Abstract
The lips and the eyes enhance facial beauty, and they have been highlighted since time immemorial. Rejuvenating the lips with fillers, frequently hyaluronic acid (HA), is a common procedure but requires expertise. The objective of this text is to describe the procedure in detail and cover the practical aspects of injecting lips with fillers. An analysis of treating lips with needles and cannulae has been made with special emphasis on achieving optimum results.
KEYWORDS: Dermal fillers, hyaluronic acid (HA), lip rejuvenation, needles, canulae
INTRODUCTION
The lip region is an extremely important area when it comes to facial aesthetic enhancement. The lips have since time immemorial been highlighted along with the eyes as the two most beautiful regions of a woman's or a man's face.
With the passage of time, photodamage, hereditary factors, and smoking contribute to loss of lip volume, perioral rhytides, and prominence of mentolabial folds. Genetically thin lips and cosmetic asymmetries of the lips are also issues that can be dealt with similarly, that is, by soft tissue augmentations using fillers. Successful rejuvenation of the perioral region requires sophistication in using a combination of technologies and injectables.
Various fillers, temporary and permanent, have been tried in shaping the lips, with gratifying results. Disasters in the form of granulomas have been reported with both temporary and permanent fillers, more often with the latter.
Hyaluronic acid (HA) and polyacrylamide (PA) are the two main fillers widely available. HA is the predominant one, with PA being virtually out of the race because of fears of granuloma. Worldwide usage and published reports clearly confirm the efficacy and safety of HA fillers. They are one of the key components of successful combination treatments of the aging face and lips.[1]
Common commercial preparations of HA that are widely available include the Anteis range (Fortélis® and Esthélis®, Switzerland), Galderma range, USA (Restylane and Perlane), and the Allergan range, Irvine, CA 92612 (Juvéderm Ultra® and Juvéderm Ultra Plus®). Other brands such as Revanesse®, Prollenium Medical Technologies Inc., Canada and Amazing Fill® are also available.[2]
ANATOMY
The upper lip extends from the base of the nose superiorly to the nasolabial folds laterally and to the free edge of the vermilion border inferiorly. The lower lip extends from the superior free vermilion edge superiorly, to the commissures laterally, and to the mandible inferiorly. Around the circumferential vermilion/skin border, a fine line of pale skin accentuates the color difference between the vermilion and normal skin. Along the upper vermilion/skin border, two paramedian elevations of the vermilion form the Cupid's bow. Two raised vertical columns of tissue form a midline depression called the philtrum.
WHAT TO TREAT
A deflating vermilion (the red part) is the most common complaint, followed by drooping angles of the mouth. These two together complete the picture of a sorry face. Lips that have good volume can be highlighted by defining them and injecting into the white margins (the vermilion border) [Figure 1]. Pouts can be created by injecting the filler below the muscle [Figure 2]. Typically, the upper lip is treated more often than the lower. The best approach to lip augmentation depends on the nature of the defect and the subject's aesthetic desires. For genetically thin lips, structural augmentation with a deeper-placed filler followed by volume correction with a superficial filler is ideal. For pure cosmetic enhancement of lips, a superficially placed filler with emphasis on the white roll and expansion of the vermilion is ideal.[3]
Figure 1.
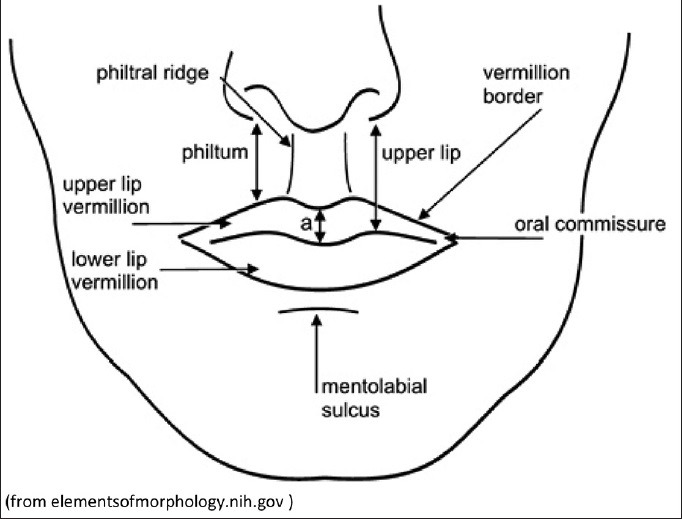
Lip: Anatomical landmarks (from elementsofmorphology.nih.gov)
Figure 2.
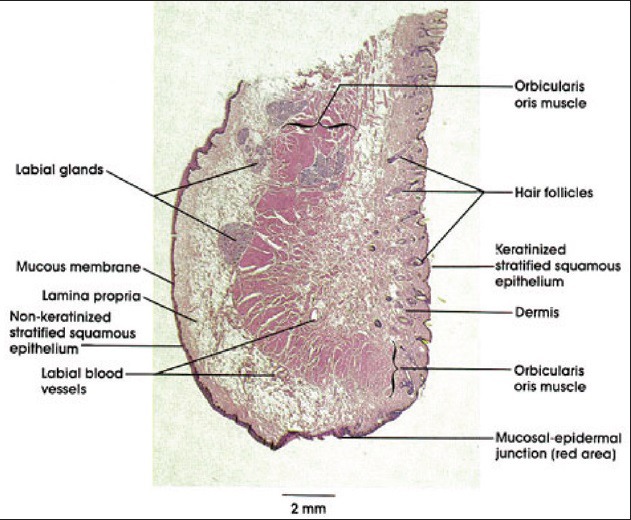
Histology of the lip in a section (from imargade.com)
Female lips are, on average, a little fuller than male lips. They bulge forward more than male lips – In other words, they are slightly more “pouty.” Female lips are not noticeably bigger when you see them from the front but they do bulge forward more as seen from the side. We need to keep this in mind while treating male and female lips. Overvolumization of the male lip can result in feminization of the area.
PATIENT SELECTION AND OUTCOMES
Careful patient selection, history, and a detailed consultation outlining the benefits, limitations, and adverse events of lip reshaping go a long way toward providing the desired results. Discussing the immediate aftermath of a lip augmentation, that is, swelling and bruising, is a key component to counselling as often patients tend to be secretive about these procedures and do not wish to disclose any treatment taken. The existence of downtime, varying from 2 days to 2 weeks, needs to be emphasized; the recent use of cannulae instead of needles has helped to reduce it. What the patient may desire may not be realistically possible and it is crucial to align them on what to expect [Box 1 and Figure 3].
Box 1. Patient alignment checklist.
Patient alignment checklist
Synchronization of patient and physician expectations
Information on immediate and late postprocedure outcomes
Number of syringes and cost
Longevity of product used
Repetitive and temporary nature of treatment
Adverse events
Postprocedure care
Figure 3.

Swelling of the lips immediately after HA injection with needles
History of herpes labialis, and aspirin and vitamin E usage needs careful consideration for a better outcome.
TREATMENT STRATEGY
Lip augmentation consists of the reshaping and/or enlargement of the visible portion of the lip, the vermilion. Alteration of the shape of the Cupid's bow and of the relationship between the vermilion and the skin underlying the nasal columella also falls within the category of lip augmentation.
It is also important to consider the relationship between lip height and incisor shown in the anatomic analysis, to evaluate possible maxillary hypoplasia and protrusion, and to consider the patient's occlusion status.
TREATMENT TECHNIQUES[3,4,5,6,7]
Anesthesia is first administered with either a eutectic mixture of lidocaine and prilocaine or regional blocks (infraorbital for the upper lip and mental for the lower lip). It is critical not to distort the shape of the lips. Using premixed HA with lidocaine as an add-on reduces the pain of the injection. Some patients may experience anxiety over the amount of swelling and bruising, and may require ice soaks, nonsteroidal anti-inflammatory drugs (NSAIDs; not in the first 6 h as that might mask any signs of vascular compromise), and even prednisolone.[3]
Medium-depth fillers such as Restylane®, Juvéderm Ultra®, and Esthélis Basic® are preferred, using either a 30-G needle or a 27-G cannula.
Expected postprocedure outcomes of lip augmentation include edema, bruising, and ecchymosis. Complications are extremely rare and include nodules and lumps, which can be massaged in or dissolved with hyaluronidase injections. Intravascular injections may result in immediate blanching, but the collateral circulation of the lips is highly forgiving. Warm compresses, use of hyaluronidase, and topical nitroglycerin help. Herpetic reactivation can be prevented with oral antivirals (acyclovir, famciclovir or valaciclovir) [Figure 4].
Figure 4.

Herpetic reactivation after fillers
The occurrence of adverse reactions relates to both the inherent properties of the product and inappropriate delivery or dilution of the filler, which may lead to harmful sequelae.[8,9,10,11]
Underscoring the need for product-specific training, uneven distribution of injected products, due to poor technique, can also lead to postinjection lumps and nodules.[12,13,14] This is of particular concern with more permanent products because the undesired results are also long-lasting. Overaggressive injection may lead to irregularity or lumpiness, whereas if the product is placed too superficially, beading can occur.[15,16]
Overcorrection is not indicated. Simultaneous vermilion and vermilion border augmentations result in a complete effect.
The techniques for injection of HA for lip augmentation have included serial puncture and linear threading, which may be antegrade or retrograde. The choice of one technique over another or a combination of techniques may be influenced by aesthetic goals and patient factors.
The use of cannulae has cut down the downtime involved in this procedure and increased the percentage of patients returning for repeat augmentations [Figure 5]. Only one point each on either side at the oral commissure is utilized to reach both the upper and the lower lip. This technique needs getting accustomed to and is difficult for a beginner. The author advises using needles initially but ultimately moving to a cannula–it pays off in the long run with better results and less downtime [Figures 6 and 7].
Figure 5.

Lip augmentation with a cannula
Figure 6.

Shaping of upper and lower lips with 1 mL of HA: Pre-treatment
Figure 7.

Shaping of upper and lower lips with 1 mL of HA: After treatment
CONCLUSION
Lip augmentation with the use of injectable fillers achieves quick results with minimal downtime. Significant ease of use, “off-the-shelf” availability, and widespread acceptance by the public make HA one of the most commonly used fillers. Lip augmentation with fillers can be performed by injecting the material in any or all of the anatomic parts of the lip, allowing for a very controlled and predictable result. Precautions regarding mode of injection and quantity of the substance injected vary widely with patient profiles. At times, budgetary constraints decide treatments, but that should be avoided, and patients need to be told about the optimum filler requirements.
Optimizing the aesthetic outcome of lip augmentation with dermal fillers, such as HA, requires skillful application of a suitable injection technique. Moreover, achieving aesthetic goals with minimal risk for adverse events requires knowledge of lip anatomy and function, clinical experience in the use of various injection techniques, and an individualized treatment approach.[6]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lupo PM. Hyaluronic acid fillers in facial rejuvenation. Semin Cutan Med Surg. 2006;25:122–6. doi: 10.1016/j.sder.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 2.Luthra A, Kumar V. Fillers and autologus fat. In: Khunger M, editor. Step by Step Treatment of Acne Scars. India: Jaypee Brothers; 2014. pp. 153–71. [Google Scholar]
- 3.Carruthers J, Narurkar VA. Management of the lips and mouth corners. In: Carruthers J, Carruthers A, editors. Soft Tissue Augmentation. Philadelphia: Saunders; 2006. pp. 109–19. [Google Scholar]
- 4.Godin MS, Majmundar MV, Chrzanowski DS, Dodson KM. Use of radiesse in combination with restylane for facial augmentation. Arch Facial Plast Surg. 2006;8:92–7. doi: 10.1001/archfaci.8.2.92. [DOI] [PubMed] [Google Scholar]
- 5.Kanchwala SK, Holloway L, Bucky LP. Reliable soft tissue augmentation: A clinical comparison of injectable soft-tissue fillers for facial-volume augmentation. Ann Plast Surg. 2005;55:30–5. doi: 10.1097/01.sap.0000168292.69753.73. [DOI] [PubMed] [Google Scholar]
- 6.Sclafani AP. Soft tissue fillers for management of the aging perioral complex. Facial Plast Surg. 2005;21:74–8. doi: 10.1055/s-2005-871766. [DOI] [PubMed] [Google Scholar]
- 7.Smith SR, Lin X, Shamban A. Small gel particle hyaluronic acid injection technique for lip augmentation. J Drugs Dermatol. 2013;12:764–9. [PubMed] [Google Scholar]
- 8.Lowe NJ. Temporary dermal fillers — European experiences. In: Lowe NJ, editor. Textbook of Facial Rejuvenation. London: Martin Dunitz/Taylor and Francis; 2002. pp. 177–88. [Google Scholar]
- 9.Klein AW. Collagen substances. (viii).Facial Plast Surg Clin North Am. 2001;9:205–18. [PubMed] [Google Scholar]
- 10.DeLustro F, Condell RA, Nguyen MA, McPherson JM. A comparative study of the biologic and immunologic response to medical devices derived from dermal collagen. J Biomed Mater Res. 1986;20:109–20. doi: 10.1002/jbm.820200110. [DOI] [PubMed] [Google Scholar]
- 11.DeLustro F, Smith TS, Sundsmo J, Salem G, Kincaid S, Ellingsworth L, et al. Reaction to injectable collagen in human subjects. J Dermatol Surg Oncol. 1998;14(Suppl 1):49. [Google Scholar]
- 12.Cotran RS, Kumar V, Robbins SL. 5th ed. Philadelphia: WB Saunders; 1994. Pathologic Basis of Disease; pp. 51–93. [Google Scholar]
- 13.Rudolph CM, Soyer HP, Sculler-Petrovic S, Kerl H. Foreign body granulomas due to injectable aesthetic microimplants. Am J Surg Pathol. 1999;23:113–7. doi: 10.1097/00000478-199901000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Duranti F, Salti G, Bivani B, Calandra M, Rosati ML. Injectable hyaluronic gel for soft tissue augmentation. A clinical and histological study. Dermatol Surg. 1998;24:1317–25. doi: 10.1111/j.1524-4725.1998.tb00007.x. [DOI] [PubMed] [Google Scholar]
- 15.Lemperle G, Romano JJ, Busso M. Soft tissue augmentation with Artecoll: 10-year history, indications, techniques, and complications. Dermatol Surg. 2003;29:573–87. doi: 10.1046/j.1524-4725.2003.29140.x. [DOI] [PubMed] [Google Scholar]
- 16.Mullins RJ, Richards C, Walker T. Allergic reactions to oral, surgical and topical bovine collagen. Anaphylactic risk for surgeons. Aust N Z J Ophthalmol. 1996;24:257–60. doi: 10.1111/j.1442-9071.1996.tb01589.x. [DOI] [PubMed] [Google Scholar]


