: 10.1213/ANE.0000000000000096. [DOI] [PubMed] [Google Scholar]
- 17.Flynn L, Zimmerman LH, McNorton K, Dolman M, Tyburski J, Baylor A, et al. Effects of Vitamin D deficiency in critically ill surgical patients. Am J Surg. 2012;203:379–82. doi: 10.1016/j.amjsurg.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 18.Garland CF, Kim JJ, Mohr SB, Gorham ED, Grant WB, Giovannucci EL, et al. Meta-analysis of all-cause mortality according to serum 25-hydroxyvitamin D. Am J Public Health. 2014;104:e43–50. doi: 10.2105/AJPH.2014.302034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 report on dietary reference intakes for calcium and Vitamin D from the Institute of Medicine: What clinicians need to know. J Clin Endocrinol Metab. 2011;96:53–8. doi: 10.1210/jc.2010-2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holick MF. Vitamin D: A millenium perspective. J Cell Biochem. 2003;88:296–307. doi: 10.1002/jcb.10338. [DOI] [PubMed] [Google Scholar]
- 21.Leow L, Simpson T, Cursons R, Karalus N, Hancox RJ. Vitamin D, innate immunity and outcomes in community acquired pneumonia. Respirology. 2011;16:611–6. doi: 10.1111/j.1440-1843.2011.01924.x. [DOI] [PubMed] [Google Scholar]
- 22.Annweiler C, Pochic S, Fantino B, Legrand E, Bataille R, Montero-Odasso M, et al. Serum Vitamin D concentration and short-term mortality among geriatric inpatients in acute care settings. Adv Ther. 2010;27:245–9. doi: 10.1007/s12325-010-0025-6. [DOI] [PubMed] [Google Scholar]
- 23.Venkatesh B, Davidson B, Robinson K, Pascoe R, Appleton C, Jones M. Do random estimations of Vitamin D3 and parathyroid hormone reflect the 24-h profile in the critically ill? Intensive Care Med. 2012;38:177–9. doi: 10.1007/s00134-011-2415-x. [DOI] [PubMed] [Google Scholar]
- 24.Reid D, Toole BJ, Knox S, Talwar D, Harten J, O’Reilly DS, et al. The relation between acute changes in the systemic inflammatory response and plasma 25-hydroxyvitamin D concentrations after elective knee arthroplasty. Am J Clin Nutr. 2011;93:1006–11. doi: 10.3945/ajcn.110.008490. [DOI] [PubMed] [Google Scholar]
- 25.Ginde AA, Mansbach JM, Camargo CA., Jr Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2009;169:384–90. doi: 10.1001/archinternmed.2008.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghashut RA, Talwar D, Kinsella J, Duncan A, McMillan DC. The effect of the systemic inflammatory response on plasma vitamin 25 (OH) D concentrations adjusted for albumin. PLoS One. 2014;9:e92614. doi: 10.1371/journal.pone.0092614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kempker JA, Han JE, Tangpricha V, Ziegler TR, Martin GS. Vitamin D and sepsis: An emerging relationship. Dermatoendocrinol. 2012;4:101–8. doi: 10.4161/derm.19859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heshmat R, Mohammad K, Majdzadeh SR, Forouzanfar MH, Bahrami A, Ranjbar Omrani GH, et al. Vitamin D deficiency in Iran: A multi-center study among different urban areas. Iran J Public Health. 2008;1:72–8. [Google Scholar]
- 29.Lips P. Vitamin D status and nutrition in Europe and Asia. J Steroid Biochem Mol Biol. 2007;103:620–5. doi: 10.1016/j.jsbmb.2006.12.076. [DOI] [PubMed] [Google Scholar]
- 30.Moradzadeh K, Larijani B, Keshtkar A, Hossein-Nezhad A, Rajabian R, Nabipour I, et al. Normative values of Vitamin D among Iranian population: A population based study. Int J Osteoporos Metab Disord. 2008;1:8–15. [Google Scholar]
- 31.Zittermann A, Kuhn J, Dreier J, Knabbe C, Gummert JF, Börgermann J. Vitamin D status and the risk of major adverse cardiac and cerebrovascular events in cardiac surgery. Eur Heart J. 2013;34:1358–64. doi: 10.1093/eurheartj/ehs468. [DOI] [PubMed] [Google Scholar]
- 32.McKinney JD, Bailey BA, Garrett LH, Peiris P, Manning T, Peiris AN. Relationship between Vitamin D status and ICU outcomes in veterans. J Am Med Dir Assoc. 2011;12:208–11. doi: 10.1016/j.jamda.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Lucidarme O, Messai E, Mazzoni T, Arcade M, du Cheyron D. Incidence and risk factors of Vitamin D deficiency in critically ill patients: Results from a prospective observational study. Intensive Care Med. 2010;36:1609–11. doi: 10.1007/s00134-010-1875-8. [DOI] [PubMed] [Google Scholar]
- 34.Zhang YP, Wan YD, Sun TW, Kan QC, Wang Lx. Association between Vitamin D deficiency and mortality in critically ill adult patients: A meta-analysis of cohort studies. Crit Care. 2014;18:684. doi: 10.1186/s13054-014-0684-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ralph R, Peter JV, Chrispal A, Zachariah A, Dian J, Sebastian T, et al. Supraphysiological 25-hydroxy Vitamin D3 level at admission is associated with illness severity and mortality in critically ill patients. J Bone Miner Metab. 2015;33:239–43. doi: 10.1007/s00774-014-0585-7. [DOI] [PubMed] [Google Scholar]
- 36.Sempos CT, Durazo-Arvizu RA, Dawson-Hughes B, Yetley EA, Looker AC, Schleicher RL, et al. Is there a reverse J-shaped association between 25-hydroxyvitamin D and all-cause mortality. Results from the U.S. nationally representative NHANES. J Clin Endocrinol Metab. 2013;98:3001–9. doi: 10.1210/jc.2013-1333. [DOI] [PMC free article] [PubMed] [Google Scholar]


