Abstract
Background and Aims:
Ultrasound (US)-guided regional blocks are becoming increasingly popular as its use increases success rate, shortens block onset time and reduces complications. Currently, there exist two methods to perform US-guided axillary brachial plexus block (US-ABPB), the perivascular (PV) and the perineural (PN) techniques. We compared the two techniques to study the block characteristics and other variables using levobupivacaine.
Methods:
In this prospective, randomised trial, 60 patients were randomly allocated to receive a PV (n = 30) or PN (n = 30) US-ABPB. The local anaesthetic agent, 0.5% levobupivacaine and total volume of 36 ml of solution were identical in all the subjects. For both the groups, the musculocutaneous nerve was first located and then anaesthetised with 6 ml. Subsequently in the PV group, 30 ml was deposited dorsal to the axillary artery (6 o’clock position). In PN group, the median, ulnar and radial nerves were individually anaesthetised with volumes of 10 ml each. The onset and duration of sensory block, the onset and duration of motor block, number of failed blocks and complications were noted.
Results:
No difference was observed between the two groups in terms of success rate (PV - 93.33%, PN - 96.66%), sensory onset (PN: 8.07 (standard deviation [SD] ± 0.651) min and PV: 8.14 [SD ± 1.079] min; P = 0.754), motor onset (PN: 14.62 [SD ± 2.077] min and PV: 14.93 [SD ± 1.844] min; P = 0.557) and total duration of anaesthesia. No complications were observed in both groups.
Conclusion:
The PV technique provides a simple alternative for PN US-ABPB. In the light of emerging needling positions for PV and PN techniques, this study calls for large scale trials and much research in this area before one defines best or safe approach. PV technique may be considered as an alternative method for US-ABPB in patients with anatomical variation or difficulties in identifying the individual nerves.
Keywords: Axillary block, levobupivacaine, perineural axillary block, perivascular axillary block, ultrasound
INTRODUCTION
Axillary brachial plexus block (ABPB) is one of the most popular techniques in upper limb surgeries because of its ease, reliability and safety.[1] Blockade occurs at the level of the terminal nerves. The use of ultrasound (US) to guide regional blocks is becoming increasingly popular as it increases success rates, shortens block onset time and reduces the number of needle insertions and complications.
Before the introduction of US, many studies compared transarterial perivascular (PV) injection and various perineural (PN) injection techniques which separately block nerves when performing ABPB. From these results, it had been agreed that there was no difference in the success rate between transarterial PV injection and PN injection.[1] Similar studies were conducted using US.[2,3] With the PN technique, the operator identifies and selectively anaesthetizes the musculocutaneous, median, radial and ulnar nerves. In contrast, the PV technique requires only the localisation (and injection) of the musculocutaneous nerve. Subsequently, local anaesthetic (LA) is deposited dorsal to the axillary artery: Circumferential spread around the latter will, in turn, block the median, radial and ulnar nerves.[2] Demonstration of septa dividing the axillary sheath incompletely refuted the concept of unicompartment structure, according to which the injected LA solution spread easily by simple diffusion to all nerve components of the brachial plexus and constituted the anatomical basis for the single injection technique.[4]
Imasogie et al. and Bernucci et al. compared PN injection and PV injection, reporting that there was no difference in the success rate.[2,3] The efficacy and safety concerns regarding these two techniques still remain questioned.[5,6,7]
Success and the quality of plexus nerve block are dependent on the correct positioning of the LA solution near the desired nerves. We hypothesised that PN technique would result in faster onset as well as better quality compared to PV approach, as LA is deposited very close to the nerves. The primary outcomes were block success rate, defined as block adequate to perform surgery without the need for supplementary blocks or anaesthesia and onset of block. Secondary outcomes were duration of motor and sensory block and the incidence of adverse events.
METHODS
After obtaining Ethics Committee approval and written informed consent, 60 patients undergoing surgery of the forearm, wrist or hand were prospectively enrolled. Block randomisation was performed, in blocks of 10 patients comprising 6 patients per treatment arm, using computer-generated random numbers. Inclusion criteria were age between 18 and 60 years, American Society of Anesthesiologists (ASA) physical status I to II and body weight of 60–90 kg. Exclusion criteria were inability to consent for the study, pre-existing neuropathy, coagulopathy, hepatic or renal failure, allergy to LA agents, pregnancy and prior surgery in the axilla. After arrival in the induction room, an 18- or 20-gauge intravenous catheter was placed in the upper limb contralateral to the surgical site, and uniform intravenous premedication (0.03 mg/kg of midazolam and 0.6 µg/kg of fentanyl) was administered to all patients. Supplemental oxygen (by nasal cannulae at 4 L/min) and standard ASA monitors were applied throughout the procedure.
The nerve block was performed by only two expert anaesthesiologists who had performed US-ABPB 50 times or more. The patients were put in a supine position with their operated arms abducted at 90° and externally rotated and with their elbows bent at 90° towards arm. The location of the nerve and artery was identified using Sonosite Micromaxx® (Sonosite®, Bothell, WA, USA) US machine. The 38-mm linear 7- to 12-MHz probe was covered with Tegaderm® (3M, St. Paul, MN, USA) and positioned across the axillary crease to allow for visualisation of the nerves and the axillary vessels in the short axis. The block was performed under aseptic precautions with the in-plane technique using a 22-gauge, 50 mm needle (Stimuplex®, B. Braun, Melsungen, Germany) connected to a syringe containing 0.5% levobupivacaine.
For both groups, the musculocutaneous nerve was first identified separately in the coracobrachialis; using US guidance, 6 ml of 0.5% levobupivacaine was injected. In the PV group, the needle was then advanced until its tip was positioned just dorsal to the artery. Were the latter to be a clock, this would correspond to the 6 o’clock position. 30 ml of 0.5% levobupivacaine was incrementally injected in this location [Figure 1]. In the PN group, the median, ulnar and radial nerves were individually anaesthetised with 10 ml of 0.5% levobupivacaine. Care was taken to ensure circumferential spread of LA around each nerve [Figure 2].
Figure 1.
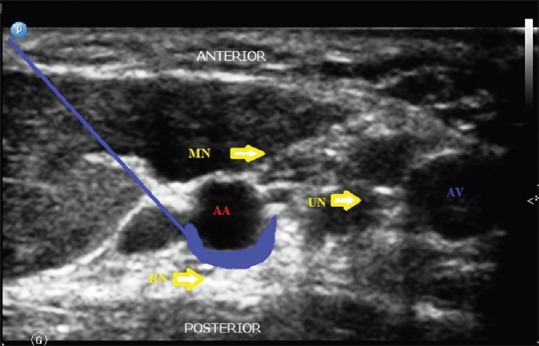
A transverse sonogram showing the median (MN), radial (RN) and ulnar (UN) nerves as indicated by the arrowheads in relation to the axillary artery (AA) and axillary vein (AV). Site of drug injection in perivascular technique shown (blue shaded area)
Figure 2.
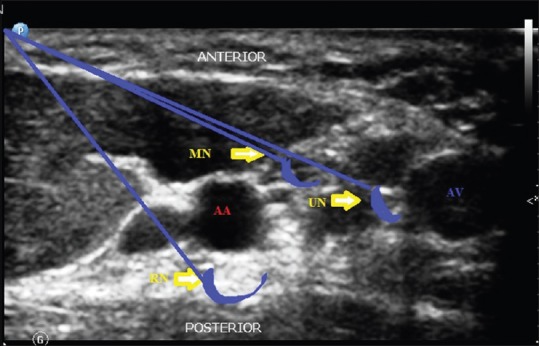
A transverse sonogram showing the median (MN), radial (RN) and ulnar (UN) nerves as indicated by the arrowheads in relation to the axillary artery (AA) and axillary vein (AV). Site of drug injection in perineural technique shown (blue shaded area)
After LA injection through the needle, measurements of brachial plexus blockade and vital parameters were carried out every 2 min until 30 min by a another anaesthesiologist who was blinded to the study methodology. Sensory blockade of the musculocutaneous, median, radial and ulnar nerves was graded according to a 3-point scale using pin prick test: 0 = Sharp pin sensation felt, 1 = analgesia (dull sensation felt), or 2 = anaesthesia (no sensation felt). Sensory blockade of the musculocutaneous, median, radial and ulnar nerves was assessed in the corresponding dermatomal areas. After the completion of the block procedure, sensory onset was considered when there was dull sensation to pin prick (Grade 1) along the distribution of any of the above-mentioned nerves. The duration of sensory block was defined as the time interval between the end of LA administration and the complete resolution of anaesthesia on all nerves.
Motor blockade assessment was based on the modified Bromage scale for upper extremities on a 3-point scale.[8] Grade 0 = normal motor function with full extension of elbow, wrist and fingers, Grade 1 = decrease motor strength with ability to move fingers and/or wrist only and Grade 2 = complete motor blockade with inability to move fingers.
Onset of motor blockade was considered when there was Grade 1 motor blockade after completion of block procedure. Peak motor block was considered when there was Grade 2 motor blockade. The duration of motor block was defined as the time interval between the end of LA administration and the recovery of complete motor function of the hand and forearm.
Postoperatively, motor and sensory blockade and vitals of the patient were noted half hourly till the block completely wore off. The block was considered as failed when analgesia to pin prick was not elicited at the site of surgical incision even after 30 min of drug administration. The onset and duration of sensory block, the onset and duration of motor block, number of failed blocks and complications were noted.
Sample size was calculated based on the onset time of block. According to a previous trial,[2] the onset time (mean ± standard deviation) in PV group and PN group was 18.9 (7.0) min and 13.8 (7.0) min, respectively. To obtain a two-tailed α error of 0.05 (95% confidence level) and a β error of 0.2 (80% power of the study), the calculated sample size was 30 patients in each group, that is, PV group and PN group. Statistical analysis was performed using SPSS version 17 statistical software (SPSS, Chicago, Illinois, USA). Normality of the continuous data was first assessed with the Kolmogorov–Smirnov test. Continuous data were then analysed with the t-test for independent variables. For categorical data, the Chi-square test was used as appropriate. Hypotheses tested were two-tailed. P < 0.05 was considered statistically significant.
RESULTS
Patient demographics and baseline clinical characteristics were similar across the two groups, including the types of surgical procedures performed [Table 1].
Table 1.
Patient characteristics
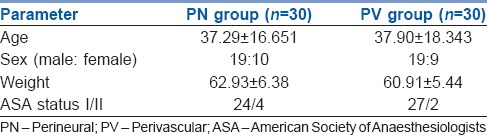
In PN group, there were 19 male patients and 10 female patients and in PV group there were 19 male and 9 female patients. Both groups had predominantly male population. The average age of the patients was 37.29 ± 16.65 years in PN group and 37.90 ± 18.343 years in PV group. The average weight of the patients was 62.93 ± 6.38 kg in PN group and 60.91 ± 5.44 kg in PV group. There were no significant differences in weight and age between the two groups.
In three patients (2 in PV, 1 in PN), block was labelled as failed because of inadequate block and were supplemented with IV agents. No significant difference in the success rates was noted. (PV is 93.33%, PN is 96.66% [P = 0.14]).
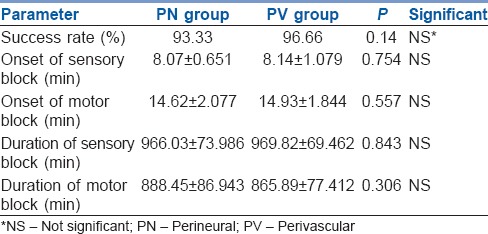
The mean time for onset of sensory block in PN group was 8.07 ± 0.651 min and in PV group was 8.14 ± 1.079 min. The mean time for onset of motor block in PN group was 14.62 ± 2.077 min and in PV group was 14.93 ± 1.844 min. The mean duration of sensory block in PN group was 966.03 ± 73.986 min and in PV group was 969.82 ± 69.462 min. The mean duration of motor block in PN group was 888.45 ± 86.943 min and in PV group was 865.89 ± 77.412 min. The statistical analysis by Student's t-test and unpaired t-test showed that there were no significant differences in the time for onset of sensory block, time for onset of motor block, duration of sensory block and duration of motor block between the two groups. No other adverse events were noted in either groups [Table 2, Graphs 1 and 2].
Table 2.
Block performance characteristics
Graph 1.
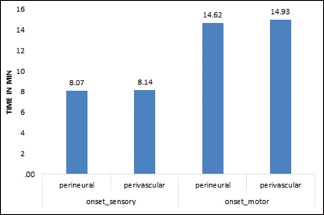
Mean time of onset of sensory and motor block
Graph 2.
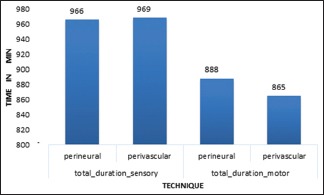
Duration of sensory and motor blockade
DISCUSSION
In this prospective, randomised study, we compared PN and PV US-ABPB. There were no significant differences in patient characteristics between the two groups. The hypothesis of this study was that PN block would be more effective and provide longer duration of anaesthesia as the drug would be in close contact with the nerve. In the present study, we found that PV is as effective as PN technique. Our findings are in line with the findings of Imasogie et al.[3] and Bernucci et al.,[2] who compared PV and PN axillary block. Tran et al. in their study found that double injection technique has similar outcomes compared with its 3 and 4 injection counterparts.[9]
In our study, we have found that onset time in PN was less than PV which was not statistically significant. Bernucci et al. have found that PN resulted in quicker onset times which was statistically significant.[2] This might be because of the use of composite score for analysis of sensory and motor block. The author had graded the sensory and motor blockade of the musculocutaneous, median, radial and ulnar nerves according to a 3-point scale. Our definition of onset times was different (achievement of Grade 1) compared to other studies.
No significant difference was observed in the success rate (PV - 93.33%, PN - 96.66%) as in other studies.[2,3] Pfeiffer et al. observed a success rate of 96.5% with PV US-ABPB.[10] Unlike study by Bernucci et al., our primary outcome measures were block success rate and onset of sensory and motor block. The primary outcome measure in their trial was total anaesthesia-related time (sum of performance and onset times). Factors influencing the success rate are LA volume, time set for determining the success and probably topographical anatomy of nerves in relation to axillary artery.
A study determining the minimum effective volume in double-injection US-ABPB using lignocaine, showed that in regard to 1.5% lignocaine with epinephrine 5 μg/ml, the volume was 23.5 ml for PV and 5.5 ml for the musculocutaneous nerve.[11] Other authors reported that when 2% lignocaine was used in PN injection, anaesthesia was achieved with just 1 ml per nerve.[12] The disadvantage of PV injection is that a larger amount of LA could be required compared to PN injection. In our study, a volume of 36 ml of LA agent was taken to ensure complete spread. Bernucci et al.[2] and Imasogie et al.[3] asserted the ‘silhouette sign’ and ‘doughnut sign’ on US, respectively, as a method to reduce such waste of LA. We did not resort to any such objective parameter for LA spread, as we believe three dimensional spread would be adequate. A recent study that compared two different techniques (6 o’clock and 12 o’clock position) of PV US-ABPB showed no differences.[13]
We did not encounter a single case of vascular puncture in our study. It might be because of extreme caution and attention given to every detail in order to avoid intravascular injection or damaging the nerve. We always made sure that the needle tip was clearly visible throughout the procedure. Sites et al. reported incidences of venous and arterial punctures of 0.6/1000 blocks and 1.2/1000 blocks, respectively.[14] Vascular complication rate was higher (24%) in study by Bernucci et al.[2] This was pointed out by several authors and questioned concerns of safety of PV approach.[5,6,7] We believe, vascular as well as neural complications can be reduced to minimum with good needling techniques in trained hands. In our study, all blocks were performed by only two expert anaesthesiologists who had performed US-ABPB 50 times or more. We concur with Tran et al., in this regard, as our operators’ experience was equally distributed between the two study groups.[15]
The incidence of convulsions and paraesthesia was nil in both the groups. Patients were followed up during the post-operative time for a period of 4 weeks to note delayed onset paraesthesia. Vital parameters, such as pulse rate, systolic blood pressure, diastolic blood pressure and saturation values, were similar in both the groups. No patients in either group required any interventions.
Our study has limitations. We failed to record the number of needle passes, time for surgical readiness after 30 min and performance times. Considering numerous topographical variations in the axilla, we cannot rule out the possibility that some nerves were misidentified. Zero complication rate in our study may be attributable to smaller sample size.
CONCLUSION
The PV technique provides a simple alternative for PN US-ABPB. In the light of emerging needling positions for PV and PN techniques, this study calls for large scale trials and much research in this area before one defines best or safe approach. PV technique may be considered as an alternative method for US-ABPB in patients with anatomical variation or difficulties in identifying the individual nerves.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors would like to thank Dr. R Manjula, Assistant Professor, Department of Community Medicine and Dr. Anita Herur, Associate Professor, Department of Physiology, SN Medical College, Bagalkot, for statistical analyses.
REFERENCES
- 1.Tran QH, Clemente A, Doan J, Finlayson RJ. Brachial plexus blocks: A review of approaches and techniques. Can J Anaesth. 2007;54:662–74. doi: 10.1007/BF03022962. [DOI] [PubMed] [Google Scholar]
- 2.Bernucci F, Gonzalez AP, Finlayson RJ, Tran DQ. A prospective, randomized comparison between perivascular and perineural ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med. 2012;37:473–7. doi: 10.1097/AAP.0b013e3182576b6f. [DOI] [PubMed] [Google Scholar]
- 3.Imasogie N, Ganapathy S, Singh S, Armstrong K, Armstrong P. A prospective, randomized, double-blind comparison of ultrasound-guided axillary brachial plexus blocks using 2 versus 4 injections. Anesth Analg. 2010;110:1222–6. doi: 10.1213/ANE.0b013e3181cb6791. [DOI] [PubMed] [Google Scholar]
- 4.Serradell A, Herrero R, Villanueva JA, Santos JA, Moncho JM, Masdeu J. Comparison of three different volumes of mepivacaine in axillary plexus block using multiple nerve stimulation. Br J Anaesth. 2003;91:519–24. doi: 10.1093/bja/aeg215. [DOI] [PubMed] [Google Scholar]
- 5.Aveline C. Ultrasound-guided axillary perivascular approach: Efficacy and safety remain to be proved. Reg Anesth Pain Med. 2013;38:74. doi: 10.1097/AAP.0b013e31827775ae. [DOI] [PubMed] [Google Scholar]
- 6.Alakkad H, Chin KJ. The importance of good needling technique in ultrasound-guided axillary block. Reg Anesth Pain Med. 2013;38:166. doi: 10.1097/AAP.0b013e31827adca7. [DOI] [PubMed] [Google Scholar]
- 7.Wong MH, George A, Varma M. Ultrasound-guided perivascular axillary brachial plexus block: Not so simple. Reg Anesth Pain Med. 2013;38:167. doi: 10.1097/AAP.0b013e31827b6750. [DOI] [PubMed] [Google Scholar]
- 8.Swami SS, Keniya VM, Ladi SD, Rao R. Comparison of dexmedetomidine and clonidine (α2 agonist drugs) as an adjuvant to local anaesthesia in supraclavicular brachial plexus block: A randomised double-blind prospective study. Indian J Anaesth. 2012;56:243–9. doi: 10.4103/0019-5049.98767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tran DQ, Pham K, Dugani S, Finlayson RJ. A prospective, randomized comparison between double-, triple-, and quadruple-injection ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med. 2012;37:248–53. doi: 10.1097/AAP.0b013e31824611bf. [DOI] [PubMed] [Google Scholar]
- 10.Pfeiffer K, Weiss O, Krodel U, Hurtienne N, Kloss J, Heuser D. Ultrasound-guided perivascular axillary brachial plexus block. A simple, effective and efficient procedure. Anaesthesist. 2008;57:670–6. doi: 10.1007/s00101-008-1377-z. [DOI] [PubMed] [Google Scholar]
- 11.González AP, Bernucci F, Pham K, Correa JA, Finlayson RJ, Tran DQ. Minimum effective volume of lidocaine for double-injection ultrasound-guided axillary block. Reg Anesth Pain Med. 2013;38:16–20. doi: 10.1097/AAP.0b013e3182707176. [DOI] [PubMed] [Google Scholar]
- 12.O’Donnell BD, Iohom G. An estimation of the minimum effective anesthetic volume of 2% lidocaine in ultrasound-guided axillary brachial plexus block. Anesthesiology. 2009;111:25–9. doi: 10.1097/ALN.0b013e3181a915c7. [DOI] [PubMed] [Google Scholar]
- 13.Cho S, Kim YJ, Kim JH, Baik HJ. Double-injection perivascular ultrasound-guided axillary brachial plexus block according to needle positioning: 12 versus 6 o’clock position of the axillary artery. Korean J Anesthesiol. 2014;66:112–9. doi: 10.4097/kjae.2014.66.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sites BD, Taenzer AH, Herrick MD, Gilloon C, Antonakakis J, Richins J, et al. Incidence of local anesthetic systemic toxicity and postoperative neurologic symptoms associated with 12,668 ultrasound-guided nerve blocks: An analysis from a prospective clinical registry. Reg Anesth Pain Med. 2012;37:478–82. doi: 10.1097/AAP.0b013e31825cb3d6. [DOI] [PubMed] [Google Scholar]
- 15.Tran DQ, Bernucci F, González AP, Finlayson RJ. Reply to Dr Aveline. Reg Anesth Pain Med. 2013;38:75. doi: 10.1097/AAP.0b013e318278187d. [DOI] [PubMed] [Google Scholar]


