ABSTRACT
Human enterovirus A71 (EV-A71) belongs to the Enterovirus A species in the Picornaviridae family. Several vaccines against EV-A71, a disease causing severe neurological complications or even death, are currently under development and being tested in clinical trials, and preventative vaccination programs are expected to start soon. To characterize the potential for antigenic change of EV-A71, we compared the sequences of two antigenically diverse genotype B4 and B5 strains of EV-A71 and identified substitutions at residues 98, 145, and 164 in the VP1 capsid protein as antigenic determinants. To examine the effects of these three substitutions on antigenicity, we constructed a series of recombinant viruses containing different mutation combinations at these three residues with a reverse genetics system and then investigated the molecular basis of antigenic changes with antigenic cartography. We found that a novel EV-A71 mutant, containing lysine, glutamine, and glutamic acid at the respective residues 98, 145, and 164 in the VP1 capsid protein, exhibited neutralization reduction against patients' antisera and substantially increased virus binding ability to human cells. These observations indicated that this low-neutralization-reactive EV-A71 VP1-98K/145Q/164E mutant potentially increases viral binding ability and that surveillance studies should look out for these mutants, which could compromise vaccine efficacy.
IMPORTANCE Emerging and reemerging EV-A71 viruses can cause severe neurological etiology, primarily affecting children, especially around Asia-Pacific countries. We identified a set of mutations in EV-A71 that both reduced neutralization activity against humoral immunity in antisera of patients and healthy adults and greatly increased the viral binding ability to cells. These findings provide important insights for EV-A71 antigenic determinants and emphasize the importance of continuous surveillance, especially after EV-A71 vaccination programs begin.
INTRODUCTION
Enterovirus A71 (EV-A71) has become a public health issue primarily affecting children, especially around Asia-Pacific countries. EV-A71 infection causes fever, hand, foot, and mouth disease (HFMD), or herpangina, occasionally resulting in severe neurological complications (1). EV-A71, a positive-sense single-stranded RNA virus in the Picornaviridae family, has an RNA genome that encodes the capsid proteins VP1 to VP4 and the nonstructural proteins 2A to 2C and 3A to 3D. The EV-A71 capsid proteins VP1 to VP3 are exposed on the viral external surface and are involved in receptor binding and viral antigenicity. P-selectin glycoprotein ligand-1 (PSGL-1), expressed in lymphoid cells, and scavenger receptor B2 (SCARB2), broadly expressed in most tissues, are the first two EV-A71 receptors identified (2, 3). The structural protein VP1 contains key binding residues to these two receptors (4, 5) and antigenic sites for antibody recognition (6–9).
Based on phylogenetic analysis of VP1 protein coding sequences, most EV-A71 isolates are classified into genotypes A, B, and C (10–12), while some isolates belong to the recently described/discovered genotypes D, E, F, and G (13). Genotypes B and C consist of subgenotypes B1 to B5 and C1 to C5, respectively. EV-A71 genotype A was first reported in California, and genotypes B and C have caused large outbreaks worldwide. The emergence of a novel genotype or subgenotype can lead to large outbreaks, and high-incidence epidemics have occurred in the Asia-Pacific region since 1997. These outbreaks, resulting from intergenotypic and intragenotypic shifts, have occurred in Malaysia, Singapore, Australia, Brunei, Taiwan, and Japan in Asia, as well as in the Netherlands, Denmark, Germany, and France in Europe (reviewed in reference 14). Each genotypic change reflects the accumulation of mutations due to the error-prone nature of the RNA polymerase in viral replication (15). Because genetic adaptation of the virus might increase viral survival advantage, we need to investigate and understand the driving forces behind these genotypic changes. One such potential force is preexisting humoral immunity: for influenza virus, for example, the observed antigenic drift in the hemagglutinin gene is a result of antibody escape (16). We have previously reported and characterized antigenic variation among genotypes isolated from EV-A71 outbreaks with antigenic cartography (15); we also observed antigenic variation within each genotype, as a result of sporadic sequence variations. Importantly, genotyping of a virus strain cannot predict its antigenicity (17), and we hypothesize that changes in antigenicity may be governed by only a few positions on the capsid protein. Both sequence differences between genotypes and within-genotype genetic variations of the capsid proteins are thought to be responsible for antigenic variation among circulating EV-A71 strains.
To date, several EV-A71 vaccines have been progressively developed, and clinical trials are being or have been performed in China (phase III), Taiwan (phase I), and Singapore (phase I) (reviewed in reference 18). The seed strains for these vaccines were from different genotypes: C4a in China, B4 (E59 strain) in Taiwan, and B3 in Singapore. Cross-reactivity results of antisera from these different trials suggest a broad protection against several strains from different genotypes (19, 20). However, these results report only antiserum reactivity against a limited number of viruses and may not fully reflect the cross-reactivity against all circulating viruses, especially if antigenicity can differ based on a few mutations on the capsid protein. Once the EV-A71 vaccine is approved and the vaccination program rolled out, the build-up of intestinal immunity among vaccinees may contribute to evolutionary pressures on EV-A71. Strains that contain adaptive mutations will thus acquire a viral fitness advantage and may consequently become new globally dominant strains. Here, we identified genetic mutations among circulating viruses that may be at the basis of antigenic change and constructed a series of mutant viruses with these mutations. The antigenic properties of each combination of mutations were examined based on the neutralizing activity of human antisera, using antigenic cartography. This study provides an approach to map antigenic determinants of EV-A71 as well as to predict potential low antibody reactive mutations that may arise and cause a public health concern upon rolling out of EV-A71 vaccination programs.
MATERIALS AND METHODS
Cells and viruses.
RD (rhabdomyosarcoma) cells were maintained in Dulbecco's modified Eagle's medium (Gibco) containing 10% fetal bovine serum (FBS) and 2% streptomycin-ampicillin. Viruses were grown in RD cells with 2% FBS and 100 IU of penicillin, with 100 μg of streptomycin per ml at 37°C in 5% CO2. EV-A71 isolates N7008-TW99 (B4, GenBank accession number FJ357375) and N1745-TW08 (B5, GenBank accession number KF974789) were obtained from National Cheng Kung University Hospital, Tainan, Taiwan. To prepare stocks, viruses were propagated with a single passage in RD cells, and their titers were determined by plaque assay in RD cells as described previously (21).
Sera.
Anti-EV-A71 human sera were obtained from healthy adults or infected children under 3 years of age in the National Cheng Kung University Hospital, Tainan, Taiwan. We used information on the viral genotype that infected each patient to randomly select one or two antisera against genotypes B4, B5, C2, and C4 and measured neutralization titers against each recombinant mutant virus. To select the healthy donor sera, a total of 15 sera from healthy adults were examined for their neutralization titers against N7008-TW99 virus. All sera from healthy adults had neutralization antibody titers of ≥1:8, and the six sera containing neutralization antibody titers of ≥1:128 were selected for further investigation of antigenicity. This study was approved by the Institutional Review Board of the National Cheng Kung University Hospital (Tainan, Taiwan).
Construction of infectious cDNA clones of the wild type and site-directed mutagenesis.
EV-A71 viral RNA was extracted from culture fluid of infected cells by a viral nucleic acid extraction kit (Geneaid), and reverse transcription (RT)-PCR was performed with SuperScript III reverse transcriptase (Invitrogen). Full-length cDNA fragments were amplified by RT-PCR with specific primer pairs, as described previously (21). Specific primer pairs were designed based on EV-A71 sequences, and cDNA products of RT-PCR were cloned into a pCR-XL-TOPO vector (Invitrogen). To construct reverse genetics viruses with various mutations, we designed a series of primers (available upon request) and performed site-directed mutagenesis by overlapping PCR as previously described (21). Wild-type and mutant cDNA clones were sequenced to confirm the presence of mutations. These recombinant DNA experiments were approved by the Biohazard Safety Committee of the National Cheng Kung University (Tainan, Taiwan).
Viral RNA synthesis and transfection.
Plasmid DNAs of wild-type and mutant cDNA clones were linearized by restriction enzyme SmaI (New England BioLabs), and we performed RNA synthesis by RiboMAX Large Scale RNA Production System-T7 (Promega), as per the manufacturer's instructions. After purification, 2 μg viral RNA was transfected into RD cells, using TransMessenger transfection reagent (Qiagen). Recombinant viruses were collected from transfected cells when 90% of cells exhibited cytopathic effects (CPE) and were stored at −80°C.
Microneutralization in conjunction with ELISA detection.
The neutralization-enzyme-linked immunosorbent assay (microNT ELISA) protocol was adapted from the WHO Manual on Animal Influenza Diagnosis and Surveillance (22). Briefly, to quantify the tissue culture infective dose (TCID50) viral titer in microNT ELISA, 10-fold serial dilutions of virus were added to confluent RD cells in a 96-well plate and incubated at 37°C, 5% CO2. After 24 h, supernatants were removed, and cells were fixed by acetone for 30 min and then washed with phosphate-buffered saline containing 0.05% Tween 20 (PBS-T). We then used an ELISA to detect virus. Acetone-fixed cells were incubated with mouse anti-EV-A71 monoclonal antibody (Mab979, 1:2,000; Millipore) at 37°C for 2 h. After washing with PBS-T, cells were incubated with goat peroxidase-labeled antibody against mouse IgG (1:2,000; KPL) at 37°C for 2 h. Cells were washed with PBS-T six times; subsequently, 3,3′,5,5′-tetramethylbenzidine substrate was added to detect viral antigen, and absorbance was measured at 450 nm (A450). Wells displaying a 2-fold increase of absorbance relative to cell-only wells were positive for virus antigen, and the TCID50 of virus was calculated from these data. To perform microNT ELISA, serum was heat inactivated at 56°C for 30 min and then serially diluted. We added 100 TCID50 of virus to the diluted sera, incubated the mixture for 2 h at 37°C, and then transferred the mixture to seeded RD cells for a 1-day incubation. Viral antigen was detected by ELISA (see above), and the neutralizing endpoint was ascertained by 50% specific signal (X) calculation and expressed as a reciprocal of the highest serum dilution with an A450 value of less than X, where X = [(average A450 of virus control wells) − (average A450 of cell control wells)]/2 + (average A450 of cell control wells). Neutralization titers are shown as the geometric means of the duplicate measurements. Sera were randomized to prevent experimental bias. As limited sera were available from infant or children patients, the analyzed serum-virus pairs were selected according to the necessity for antigenic cartography analysis.
Antigenic cartography.
Tabular neutralization data were analyzed with antigenic cartography as detailed previously (15, 23–26). Briefly, antigenic cartography is a method to visualize and increase the resolution of binding assay data, including microneutralization results. In an antigenic map, the distance between serum point S and antigen point A corresponds to the difference between the log2 of the maximum titer observed for this serum S against any antigen and the log2 of the titer for serum S and antigen A. Thus, each titer in a neutralization assay table can be viewed as specifying a target distance for the points in an antigenic map. Modified multidimensional scaling methods serve to arrange the antigen and serum points in an antigenic map to satisfy target distances specified by neutralization data, yielding a map in which the antigenic distance between points represents antigenic distance as measured in the binding assay. If the maximum neutralization value for each serum was below 1,024, this value was used as the maximum titer (the column basis), with the aim of partially correcting for the absence of homologous viruses for some sera.
Virus binding assay.
ELISA was used to evaluate the binding ability of each virus, as previously described (21). Briefly, 2 × 105 PFU of EV-A71 mutants was added to RD cells at a multiplicity of infection (MOI) of 10 at 37°C. Unbound virus was washed out of cells with PBS before the cells were fixed with 80% acetone and stained with monoclonal antibody against EV-A71 (MAb 979; Millipore) and peroxidase-conjugated goat antibody to mouse IgG (Cell Signaling) for detection at 37°C.
Nucleotide sequences accession numbers.
Complete sequences of the eight viruses constructed with reverse genetics have been deposited in the GenBank database under accession numbers KT354866 to KT354875.
RESULTS
Genetic variations at positions 98, 145, and 164 on VP1 are critical determinants for antigenic properties.
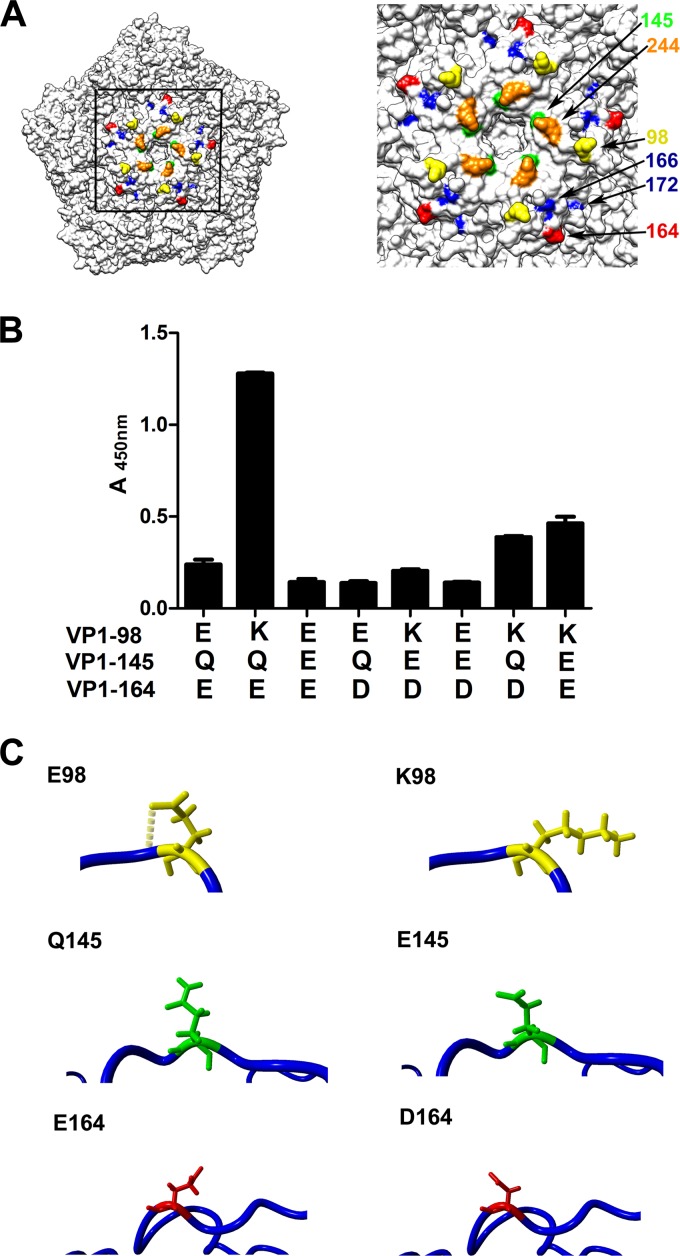
We previously reported the reemergence of genotype B5 in 2008, with antigenic properties different from genotypes B1 and B4 or C (15). To determine the genetic base of these antigenic changes, we compared the B5 and B4 amino acid sequences available in GenBank for the external capsid proteins, the proteins that are thought to determine viral antigenicity. Amino acid sequences of the capsid region were identical for genotypes B4 and B5, except for amino acid variations at position 177 of the VP2 protein (VP2-177) and positions 98, 145, and 164 of the VP1 protein (VP1-98, VP1-145, VP1-164) (available upon request). We mapped these positions on the EV-A71 crystal structure (27) and found that residues VP1-98, VP1-145, and VP1-164, but not VP2-177, were located on the virion external surface (Fig. 1A).
FIG 1.
VP1 mutations changed the viral antigenicity and cell binding ability of EV-A71. (A) Locations of key substitutions on the EV-A71 capsid pentamer. The external surface of the EV-A71 capsid pentamer is shown, using the UCSF Chimera program version 1.9 (26). The antigenic determinants VP1-98 (yellow), VP1-145 (green), and VP1-164 (red) and previously identified receptor binding sites of PSGL-1 (orange, VP1-244) and SCARB2 (blue, VP1-166 and VP1-172) are highlighted. (B) Assessing the binding ability of mutant viruses. The abilities of the different mutant EV-A71 viruses (containing indicated substitutions in VP1-98, VP1-145, and VP1-164) to bind RD cells were measured with the virus absorption assay. ELISA was used to evaluate the binding ability of each virus, as previously described (21). (C) Modeling amino acid structures of the VP1 mutations. The amino acid structures of substitutions at positions 98, 145, and 164 of VP1 were homology modeled based on the EV-A71 protein structure 4AED using FoldX (27) and displayed by the program YASARA (28). The side chains of the indicated amino acid residues are shown, and hydrogen bonds are displayed as yellow dashed lines.
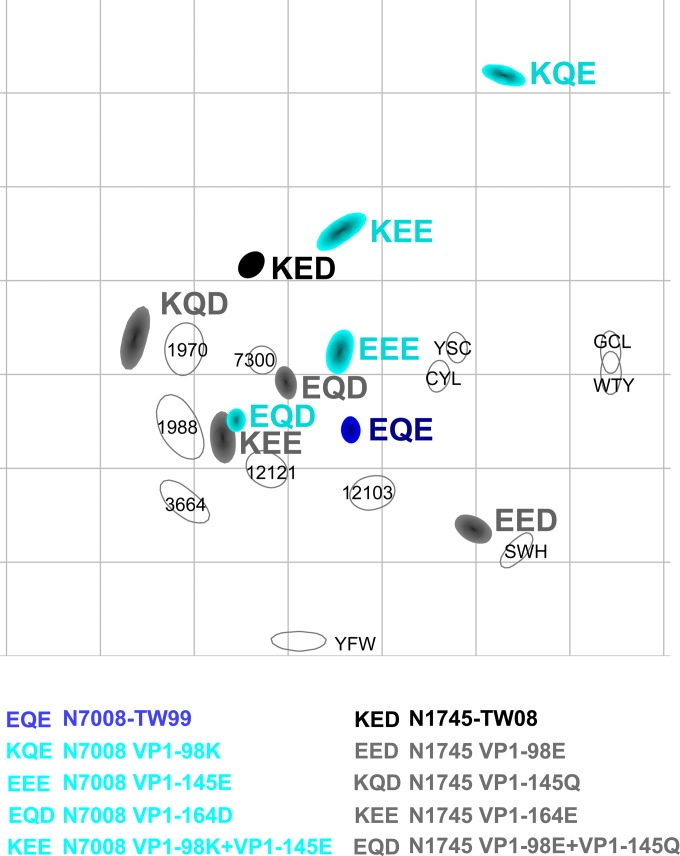
To characterize the impact of residues at positions 98, 145, and 164 on VP1 on the viral antigenic properties, we identified two strains, N1745-TW08 (genotype B5) and N7008-TW99 (genotype B4), that contained VP2, VP3, and VP4 capsid protein sequences that were identical except for these three VP1 residues. We used three amino acid abbreviations to create a shorthand notation representing the sequential amino acids at these three positions, e.g., KQE for VP1-98K, VP1-145Q, and VP1-164E (Table 1). By creating cDNA clones of the two representative strains, N1745-TW08 and N7008-TW99, and introducing mutations into these clones, we obtained a series of mutant cDNA clones, each carrying a different combination of mutations. The antigenic properties of these mutant viruses were assessed by performing neutralization assays of the viruses against serum samples from hospitalized children and healthy, seropositive adults. To interpret the table of neutralization titers (Table 1), an antigenic map was constructed using antigenic cartography (15) (Fig. 2). In this two-dimensional antigenic map, viruses and antisera are positioned such that the distance between any strain and antiserum in the map represents the corresponding neutralization assay measurement, and the size and shape represent the confidence area of this positioning. All mutant viruses but KQE are closely located in a cluster on the antigenic map (Fig. 2). These mutants were within an antigenic distance of 0.24 to 4.14 antigenic units from each other (Table 2), as a result of their similar antigenic properties. To investigate the influence of variation in genomic regions other than the capsid proteins on neutralization, we had two different versions of mutant KEE with identical sequences in the capsid protein coding region: N7008 VP1-98K+VP1-145E (KEE, cyan) and N1745 VP1-164E (KEE, gray), and similarly two different versions of EQD: N7008 VP1-164D (EQD, cyan) and N1745 VP1-98E+VP1-145Q (EQD, gray) (Table 1 and Fig. 2). Only slight changes in the positions on the antigenic map for these two KEE and EQD mutants with divergent genomic backgrounds were observed (26-amino-acid [1.18%] difference between N7008-TW99 and N1745-TW08), not exceeding the intrinsic variability of the assay measurements. This implies that the influence of the viral genome outside the capsid protein coding region on the antigenic properties of the virus is small.
TABLE 1.
Neutralization titers from patients' and healthy donors' sera against VP1 mutant viruses
| Amino acid abbreviationsa | Virus | Neutralization titers of sera from: |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patientsb |
Healthy donors |
||||||||||||
| B5 |
B4 |
C4 |
C2 |
SWH | YFW | GCL | WTY | CYL | YSC | ||||
| 12121 | 12103 | 3664 | 7309 | 1988 | 1970 | ||||||||
| KED | N1745-TW08 | 1,024 | 128 | 1,024 | —c | 128 | 512 | 64 | 64 | 64 | 128 | 256 | |
| EED | N1745-TW08 VP1-K98E | 4,096 | 1,024 | 2,048 | 2,048 | 256 | 256 | 128 | 256 | 512 | |||
| KQD | N1745-TW08 VP1-E145Q | 128 | 32 | 32 | 32 | 128 | 128 | ||||||
| KEE | N1745-TW08 VP1-D164E | 512 | 128 | 64 | 64 | 256 | 128 | ||||||
| EQD | N1745-TW08 VP1-K98E+E145Q | 4,096 | 512 | 2,048 | 2,048 | 128 | 128 | 64 | 256 | 256 | |||
| EQE | N7008-TW99 | 8,192 | 2,048 | 2,048 | 4,096 | 256 | 1,024 | 1,024 | 128 | 128 | 128 | 512 | 512 |
| KQE | N7008-TW99 VP1-E98K | 128 | 64 | 128 | 512 | 512 | 256 | 16 | 128 | 64 | 128 | 256 | |
| EEE | N7008-TW99 VP1-Q145E | 1,024 | 128 | 128 | 128 | 512 | 512 | ||||||
| EQD | N7008-TW99 VP1-E164D | 8,192 | 512 | 4,096 | 8,192 | 8,192 | 2,048 | 128 | 32 | 128 | 256 | 128 | |
| KEE | N7008-TW99 VP1-E98K+Q145E | 256 | 512 | 64 | 128 | 128 | 256 | 256 | |||||
The amino acid abbreviations indicate the residues of VP1-98, VP1-145, VP1-164 in the mutant virus.
Sera collected from patients infected with various genotypes of EV-A71.
As limited sera were available from infant or children patients, the analyzed serum-virus pairs were selected according to the necessity for antigenic cartography analysis.
FIG 2.
Antigenic map of EV-A71 mutant viruses. Antigenic cartography displays the antigenic properties of EV-A71 viruses with various substitutions at VP1-98, VP1-145, and VP1-164. The viruses are shown in color and the antisera as open shapes. Distances between each mutant and antiserum on the map represent the corresponding neutralization assay titer, as described previously (15). The size and shape of each antiserum and virus represent the confidence area in the placement of the antiserum or virus. Both the vertical and horizontal dimensions represent antigenic distance; only the relative positions of antigens and antisera can be determined, i.e., the map can be freely rotated. Each grid line represents a unit of antigenic distance, corresponding to a 2-fold dilution of antiserum in the neutralization table.
TABLE 2.
Antigenic distance between the EV-A71 mutants in the antigenic map
| Mutanta | Antigenic distancec from mutant: |
||||||
|---|---|---|---|---|---|---|---|
| EQDb | EEE | KQD | KEEb | KED | EED | KQE | |
| EQE | 1.227 | 0.836 | 2.501 | 1.364 | 2.055 | 1.680 | 4.116 |
| EQD | 1.316 | 1.388 | 0.238 | 1.664 | 2.783 | 4.651 | |
| EEE | 2.186 | 1.540 | 1.323 | 2.364 | 3.434 | ||
| KQD | 1.420 | 1.472 | 4.142 | 4.831 | |||
| KEE | 1.873 | 2.839 | 4.889 | ||||
| KED | 3.678 | 4.116 | |||||
| EED | 4.847 | ||||||
Amino acid abbreviations indicate the amino acid residues in VP1-98, VP1-145, and VP1-164, respectively.
EQD indicates the antigenic distance of virus N7008-TW99 VP1-E164D, and KEE indicates the antigenic distance of virus N1745-TW08 VP1-D164E.
Units of antigenic distance; each unit corresponds to a 2-fold dilution of antiserum in the neutralization table.
Interestingly, the KQE mutant was not located in this cluster. The KQE mutant was located at a distance of 3.43 from the closest strain in the cluster (maximum distance, 4.89). This mutant has the lowest neutralization titers against all hospitalized children's antisera (Table 1); however, when the titers were raised to investigate avidity, the virus stayed in approximately the same position, moving not more than one antigenic unit toward the main cluster. These results therefore highlight divergent antigenic traits and a potential for neutralization reduction of KQE viruses. The mutants that differed in one position from KQE, namely, EQE, KEE, and KQD were located in the main antigenic cluster, and this confirmed that all three mutations are involved in determining the antigenic properties of EV-A71. These results suggest that genetic variations in the VP1-98, VP1-145, and VP1-164 residues cooperatively cause antigenic changes of EV-A71, and none of the single mutations are individually responsible for such antigenic change.
Antigenically relevant positions on VP1 are next to identified receptor binding sites.
It was previously shown that the VP1 protein contains binding residues for the identified cellular receptors PSGL-1 and SCARB2 (4, 5). To gain insight into the effects on virus binding of the three antigenically relevant VP1 positions, we assessed the binding ability of the eight mutant viruses to RD cells. The binding ability of these eight mutant viruses in RD cells varied widely (Fig. 1B). The KQE mutant, which displayed antigenically different properties on the antigenic map (Fig. 2), had a substantially higher binding ability to RD cells than the other viruses/mutants. Similar to the effects of the VP1 substitutions on viral antigenic properties, where none of these VP1-98, VP1-145, or VP1-164 mutations independently affected the antigenicity, it appeared that the three mutations cooperatively affected the increases and decreases in binding ability to cells. We thus found that in addition to the antigenic properties of the KQE mutant resulting in neutralization reduction from patients' antisera, this mutant displays increased binding ability to cells.
Virus substitutions near the receptor binding site of influenza virus have been shown to be the main cause of antigenic evolution in this virus (28). The EV-A71 crystal structure similarly reveals that the antigenically important VP1-145 and VP1-164 residues are located adjacent to the identified PSGL-1 and SCARB2 receptor binding residues (Fig. 1A). Residue VP1-145 is located in the DE loop on the virion surface, in close contact with residue VP1-244 on the HI loop, which is essential for virus binding to the PSGL-1 receptor (4) (Fig. 1). Residue VP1-98 in the BC loop was previously shown to affect viral replication in RD and Jurkat cells when combined with glutamic acid of VP1-145 (4). The location of residue VP1-164 in the VP1 EF loop is proximal to identified SCARB2 receptor binding residues in the canyon region, especially the receptor binding residue VP1-166 (5).
We next modeled expected protein structure changes resulting from the three VP1 mutations based on the EV-A71 crystal structure (4AED), using FoldX (29). We found that mutation of the VP1-98 and VP1-164 positions caused a rotation of these side chains on the capsid structure (Fig. 1C). The changed orientation of the VP1-98E acidic side chain resulted in the disappearance of a hydrogen bond present for the VP1-98K basic side chain (Fig. 1C). Similarly, mutation of VP1-164 from D to E changed the orientation of the side chain. A mutation of the VP1-145 residue from Q to E, however, elongated the side chain rather than causing a rotation. To determine if these side chain changes affected the stability of the virion structure, free-energy changes (ΔΔG) of the three mutations were calculated with FoldX. Based on the average ΔΔG results, the VP1-Q145E mutation stabilized the virion (average ΔΔG, −0.600466), but the effects of the VP1-E98K and VP1-E164D mutations were small, with average ΔΔGs of 0.258537 and −0.1818, respectively; a ΔΔG of >0 indicates that the mutation is destabilizing, a ΔΔG of <0 indicates that the mutation is stabilizing, and changes exceeding 0.5 kcal/mol are significant (29). In summary, the VP1-145 and VP1-164 residues were located on the exposed virion surface in close proximity to known EV-A71 receptor binding residues. Mutations in these three positions resulted in changes of the orientation or length of the amino acid side chain in the EV-A71 protein structure, which cooperatively influenced viral antigenic properties and cell binding ability.
DISCUSSION
Since the late 20th century, EV-A71 has caused severe outbreaks, notably in the Asia-Pacific region, and has been endemic to this region for years. The phase III clinical trials of one vaccine candidate have finished recently, and this vaccine is likely to be approved in the near future. We wished to address the concern that mutations in EV-A71 might confer a selective advantage to such variants and have increased viral fitness under immune pressure of neutralizing antibodies of vaccinees generated in the vaccine program—leading to immune escape and reduced vaccine efficacy. Using genetic and antigenic analyses, we demonstrated that the amino acids at positions VP1-98, VP1-145, and VP1-164, as antigenic determinants, cooperatively influence the viral antigenic phenotype, using human antiserum samples obtained after natural infection. Interestingly, the KQE mutant showed lower reactivity to all antisera from infected children than did strain N7008-TW99 (EQE), and it also had a 4-fold reduction of neutralization titers against three of six antisera from healthy adults (Table 1). The variation in neutralizing antibody titers in the sera from healthy adults may be a result of different virus exposure histories. Although both infected children and healthy adult antisera consistently reacted to all mutant viruses with neutralization titers above 1:8, antigenic changes of the KQE mutant were clearly observed as reduced reactivity in all tested sera except for serum GCL. In addition to the sera tested from patients and healthy donors, we examined the rabbit anti-EV-A71 (genotype B4, E59 vaccine strain) serum against mutant viruses as well (data not shown). Similar to human antisera, the rabbit antiserum has a 4-fold reduction of neutralization titer against the KQE mutant, indicating that the reduction pattern against the KQE mutant remains the same using either human or rabbit antisera. Future research should investigate whether similar patterns of neutralization reactivity are observed for this mutant when using human antisera of volunteer EV-A71 vaccinees.
Several reports have identified various linear epitopes in the VP1 region (30, 31) as well as in the VP2 and VP3 regions (32). The residues VP1-98 (31) and VP1-164 (32) were located in these identified linear epitopes. Also, positions 145 and 164 on VP1 were in the proximity of previously identified receptor binding determinants, and thus amino acid changes in these residues can plausibly lead to viral structure changes with phenotypic binding alterations. Chen et al. (17) reported that 50 of 83 monoclonal antibodies recognized conformational epitopes with neutralizing activity, suggesting that substitutions on conformational epitopes are the major determinant of neutralizing activity of antisera. As the substitutions VP1-98K, VP1-145Q, and VP1-164E in combination altered the viral antigenic phenotype, we suggest that these residues potentially belong to a single conformational epitope that is recognized by polyclonal antisera, a hypothesis that requires further investigation. Besides the three positions that we described here as influencing the antigenic properties of EV-A71, it is likely that other combinations of substitutions can lead to antigenic changes and low vaccine effectiveness. These may not necessarily change cellular binding but are nonetheless equally important for monitoring vaccine effectiveness and global surveillance of strains, and future studies should target the identification of these locations.
Virus epitopes accumulate mutations in major surface proteins that evade antibody-mediated inhibition, and this antigenic evolution is known as antigenic drift. The evolution of the hemagglutinin (HA) protein of influenza virus, for example, causes sequential antigenic drift over time (33). Koel et al. (28) determined that the antigenic clusters of influenza virus A/H3N2 from 1968 to 2003, where the existing antigenic cluster is consecutively replaced by an emerging cluster, is often based on antigenic change caused mostly by a single substitution (28), located in only seven HA positions peripheral to receptor binding sites. Similar to influenza virus, we showed that two of these three antigenically important locations are in close proximity to known receptor binding residues and that all three positions influenced cell binding ability. Changes of amino acid side chains in these positions might alter both virus-cell interaction and viral antigenicity. Interestingly, among eight constructed mutants, the KQE mutant exhibited the highest cell binding ability and also displayed the lowest neutralization antibody titers when tested against patients' sera. Whether the KQE mutant reduced neutralization by antibody through the increased cell binding ability needs further investigation.
Although enteroviruses rarely display antigenic drift to escape vaccine-mediated immunity (28, 29), they are often observed to have evolving antigenic properties (30). As an example of the importance of mutations in antigenic sites for the evolution of enteroviruses and their implications for the success of vaccine programs, we consider the live attenuated oral poliovirus vaccine (OPV), which is one of the most efficacious and safe vaccines (31). As OPV is genetically unstable, it occasionally evolves into pathogenic vaccine-derived poliovirus (VDPV), where the virus has acquired amino acid alterations in various individual epitopes as an evolutionary response to immunologic pressures on the capsid protein (32). Although the current inactivated poliovirus vaccine and OPV both exhibit high potency against circulating wild-type virus and VDPV in various outbreaks (33) despite their antigenic divergent properties, there is reduced neutralizing antibody against VDPV compared to the wild-type virus. Such lower neutralization titers confer a selective advantage and an increasing viral fitness for antigenic mutant VDPV, which might allow poliomyelitis outbreaks (28, 29). Indeed, the World Health Organization is keen to monitor antigenic changes of poliovirus and recommends to characterize poliovirus isolates in at least one of the standard intratypic differentiation tests (34), including an antigenic test. Therefore, continuous surveillance and the vaccination program have been informed by knowledge of amino acid changes at antigenic determinants in circulating viruses. Because antigenic changes of EV-A71 are similarly thought to frequently occur in naturally circulating viruses (13), our results highlight the importance of monitoring possible antigenic sites for viral antigenicity and in particular identify substitutions at positions 98, 145, and 164 in VP1 as important for the antigenicity of the EV-A71 virus.
When EV-A71 vaccine programs start, the virus may respond to the resulting herd immunity and obtain antibody escape mutations in its capsid protein. Fortunately, such natural isolates containing the KQE mutations are not yet found in the GenBank database, but this does not preclude the possibility that some viruses have already acquired, or future viruses may evolve, substitutions at these antigenic sites, especially when the pressure for herd immunity increases as a result of extensive vaccination programs. This KQE mutant, which indeed is a construct, is a simple intermediate, only 1 or 2 mutations away from two strains that were actually isolated. It is between genotypes already circulating and therefore likely within evolutionary reach. Continuous surveillance of EV-A71 antigenic evolution can forewarn and preempt problems with reduced vaccine effectiveness as a result of mutations at antigenic sites.
To prevent and control disease, it is necessary to identify the antigenic determinants of EV-A71. We systematically characterized the antigenic determinants of EV-A71 with a reverse genetics system and antigenic cartography. We found that positions VP1-145 and VP1-164, near known receptor binding sites, and VP1-98, at which substitution potentially causes a hydrogen bond destruction and which influences viral replication (4), affect the antigenic properties of EV-A71; viruses containing mutations at these three key positions might become predominant and potentially decrease the effectiveness of the protection provided by EV-A71 vaccines. These findings provide important new insights that can be used to ensure the effectiveness of the vaccine and for viral surveillance of emerging and endemic EV-A71 in the future.
ACKNOWLEDGMENTS
This work was financially supported by the Center of Infectious Disease and Signaling Research, National Cheng Kung University, Aim for the Top University Project, Ministry of Education; by a Centers for Disease Control, Ministry of Health and Welfare, grant; by a National Health Research Institute grant; and by Ministry of Science and Technology, Taiwan, grants 101-2321-B-006-027-MY2, 103-2321-B-006-011, and 104-2321-B-006-002. J.M.F. is supported by a Fellowship in Biomedical Informatics from the Medical Research Council UK (MR/K021885/1) and a Junior Research Fellowship from Homerton College, Cambridge, United Kingdom.
We declare that we have no conflicts of interest.
REFERENCES
- 1.Ho M, Chen ER, Hsu KH, Twu SJ, Chen KT, Tsai SF, Wang JR, Shih SR. 1999. An epidemic of enterovirus 71 infection in Taiwan. Taiwan Enterovirus Epidemic Working Group. N Engl J Med 341:929–935. [DOI] [PubMed] [Google Scholar]
- 2.Nishimura Y, Shimojima M, Tano Y, Miyamura T, Wakita T, Shimizu H. 2009. Human P-selectin glycoprotein ligand-1 is a functional receptor for enterovirus 71. Nat Med 15:794–797. doi: 10.1038/nm.1961. [DOI] [PubMed] [Google Scholar]
- 3.Yamayoshi S, Yamashita Y, Li J, Hanagata N, Minowa T, Takemura T, Koike S. 2009. Scavenger receptor B2 is a cellular receptor for enterovirus 71. Nat Med 15:798–801. doi: 10.1038/nm.1992. [DOI] [PubMed] [Google Scholar]
- 4.Nishimura Y, Lee H, Hafenstein S, Kataoka C, Wakita T, Bergelson JM, Shimizu H. 2013. Enterovirus 71 binding to PSGL-1 on leukocytes: VP1-145 acts as a molecular switch to control receptor interaction. PLoS Pathog 9:e1003511. doi: 10.1371/journal.ppat.1003511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen P, Song Z, Qi Y, Feng X, Xu N, Sun Y, Wu X, Yao X, Mao Q, Li X, Dong W, Wan X, Huang N, Shen X, Liang Z, Li W. 2012. Molecular determinants of enterovirus 71 viral entry: cleft around GLN-172 on VP1 protein interacts with variable region on scavenge receptor B 2. J Biol Chem 287:6406–6420. doi: 10.1074/jbc.M111.301622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Foo DG, Alonso S, Phoon MC, Ramachandran NP, Chow VT, Poh CL. 2007. Identification of neutralizing linear epitopes from the VP1 capsid protein of Enterovirus 71 using synthetic peptides. Virus Res 125:61–68. doi: 10.1016/j.virusres.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Foo DG, Ang RX, Alonso S, Chow VT, Quak SH, Poh CL. 2008. Identification of immunodominant VP1 linear epitope of enterovirus 71 (EV71) using synthetic peptides for detecting human anti-EV71 IgG antibodies in Western blots. Clin Microbiol Infect 14:286–288. doi: 10.1111/j.1469-0691.2007.01904.x. [DOI] [PubMed] [Google Scholar]
- 8.Mizuta K, Aoki Y, Suto A, Ootani K, Katsushima N, Itagaki T, Ohmi A, Okamoto M, Nishimura H, Matsuzaki Y, Hongo S, Sugawara K, Shimizu H, Ahiko T. 2009. Cross-antigenicity among EV71 strains from different genogroups isolated in Yamagata, Japan, between 1990 and 2007. Vaccine 27:3153–3158. doi: 10.1016/j.vaccine.2009.03.060. [DOI] [PubMed] [Google Scholar]
- 9.Wu CN, Lin YC, Fann C, Liao NS, Shih SR, Ho MS. 2001. Protection against lethal enterovirus 71 infection in newborn mice by passive immunization with subunit VP1 vaccines and inactivated virus. Vaccine 20:895–904. doi: 10.1016/S0264-410X(01)00385-1. [DOI] [PubMed] [Google Scholar]
- 10.Brown BA, Oberste MS, Alexander JP Jr, Kennett ML, Pallansch MA. 1999. Molecular epidemiology and evolution of enterovirus 71 strains isolated from 1970 to 1998. J Virol 73:9969–9975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McMinn P, Lindsay K, Perera D, Chan HM, Chan KP, Cardosa MJ. 2001. Phylogenetic analysis of enterovirus 71 strains isolated during linked epidemics in Malaysia, Singapore, and Western Australia. J Virol 75:7732–7738. doi: 10.1128/JVI.75.16.7732-7738.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van der Sanden S, van Eek J, Martin DP, van der Avoort H, Vennema H, Koopmans M. 2011. Detection of recombination breakpoints in the genomes of human enterovirus 71 strains isolated in the Netherlands in epidemic and non-epidemic years, 1963-2010. Infect Genet Evol 11:886–894. doi: 10.1016/j.meegid.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 13.Bessaud M, Razafindratsimandresy R, Nougairede A, Joffret ML, Deshpande JM, Dubot-Peres A, Heraud JM, de Lamballerie X, Delpeyroux F, Bailly JL. 2014. Molecular comparison and evolutionary analyses of VP1 nucleotide sequences of new African human enterovirus 71 isolates reveal a wide genetic diversity. PLoS One 9:e90624. doi: 10.1371/journal.pone.0090624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yip CC, Lau SK, Woo PC, Yuen KY. 2013. Human enterovirus 71 epidemics: what's next? Emerg Health Threats J 6:19780. doi: 10.3402/ehtj.v6i0.19780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang SW, Hsu YW, Smith DJ, Kiang D, Tsai HP, Lin KH, Wang SM, Liu CC, Su IJ, Wang JR. 2009. Reemergence of enterovirus 71 in 2008 in Taiwan: dynamics of genetic and antigenic evolution from 1998 to 2008. J Clin Microbiol 47:3653–3662. doi: 10.1128/JCM.00630-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pereira MS, Schild GC. 1971. An antigenic variant of the Hong Kong-68 influenza A 2 virus. J Hyg (Lond) 69:99–103. doi: 10.1017/S0022172400021306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Y, Li C, He D, Cheng T, Ge S, Shih JW, Zhao Q, Chen PJ, Zhang J, Xia N. 2013. Antigenic analysis of divergent genotypes human Enterovirus 71 viruses by a panel of neutralizing monoclonal antibodies: current genotyping of EV71 does not reflect their antigenicity. Vaccine 31:425–430. doi: 10.1016/j.vaccine.2012.10.032. [DOI] [PubMed] [Google Scholar]
- 18.Kung YA, Hung CT, Liu YC, Shih SR. 2014. Update on the development of enterovirus 71 vaccines. Expert Opin Biol Ther 14:1455–1464. doi: 10.1517/14712598.2014.935330. [DOI] [PubMed] [Google Scholar]
- 19.Huang ML, Chiang PS, Chia MY, Luo ST, Chang LY, Lin TY, Ho MS, Lee MS. 2013. Cross-reactive neutralizing antibody responses to enterovirus 71 infections in young children: implications for vaccine development. PLoS Negl Trop Dis 7:e2067. doi: 10.1371/journal.pntd.0002067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mao Q, Li N, Yu X, Yao X, Li F, Lu F, Zhuang H, Liang Z, Wang J. 2012. Antigenicity, animal protective effect and genetic characteristics of candidate vaccine strains of enterovirus 71. Arch Virol 157:37–41. doi: 10.1007/s00705-011-1136-3. [DOI] [PubMed] [Google Scholar]
- 21.Huang SW, Wang YF, Yu CK, Su IJ, Wang JR. 2012. Mutations in VP2 and VP1 capsid proteins increase infectivity and mouse lethality of enterovirus 71 by virus binding and RNA accumulation enhancement. Virology 422:132–143. doi: 10.1016/j.virol.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. 2002. WHO manual on animal influenza diagnosis and surveillance. WHO/CDS/CSR/NCS/2002.5 Rev 1. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 23.de Jong JC, Smith DJ, Lapedes AS, Donatelli I, Campitelli L, Barigazzi G, Van Reeth K, Jones TC, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. 2007. Antigenic and genetic evolution of swine influenza A (H3N2) viruses in Europe. J Virol 81:4315–4322. doi: 10.1128/JVI.02458-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Russell CA, Jones TC, Barr IG, Cox NJ, Garten RJ, Gregory V, Gust ID, Hampson AW, Hay AJ, Hurt AC, de Jong JC, Kelso A, Klimov AI, Kageyama T, Komadina N, Lapedes AS, Lin YP, Mosterin A, Obuchi M, Odagiri T, Osterhaus AD, Rimmelzwaan GF, Shaw MW, Skepner E, Stohr K, Tashiro M, Fouchier RA, Smith DJ. 2008. The global circulation of seasonal influenza A (H3N2) viruses. Science 320:340–346. doi: 10.1126/science.1154137. [DOI] [PubMed] [Google Scholar]
- 25.Russell CA, Jones TC, Barr IG, Cox NJ, Garten RJ, Gregory V, Gust ID, Hampson AW, Hay AJ, Hurt AC, de Jong JC, Kelso A, Klimov AI, Kageyama T, Komadina N, Lapedes AS, Lin YP, Mosterin A, Obuchi M, Odagiri T, Osterhaus AD, Rimmelzwaan GF, Shaw MW, Skepner E, Stohr K, Tashiro M, Fouchier RA, Smith DJ. 2008. Influenza vaccine strain selection and recent studies on the global migration of seasonal influenza viruses. Vaccine 26(Suppl 4):D31–D34. doi: 10.1016/j.vaccine.2008.07.078. [DOI] [PubMed] [Google Scholar]
- 26.Smith DJ, Lapedes AS, de Jong JC, Bestebroer TM, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. 2004. Mapping the antigenic and genetic evolution of influenza virus. Science 305:371–376. doi: 10.1126/science.1097211. [DOI] [PubMed] [Google Scholar]
- 27.Plevka P, Perera R, Cardosa J, Kuhn RJ, Rossmann MG. 2012. Crystal structure of human enterovirus 71. Science 336:1274. doi: 10.1126/science.1218713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koel BF, Burke DF, Bestebroer TM, van der Vliet S, Zondag GC, Vervaet G, Skepner E, Lewis NS, Spronken MI, Russell CA, Eropkin MY, Hurt AC, Barr IG, de Jong JC, Rimmelzwaan GF, Osterhaus AD, Fouchier RA, Smith DJ. 2013. Substitutions near the receptor binding site determine major antigenic change during influenza virus evolution. Science 342:976–979. doi: 10.1126/science.1244730. [DOI] [PubMed] [Google Scholar]
- 29.Schymkowitz JW, Rousseau F, Martins IC, Ferkinghoff-Borg J, Stricher F, Serrano L. 2005. Prediction of water and metal binding sites and their affinities by using the Fold-X force field. Proc Natl Acad Sci U S A 102:10147–10152. doi: 10.1073/pnas.0501980102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu CC, Chou AH, Lien SP, Lin HY, Liu SJ, Chang JY, Guo MS, Chow YH, Yang WS, Chang KH, Sia C, Chong P. 2011. Identification and characterization of a cross-neutralization epitope of Enterovirus 71. Vaccine 29:4362–4372. doi: 10.1016/j.vaccine.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 31.Gao F, Wang YP, Mao QY, Yao X, Liu S, Li FX, Zhu FC, Yang JY, Liang ZL, Lu FM, Wang JZ. 2012. Enterovirus 71 viral capsid protein linear epitopes: identification and characterization. Virol J 9:26. doi: 10.1186/1743-422X-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chow M, Yabrov R, Bittle J, Hogle J, Baltimore D. 1985. Synthetic peptides from four separate regions of the poliovirus type 1 capsid protein VP1 induce neutralizing antibodies. Proc Natl Acad Sci U S A 82:910–914. doi: 10.1073/pnas.82.3.910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barr IG, McCauley J, Cox N, Daniels R, Engelhardt OG, Fukuda K, Grohmann G, Hay A, Kelso A, Klimov A, Odagiri T, Smith D, Russell C, Tashiro M, Webby R, Wood J, Ye Z, Zhang W, Writing Committee of the World Health Organization Consultation on Northern Hemisphere Influenza Vaccine Composition for 2009-2010. 2010. Epidemiological, antigenic and genetic characteristics of seasonal influenza A(H1N1), A(H3N2) and B influenza viruses: basis for the WHO recommendation on the composition of influenza vaccines for use in the 2009-2010 northern hemisphere season. Vaccine 28:1156–1167. doi: 10.1016/j.vaccine.2009.11.043. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization. 2004. Poliovirus laboratory manual, 4th ed. World Health Organization, Geneva, Swizerland. [Google Scholar]