Abstract
Objective
Children diagnosed with autism spectrum disorder (ASD) require substantial support to address not only core ASD symptoms, but also a range of co-occurring conditions. This study explores treatment and service use among children with ASD with and without intellectual disability (ID), and parents’ perception of unmet needs from these treatments.
Methods
Data come from a probability-based national sample of 2,077 children diagnosed with either ASD, ID, or both (ASD and ID). Weighted multivariate logistic regressions examined differences between diagnostic groups for current medication and service utilization with a sub-analysis exploring differences among those with co-occurring psychiatric conditions. Additional modeling examined parents’ perception of unmet needs.
Results
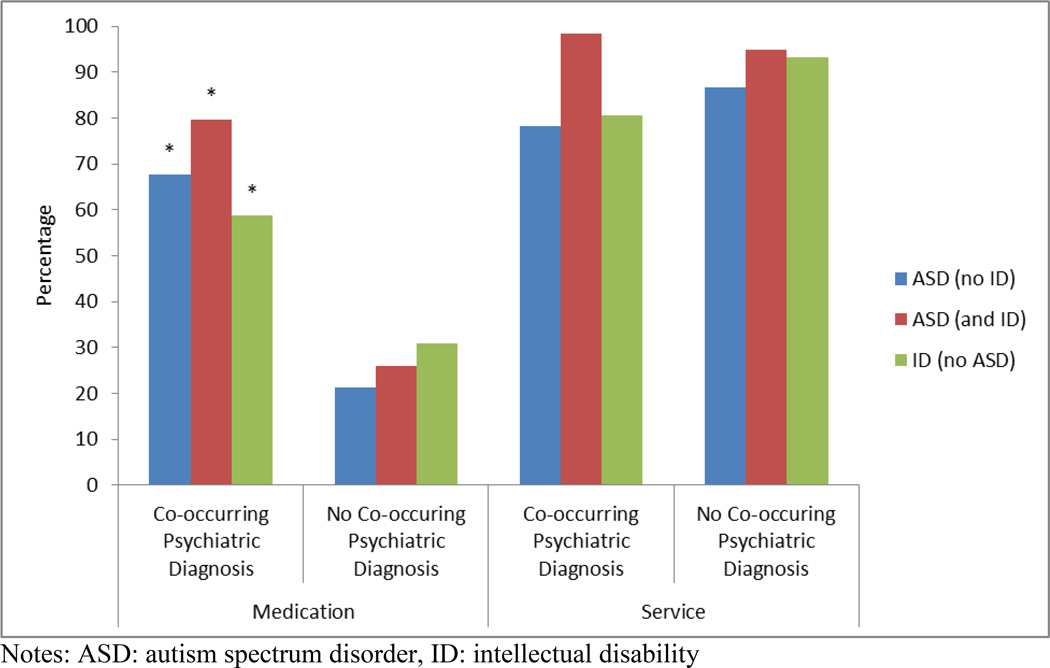
Children diagnosed with ASD and ID were significantly more likely to be receiving current medication and services when compared to children with ID only or ASD only. Children with a co-occurring psychiatric diagnosis, from all 3 diagnostic groups, were more likely to be receiving a current medication, but not more likely to be receiving a current service when compared with children without a co-occurring psychiatric diagnosis. Children with ASD and a co-occurring psychiatric diagnosis were significantly more likely to have parents who reported unmet needs when compared with parents of children with ASD without a co-occurring psychiatric diagnosis.
Conclusions
Children diagnosed with ASD and ID, especially those with a comorbid psychiatric condition, represent a vulnerable population with substantial rates of current service (98%) and medication (67%) usage, but despite these high rates, approximately 30% of parents report that their child’s developmental needs are still not being met by their current treatment and services.
Keywords: Autism Spectrum Disorder, Intellectual Disability, National Surveys
INTRODUCTION
Children diagnosed with autism spectrum disorder (ASD) are characterized by deficits in social communication and interaction, and the presence of stereotyped and repetitive behaviors.1 In addition to a primary ASD diagnosis, co-occurring conditions such as developmental, psychiatric, neurological, and other medical conditions are also common.2–4 It is therefore unsurprising that children diagnosed with an ASD require substantial support to address not only the core symptoms of an ASD but the range of co-occurring conditions and symptoms as well. Previous research has indicated high rates of psychotropic medication use and service use, including school-based services, among children diagnosed with an ASD.5–8 However, only a limited number of studies have delineated how co-occurring conditions, including common conditions such as intellectual disability (ID), are associated with service use. Given that treatments for children with ASD can translate into high costs for families, insurance providers, school districts, and society,9–13 it is also important to better understand the service needs, the patterns of service use, and the adequacy of existing services in meeting the manifold support and intervention needs among a diverse population of children with ASD. In particular, children diagnosed with ASD and ID have been noted to receive an ASD diagnosis earlier than those with ASD only,14 so these children may also receive earlier and different services and treatments than children without ID.15
Variations in how well the needs of children with ASD are being met, and the degree to which their parents are satisfied with the services they receive are poorly understood and may vary by the co-occurring diagnoses of the child. There are several reports of parental dissatisfaction with the diagnostic process for children with ASD,16–17 but little is known about parental satisfaction and perception of unmet needs regarding their child’s treatment.18–19 Previous research highlights parental concern about limitations in specialty medical care, including mental health care, and lack of a medical home among families raising children with an ASD.20–23 These studies, however, do not examine the presence of co-occurring psychiatric conditions, thereby overlooking the heterogeneous nature of children diagnosed with ASD.
This study attempts to address the current gaps in the literature by exploring treatment and service use among a nationally representative and clinically diverse population of children diagnosed with ASD with and without co-occurring psychiatric conditions, with an additional investigation of parents’ perception of whether their child has unmet developmental needs. Children diagnosed with ID without ASD provide an appropriate statistical (and clinical) reference to children diagnosed with both ASD and ID, given the need for significant (and potentially) lifelong support needs for learning and behavioral challenges among children diagnosed with ID.24–26
It is hypothesized that service use and unmet needs would increase as the complexity of the conditions in need of treatment increased. Mainly, (1) children with ASD and ID would have higher rates of medication, service use, and unmet needs than children with ASD only or ID only, and given the potential for additional symptomatology unrelated to ASD requiring treatment, (2) children diagnosed with ASD and a co-occurring psychiatric condition would have higher rates of service and medication use, as well as greater rates of unmet needs, compared to those diagnosed with ASD, but no co-occurring psychiatric condition.
METHODS
Data Source
Data for the current study were retrieved from the 2011 Survey of Pathways to Diagnosis and Services (also known as “Pathways”), a follow-up study to the 2009–2010 National Survey of Children with Special Health Care Needs (NS-CSHCN), a cross-sectional random-digit-dial telephone survey (landlines and cell phones) of US households with at least one child aged 0 to 17 years at the time of interview with special health care needs. Pathways, conducted by the National Center for Health Statistics (NCHS), was a module of the State and Local Area Integrated Telephone Survey (SLAITS), and was sponsored by the National Institute of Mental Health (NIMH) of the National Institutes of Health (NIH) to collect information about the diagnostic experiences of children with special health care needs (CSHCN) aged 6 to 17 years old who were ever diagnosed with autism spectrum disorder (ASD), intellectual disability (ID), and/or developmental delay (DD). Additionally, Pathways was designed to provide information about the current clinical treatment, interventions, and educational services these children receive. The completion rate for the Pathways survey was 62%, which translates into a 16% response rate when incorporating the 26% response rate of the NS-CSHCN. Pathways shares the complex survey design of the NS-CSHCN, with clustering of children within households and stratification by state and sample type (landline or cell phone). More information about both Pathways and the NS-CSHCN including the consent procedures can be found at http://www.cdc.gov/nchs/slaits.htm. Verbal consent was obtained from a parent or guardian respondent at the time of the interview (hereafter referred to as the parent), with respondents being informed of their rights as survey participants. Only one child was sampled from a given household; if more than one child was eligible, one was randomly selected.
Sample
The study sample was restricted to CSHCN with a parent-reported diagnosis of ASD or ID (n=2,077), which included CSHCN diagnosed with ASD only (n=1,117), ASD and ID (n=303), and ID only (n=657). Because children who were diagnosed with either ASD or ID are almost exclusively identified as CSHCN given the need for routine health and related services,27 hereafter we simply identify them as children with ASD or ID. Basic demographics by diagnostic classification appear in Table 1.
Table 1.
Demographics of children diagnosed with autism spectrum disorders or intellectual disabilities
| Total (n=2,077) |
ASD (no ID) (n=1,117) (A) |
ASD (and ID) (n=303) (B) |
ID (no ASD) (n=657) (C) |
Significant comparisons |
|
|---|---|---|---|---|---|
| Child Characteristics (%) | |||||
| Age, yr | |||||
| 6–11 | 50.6 | 56.4 | 48.7 | 42.0 | A>C** |
| 12–17 | 49.4 | 43.6 | 51.3 | 58.0 | |
| Male | 72.2 | 82.6 | 80.5 | 51.4 | A>C***; B>C*** |
| Race/ethnicity | |||||
| Non-Hispanic White | 63.5 | 69.3 | 55.8 | 57.9 | |
| Non-Hispanic Black | 13.3 | 11.0 | 9.6 | 18.7 | |
| Non-Hispanic Other | 10.8 | 8.6 | 15.1 | 12.4† | |
| Hispanic | 12.4 | 11.1 | 19.6 | 11.0 | |
| Current Health Insurance | |||||
| Public | 35.8 | 29.3 | 35.2 | 46.5 | C>A** |
| Private | 61.8 | 68.0 | 63.5 | 50.9 | A>C** |
| Not Insured | 2.4 | 2.7 | 1.3† | 2.6† | |
| Child Clinical Characteristics (%) | |||||
| Depression | 18.5 | 19.3 | 22.7 | 15.1 | |
| Anxiety Problems | 37.5 | 41.1 | 49.0 | 26.1 | A>C**; B>C*** |
| ADHD | 47.8 | 49.4 | 54.6 | 42.0 | |
| Behavioral/Conduct Problems | 29.4 | 30.2 | 43.2 | 21.5 | B>A*; A>C*; B>C*** |
| Any Psychiatric Diagnosis | 64.4 | 67.8 | 76.6 | 53.1 | B>C***; A>C** |
| Household Characteristics (%) | |||||
| Highest Parental Education Level | |||||
| No High School | 8.5 | 7.1 | 7.3† | 11.4 | |
| High School | 17.7 | 13.9 | 23.8 | 21.0 | |
| College or More | 73.8 | 79.0 | 68.9 | 67.6 | |
| Federal Poverty Level | |||||
| < 100% | 21.0 | 16.0 | 20.6 | 29.4 | C>A** |
| 100–199% | 19.6 | 19.4 | 21.1 | 19.1 | |
| 200–399% | 32.1 | 32.6 | 34.6 | 30.2 | |
| ≥ 400% | 27.3 | 32.0 | 23.8 | 21.3 | A>C** |
| Household Structure (%) | |||||
| Two parent household | 66.0 | 71.8 | 66.3 | 56.3 | A>C** |
| Other | 34.0 | 28.2 | 33.7 | 43.7 | |
Notes:
.01≤p<.05
.001≤p<.01
p<.001
ASD: autism spectrum disorder, ID: intellectual disability, ADHD: attention deficit-hyperactivity disorder
Estimates have a relative standard error above 30% and may be unreliable
Measures
Diagnostic criteria
An initial screener question for the Pathways survey asked the parents to confirm whether “a doctor or other health care provider” had ever told them that the child had “autism, Asperger’s Disorder, pervasive developmental disorder, or other autism spectrum disorder”, “any developmental delay that affects [his/her] ability to learn,” or an “intellectual disability or mental retardation.” The parent was subsequently asked whether the diagnosis was current for each confirmed diagnosis. Parents were also asked whether their child has a current co-occurring psychiatric condition (“depression,” “anxiety problems,” “Attention-Deficit Disorder or Attention-Deficit/Hyperactivity Disorder (ADHD),” or “behavioral or conduct problems”). Data on the presence of selected neurodevelopmental conditions (“Down Syndrome,” “Cerebral Palsy,” “epilepsy or seizure disorder,” and “a head injury, concussion, or traumatic brain injury”) were obtained from the NS-CSHCN, because parent report of these diagnoses was not confirmed in Pathways.
Medication and service use
Parents were asked whether their child currently receives various medications and services on a regular basis. Medications were categorized as stimulants, antidepressants, antianxiety or mood stabilizers, antiseizure, antipsychotics, and sleep medications. School and community services included physical therapy, social skills training, occupational therapy, and speech or language therapy. Additional community services included behavioral intervention or modification services, sensory integration therapy, and cognitive based therapy.
Demographics
Child demographics included child’s age, gender, race, ethnicity, and current health insurance coverage status (and type if insured). Household characteristics included income level (recoded as a percentage of the federal poverty level28), educational attainment of the highest educated parent, and family structure (2 biological, adoptive or step parents compared to all other family types).
Unmet needs
The parent was asked whether in the past 12 months their child received “all the treatments and services necessary to meet [his/her] developmental needs” as well as “[saw] all the service providers needed to care for [his/her] developmental needs.” The child’s physical, social, and emotional growth and learning were provided as examples of child development, with unmet developmental needs being present when supports and care were not available or provided.
Statistical Analysis
All estimates were calculated using Stata 12.029 which accounted for the complex survey design. Statistical differences between ASD and ID groups on current treatment use are presented in Table 2. Corrected χ2 tests were used to explore whether a difference exists between the diagnostic groups, with post hoc logistic regressions comparing each diagnostic groups to each other when applicable. Multivariate logistic regressions were run to determine if the use of medication, school-based services, and community-based services differed by diagnostic groups, adjusting for child and household characteristics, including child’s age, gender, race, ethnicity, current health insurance status and type, and the presence of co-occurring medical conditions, as well as the household’s federal poverty level, family structure and the highest level of education attained by a household member (adjusted odds ratios (AORs) are presented).
Table 2.
Prevalence of current medication and services
| Total | ASD (no ID) (A) |
ASD (and ID) (B) |
ID (no ASD) (C) |
Significant comparisons | |
|---|---|---|---|---|---|
| Current Medication (%) | |||||
| Stimulant | 27.4 | 32.6 | 28.3 | 18.7 | A>C*** |
| Anti-depressant | 18.1 | 17.9 | 27.7 | 13.8 | B>C*; B>A* |
| Anti-anxiety or mood stabilizer | 22.7 | 22.8 | 35.5 | 16.4 | B>C**; B>A* |
| Anti-psychotic | 11.8 | 12.2 | 20.4 | 7.1† | B>C** |
| Anti-seizure | 11.2 | 5.4 | 17.6 | 17.4 | B>A***; C>A*** |
| Sleep | 16.6 | 18.0 | 22.5 | 11.6 | |
| Any medication class | 52.6 | 52.7 | 66.9 | 45.7 | B>A**; B>C** |
| Two or more classes | 28.5 | 30.3 | 36.7 | 21.9 | B>C* |
| Community-based Services (%) | |||||
| Behavioral modification | 33.1 | 38.2 | 44.4 | 19.4 | B>C***; A>C*** |
| Sensory integration | 17.9 | 17.8 | 28.3 | 12.5 | B>A*; B>C** |
| Cognitive behavioral | 27.8 | 23.1 | 42.9 | 28.4 | B>A***; B>C* |
| Occupational therapy | 11.4 | 10.5 | 12.3 | 12.6 | |
| Physical therapy | 7.6 | 3.9 | 10.1† | 12.2 | B>A*; C>A*** |
| Social skills training | 21.4 | 24.4 | 23.5 | 15.7 | |
| Speech language therapy | 13.0 | 12.3 | 21.3 | 10.2 | B>A*; B>C** |
| Any community -based service | 62.8 | 61.7 | 72.2 | 59.9 | |
| School-based Services (%) | |||||
| Occupational therapy | 41.7 | 33.7 | 51.7 | 49.9 | B>A**; C>A** |
| Physical therapy | 18.6 | 10.8 | 27.3 | 27.0 | B>A***; C>A*** |
| Social skills training | 46.6 | 46.5 | 60.3 | 40.5 | B>A*; B>C** |
| Speech language therapy | 56.0 | 47.0 | 78.1 | 60.0 | B>C**; C>A**; B>A*** |
| Any school-based service | 74.4 | 66.8 | 93.4 | 77.8 | B>C***; C>A**; B>A*** |
| Total services (%) | |||||
| Any service | 85.3 | 81.0 | 97.7 | 86.3 | B>A***; B>C*** |
| Two or more services | 68.8 | 62.6 | 82.4 | 73.0 | B>A***; C>A* |
Notes:
.01≤p<.05
.001≤p<.01
p<.001
ASD: autism spectrum disorder, ID: intellectual disability, ADHD: attention deficit-hyperactivity disorder
Estimates have a relative standard error 30% or greater (but less than 50%) and may be unreliable
Additional multivariate logistic regressions compared service and treatment use based on the presence of co-occurring psychiatric conditions (depression, anxiety problems, ADHD and conduct or behavioral problems) for each diagnostic group. A final series of multivariate logistic regressions compared the views of parents of children with ASD regarding whether the developmental needs of their child were being met. All models were adjusted for child and household demographics and are presented as AORs.
RESULTS
Table 1 presents demographics estimates of the population subdivided by diagnosis. Overall, children with autism spectrum disorder (ASD) or intellectual disability (ID) were primarily male (72.2%), currently insured (97.6%), and living in households with a highly educated parent (73.8%) having attended some or more college. Children diagnosed with ASD and ID (80.5%) or with ASD only (82.6%) were more likely to be male than children with ID only (51.4%). Children diagnosed with ASD only were more likely to live in two-parent households and were younger than children with ID only.
Co-occurring psychiatric diagnoses were common (64.4%). Children diagnosed with ASD and ID (76.6%) and ASD only (67.8%) had higher rates than children with ID only (53.1%). Children with ID only were the least likely to have behavioral or conduct problems or anxiety problems. Children diagnosed with ASD and ID were the most likely to have behavioral or conduct problems.
Table 2 highlights the percentage of children currently receiving specific treatments and services, again subdivided by diagnosis. Children with both ASD and ID were the most likely to be receiving services for their condition when compared with children with ASD only (OR=9.85, 95% CI: 4.14–23.40, p<.001) or ID only (OR=6.67, 95% CI: 2.61–17.03, p<.001). They were also more likely to be receiving medication compared with children with ASD only (OR=1.81, 95% CI: 1.17–2.82, p<.01) or ID only (OR=2.40, 95% CI: 1.44–4.03, p<.01). Children with ASD and ID were more likely to be receiving antidepressants, antipsychotics, and antianxiety or mood stabilizers when compared to children with ID only, and they were more likely to be receiving antiseizure medications, antidepressants and antianxiety or mood stabilizers than children with ASD only. Children diagnosed with ASD only were more likely to be receiving stimulants than children with ID only.
Children diagnosed with ASD and ID had the highest current use of school-based social skills training and speech language therapy, and the highest current use of community-based sensory integration services, cognitive behavioral services, and speech language therapy. Children with ID only were less likely to be receiving behavioral modification services compared to children with both ASD and ID or children with ASD only.
Multivariate logistic regressions adjusting for child and household demographics revealed that children with both ASD and ID were receiving more intervention services than children in the other two diagnostic categories. More specifically, children with ASD and ID were more likely to be receiving current medication (AOR=2.54, 95% CI: 1.37–4.71, p<.01) and current services (AOR=7.73, 95% CI: 2.81–21.24, p<.001) than children with ID only. They were also more likely to be receiving current medication (AOR=2.08, 95% CI: 1.23–3.53, p<.01) and current services (AOR=8.87, 95% CI: 3.76–20.92, p<.001) than children with ASD only. Additionally, children diagnosed with ASD and ID were more likely to currently be receiving 2 or more classes of medication than children with ID only (AOR=2.18, 95% CI: 1.17–4.03, p<.05), and 2 or more current services than children with ID only (AOR=2.19, 95% CI: 1.09–4.39, p<.05) or ASD only (AOR=2.50, 95% CI: 1.29–4.83, p<.01). Finally, children diagnosed with ASD and ID were more likely to be receiving services in the school and in the community concurrently when compared to children with ID only (AOR=2.32, 95% CI: 1.30–4.12, p<.01) or ASD only (AOR=1.89, 95% CI: 1.15–3.10, p<.05).
The percentages of children receiving any current medication or service are displayed in Figure 1, which further divides the diagnostic groups into children with and without a current co-occurring psychiatric diagnosis of depression, anxiety problems, attention-deficit/hyperactivity disorder (ADHD), or behavioral or conduct problems. Across diagnostic categories, children with a co-occurring psychiatric diagnosis were more likely to be receiving medication than children without a psychiatric diagnosis, after adjusting for child and household demographics. However, children with a co-occurring diagnosis were not more likely to be receiving current services within each diagnostic group. When examining all current diagnoses (including co-occurring psychiatric conditions and diagnostic classification), ID (AOR=1.75, 95% CI: 1.01–3.03, p<.05), anxiety problems (AOR=3.13, 95% CI: 2.05–4.77, p<.001) and ADHD (AOR=4.83, 95% CI: 3.17–7.35, p<.001) were significantly associated with current medication use (Table 3). In contrast, current ASD (AOR=7.86, 95% CI: 2.78–22.24, p<.001) and current ID (AOR=9.22, 95% CI: 3.82–22.25, p<.001) diagnoses – but no psychiatric diagnoses – were significantly associated with service use.
Figure 1.
Prevalence of medication and service use, by presence of a co-occurring psychiatric diagnosis
Notes: ASD: autism spectrum disorder, ID: intellectual disability
* Indicates significant differences in prevalence estimates (p<.05) between children with and without psychiatric comorbidity for a given diagnosis
Co-occurring psychiatric diagnoses include ADHD, depression, anxiety problems, and conduct and behavioral problems
Table 3.
Associations between current diagnoses and current service and medication use
| Current diagnosis | Service use AOR (95% CI) |
Medication use AOR (95% CI) |
|---|---|---|
| Autism spectrum disorder | 7.86*** (2.78–22.24) |
1.96 (0.99–3.88) |
| Intellectual disability | 9.22*** (3.82–22.25) |
1.75* (1.01–3.03) |
| Depression | 0.65 (0.34–1.23) |
1.51 (0.75–3.05) |
| Anxiety problems | 0.97 (0.59–1.60) |
3.13*** (2.05–4.77) |
| ADHD | 0.67 (0.43–1.06) |
4.83*** (3.17–7.35) |
| Conduct or behavioral problems | 1.12 (0.60–2.10) |
1.39 (0.82–2.35) |
Notes:
.001≤p<.05
p<.001
ADHD: Attention-Deficit/Hyperactivity Disorder, AOR: adjusted odds ratio, CI: confidence interval
Odds ratios are adjusted by child and family demographics.
Finally, multivariate logistic regressions examined parental views on whether their child’s developmental needs were being met among children diagnosed with ASD (Table 4). Children with an ASD and a co-occurring psychiatric diagnosis were significantly more likely to have unmet treatment and service needs (AOR=2.36, 95% CI: 1.46–3.81, p<.001) and provider needs (AOR=1.87, 95% CI: 1.11–3.13, p<.05) for their child’s development when compared with children with ASD without a co-occurring psychiatric diagnosis.
Table 4.
Prevalence of unmet developmental needs for treatment and services and providers by the presence of a co-occurring psychiatric condition
| Group | Co-occurring Psychiatric Condition |
Prevalence of Unmet Needs for Treatment and Services |
Adjusted Odds Ratio (95% CI) |
Prevalence of Unmet Needs for Providers |
Adjusted Odds Ratio (95% CI) |
|---|---|---|---|---|---|
| ASD (with or without ID) | Total | 29.0 | 2.36*** (1.46–3.81) |
22.7 | 1.87* (1.11–3.13) |
| Yes | 32.5a | 24.8b | |||
| No | 21.0 | 17.8 | |||
Notes:
.001≤p<.05
p<.001
ASD: autism spectrum disorder, ID: intellectual disability, CI: confidence interval
The prevalence of unmet needs for treatment and services for children diagnosed with an ASD and ID and a co-occurring psychiatric condition was 29.0% compared to 33.6% for children diagnosed with ASD without ID.
The prevalence of unmet needs for providers for children diagnosed with an ASD and ID and a co-occurring psychiatric condition was 21.0% compared to 26.0% for children diagnosed with ASD without ID.
Odds ratios are adjusted by child and family demographics.
DISCUSSION
In this study, children with special health care needs who were diagnosed with either autism spectrum disorder (ASD), intellectual disability (ID), or both conditions had high rates of medication and service use, with the highest rates found for children with combined ASD and ID diagnoses. Of the total sample, 52.6% of children were currently receiving at least one class of medication, whereas 66.9% of children diagnosed with both ASD and ID were receiving at least one class of medication. A similar finding was found for service use, with virtually all children diagnosed with an ASD and ID receiving at least one current service (97.7%), compared with 81.0% of children with ASD only and 86.3% of children with ID only. In adjusted models, these differences were significant; children with ASD and ID were more likely to be receiving current medication and services compared with children with ASD only and ID only. Among children diagnosed with ASD only, 66.8% were receiving specialized school-based intervention services compared with 93.4% of children diagnosed with ASD and ID. Community-based services were also common within this population, with 61.7% of children with ASD only receiving these services compared with 72.2% of children with ASD with ID. The combined rates among those children diagnosed with ASD, be they ASD and ID or ASD only, are similar to other studies of medication use and use of community-based services.30–32
Children diagnosed with ASD (with or without ID) who had a co-occurring psychiatric diagnosis were more likely to be receiving medication, a finding that is supported by previous research with a national registry of children with ASD.33 Medication use was related to the presence of a co-occurring psychiatric diagnosis, but not to the presence of ASD, with anxiety and ADHD being significant predictors of medication use. In contrast, psychiatric diagnoses were not associated with current service use; rather, service use was related to the child’s ASD or ID diagnosis. It is possible that this finding reflects the efficacious of medications for ADHD and anxiety, but not necessarily for ASD, where behavioral therapy may be more appropriate.34–35
Finally, children with ASD (with or without ID) and co-occurring psychiatric conditions, when compared to children with ASD and no psychiatric conditions, were more likely to have unmet developmental needs – both in terms of receiving all necessary treatment and services as well as in seeing all necessary providers. A previous national survey found that children diagnosed with ASD were more likely to have unmet needs when compared with children with other special health care needs,36 but the study did not evaluate the presence of co-occurring psychiatric conditions among children with ASD.
The high rate of unmet needs despite high service usage warrants a further investigation. There has been noted variability in the structure of community early intervention programs37 and the availability of specialists38 which could factor into the quality of the services received. It is also possible that a parent’s perception of whether their child’s developmental needs are being met may be influenced by a parent’s belief of what services can and should accomplish for their child, and could be based on unrealistic expectations. Unfortunately, data were not available in this study to evaluate parental expectations nor the quality of services received.
Limitations
The current study uses a large probability based national sample of children with ASD, perhaps the largest available to date. The large sample size allows for subanalysis between children with and without ID, as well as with or without a comorbid psychiatric condition. Despite these strengths, the study needs to be viewed in light of its limitations. Pathways was a cross-sectional parent-reported survey; thus it is not possible to determine the directionality of associations or the existence of causality. Although efforts were made to collect data regarding the most common psychiatric diagnoses, it is not possible to rule out unmeasured confounding for nonreported disorders and conditions that could increase a child’s use of medication or services. Moreover, estimates based on telephone surveys with low response rates may be unreliable due to selection biases resulting from sampling, nonresponse, lack of coverage of households without telephones, and respondent classification and reporting errors (due perhaps to a lack of clinical validation of conditions which parents believed their children to still have and the broad terminology of some conditions used in the survey). The impact of these potential biases on the results presented in the study is unknowable. Therefore, the representativeness of the estimates (which are limited to children aged 6 to 17) cannot be confirmed because biases may remain that are not related to known demographics. However, sample weights were adjusted to account for known demographic correlates of nonresponse and were calculated in accordance with best practices for sample surveys.
Implications
Given the multiple developmental, emotional, and behavioral issues that children with ASD and co-occurring psychiatric conditions have, it is perhaps unsurprising that these children have a higher proportion of unmet developmental needs, both with treatment and services (32.5%) and providers (24.8%). Psychiatric disorders, as well as the presence of ID, are prevalent among children diagnosed with an ASD; other studies have found rates as high as 70%, with approximately 30% of children being diagnosed with ADHD and anxiety disorders.3 These estimates coincide with the overall prevalence of co-occurring psychiatric diagnoses found in the present study. These findings suggest that children with ASD and co-occurring psychiatric diagnoses, as well as those with ID, who use the highest rates of services and treatments, represent a unique subpopulation that may be in need of further service and treatment options that address these children’s distinct behavioral and emotional challenges.39
Footnotes
Conflicts of Interest and Source of Funding: The authors have no financial relationships relevant to this article to disclose. The authors have no conflicts of interest to disclose.
Disclaimer: The findings and conclusions in this paper are those of the authors are do not necessarily represent the views of the Centers for Disease Control and Prevention, the National Institute of Mental Health, or the Maternal and Child Health Bureau.
Contributor Information
Benjamin Zablotsky, National Center for Health Statistics, Hyattsville, MD.
Beverly A. Pringle, National Institute of Mental Health, Bethesda, MD.
Lisa J. Colpe, National Institute of Mental Health, Bethesda, MD.
Michael D. Kogan, Maternal and Child Health Bureau, Rockville, MD.
Catherine Rice, National Center on Birth Defects and Developmental Disabilities, Atlanta, GA.
Stephen J. Blumberg, National Center for Health Statistics, Hyattsville, MD.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Levy SE, Giarelli E, Lee LC, et al. Autism spectrum disorder and co-occurring developmental, psychiatric, and medical conditions among children in multiple populations of the United States. J Dev Behav Pediatr. 2010;31(4):267–275. doi: 10.1097/DBP.0b013e3181d5d03b. [DOI] [PubMed] [Google Scholar]
- 3.Simonoff E, Pickles A, Charman T, et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- 4.Matson JL, Shoemaker M. Intellectual disability and its relationship to autism spectrum disorders. Res Dev Disabil. 2009;30(6):1107–1114. doi: 10.1016/j.ridd.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 5.Spencer D, Marshall J, Post B, et al. Psychotropic medication use and polypharmacy in children with autism spectrum disorders. Pediatrics. 2013;132(5):833–840. doi: 10.1542/peds.2012-3774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ruble LA, Heflinger CA, Renfrew JW, et al. Access and service use by children with autism spectrum disorders Medicaid managed care. J Autism Dev Disord. 2005;35(1):3–13. doi: 10.1007/s10803-004-1026-6. [DOI] [PubMed] [Google Scholar]
- 7.Ruble LA, McGrew JH. Community service outcomes for families and children with autism spectrum disorders. Res Autism Spectr Disord. 2007;1(4):360–372. [Google Scholar]
- 8.Mandell DS, Walrath CM, Manteuffel B, et al. Characteristics of children with autistic spectrum disorders served in comprehensive community-based mental health settings. J Autism and Dev Disord. 2005;35(1):313–321. doi: 10.1007/s10803-005-3296-z. [DOI] [PubMed] [Google Scholar]
- 9.Cidav Z, Lawer L, Marcus SC, et al. Age-related variation in health service use and associated expenditures among children with autism. J Autism Dev Disord. 2013;43(4):924–931. doi: 10.1007/s10803-012-1637-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ganz ML. The lifetime distribution of the incremental societal costs of autism. Arch Pediatr Adolesc Med. 2007;161(4):343–349. doi: 10.1001/archpedi.161.4.343. [DOI] [PubMed] [Google Scholar]
- 11.Liptak GS, Stuart T, Auinger P. Health care utilization and expenditures for children with autism: data from U.S. national samples. J Autism Dev Disord. 2006;36(7):871–879. doi: 10.1007/s10803-006-0119-9. [DOI] [PubMed] [Google Scholar]
- 12.Mandell DS. Understanding and addressing the impact of autism on the family. LDI Issue Brief. 2012;17(7):1–4. [PubMed] [Google Scholar]
- 13.Wang L, Leslie DL. Health care expenditures for children with autism spectrum disorders in Medicaid. J Am Acad Child Adolesc Psychiatry. 2010;49(11):1165–1171. doi: 10.1016/j.jaac.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mandell DS, Wiggins LD, Arnstein Carpenter L, et al. Racial/ethnic disparities in the identification of children with autism spectrum disorders. Am J Public Health. 2009;99(3):493–498. doi: 10.2105/AJPH.2007.131243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dawson G, Bernier R. A quarter century of progress on the early detection and treatment of autism spectrum disorder. Dev Psychopathol. 2013;25(4 Pt 2):1455–1472. doi: 10.1017/S0954579413000710. [DOI] [PubMed] [Google Scholar]
- 16.Goin-Kochel RP, Mackintosh VH, Myers BJ. How many doctors does it take to make an autism spectrum diagnosis. Autism. 2006;10(5):439–451. doi: 10.1177/1362361306066601. [DOI] [PubMed] [Google Scholar]
- 17.Siklos S, Kerns KA. Assessing the diagnostic experiences of a small sample of parents of children with autism spectrum disorders. Res Dev Disabil. 2007;28(1):9–22. doi: 10.1016/j.ridd.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 18.Bromley J, Hare DJ, Davison K, et al. Mothers supporting children with autistic spectrum disorders, social support, mental health status and satisfaction with services. Autism. 2004;8(4):425–444. doi: 10.1177/1362361304047224. [DOI] [PubMed] [Google Scholar]
- 19.Liptak GS, Orlando M, Yingling JT, et al. Satisfaction with primary health care received by families of children with developmental disabilities. J Pediatr Health Care. 2006;20(4):245–252. doi: 10.1016/j.pedhc.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 20.Chiri G, Warfield ME. Unmet need and problems accessing core health care services for children with autism spectrum disorder. Matern Child Health J. 2012;16(5):1081–1091. doi: 10.1007/s10995-011-0833-6. [DOI] [PubMed] [Google Scholar]
- 21.Krauss MW, Gulley S, Sciegaj M, et al. Access to specialty medical care for children with mental retardation, autism, and other special health care needs. Ment Retard. 2003;41(5):329–339. doi: 10.1352/0047-6765(2003)41<329:ATSMCF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Carbone PS, Behl DD, Azor V, et al. The medical home for children with autism spectrum disorders: parent and pediatrician perspectives. J Autism Dev Disord. 2010;40(3):317–324. doi: 10.1007/s10803-009-0874-5. [DOI] [PubMed] [Google Scholar]
- 23.Kogan MD, Blumberg SJ, Schieve LA, et al. Prevalence of parent-reported diagnosis of autism spectrum disorder among children in the US, 2007. Pediatrics. 2009;124(5):1395–1403. doi: 10.1542/peds.2009-1522. [DOI] [PubMed] [Google Scholar]
- 24.Dekker MC, Koot HM, van der Ende J, et al. Emotional and behavioral problems in children and adolescents with and without intellectual disability. J Child Psychol Psychiatry. 2002;43(8):1087–1098. doi: 10.1111/1469-7610.00235. [DOI] [PubMed] [Google Scholar]
- 25.Dekker MC, Koot HM. DSM-IV disorders in children with borderline to moderate intellectual disability. I: Prevalence and impact. J Am Acad Child Adolesc Psychiatry. 2003;42(8):915–922. doi: 10.1097/01.CHI.0000046892.27264.1A. [DOI] [PubMed] [Google Scholar]
- 26.Matson JL, Neal D. Psychotropic medication use for challenging behaviros in person with intellectual disabilities: an overview. Res Dev Disabil. 2009;30(3):572–586. doi: 10.1016/j.ridd.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 27.Child and Adolescent Health Measurement Initiative. National Profile of Children with Special Health Care Needs and Autism Spectrum Disorders: Key Findings from the 2009/10 NS-CSHCN & 2011/12 NSCH. Maternal and Child Health Bureau (MCHB) 2013 Available at www.childhealthdata.org. [Google Scholar]
- 28.U.S. Department of Health and Human Services. 2011 HHS Guidelines. Federal Register. 2011 Jan 20;76(13):3637–3638. [Google Scholar]
- 29.StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 30.Mandell DS, Morales KH, Marcus SC, et al. Psychotropic medication use among Medicaid-enrolled children with autism spectrum disorders. Pediatrics. 2008;121(3):e441–e448. doi: 10.1542/peds.2007-0984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomas KC, Ellis AR, McLaurin C, et al. Access to care for autism-related services. J Autism Dev Disord. 2007;37(10):1902–1912. doi: 10.1007/s10803-006-0323-7. [DOI] [PubMed] [Google Scholar]
- 32.Thomas KC, Morrissey JP, McLaurin C. Use of autism-related services by families and children. J Autism and Dev Disord. 2007;37(5):818–829. doi: 10.1007/s10803-006-0208-9. [DOI] [PubMed] [Google Scholar]
- 33.Rosenberg RE, Mandell DS, Farmer JE, et al. Psychotropic medication use among children with autism spectrum disorders enrolled in a national registry, 2007–2008. J Autism Dev Disord. 2010;40(3):342–351. doi: 10.1007/s10803-009-0878-1. [DOI] [PubMed] [Google Scholar]
- 34.Taurines R, Schwenck C, Westerwald E, et al. ADHD and autism: differential diagnosis or overlapping traits? A selective review. ADHD Atten Def Hyp Disord. 2012;4:115–139. doi: 10.1007/s12402-012-0086-2. [DOI] [PubMed] [Google Scholar]
- 35.Walkup JT, Albano AM, Piacentini J, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008;359(26):2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kogan MD, Strickland BB, Blumberg SJ, et al. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005–2006. Pediatrics. 2008;122(6):e1149–e1158. doi: 10.1542/peds.2008-1057. [DOI] [PubMed] [Google Scholar]
- 37.Stahmer AC. The basic structure of community early intervention programs for children with autism: provider descriptions. J Autism Dev Disord. 2007;37:1344–1354. doi: 10.1007/s10803-006-0284-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Myers SM, Johnson CP. Management of children with autism spectrum disorders. Pediatrics. 2007;120(5):1162–1182. doi: 10.1542/peds.2007-2362. [DOI] [PubMed] [Google Scholar]