Abstract
Oral focal mucinosis (OFM) is a rare soft tissue lesion of unknown aetiology. Clinically, it is most commonly found on the gingiva and presents as a painless, sessile or pedunculated mass. Histologically, it is characterized by focal myxoid degeneration of underlying connective tissue. Fifty-three-year-old patient reported with a painless, firm and fibrous gingival overgrowth present from 7 to 8 months. Clinical examination and patient's history pointed towards “irritation fibroma”. An excisional biopsy was performed. The histopathologic diagnosis was established as OFM, an uncommon and poorly characterized type of lesion. This case report stresses on the fact that prediagnosis of OFM is almost impossible. Thus though rare, OFM must be considered in the differential diagnosis of soft tissue overgrowths in oral cavity.
Keywords: Alcian blue, biopsy, gingival overgrowth
INTRODUCTION
Oral focal mucinosis (OFM) is an uncommon tumor-like growth arises due to unknown etiology.[1] It is considered to be the oral counterpart of cutaneous focal mucinosis. In 1966 Jhonson and Hoelwing reported skin lesions with similar features on face, trunk and extremities.[2] Tomich was the first to describe the occurrence of oral lesions in 1974. He proposed that OFM develops as a result of local hyaluronic acid overproduction by fibroblasts.[3]
The objective of this article is to report the occurrence of relatively rare lesion and its management.
CLINICAL PRESENTATION
A 53-year-old female patient reported to the MGV's KBH Dental College and Hospital, Nashik with the chief complaint of a lump on the gums. After primary evaluation, the patient was referred to the Department of Periodontology.
On oral examination, a painless, firm and fibrous gingival overgrowth approximately (10 cm × 2 cm) was located on the buccal aspect of 33–35 region. Lesion was sessile and firmly attached to underlying gingiva. The lesion appeared pale pink with flecks of melanin pigmentation which was similar to adjacent gingival tissues. Surface of the lesion was smooth and non-lobulated. Lesion had well defined borders extending from mesial aspect of 33 to distal aspect of 35. It was limited laterally by the lower lip mucosa and coronally by the gingival sulcus of the involved teeth [Figure 1].
Figure 1.

Clinical appearance of lesion at first presentation. (a) Frontal view. (b) Left lateral view. (c) Lingual view
The patient was otherwise systemically healthy having no adverse habits. The lesion was present approximately since last 7–8 months. Initially, it was very small in size and the patient attempted to rupture it twice with a safety pin. Since her last attempt about a month and half ago, the lesion initially shrunk in its size however after which it expanded quite rapidly to existing one. The discomfort due to its increased size made her to report to the college. Based on history and clinical examination, a provisional diagnosis of “irritation fibroma” was made.
Investigations
Routine laboratory investigations like Hb%, bleeding time and clotting time were in normal limits. The intraoral periapical radiographic revealed mild horizontal interproximal crestal bone loss between 33 and 34. Also vertical interproximal bone loss observed between 34 and 35. Lamina dura was intact and periodontal ligament space appeared normal [Figure 2]. An occlusal radiograph was also taken to rule out any evidence of calcification within the lesion [Figure 3].
Figure 2.
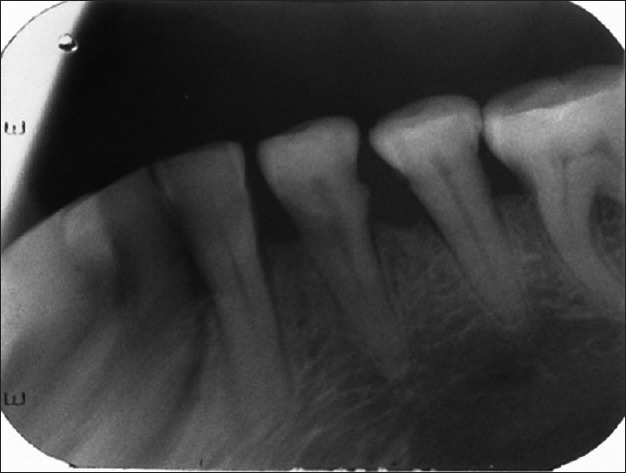
Intraoral periapical projection of teeth involved
Figure 3.

Occlusal projection of the lesion. Arrow indicates shadow of the lesion on X-ray without any calcifications
Management
A thorough scaling and root planning was done to remove local irritants. With patient's consent a surgical excision of the lesion was planned. Under local anesthesia, a 3-0 silk suture was passed through the lesion for ease of retraction during excision. Using no. 15 B. P. blade, lesion was excised in toto [Figure 4]. Operated area was debrided and periodontal dressing was placed [Figure 5]. The excised lesion was stored in 10% formalin and sent for histopathological examination. After a week, dressing was removed and uneventful healing by secondary intention was observed [Figure 6].
Figure 4.
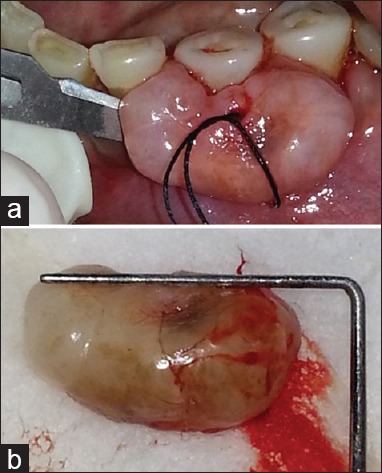
(a) Excision of the lesion under local anaesthesia using No. 15 blade. (b) Excised lesion
Figure 5.
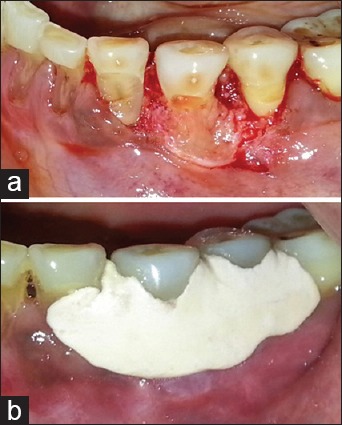
(a) Thorough debridement performed. (b) Periodontal dressing given
Figure 6.

Healing after 7 days
Histopathological findings
The hematoxylin and eosin, staining revealed stratified squamous hyper-parakeratinized epithelium. Sub-epithelial stroma demonstrated loose, pale eosinophilic myxomatous connective tissue. Deeper stroma composed of stellate shaped fibroblasts interspersed between thin collagen fiber bundles and numerous small capillaries [Figure 7]. Alcian blue at pH 2.5 showed strong blue staining due presence of abundant hyaluronic acid [Figure 8]. Based on these histological features,[1] a definitive diagnosis of “OFM” was made.
Figure 7.
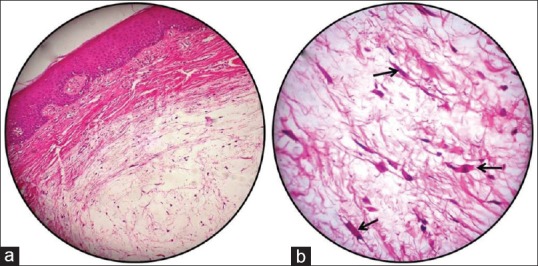
(a) Photomicrograph showing the surface epithelium with the underlying myxoid stroma (H and E, ×10) (b) Loose myxoid stroma having numerous plump fibroblasts (black arrows)
Figure 8.
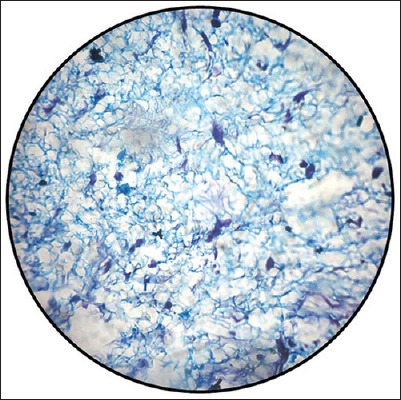
Positive alcian blue staining (pH 2.5) of myxoid stroma suggesting presence of hyaluronic acid
Clinical course
Patient is being reviewed periodically. At 3rd month postoperative review, surgical area healed satisfactorily with no signs of recurrence.
DISCUSSION
Since the original report by Tomich, 60 cases of OFM were reported in English literature and only five cases have been reported in Indian literature.[2]
Based on the literature review, OFM shows predilection for adult women (62%),[4] keratinized mucosa, gingiva in particular (80% of reported cases)[2] and mandibular arch over maxillary arch.[5] Clinically OFM presents as a solitary, painless, non-ulcerated, round, elevated overgrowth.[2] Current case corroborates all these observations.
The etiology of OFM is unknown. Tomich suggested a probable mechanism for formation of OFM as “overproduction of hyaluronic acid by the fibroblasts at the expense of collagen production”.[1] However, the reason behind this overproduction is not well understood. In the current case, intense blue staining of hyaluronic acid by alcian blue stain during histopathological analysis is in accordance with given theory.
There is controversy as to whether local trauma plays a role in the etiology of OFM. Tomich[1] said it does not play a role while Gnepp et al. documented trauma as a contributing factor.[6] In the current case, the history of trauma seems to have aggravated size of the lesion. Shafer et al. suggested that most of these lesions actually represent myxomatous or “mucinous” change in a preexisting fibrous lesion.[7,8] The possibility of it cannot be ruled out in the existing case.
From histological aspect, OFM needs to be differentiated from nerve sheath myxoma and peripheral odontogenic myxoma. The nerve sheath myxoma is more circumscribed, has fibrous septa between multiple myxoid nodules, and has more plump stromal cells. Peripheral odontogenic myxoma shows presence of mast cells, increased reticular fibers and islands of odontogenic epithelium.[5,8] Central odontogenic myxoma is a symptomless bony swelling expanding cortices from within whereas OFM is a peripheral soft tissue lesion.[5] None of these histologic features were found in our case. Hence diagnosis of OFM was confirmed.
Clinically, the differential diagnoses of OFM will include:[8,9]
-
Inflammatory lesions:
- Fibrous hyperplasia
- Peripheral giant cell granuloma
- Epulis fissuratum
- Pyogenic granuloma.
-
Tumors:
- Peripheral fibroma
- Peripheral ossifying fibroma
- Peripheral ameloblatoma
- Peripheral odontogenic myxoma
- Malignant and metastatic tumors in gingiva.
-
Non-plaque induced lesions:
- Irritation fibroma.
However, none of the articles reported a clinical diagnosis of “OFM” at its first presentation. The histological analysis was always the basis for diagnosis. Thus due to rarity of its occurrence, a preoperative diagnosis is almost impossible.[9,10] Nevertheless surgical excision of lesion seems to be a safe approach without any reports of recurrence.[1]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bosco AF, Macarini VC, Milanezi de Almeida J, Theodoro LH, Novaes VC, Júnior EC, et al. Oral focal mucinosis: Clinical case presentation with a focus on esthetic and functional surgical resolution. Clin Adv Periodontics. 2014;4:251–5. doi: 10.1902/cap.2013.130018. [DOI] [PubMed] [Google Scholar]
- 2.Bharti V, Singh J. Oral focal mucinosis of palatal mucosa: A rare case report. Contemp Clin Dent. 2012;3(Suppl 2):S214–8. doi: 10.4103/0976-237X.101098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tomich CE. Oral focal mucinosis. A clinicopathologic and histochemical study of eight cases. Oral Surg Oral Med Oral Pathol. 1974;38:714–24. doi: 10.1016/0030-4220(74)90392-2. [DOI] [PubMed] [Google Scholar]
- 4.Garcia A, Bravo-Calderón D, Costa M, Oliveira D. Oral focal mucinosis arising on the gingiva of orthodontic patient. J Stomatol. 2012;2:277–9. [Google Scholar]
- 5.Iezzi G, Rubini C, Fioroni M, Piattelli A. Oral focal mucinosis of the gingiva: Case report. J Periodontol. 2001;72:1100–2. doi: 10.1902/jop.2001.72.8.1100. [DOI] [PubMed] [Google Scholar]
- 6.Gnepp DR, Vogler C, Sotelo-Avila C, Kielmovitch IH. Focal mucinosis of the upper aerodigestive tract in children. Hum Pathol. 1990;21:856–8. doi: 10.1016/0046-8177(90)90056-b. [DOI] [PubMed] [Google Scholar]
- 7.Saito I, Ide F, Enomoto T, Kudo I. Oral focal mucinosis. J Oral Maxillofac Surg. 1985;43:372–4. doi: 10.1016/0278-2391(85)90259-9. [DOI] [PubMed] [Google Scholar]
- 8.Safer WG, Hine MK, Levy BM. Disturbances of development and growth. In: Rajendran R, editor. A Textbook of Oral Pathology. 6th ed. Philadephia: WB Saunders Co; 2009. p. 148. [Google Scholar]
- 9.Gabay E, Akrish S, Machtei EE. Oral focal mucinosis associated with cervical external root resorption: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e75–8. doi: 10.1016/j.tripleo.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 10.Lee JG, Allen G, Moore L, Gue S. Oral focal mucinosis in an adolescent: A case report. Aust Dent J. 2012;57:90–2. doi: 10.1111/j.1834-7819.2011.01649.x. [DOI] [PubMed] [Google Scholar]


