Abstract
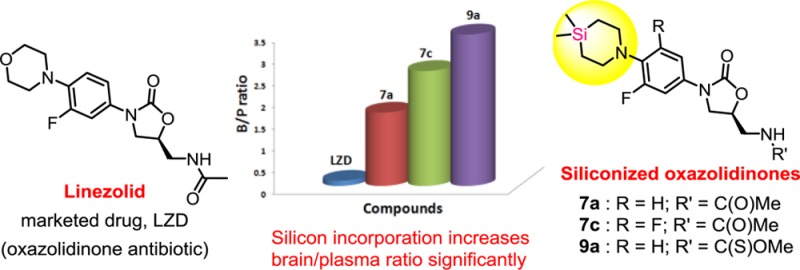
Therapeutic options for brain infections caused by pathogens with a reduced sensitivity to drugs are limited. Recent reports on the potential use of linezolid in treating brain infections prompted us to design novel compounds around this scaffold. Herein, we describe the design and synthesis of various oxazolidinone antibiotics with the incorporation of silicon. Our findings in preclinical species suggest that silicon incorporation is highly useful in improving brain exposures. Interestingly, three compounds from this series demonstrated up to a 30-fold higher brain/plasma ratio when compared to linezolid thereby indicating their therapeutic potential in brain associated disorders.
Keywords: Antibacterial, linezolid, oxazolidinone, brain exposure, sila analogue
Bacterial meningitis is a very severe condition with sudden onset of symptoms and death within hours. According to WHO statistics, bacterial meningitis affects more than 400 million people per year in the “African meningitis belt”. Of the 22 831 cases diagnosed in 2010 across 14 African countries, 2415 deaths were reported with a case-fatality ratio of 10.6%.1 The diagnosis is done by investigating the cerebrospinal fluid of patients obtained by a lumbar puncture. Since meningitis is fatal, wide spectrum antibiotics are given even before the disease is actually confirmed. The choice of antibiotics depends on the pathogen that causes meningitis, the most common ones being Streptococcus pneumoniae and Neisseria meningitidis. Cephalosporin, ampicillin, vancomycin, and rifampin are some of the commonly used antibiotics for treating bacterial meningitis.2 The central nervous system (CNS) is protected by the highly selective blood–brain barrier (BBB) that controls the entry of compounds into the brain. In a normal individual, the BBB efficiently protects the brain from pathogens that can easily cause infections in other parts of the body. While brain infections are not common, they can be difficult to treat in affected individuals due to the inability of drugs to cross the BBB. The BBB, therefore, makes drug delivery to the CNS a challenging task for medicinal chemists.3,4 In addition to permeability, development of resistance to existing antibiotics is yet another problem encountered in treatment of brain infections. Hence, a global demand and medical need exists to develop novel lipophilic antibiotics with better BBB penetration for treating brain infections.
Linezolid5,6 is the first oxazolidinone antibiotic to be marketed for clinical use that suppresses bacterial growth via inhibition of ribosomal protein synthesis. Linezolid binds to a site on the 50S ribosomal subunit near its interface with the 30S unit and thus prevents the formation of a 70S initiation complex.7 Linezolid’s broad spectrum of activity against virtually all Gram-positive bacteria, including methicillin resistant and vancomycin resistant bacteria, led to an increased usage of the drug and resulted in significant worldwide sales ever since its approval in 2000. However, only limited information has been established with respect to linezolid’s efficacy in treating infections of the central nervous system (CNS). The cerebrospinal fluid (CSF) penetration of linezolid, a limitation observed with other frontline antibiotics in the treatment of CNS infections, is relatively better. Although, it was not evaluated in a large number of patients suffering from CNS infections, positive clinical experience with linezolid was documented in the literature by a few groups.8,9 To increase the utility of linezolid in CNS infections, synthesis of novel compounds is necessary; in particular, by improving B/P ratios of drug concentrations. Sutezolid (PNU-100480)10 is another closely related molecule that falls in the oxazolidinone category and is currently in phase II clinical trials for the treatment of both drug resistant and sensitive tuberculosis. While oxazolidinone antibiotics are typically bacteriostatic, their clinical activity is governed by the clinical dose as well as the pharmacokinetics. Other bacteriostatic agents such as tetracycline and chloramphenicol also possess good CSF penetration and are used in the treatment of bacterial meningitis.11
Bioisosterism is one of the widely used methods for the efficient optimization of pharmacokinetic (PK) properties of a lead molecule.12−14 The incorporation of silicon into known drug scaffolds called the “silicon switch approach” has gained momentum in recent times.15−22 It is worth highlighting the efforts of Tacke’s group for their work on this interesting approach. In general, silicon analogues are more lipophilic than their carbon counterparts. Hence this strategy would be beneficial in CNS drug discovery wherein siliconized compounds could potentially display better blood–brain barrier (BBB) penetration. In our group, we are interested in synthesizing novel bioactive molecules with the incorporation of silicon.23 Along these lines, we have designed and synthesized silicon analogues of the oxazolidinone antibiotics linezolid/sutezolid. We reasoned that the incorporation of silicon instead of an oxygen atom or sulfur atom in the morpholine/thiomorpholine ring can lead to a more lipophilic molecule, which was further supported by simple clogP calculations (Figure 1).24,25 Since the morpholine/thiomorpholine ring is not essential for activity and is amenable to different sterics around this moiety while retaining potency, we anticipated that the newly designed compounds would show similar activity to that of the parent. The details of experimental results are disclosed herein.26
Figure 1.
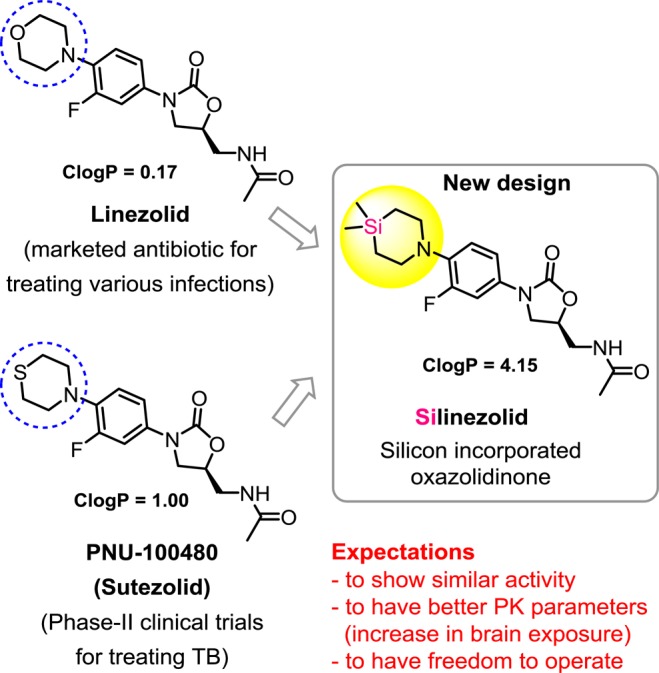
Design of silicon incorporated oxazolidinones.
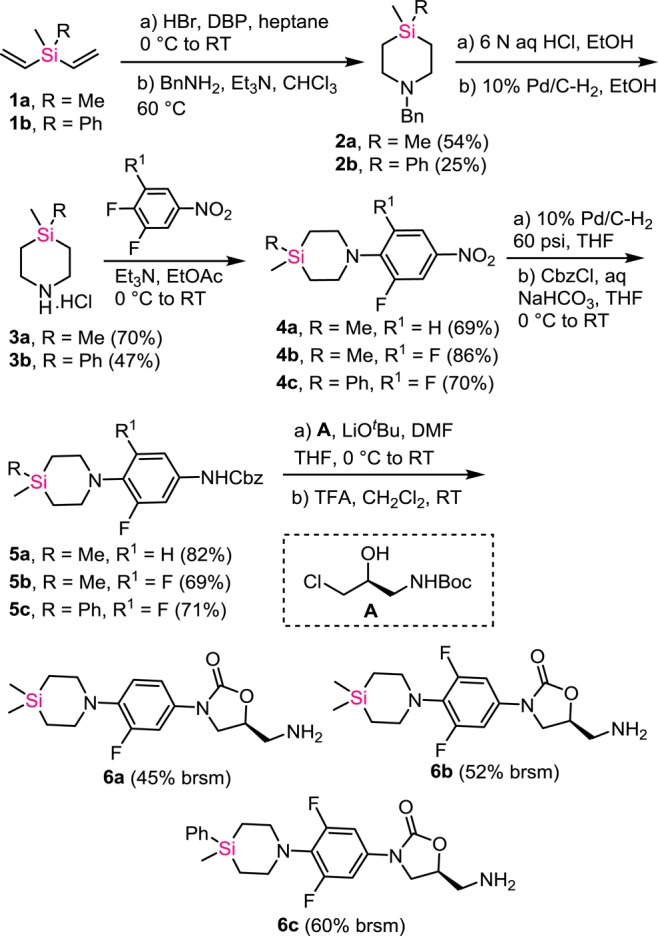
The chemical synthesis commenced with the preparation of 1,4-azasilinanes 3a(27) and 3b(28) from commercially available divinylsilanes 1a and 1b. The treatment of HBr gas to vinylsilanes in heptane in the presence of a catalytic amount of dibenzoyl peroxide (DBP) gave bis(bromoethyl)silanes, which on reaction with benzylamine in CHCl3 resulted in silapiperidines with benzyl protection 2a and 2b, respectively. The compounds 2a and 2b were debenzylated to give the key silapiperidines 3a and 3b. These important intermediates were synthesized on multigram scale, which helped us to generate a library of silicon analogues of linezolid without much difficulty. The silapiperidines 3a and 3b on treatment with 3,4-difluoronitrobenzene and 3,4,5-trifluoronitrobenzene, resulted in compounds 4a–4c by a simple nucleophilic aromatic substitution. The nitro group was reduced with H2–Pd/C in THF followed by Cbz protection of the resulting amine in one pot to give the intermediates 5a–5c. Compounds 5a–5c were treated with chiral building block A(29) in the presence of LiOtBu in dimethylformamide (DMF) to furnish the oxazolidinone core. Boc deprotection was achieved with trifluoroacetic acid (TFA) in CH2Cl2, and the salts were neutralized to afford the free amines 6a–6c (Scheme 1).
Scheme 1. Synthesis of Oxazolidinone Amines with Silicon Incorporation.
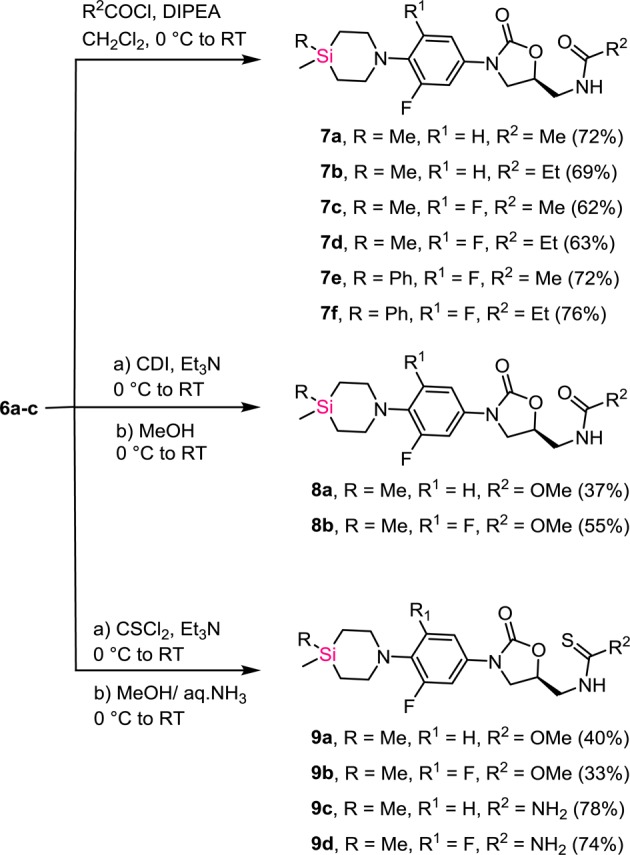
These oxazolidinone amines 6a–6c were treated with acetyl chloride and propionyl chloride to give the corresponding amides 7a–7f. Treatment of amines 6a and 6b with carbonyldiimidazole (CDI) followed by addition of methanol produced two methylcarbamate derivatives 8a and 8b.29 The reaction of amines 6a and 6b with thiophosgene followed by methanol yielded the thiocarbamates 9a and 9b. Similarly, quenching with aqueous ammonia resulted in the thiourea derivatives 9c and 9d (Scheme 2).
Scheme 2. Synthesis of Target Oxazolidinones with Silicon Incorporation.
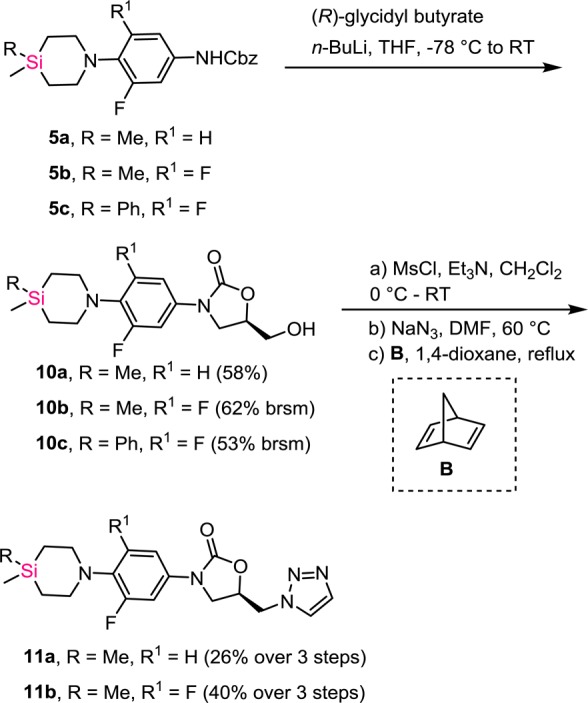
For the generation of compounds with varying structural features, compounds 5a–5c were treated with n-BuLi and (R)-glycidyl butyrate to furnish the hydroxyl derivatives 10a–10c. The alcohols 10a and 10b were converted to the corresponding mesylates and the mesylate group was displaced with azide. The azide on heating with norbornadiene underwent a 1,3-dipolar cycloaddition followed by retro Diels–Alder reaction to furnish the triazoles 11a and 11b, respectively (Scheme 3).
Scheme 3. Synthesis of Triazole-Based Oxazolidinones.
After synthesizing several silicon analogues, the antibacterial activity was assessed against various strains. MIC (minimum inhibitory concentration) of NCEs were determined by microbroth dilution method against facultative bacteria. The screening results of all compounds are provided in the Supporting Information. Among the screened oxazolidinones, the compounds 7a, 7c, 7d, 9a, and 9d were more active against a majority of the bacterial strains tested. Compound 7a, which is the closest linezolid analogue of all the compounds synthesized, showed good potency, but 4–8-fold less potent compared to linezolid across the strains. Introduction of additional fluorine atom on to aromatic ring (7c) resulted in a modest improvement in the potency. The compound with thiocarbamate functionality 9a was the most potent compound in the series with activity comparable to that of linezolid. The presence of phenyl group on silicon resulted in a loss of potency (see Supporting Information). The alcohols 10a–10c were found to be less potent. In general the addition of fluorine atom in the aromatic ring enhanced the antibacterial activity. However, addition of a fluorine atom onto the aromatic ring resulted in a marked decrease in potency (9a vs 9b, see Supporting Information) in compounds belonging to the thiocarbamate series. After analysis of the structural features present in some of the potent oxazolidinones reported in literature, compounds 11a and 11b were prepared with triazole moieties in place of N-acyl group.30 However, we did not observe significant activity with these compounds.
Upon completion of in vitro testing of antibacterial activities, three out of the five best compounds (7a, 7c, and 9a) from this series were selected for ADME and physicochemical property studies. Specifically, solubility across the pH range, stability in plasma, stability in microsomes, and plasma protein binding were evaluated (results compiled in Table 1). Compound 7a was soluble across the pH range tested with values being similar to that of linezolid. The solubility of compounds 7c and 9a was also comparable to linezolid at acidic pH; however, it was decreased at higher pH conditions. All silicon compounds demonstrated very good plasma stability profile similar to that of linezolid. All three compounds (7a, 7c, and 9a), along with linezolid, were screened for their microsomal metabolic stability in three different species (mouse, rat, and human). Compounds 7a and 7c were moderately stable in both mouse and human liver microsomes with 7c being superior among the two. Compound 9a showed poor stability in rodent liver microsomes, but it showed better stability in human microsomes. In the case of plasma protein binding studies, we found striking difference between linezolid and sila compounds. All three compounds, 7a, 7c, and 9a, were strongly bound to the plasma proteins. Hence, this can be an advantage for the improvement in BBB penetration. Although free drug concentrations are generally associated with greater antimicrobial activity, the success of telavancin and daptomycin reflect the benefit associated with high protein binding (lower clearance, longer half-life, and longer duration of action). The discrepancy in findings can be attributed to the difference in the static in vitro test systems vis-à-vis the dynamic nature in an in vivo setting wherein several factors such as binding affinity of the drug to the proteins, transport across barriers, physiological conditions, and metabolism play a major role.31 Based on the overall in vitro profile, compound 7a was selected for detailed in vivo pharmacokinetic studies in mice (results are compiled in the table provided in the Supporting Information). Although compound 7a demonstrated 100% bioavailability and similar half-life as compared to linezolid, it was inferior in terms of Cmax, AUC, and clearance. However, the volume of distribution (Vz) of 7a was twice that of linezolid, which can be attributed to its high plasma protein binding. Next, we decided to understand BBB penetrating potential of the silicon compounds, which was the main objective of this project. Toward this goal, all three selected compounds, i.e., 7a, 7c, and 9a were administered through oral route and various parameters were measured. The details of experimental protocol and all the measurements are placed in the Supporting Information. Interestingly, all the three compounds displayed significant brain penetration. Compounds 7a, 7c, and 9a had a 14-, 22-, and 29-fold higher B/P ratios compared to linezolid (see Table 2). These ratios were calculated using AUC measurements. Calculations using Cmax also gave similar ratios. It is worth highlighting that actual brain concentrations of the sila compounds 7a, 7c, and 9a are much superior with respect to linezolid. Out of the three compounds, 7c was the best in terms of actual drug concentration (Cmax = 5.58 μg/g and AUC = 16.44 μg·h/g). As the siliconized linezolid analogues displayed impressive B/P ratio, we became interested in testing these compounds against selected bacterial strains (S. pneumoniae and N. meningitidis) that cause brain infections.2 The MIC values generated using various strains suggest that all three compounds possess comparable activity with respect to S. pneumoniae (Table 3).32 However, in the case of N. meningitidis strains, only compound 9a showed significant activity and other two compounds 7a and 7c did not show the activity up to 32 μg/mL. Although the antibacterial potencies are less when compared to the marketed drug linezolid, the higher B/P ratio of silicon compounds suggest that incorporation of silicon is beneficial in terms of BBB penetration.
Table 1. In Vitro PhysChem and ADME Data.
| solubility (μM) at pH |
% plasma stability |
% metabolic stability in liver microsomes
(after 30 min) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| compd | 1.2 | 2.2 | 4.5 | 7.4 | 10.2 | rat | human | mouse | rat | human | % human PPB |
| LZD | 50 | 50 | 50 | 49 | 50 | 100.0 | 100.0 | 100.0 | 88.3 | 100.0 | 26.04 |
| 7a | 50 | 50 | 41 | 40 | 41 | 97.3 | 100.0 | 40.8 | 10.8 | 48.9 | 94.33 |
| 7c | 48 | 43 | 20 | 17 | 20 | 94.7 | 100.0 | 68.4 | 9.6 | 69.8 | 99.60 |
| 9a | 48 | 47 | 9 | 2 | 2 | 100.0 | 100.0 | 15.2 | 5.7 | 43.0 | 100.00 |
Table 2. Brain PK Comparison of 7a, 7c, 9a, and LZDa.
|
7a |
7c |
9a |
LZD |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| route | brain | plasma | B/P ratio | brain | plasma | B/P ratio | brain | plasma | B/P ratio | brain | plasma | B/P ratio |
| dose | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | ||||
| N | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | ||||
| Cmax | 1.33 | 1.05 | 1.27 | 5.58 | 2.02 | 2.76 | 1.47 | 0.37 | 3.96 | 0.45 | 3.65 | 0.12 |
| AUC 0-t | 3.01 | 1.78 | 1.69 | 14.74 | 5.80 | 2.54 | 3.11 | 0.87 | 3.57 | 0.83 | 7.58 | 0.11 |
| AUC 0-inf | 3.05 | 1.80 | 1.69 | 16.44 | 6.21 | 2.65 | 3.24 | 0.93 | 3.49 | 0.90 | 7.70 | 0.12 |
Units for brain: Cmax = μg/g, AUC0-t = μg·h/g, AUC0-inf = μg·h/g. Units for plasma: Cmax = μg/mL, AUC0-t = μg·h/mL, AUC0-inf = μg·h/mL.
Table 3. Antibacterial Activity of Selected Compounds against S. pneumoniae and N. meningitidis.
| strain | 7ab | 7cb | 9ab | LZDb |
|---|---|---|---|---|
| S.pneumoniae ATCC 49619 | 8 | 16 | 4 | 0.5 |
| S.pneumoniae ATCC 6303 | 4 | 8 | 4 | 0.5 |
| S.pneumoniae 6303 LZDR | >32 | >32 | 32 | 32 |
| S.pneumoniae ATCC 700904 PenR, erm+ve | 4 | 16 | 4 | 1 |
| N.meningitidisa E-63 | 32 | >32 | 32 | 8 |
| N.meningitidisa M-1 | >32 | >32 | 32 | 8 |
| N.meningitidisa 306 | >32 | >32 | 32 | 8 |
| N.meningitidisa E-95 | >32 | >32 | 32 | 8 |
| N.meningitidisa 184 | >32 | >32 | 32 | 8 |
Clinical isolates.
MIC values are measured in μg/mL.
In conclusion, we have designed and synthesized various oxazolidinones with the incorporation of silicon. Three compounds 7a, 7c, and 9a were identified as potential lead molecules from the present series, demonstrating up to 30-fold higher B/P ratio as compared to the marketed antibiotic drug, linezolid. These results can be considered as an initial step toward the development of brain penetrant oxazolidinone antibiotics. The demonstrated concept with the incorporation of silicon into known drug scaffold to improve CNS exposures can also be applied to other classes of compounds. Profiling of selected compounds in brain infected preclinical models is the future course of action and the goal is to further optimize the identified compounds toward the development of an antibiotic that can be useful in treating CNS infections.
Glossary
ABBREVIATIONS
- NCE
new chemical entity
- brsm
based on recovered starting material
- LZD
linezolid
- ADME
absorption, distribution, metabolism, excretion
- N
number of subjects
- AUC
area under the curve
- t1/2
half-life
- Kel
elimination rate constant
- Clz
clearance
- BA
bioavailability
- B/P ratio
brain to plasma ratio
- PPB
plasma protein binding
Supporting Information Available
The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acsmedchemlett.5b00213.
Experimental details; compound characterization details; screening details; antibacterial data for all the compounds; protocols for pharmacokinetic studies including brain PK; data from mice PK experiments (PDF)
Author Contributions
The manuscript was written through contributions of all authors. All authors have given approval to the final version of the manuscript.
BIRAC (Biotechnology Industry Research Assistance Council), New Delhi for the support through CRS Scheme (BT/CRS0046/CRS-02/12). Initially, this project was supported by NCL-IGIB joint collaborative project (BSC-0124) and NCL in-house grants. B.S.R. and R.R. thank CSIR, New Delhi for the award of fellowship.
The authors declare no competing financial interest.
Dedication
This work is dedicated to Professor Sourav Pal, Indian Institute of Technology, Bombay and former Director, CSIR-NCL, Pune on the occasion of his 60th birthday.
Supplementary Material
References
- Data taken from WHO factsheet on meningitis. http://www.who.int/gho/epidemic_diseases/meningitis/en/ (accessed on May 2015).
- Hoffman O.; Weber J. R. Pathophysiology and treatment of bacterial meningitis. Ther. Adv. Neurol. Disord. 2009, 2, 401–412. 10.1177/1756285609337975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabathuler R. Approaches to transport therapeutic drugs across the blood-brain barrier to treat brain diseases. Neurobiol. Dis. 2010, 47, 48–57. 10.1016/j.nbd.2009.07.028. [DOI] [PubMed] [Google Scholar]
- Hawkins B. T.; Davis T. P. The blood-brain barrier/ neurovascular unit in health and disease. Pharmacol. Rev. 2005, 57, 173–185. 10.1124/pr.57.2.4. [DOI] [PubMed] [Google Scholar]
- Gregory W. A.; Brittelli D. R.; Wang C. L. J.; Wuonola M. A.; McRipley R. J.; Eustice D. C.; Eberly V. S.; Bartholomew P. T.; Slee A. M.; Forbes M. Antibacterials. Synthesis and structure-activity studies of 3-aryl-2-oxooxazolidines. 1. The “B’’ group. J. Med. Chem. 1989, 32, 1673–1681. 10.1021/jm00128a003. [DOI] [PubMed] [Google Scholar]
- Barbachyn M. R.; Ford C. W. Oxazolidinone structure–activity relationships leading to linezolid. Angew. Chem., Int. Ed. 2003, 42, 2010–2023. 10.1002/anie.200200528. [DOI] [PubMed] [Google Scholar]
- Stevens D. L.; Dotter B.; Madaras-Kelly K. A review of linezolid: the first oxazolidinone antibiotic. Expert Rev. Anti-Infect. Ther. 2004, 2, 51–59. 10.1586/14787210.2.1.51. [DOI] [PubMed] [Google Scholar]
- Rupprecht T. A.; Pfister H.-W. Clinical experience with linezolid for the treatment of central nervous system infections. Eur. J. Neuro. 2005, 12, 536–542. 10.1111/j.1468-1331.2005.01001.x. [DOI] [PubMed] [Google Scholar]
- Nau R.; Sörgel F.; Eiffert H. Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system infections. Clin. Microbiol. Rev. 2010, 23, 858–883. 10.1128/CMR.00007-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbachyn M. R.; Hutchinson D. K.; Brickner S. J.; Cynamon M. H.; Klemens S. P.; Glickman S. E.; Grega K. C.; Hendges S. K.; Toops D. S.; Ford C. W.; Zurenko G. E. Identification of a novel oxazolidinone (U-100480) with potent antimycobacterial activity. J. Med. Chem. 1996, 39, 680–685. 10.1021/jm950956y. [DOI] [PubMed] [Google Scholar]
- Pankey G. A.; Sabath L. D. Clinical relevance of bacteriostatic versus bactericidal mechanisms of action in the treatment of gram-positive bacterial infections. Clin. Infect. Dis. 2004, 38, 864–870. 10.1086/381972. [DOI] [PubMed] [Google Scholar]
- Patani G. A.; LaVoie E. J. Bioisosterism: A rational approach in drug design. Chem. Rev. 1996, 96, 3147–3176. 10.1021/cr950066q. [DOI] [PubMed] [Google Scholar]
- Lima L. M.; Barreiro E. J. Bioisosterism: A useful strategy for molecular modification and drug design. Curr. Med. Chem. 2005, 12, 23–49. 10.2174/0929867053363540. [DOI] [PubMed] [Google Scholar]
- Meanwell N. A. Synopsis of some recent tactical application of bioisosteres in drug design. J. Med. Chem. 2011, 54, 2529–2591. 10.1021/jm1013693. [DOI] [PubMed] [Google Scholar]
- Franz A. K.; Wilson S. O. Organosilicon molecules with medicinal applications. J. Med. Chem. 2013, 56, 388–405. 10.1021/jm3010114. [DOI] [PubMed] [Google Scholar]
- Ortega R.; Sanchez-Quesada J.; Lorenz C.; Dolega G.; Karawajczyk A.; Sanz M.; Showell G.; Giordanetto F. Design and synthesis of 1,1-disubstituted-1-silacycloalkane-based compound libraries. Bioorg. Med. Chem. 2015, 23, 2716–2720. 10.1016/j.bmc.2015.01.046. [DOI] [PubMed] [Google Scholar]
- Geyer M.; Wellner E.; Jurva U.; Saloman S.; Armstrong D.; Tacke R. Can silicon make an excellent drug even better? An in vitro and in vivo head-to-head comparison between loperamide and its silicon analogue sila-loperamide. ChemMedChem 2015, 10, 911–924. 10.1002/cmdc.201500040. [DOI] [PubMed] [Google Scholar]
- Tacke R.; Heinrich T.; Bertermann R.; Burschka C.; Hamacher A.; Kassack M. U. Sila-haloperidol: A silicon analogue of the dopamine (D2) receptor antagonist haloperidol. Organometallics 2004, 23, 4468–4477. 10.1021/om040067l. [DOI] [Google Scholar]
- Mills J. S.; Showell G. A. Chemistry challenges in lead optimization: silicon isosteres in drug discovery. Drug Discovery Today 2003, 8, 551–556. 10.1016/S1359-6446(03)02726-0. [DOI] [PubMed] [Google Scholar]
- Mills J. S.; Showell G. A. Exploitation of silicon medicinal chemistry in drug discovery. Expert Opin. Invest. Drugs 2004, 13, 1149–1157. 10.1517/13543784.13.9.1149. [DOI] [PubMed] [Google Scholar]
- Gately S.; West R. Novel therapeutics with enhanced biological activity generated by the strategic introduction of silicon isosteres into known drug scaffolds. Drug Dev. Res. 2007, 68, 156–163. 10.1002/ddr.20177. [DOI] [Google Scholar]
- Geyer M.; Karlsson O.; Baus J. A.; Wellner E.; Tacke R. Si- and C- Functional organosilicon building blocks for synthesis based on 4-Silacyclohexan-1-ones containing the silicon protecting groups MOP (4-Methoxyphenyl), DMOP (2,6-Dimethoxyphenyl), or TMOP (2,4,6-Trimethoxyphenyl). J. Org. Chem. 2015, 80, 5804–5811. 10.1021/acs.joc.5b00774. [DOI] [PubMed] [Google Scholar]
- Ramesh R.; Reddy D. S. Zinc mediated allylations of chlorosilanes promoted by ultrasound: Synthesis of novel constrained sila amino acids. Org. Biomol. Chem. 2014, 12, 4093–4097. 10.1039/c4ob00294f. [DOI] [PubMed] [Google Scholar]
- Vivet B.; Cavelier F.; Martinez J. Synthesis of silaproline, a new proline surrogate. Eur. J. Org. Chem. 2000, 2000, 807–811. . [DOI] [Google Scholar]
- Calculated logP (ClogP) values were computed by using the ChemBioDraw Ultra14.0 by Perkin-Elmer.
- The initial results from this series are patented and available in public domain.Reddy D. S.; Balamkundu S.; Ramesh R.. Sila analogs of oxazolidinone derivatives and synthesis thereof. Patent WO 2013054275, 2013.
- Wendeborn S. V.; Lamberth C.; Nebel K.; Crowley P. J.; Nussbaumer H.. Novel triazolepyrimidine derivatives. Patent WO 2006066872, 2006.
- Namane C.; Nicolai E.; Pacquet F.; Pascal C.; Venier O.. Tetrahydroquinoxaline urea derivatives, preparation thereof and therapeutic use thereof. Patent US 20120135958, 2012.
- Perrault W. R.; Pearlman B. A.; Godrej D. B.; Jeganathan A.; Yamagata K.; Chen J. J.; Lu C. V.; Herrinton P. M.; Gadwood R. C.; Chan L.; Lyster M. A.; Maloney M. T.; Moeslein J. A.; Greene M. L.; Barbachyn M. R. The synthesis of N-aryl-5(S)-aminomethyl-2-oxazolidinone antibacterials and derivatives in one step from aryl carbamates. Org. Process Res. Dev. 2003, 7, 533–546. 10.1021/op034028h. [DOI] [Google Scholar]
- Cho Y. L.; Chae S. E.; Baek S. Y.; Kim Y. O.; Kim S. J.; Lee H. S.; Park J. H.; Park T. K.; Woo S. H.; Kim Y. Z.. Novel oxazolidinone derivatives with cyclic amidoxime or cyclic amidrazone and pharmaceutical composition thereof. Patent US 20110178293, 2011.
- Zeitlinger M. A.; Derendorf H.; Mouton J. W.; Cars O.; Craig W. A.; Andes D.; Theuretzbacher U. Protein binding: do we ever learn?. Antimicrob. Agents Chemother. 2011, 55, 3067–3074. 10.1128/AAC.01433-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- We have also determined the cytotoxicity of compounds 7a, 7c, and 9a following 24 h incubation with human hepatoma (HepG2) and tracheal epithelial cells (HTEpiC). Compounds 7c and 9a were nontoxic at >10 μM concentration in both HepG2 and HTEpiC cells. However, the IC50 of compound 7a incubation was 9 μM in HepG2 cells and 5 μM in HTEpiC cells. Details are provided in the Supporting Information.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


