Abstract
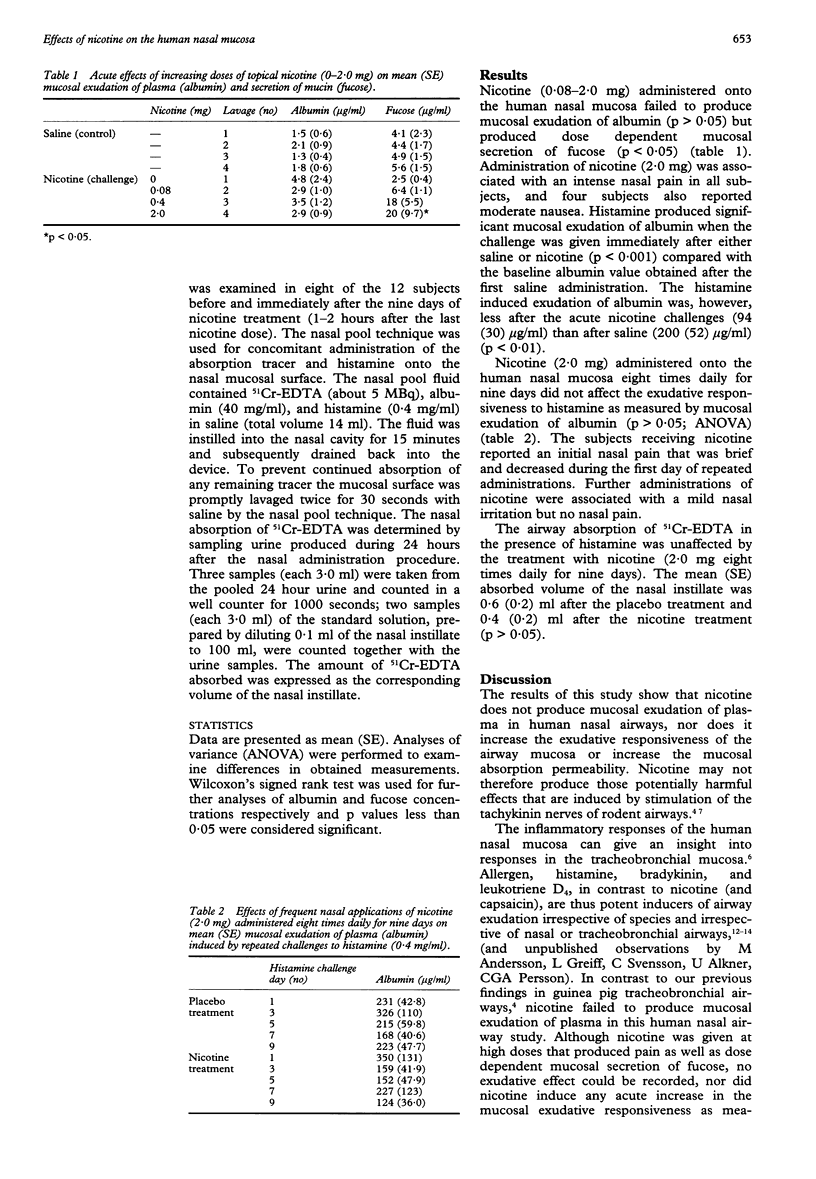
BACKGROUND--Topical application of nicotine and stimulation of tachykinin containing sensory nerves have been shown to produce mucosal exudation of plasma and derangement of the epithelial lining in guinea pig and rat airways. If this occurred in man these effects might contribute to the pathogenesis of airway disease. This study, performed in healthy volunteers without atopy, examined whether nicotine affects the plasma exudation response and the mucosal absorption permeability of the human nasal airway. METHODS--The acute effects of increasing topical doses of nicotine (0.08-2.0 mg) were examined (n = 8) on nasal symptoms (pain), mucosal exudation of plasma (albumin), mucosal secretion of mucin (fucose), and mucosal exudative responsiveness (histamine induced mucosal exudation of albumin). A separate placebo controlled study was carried out to determine whether frequent applications of the high dose of nicotine (2.0 mg given eight times daily for nine days) had any deleterious effects on the airway mucosa detectable as altered responses to histamine challenge. Both mucosal exudation of plasma (n = 12) and mucosal absorption of chromium-51 labelled EDTA (n = 8) were thus examined in nasal airways exposed to both nicotine and histamine. RESULTS--Nicotine caused nasal pain and produced dose dependent mucosal secretion of fucose but failed to produce any mucosal exudation of albumin. The exudative responsiveness to histamine was, indeed, decreased when the challenge was performed immediately after administration of acute doses of nicotine, whereas the responsiveness was unaffected when histamine challenges were carried out during prolonged treatment with nicotine. The nasal mucosal absorption of 51Cr-EDTA in the presence of histamine did not differ between subjects receiving either placebo or nicotine treatment for nine days. CONCLUSIONS--The results indicate that nicotine applied to the human airway mucosa produces pain and secretion of mucin, but inflammatory changes such as mucosal exudation of plasma and epithelial disruption may not be produced. Neurogenic inflammatory responses, which are so readily produced in guinea pig and rat airways, may not occur in human airways.
Full text
PDF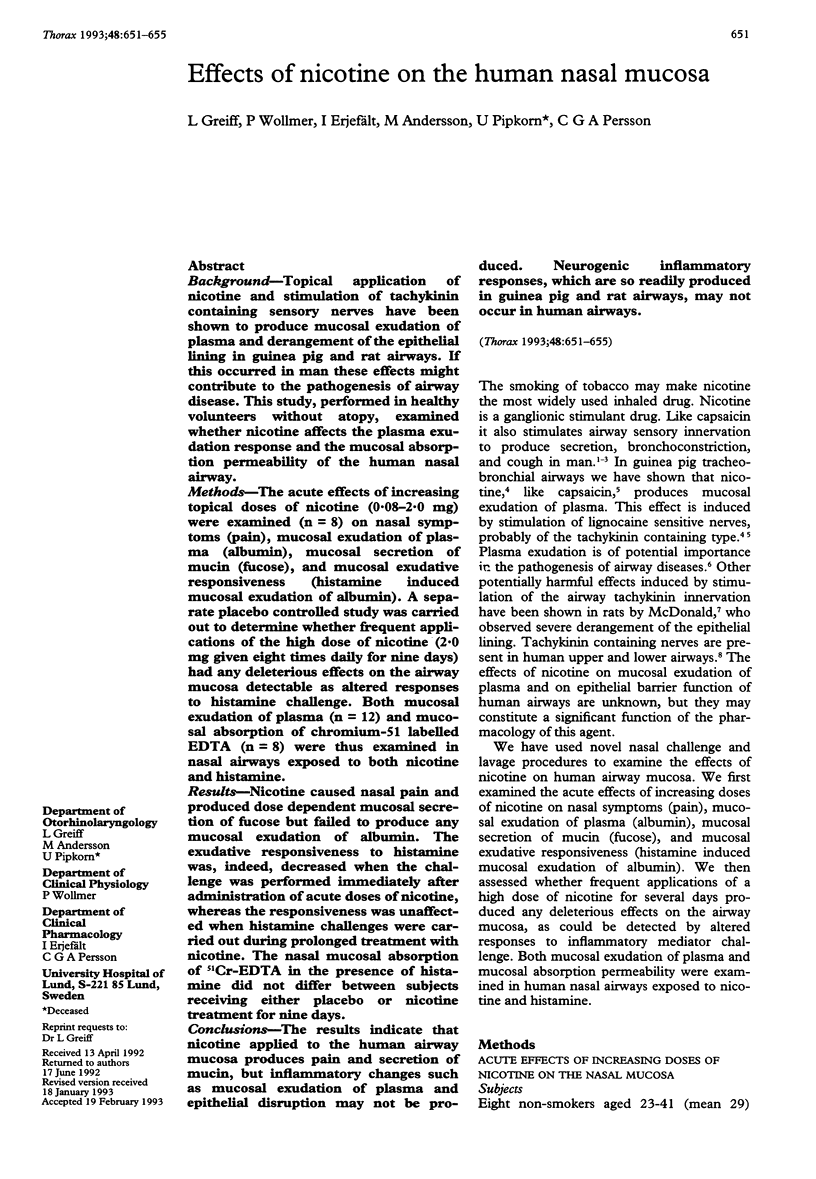

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bascom R., Kagey-Sobotka A., Proud D. Effect of intranasal capsaicin on symptoms and mediator release. J Pharmacol Exp Ther. 1991 Dec;259(3):1323–1327. [PubMed] [Google Scholar]
- Cohenford M. A., Abraham A., Abraham J., Dain J. A. Colorimetric assay for free and bound L-fucose. Anal Biochem. 1989 Feb 15;177(1):172–177. doi: 10.1016/0003-2697(89)90035-3. [DOI] [PubMed] [Google Scholar]
- Erjefält I., Luts A., Persson C. G. Appearance of airway absorption and exudation tracers in guinea pig tracheobronchial lymph nodes. J Appl Physiol (1985) 1993 Feb;74(2):817–824. doi: 10.1152/jappl.1993.74.2.817. [DOI] [PubMed] [Google Scholar]
- Erjefält I., Persson C. G. Inflammatory passage of plasma macromolecules into airway wall and lumen. Pulm Pharmacol. 1989;2(2):93–102. doi: 10.1016/0952-0600(89)90030-6. [DOI] [PubMed] [Google Scholar]
- Geppetti P., Fusco B. M., Marabini S., Maggi C. A., Fanciullacci M., Sicuteri F. Secretion, pain and sneezing induced by the application of capsaicin to the nasal mucosa in man. Br J Pharmacol. 1988 Mar;93(3):509–514. doi: 10.1111/j.1476-5381.1988.tb10305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greiff L., Erjefält I., Wollmer P., Pipkorn U., Persson C. G. Effects of histamine, ethanol, and a detergent on exudation and absorption across guinea pig airway mucosa in vivo. Thorax. 1991 Oct;46(10):700–705. doi: 10.1136/thx.46.10.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greiff L., Pipkorn U., Alkner U., Persson C. G. The 'nasal pool' device applies controlled concentrations of solutes on human nasal airway mucosa and samples its surface exudations/secretions. Clin Exp Allergy. 1990 May;20(3):253–259. doi: 10.1111/j.1365-2222.1990.tb02680.x. [DOI] [PubMed] [Google Scholar]
- Greiff L., Wollmer P., Pipkorn U., Persson C. G. Absorption of 51Cr EDTA across the human nasal airway barriers in the presence of topical histamine. Thorax. 1991 Sep;46(9):630–632. doi: 10.1136/thx.46.9.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafsson B. G., Persson C. G. Asymmetrical effects of increases in hydrostatic pressure on macromolecular movement across the airway mucosa. A study in guinea-pig tracheal tube preparations. Clin Exp Allergy. 1991 Jan;21(1):121–126. doi: 10.1111/j.1365-2222.1991.tb00813.x. [DOI] [PubMed] [Google Scholar]
- Jarvis M. J., Hajek P., Russell M. A., West R. J., Feyerabend C. Nasal nicotine solution as an aid to cigarette withdrawal: a pilot clinical trial. Br J Addict. 1987 Sep;82(9):983–988. doi: 10.1111/j.1360-0443.1987.tb01558.x. [DOI] [PubMed] [Google Scholar]
- Karlsson G., Pipkorn U., Andreasson L. Substance P and human nasal mucociliary activity. Eur J Clin Pharmacol. 1986;30(3):355–357. doi: 10.1007/BF00541544. [DOI] [PubMed] [Google Scholar]
- McDonald D. M. Neurogenic inflammation in the rat trachea. I. Changes in venules, leucocytes and epithelial cells. J Neurocytol. 1988 Oct;17(5):583–603. doi: 10.1007/BF01260988. [DOI] [PubMed] [Google Scholar]
- Miadonna A., Tedeschi A., Leggieri E., Lorini M., Qualizza R., Froldi M., Zanussi C. Activity of substance P on human skin and nasal airways. Ann Allergy. 1988 Sep;61(3):220–223. [PubMed] [Google Scholar]
- Midgren B., Hansson L., Karlsson J. A., Simonsson B. G., Persson C. G. Capsaicin-induced cough in humans. Am Rev Respir Dis. 1992 Aug;146(2):347–351. doi: 10.1164/ajrccm/146.2.347. [DOI] [PubMed] [Google Scholar]
- Persson C. G., Erjefält I., Gustafsson B., Luts A. Subepithelial hydrostatic pressure may regulate plasma exudation across the mucosa. Int Arch Allergy Appl Immunol. 1990;92(2):148–153. doi: 10.1159/000235206. [DOI] [PubMed] [Google Scholar]
- Persson C. G., Erjefält I. Inflammatory leakage of macromolecules from the vascular compartment into the tracheal lumen. Acta Physiol Scand. 1986 Apr;126(4):615–616. doi: 10.1111/j.1748-1716.1986.tb07863.x. [DOI] [PubMed] [Google Scholar]
- Persson C. G., Svensson C., Greiff L., Anderson M., Wollmer P., Alkner U., Erjefält I. The use of the nose to study the inflammatory response of the respiratory tract. Thorax. 1992 Dec;47(12):993–1000. doi: 10.1136/thx.47.12.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raphael G. D., Druce H. M., Baraniuk J. N., Kaliner M. A. Pathophysiology of rhinitis. 1. Assessment of the sources of protein in methacholine-induced nasal secretions. Am Rev Respir Dis. 1988 Aug;138(2):413–420. doi: 10.1164/ajrccm/138.2.413. [DOI] [PubMed] [Google Scholar]
- Salomonsson P., Grönneberg R., Gilljam H., Andersson O., Billing B., Enander I., Alkner U., Persson C. G. Bronchial exudation of bulk plasma at allergen challenge in allergic asthma. Am Rev Respir Dis. 1992 Dec;146(6):1535–1542. doi: 10.1164/ajrccm/146.6.1535. [DOI] [PubMed] [Google Scholar]
- Stjärne P., Lundblad L., Lundberg J. M., Anggård A. Capsaicin and nicotine-sensitive afferent neurones and nasal secretion in healthy human volunteers and in patients with vasomotor rhinitis. Br J Pharmacol. 1989 Mar;96(3):693–701. doi: 10.1111/j.1476-5381.1989.tb11870.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uddman R., Sundler F. Neuropeptides in the airways: a review. Am Rev Respir Dis. 1987 Dec;136(6 Pt 2):S3–S8. doi: 10.1164/ajrccm/136.6_Pt_2.S3. [DOI] [PubMed] [Google Scholar]


