Abstract
Background:
Facial aging is characterized by skin changes, sagging and volume loss. Volume is frequently addressed with reabsorbable fillers like hyaluronic acid gels.
Materials and Methods:
From an anatomical point of view, the deep and superficial fat compartments evolve differently with aging in a rather predictable manner. Volume can therefore be restored following a technique based on restoring first the deep volumes and there after the superficial volumes. We called this strategy “dual plane”. A series of 147 consecutive patients have been treated with fillers using the dual plane technique in the last five years.
Results:
An average of 4.25 session per patient has been carried out for a total of 625 treatment sessions. The average total amount of products used has been 12 ml per patient with an average amount per session of 3.75 ml. We had few and limited adverse events with this technique.
Conclusion:
The dual plane technique is an injection technique based on anatomical logics. Different types of products can be used according to the plane of injection and their rheology in order to obtain a natural result and few side effects.
KEYWORDS: Dual plane, fat compartment, filler
INTRODUCTION
Aging of the face is characterized by different phenomena happening at more or less the same time: Variable skin atrophic changes and wrinkle formation caused by genetic, actinic, and environmental factors; bone volume and facial fat loss; and skin sagging. These issues can be addressed both surgically and nonsurgically, with nonsurgical cosmetic medicine being exponentially more popular than surgical intervention.[1]
From an etiologic point of view, volume loss takes place mostly in the bony skeleton and fat compartments with predictable patterns.[2,3] The most common nonsurgical tools for volume correction are fillers, the main players of which are represented by hyaluronic acid gels; however, other fillers are on the market too. The concept of filling, blended with other nonsurgical techniques and based on surgical logics, allows the physician to get optimal results with minimal downtime and good longevity.[4]
In the past, fillers were used for surface treatments with a dermatologic approach and short-lived results. Today, fillers are no longer used to address wrinkles but mostly to restore volumes and as a matter of fact, the level of their injection is the deep planes and not the skin; their strategy of injection is based on surgical concepts and maintanance of results is the rule. This has been possible after the introduction of hyaluronic acid gels in the market at the end of the last century[5] and their use as volumizers in analogy with fat grafting. Restoring volume helps, to a certain point, to limit the impact of sagging and can have a lifting effect. We have been using fillers as volume enhancers for the last 10 years, with slight modifications of the injection technique according to the evolution of anatomical knowledge and the basic science of filler rheology, and report our experience here.
MATERIALS AND METHODS
In the last 5 years, we adopted a technique for the use of fillers based on surgical anatomy that allows good efficacy, limited use of materials, and optimal longevity. Since two separate layers of subcutaneous tissues are injected, we call the method “dual plane technique.”
Surgical anatomy of aging relevant for fillers
The face consists of several layers and hence, we can consider it to be similar to an onion [Figure 1].
Figure 1.
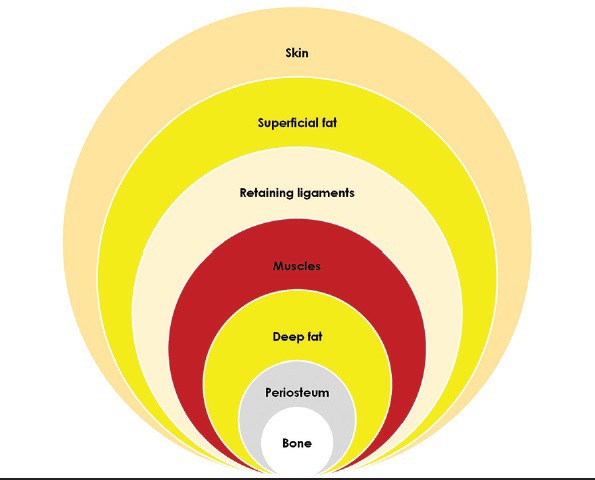
Onion-like layers of the face
With aging, the bony layer undergoes a reabsorption of the skeleton, mostly in the orbital, periorbital, malar, submalar, and mandibular areas.[2,6]
The fat compartments follow a rather predictable pattern of depletion. In the deep supraperiosteal layer, most of the volume loss takes place in the lateral and medial suborbicularis oculi fat, the deep medial cheek compartment, and the chin fat compartments. In the superficial subcutaneous layer, most of the volume loss takes place in the lateral compartments, both in their temporal and preauricular districts and to a lesser extent, in the middle and medial fat compartments of the superficial cheek fat pad.[3,7] It is remarkable that both the superficial nasolabial compartment and the superior and inferior jowl compartments are not greatly affected by volume loss and tend to move medially due to lack of lateral support caused by volume depletion in the lateral fat areas and lack of fibrous fixation points[8] [Figure 2].
Figure 2.
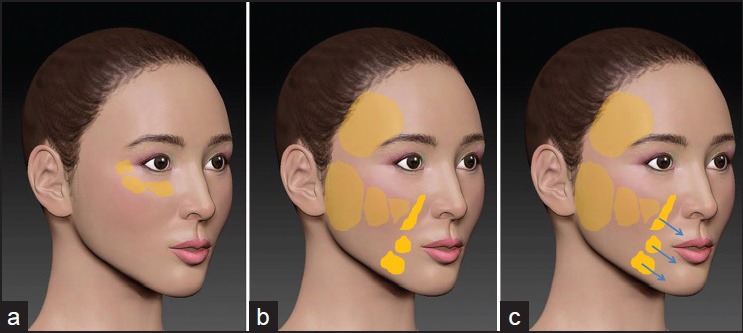
(a) Deep fat compartments of the midface (b) Superficial fat compartments of the midface (c) Sliding of the central, nonreabsorbing, superficial fat compartments
All the areas of fat reabsorption are confined in between the ligaments,[3,4] so that on the surface of the skin, several grooves become identifiable with the volume deflation: The tear trough and the palpebro-malar groove (tear trough ligament and orbital retaining ligaments), the midcheek groove (zygomatico-cutaneous ligament), the nasolabial fold (nasolabial ligament), the buccal fat groove (parotidomasseteric ligament), and the marionette line (labiomandibular ligament) [Figure 3].[4,7,9] All these ligaments tend to keep their strength in the central area of the face where a strong fixation exists, and become looser laterally.
Figure 3.

Ligaments of the face
Anatomic strategy of filler injection (dual plane technique)
Since bone and fat aging progress in a rather predictable fashion, the goal of restoring volumes in the face should follow a quite standardized sequence, useful in targeting the different areas of evolving atrophy, in order to achieve a full face volumetric rejuvenation in multiple sessions.
The areas of injection are selected precisely according to the anatomy and the strategy is based first on deep injections to the periosteal layer, and later on superficial injections in the superficial subcutaneous fat in a dual plane technique. The whole treatment usually requires three to five monthly sessions.
Soft tissue fillers are characterized by their rheological properties. The most relevant factors to consider are the viscoelasticity and cohesivity of the material.[10]
Viscoelasticity describes the hardness or softness of a gel and is defined by its elasticity (elastic modulus, G’), that is, how the filler is able to retain its shape when a force is applied and its viscosity (viscous modulus, G”), that is, how the filler resists gradual deformaton by shear stress. Their cumulated values identify the viscoelasic modulus (G*). The higher the G*, the higher the resistance to deformation and the capacity to keep its shape and hence, a major lifting effect.[11]
Cohesivity describes the property of the gel to stick together when an external force is applied. Gels with higher cohesivity tend to uniformly infiltrate the tissues and are not fractionated by movements.[11]
The deep malar plane is injected with hyaluronic acid gels with a high G* that are capable of an important lifting effect in order to get the maximum anterior projection with a limited amount of gel. The compartments injected are the lateral suborbicularis oculi fat, the medial suborbicularis oculi fat, and the deep medial cheek fat in this precise sequence. The area is marked [Figure 4] and each compartment is then injected with a 29 G or 27 G 25 mm long needle: Quite a long needle is needed in order to get to the bone where small boluses are deposited in each compartment. An average of 0.3/0.4 mL of gel is released in each compartment in 2/3 separate deposits. No more than 0.1-0.2 mL is released per bolus to avoid the risk of compression over lymphatic vessels. By this way of injecting, vertical pillars are created over the bone in order to support and lift the malar area [Figure 5]. The lateral to medial sequence of injection helps in achieving a tenting effect so that less material is needed in the more medial compartment. Augmentation of the deep medial cheek fat increases the anterior projection not completely addressed by lateral redraping, reduces the nasolabial fold, and recreates a youthful cheek within its natural boundaries [Figure 6].
Figure 4.

Markings
Figure 5.

Deep plane pillars: Several boluses per compartment
Figure 6.

Anterior malar projection
The deep orbital plane is equally injected with high G* gels, as deep as possible, directly on the periosteum or even infraperiosteally. In this case, a 25 G 40 mm long microcannula is used in order to prevent bleeding and as a tool to partially undermine the ligamentous areas of the orbital retaining ligaments. Two access points are chosen: The first one is located lateral to the lateral canthus of the eye in the area of the lateral orbital thickening and the cannula is moved inferomedially to target the area of the palpebromalar groove; the second one is located inferiorly to the zygomaticocutaneous ligament and the cannula is directed superomedially, cephalad to the tear trough ligament to target the tear trough. The average amount of gel released is 0.3/0.4 mL in the palpebromalar groove and 0.1/0.2 mL in the tear trough. In both areas, the gel is released in small aliquots and not in a continuous fashion in order to avoid the “sausage” effect of too much filling [Figure 7].
Figure 7.

Periorbital filling
The mandibular plane is also a deep plane of injection and is treated on the periosteum with a series of vertical boluses with a 29 G or 27 G 25 mm long needle along the inferior border of the mandibular bone. The area of the jowl is marked, avoided, and not injected between the masseteric ligament, where the facial vessels pass, and the mandibular ligament. The chin is also injected in the deep plane, directly to the bone with vertical pillars in the same fashion. Even in these areas, a strong gel with a high G* is used in order to obtain the maximum vertical expansion of the tissue and little or no lateral spread of the material.
Once the deep areas are injected, we move to treat the superficial subcutaneous plane. This is often done in a second session, usually spaced about 25-45 days from the first one. The treatment of the superficial fatty layer is directed only to those compartments that lose volume consistently, provoking the medial displacement of other compartments.
The temporal area is injected superficially under the skin in the subcutaneous tissue overlying the temporoparietalis fascia with a 25 G 40 mm long microcannula. The port of insertion of the cannula is created anteriorly to the hairline, by careful palpation to avoid the superficial temporal artery. Then the cannula is cautiously inserted underneath in a plane parallel to the skin and slowly moved to and fro in fan-like movements to deposit the gel in the subcutaneous layer in the region delimited cephalad by the temporal fusion line and caudad by the zygomatic arch. Working superficially with a cannula in this area prevents damage to the numerous vessels in the area and to the temporal branch of the facial nerve located under the fascia. For this region, cohesive gels with moderate G’ and G” are used in order to have good spreading of the material throughout the compartment, with a filling effect potentially improvable with a delicate massage. The end point of the treatment is the elimination of the concavity of the area that usually develops with aging and the achievement of a uniform or even slightly convex contour between the temporal fusion line and the zygomatic arch [Figure 8].
Figure 8.

Temporal area filling
The lateral compartment of the superficial cheek fat pad is hence, treated following a superficial pattern of injection similar to that used for the temple. The preauricular area is very often the superficial compartment where most of the volume loss takes place and needs to be addressed systematically to recreate the oval contour of the face. In this sector, a 25 g 40 mm or 50 mm long cannula is used and the point of entry is located anteriorly to the tragus just below the zygomatic arch. Through this access point, the filler material is deposited in the subcutaneous layer parallel to the plane of the skin with fan shape movements to reach inferiorly the mandibular angle and anteriorly the parotidocutaneous ligament that separates the lateral and the middle compartments of the superficial cheek fat pad. Sometimes, a second access point is needed anteriorly to the earlobe in order to completely crisscross this quite extensive anatomic region. In this area, both volumizing and tightening effects are desirable and the choice of material will be a cohesive gel with both high G’ and G” [Figure 9].
Figure 9.

Cheek tightening after filling the superficial lateral and medial compartments
The middle compartment of the superficial cheek fat pad is located medially to the parotidocutaneous ligament and is the next compartment to be injected. Again, the plane of injection is superficial; in the subcutaneous layer and the port, the 25 G 40 mm microcannula is chosen medial to the parotidocutaneous ligament in the upper lateral area of the compartment. Then the cannula is directed inferomedially in the same fan-shape mode to evenly deliver the filler in the compartment. This compartment does not always need to be addressed since fiilling the preauricular area often moves it backward, achieving a vector directed upward and posteriorly. For this region, cohesive gels with moderate G’ and G" are used in order to spread evenly in the subcutaneous tissue and not be heavy on the skin of the area.
The medial compartment of the superficial cheek fat pad is not always injected since the tenting effect obtained with the treatment of the lateral and middle compartments is often sufficient to improve the whole area. In case of injection, our access point of choice is located distally near the corner of the mouth, just lateral to the nasolabial fat compartment and the 25 G 40 mm microcannula is directed upward to fill this small area. In this area, a cohesive, softer gel with moderate G’ and G" is used in a little amount.
The nasolabial fold is injected infrequently and mostly in its cephalad area where a deep space called Ristow's space[12] can be filled with high G* gels, as deep as possible, in order to avoid any risk of touching the facial artery. The caudad part of the fold is mostly dynamic and is treated only in those patients where an important skin impression exists. This area is treated in the superficial subcutaneous tissue with the traditional 30 G needle technique or with a 25 G microcannula.
The superficial chin compartment is injected with a 25 G 40 mm long microcannula from the mandibular ligament toward the midline. This compartment needs a little augmentation too, just sufficient to tighten the area and reduce the labiomental fold.
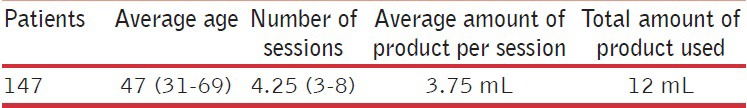
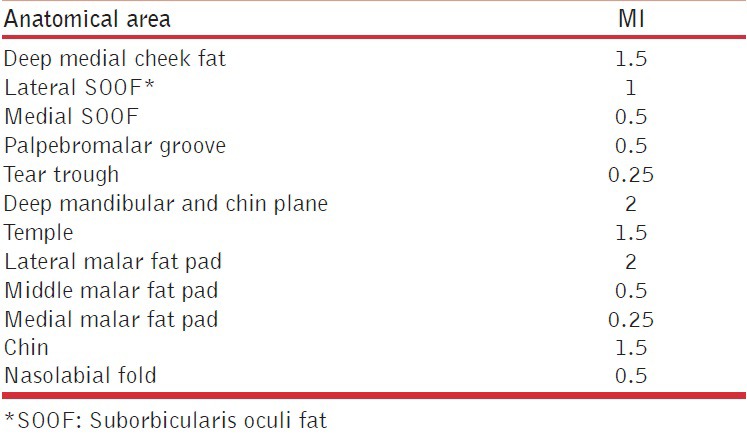
In this paper, we present a reiew of 147 consecutive patients (146 Caucasians, 1 Chinese) who underwent a “full face” treatment with volumetric fillers in the last 5 years with the dual plane technique described above [Table 1].
Table 1.
Demography
RESULTS
All patients completed at least three sessions of treatment, with an average of 4.25 sessions per patient and a maximum of 8 sessions (one patient). The sessions were spaced at 4 weeks (minimum 3 weeks, maximum 8 weeks) for a total of 625 treatment sessions. Hyaluronic acid gel was the standard filler used in the series; six patients were treated with polycaprolactone gel. The average of the total amount of product used was 12 mL per patient with an average amount per session of 3.75 mL. The average amount per anatomic area per side is detailed in Table 2.
Table 2.
Average amount per anatomical area per side
The most common side effects of the treatment were represented by swelling and bruises. Swelling is generally expected after filler injections, especially when a hyaluronic acid gel, a naturally water-attracting material, is used. All patients were instructed to drink a lot of water for 3-4 days after the treatment and to sleep in a supine position with the head upward in order to reduce water attraction around the implanted material. All patients treated in the malar and orbital area in the last 3 years were prescribed betametasone 1 mg for 2/3 days to prevent periocular swelling. Bruises are not common when injecting with an anatomical strategy since most of the vessels are in areas that are not injected; furthermore, the use of microcannulas makes the injection less traumatic for the tissues. Nevertheless, bruises were seen in 117 occasions out of 625 treatments (18.7%).
The majority of the patients in this series (124) are regularly seen for follow-up treatment once or twice in 1 year [Figure 10]. The majority of them also received synergistic treatments (121 botulinum toxin therapy, 77 retinoid-based home skin care, 43 suspension threads, and 13 fractionated CO2 laser resurfacing).
Figure 10.

Before and after
We had seven (4.8%) patients with two types of adverse effects, inflammatory reaction and nodule formation. Six patients had an unspecific inflammatory reaction at a variable distance from the injection sessions during the course of the treatment plan. All reactions resolved spontaneously or as in two cases, after a short course of sistemic steroids. Four of these patients later developed small nodular reactions in the deep tissues. One patient developed a nodular reaction without a preliminary inflammation. In two cases, hyaluronidase (Jaluronidasi, 300 UI/3 mL vials, Farmindustria, Novi Ligure, Alessandria, Italy) was succesfully used to dissolve the nodules;[13] all other cases resolved on their own with time.
DISCUSSION
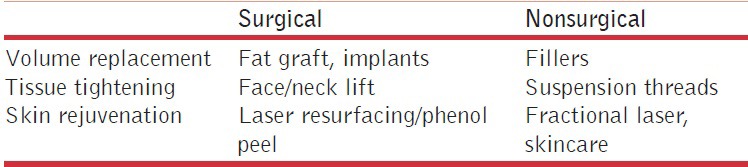
With drastic increase in the popularity of nonsurgical techniques, it is very important to approach patients seeking enhancement and/or rejuvenation with a soft modality respectful of their anatomy and age. Physicians must be guided by the safety for the patient and by an aesthetic approach respectful of proportions. A modern full face management, both surgical and nonsurgical, is based on volume replacement, tissue tightening, and skin rejuvenation. Volume is just one aspect of a full face approach[4] and it is necessary that physicians educate patients to understand the strategy of treatment [Table 3]. Aging is not a disease but the treatment of aging requires a precise evaluation and diagnosis. A thorough discussion should precede the signing of consent forms and documentation photos.
Table 3.
Strategies of treatment
Resorbable fillers comply with almost all cosmetic patients’ needs and guarantee an immediate and long-time safety but often need to be used in several sessions due to a progressive strategy from the deep planes to the surface and so as to not create evident modifications to avoid too much swelling and bruising and to reduce the cost per session for the patient. Hyaluronic acid gels are the most widely used soft tissue fillers for volume replacement.
From a rheologic point of view, gels with high G’ have more important lifting effect[10] and are more indicated in boluses over the supraperiosteal layer where they act as “pillars” to lift and support the tissues; on the other hand, gels with moderate G’ and G” are more indicated to treat the subcutaneous tissue where they act like “bridges” to reconnect the pillars, thanks to their expander capacity. Often, injecting the deep plane is sufficient to have good results in terms of natural volume and projection of tissues while the superficial plane allows for more tightening than volume, especially in the lateral/temporal compartment.
Most of the volume is obtained from injecting the deep plane and particularly the bony layer where trauma and deposition of the gel on the periosteum are able to activate the periosteal stem cells[14] with new tissue formation and almost a permanent effect [Figure 11]. Reaching the bony layer is faster and easier with a needle, a very precise tool that gives the physiscian perfect control of the release of the gel: With an accurate anatomical study of the patient and a preoperative marking, needle injections target only the bony layer of the deep fat compartments avoiding all the septa where the vessels lie, allowing injections without bleeding. In the deep periocular areas at the risk of cannulating vessels, the use of microcannula is safer and is recommended, particularly at the inner canthus of the eye where the angular artery and vein are quite superficial.
Figure 11.

Orbital filling, before treatment and on 5 years follow-up
Injecting the deep layers over the periosteum also carries the advantage of having the bulk of the correction under the muscles, avoiding the grotesque effect of too much moving volume during animation when most of the volume is placed in the skin or in the subcutaneous layer.
The superficial subcutaneous layer is mostly important in the lateral compartments where it contributes to the contour and the general shape of the face. Blending the temporal area with the preauricular area gives a nice contouring effect from the temporal fusion line to the mandibular corner, through the temporal area, zygoma, and posterior cheek. The definition of the lateral profile of the face improves the general effect of the treatment and reduces the “rat face” effect of those patients treated only in the central areas of the face and the lips. The temporal and preauricular compartments often need only a tightening effect that is commonly achieved with cohesive gels with a moderate G*. In the temple, the need for volume is really very limited and gels can be usefully diluted in order to get a better spreadability in the region.[15,16] The end point of the treatment in this area, in our opinion, is a slight convexity joining the temporal fusion line with the zygomatic arch. In the preauricular area, there is usually a more important need for volume so that in this region dilution is less convenient: An optimal deposition of the material sometimes requires two ports of entry, one in the pretragal area and the other located caudally in front of the earlobe.
The dual plane technique is based on the anatomy of the deep and superficial fat pads; hence, each single compartment should be injected separately since there is no spread of the filler from one compartment to the other due to the fibrous septa separating the fat pads. Each compartment requires a separate entry point in order to avoid the septa independently from the use of needle or microcannula. After the injections to the deep plane, no massage is needed and indeed it is useful not to touch the gel to avoid loosening its capacity of projection. In the subcutaneous plane, on the contrary, a moderate massage can help in spreading the gel laterally to improve its capacity of expansion. By filling the anatomical compartments, the major grooves of the face are treated indirectly since folds occur at transition points between compartments. On the contrary, injecting along the superficial compartment boudaries carries more risk of vascular damage. The nasolabial fold, for instance, is treated only in its nondynamic part.
Planning a full face volumization with fillers requires a double vision: To be able to see three-dimensionally the areas of volume loss and show them to the patient, and to be able to see the end result before starting. A three-dimensional remodeling through soft tissue augmentation give the face a fuller and younger aspect: A moderate volume enhancement eliminates folds, improve wrinkles, and meet the patient's expectations. Every area of injection should be treated moderately in order to give the face a good impact and not make it look “done.” The dual plane technique is a multistep treatment: First, the deep volumes (malar, orbital, chin, and jawline) are restored, then the superficial volumes (temple, lateral, middle, and medial malar fat pad and full face soft contouring) are addressed, and finally the wrinkles are treated, if there are any left and the quality of the skin is addressed. The first correction is further improved by subsequent touch up treatments and retreating a fully corrected patient requires fewer products to keep the aesthetic results.
This modality of injection allows minimal side effects. The adverse events we recorded depend, in our opinion, more on the characteristics of the gels than on the technique of injection; in fact, strong gels are usually more reticulated and this can induce a more important reactivity in the tissues, with inflammation and sometimes capsulation of the gel. This augmented reactivity also explains the increased stimulation in the tissue leading to new tissue formation and semi-permanent augmentation.[14] The multiple release of small boluses over the bone also helps in avoiding edema in the malar area.[17] Once the desired volumization is reached, maintenance of the results can be done by one session a year and this helps patients to bear the initial cost of the treatment. The adjuvant effect of other noninvasive cosmetic procedures is the ultimate strategy for aging naturally, with results that are always subtle and not noticeable. It also evident that mixed noninvasive treatment has less risk than a surgery and minimizes the recovery time. A continuum sequence of maintenance treatments requires a shift in thinking for patients and doctors too, from major procedures to maintenance protocols.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
- 1.Few JW. The beauty of blending: Surgical and nonsurgical synergy. [Last accessed on 15 Feb 2015]. Available from: http://www.plasticsurgerypulsenews.com/10 .
- 2.Shaw RB, Jr, Kahn DM. Aging of the midface bony elements: A three dimensional computed tomographic study. Plast Reconstr Surg. 2007;119:675–83. doi: 10.1097/01.prs.0000246596.79795.a8. [DOI] [PubMed] [Google Scholar]
- 3.Rohrich RJ, Pessa JE. The fat compartments of the face: Anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119:2219–31. doi: 10.1097/01.prs.0000265403.66886.54. [DOI] [PubMed] [Google Scholar]
- 4.Russo PR, Fundarò PS. Florence: OEO; 2014. The invisible lifting; pp. 109–57. [Google Scholar]
- 5.Duranti F, Salti G, Bovani B, Calandra M, Rosati ML. Injectable hyaluronic acid gel for soft tissue augmentation. A clinical and histologic study. Dermatol Surg. 1998;24:1317–25. doi: 10.1111/j.1524-4725.1998.tb00007.x. [DOI] [PubMed] [Google Scholar]
- 6.Mendelson B, Wong CH. Changes in the facial skeleton with aging: Implications and clinical applications in facial rejuvenation. Aesthetic Plast Surg. 2012;36:753–60. doi: 10.1007/s00266-012-9904-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sandoval SE, Cox JA, Koshy JC, Hatef DA, Hollier LH. Facial fat compartments: A guide for filler placement. Semin Plast Surg. 2009;23:283–7. doi: 10.1055/s-0029-1242181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ozdemir R, Kilinç H, Unlü RE, Uysal AC, Sensöz O, Baran CN. Anatomicohistologic study of the retaining ligaments of the face and use in face lift: Retaining ligament correction and SMAS plication. Plast Reconstr Surg. 2002;110:1134–49. doi: 10.1097/01.PRS.0000021442.30272.0E. [DOI] [PubMed] [Google Scholar]
- 9.Haddock NT, Saadeh PB, Boutros S, Thorne CH. The tear trough and lid-cheek junction: Anatomy and implications for surgical correction. Plast Reconstr Surg. 2009;123:1332–42. doi: 10.1097/PRS.0b013e31819f2b36. [DOI] [PubMed] [Google Scholar]
- 10.Sundaram H, Cassuto D. Byophisical characteristics of hyaluronic acid soft-tissue fillers and their relevance to aesthetic applications. Plast Reconstr Surg. 2013;132(Suppl 2):5–21s. doi: 10.1097/PRS.0b013e31829d1d40. [DOI] [PubMed] [Google Scholar]
- 11.Carruthers J, Carruthers A. 3rd ed. Philadelphia: Elsevier Saunders; 2013. Soft Tissue Augmentation: Procedures in Cosmetic Dermatology Series; pp. 91–4. [Google Scholar]
- 12.Rohrich RJ, Pessa JE, Ristow B. The youthful cheek and the deep medial compartment. Plast Reconstr Surg. 2008;121:2107–12. doi: 10.1097/PRS.0b013e31817123c6. [DOI] [PubMed] [Google Scholar]
- 13.Cavallini M, Gazzola R, Metalla M, Vaienti L. The role of hyaluronidase in the treatment of complications from hyaluronic acid dermal fillers. Aesthet Surg J. 2013;33:1167–74. doi: 10.1177/1090820X13511970. [DOI] [PubMed] [Google Scholar]
- 14.Mashiko T, Mori H, Kato H, Doi K, Kuno S, Kinoshita K, et al. Semipermant volumization by an absorbable filler: Onlay injection technique to the bone. Plast Reconstr Surg Glob Open. 2013;1:pii.e4–14. doi: 10.1097/GOX.0b013e31828c66b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lambros V. A technique for filling the temples with highly diluted hyaluronic acid: The “dilution solution”. Aesthet Surg J. 2011;31:89–94. doi: 10.1177/1090820X10391214. [DOI] [PubMed] [Google Scholar]
- 16.Fagien S, Cassuto D. Reconstituted injectable hyaluronic acid: Expanded applications in facial aesthetics and additional thoughts on the mechanism of action in cosmetic medicine. Plast Reconstr Surg. 2012;130:208–17. doi: 10.1097/PRS.0b013e318254b3f6. [DOI] [PubMed] [Google Scholar]
- 17.Funt DK. Avoiding malar edema during midface/cheek augmentation with dermal fillers. J Clin Aesthet Dermatol. 2011;4:32–6. [PMC free article] [PubMed] [Google Scholar]


