Abstract
OBJECTIVE
Specification of appropriate personal protective equipment for respiratory protection against influenza is somewhat controversial. In a clinical environment, N95 filtering facepiece respirators (FFRs) are often recommended for respiratory protection against infectious aerosols. This study evaluates the ability of N95 FFRs to capture viable H1N1 influenza aerosols.
METHODS
Five N95 FFR models were challenged with aerosolized viable H1N1 influenza and inert polystyrene latex particles at continuous flow rates of 85 and 170 liters per minute. Virus was assayed using Madin-Darby canine kidney cells to determine the median tissue culture infective dose (TCID50). Aerosols were generated using a Collison nebulizer containing H1N1 influenza virus at 1 × 108 TCID50/mL. To determine filtration efficiency, viable sampling was performed upstream and downstream of the FFR.
RESULTS
N95 FFRs filtered 0.8-µm particles of both H1N1 influenza and inert origins with more than 95% efficiency. With the exception of 1 model, no statistically significant difference in filtration performance was observed between influenza and inert particles of similar size. Although statistically significant differences were observed for 2 models when comparing the 2 flow rates, the differences have no significance to protection.
CONCLUSIONS
This study empirically demonstrates that a National Institute for Occupational Safety and Health–approved N95 FFR captures viable H1N1 influenza aerosols as well as or better than its N95 rating, suggesting that a properly fitted FFR reduces inhalation exposure to airborne influenza virus. This study also provides evidence that filtration efficiency is based primarily on particle size rather than the nature of the particle’s origin.
Pandemic influenza poses a significant health threat to the international community as novel strains emerge that vary widely in virulence and infectivity.1,2 Which of the primary modes of human transmission of influenza3–6—direct contact, inspiration, inhalation, and direct spray—are responsible for spreading influenza is a subject of active debate. As a consequence, specification of the appropriate personal protective equipment (PPE) for respiratory protection against influenza is likewise controversial. For direct-spray transmission, a surgical mask may be appropriate for reducing the risk of infection, but it is not recommended for protection against aerosol transmission via inhalation or inspiration. In accordance with guidance provided by the Centers for Disease Control and Prevention, the Occupational Safety and Health Administration (OSHA) mandates that healthcare workers wear PPE at least as protective as a properly fitted National Institute for Occupational Safety and Health (NIOSH)–certified N95 filtering facepiece respirator (FFR) when exposed to some inhalable or inspirable infectious aerosols (eg, severe acute respiratory syndrome, tuberculosis, and 2009 H1N1 pandemic influenza).7,8 For use in clinical settings, N95 FFRs are sometimes also cleared for sale by the Food and Drug Administration as a medical device having fluid-resistant properties and certified by NIOSH. Devices carrying a NIOSH certification have shown the ability to remove 95% or more of particles of the conventional most-penetrating particle size (MPPS), 0.3 µm (with larger or smaller particles being removed more efficiently).9 However, the MPPS for FFRs employing electret media (media possessing an electrical charge) is smaller.10
The mechanisms used by FFRs to remove particles from the air are well understood.11 It is also well accepted that the composition of particles of similar density does not affect particle capture efficiency. Thus, viable and inert particles of equivalent size and mass should be removed with the same filtration efficiency. Many studies have been performed to evaluate the filtration efficiency of viable microorganisms.12–16 Without exception, they all show that viable microorganisms are removed at similar or slightly greater rates than inert particles of the same size, supporting the idea that FFR effectiveness against aerosol transmission does not need to be reevaluated for every new disease-causing agent. However, even with this consistent knowledge base, end users of FFRs still want confirmation that the device is capable of removing actual infective agents of interest. We found limited studies evaluating FFR performance when challenged with viable influenza aerosols. Zuo et al17 challenged N95 FFRs with viable aerosols of human adenovirus serotype 1 and swine influenza H3N2 but were able to obtain viable data for the adenovirus only upstream of the FFR. Borkow et al18 evaluated the antimicrobial efficacy of copper-impregnated N95 FFRs by challenging with viable H1N1 aerosols. Their results showed greater than 99% viable filtration efficiency (VFE), but they did not correlate their data to inert particles. Our study challenged 5 FFR models (Table 1) with viable H1N1 influenza aerosols representative of human respiratory secretions and compares the VFE to the inert particle filtration efficiency (PFE) at 2 flow rates.
TABLE 1.
Filtering Facepiece Respirators (FFRs) Used in This Study
| Manufacturer | Model | Rating | FFR shape | Antimicrobial |
|---|---|---|---|---|
| 3M | 1860S | N95 | Cup | None |
| 3M | 1870 | N95 | Flat fold | None |
| Kimberly-Clark | PFR95 | N95 | Duck bill | None |
| SafeLife | T5000 | N95 | Cup | Triosyn (iodine) |
| GlaxoSmithKline | Actiprotect | N95 | Cup | Virucoat (citric acid) |
METHODS
H1N1 Virus
Influenza A/PR/8/34 VR-1469 (ATCC VR-95) was propagated in embryonic chicken eggs by means of standard World Health Organization protocols.19 Virus titers were determined by a median tissue culture infectious dose (TCID50) assay using Madin-Darby canine kidney cells (ATCC CCL-34) and cell culture techniques approved by the World Health Organization.19 For aerosolization studies, the H1N1 influenza virus was diluted to a concentration of 1 × 108 TCID50/mL in an artificial saliva buffer.20 The count median diameter (CMD) of the particle size distribution (PSD) of the influenza aerosol in the artificial saliva buffer was 0.83 µm, as previously determined using an Aerodynamic Particle Sizer (APS) 3321 (TSI).21
Filtration Studies
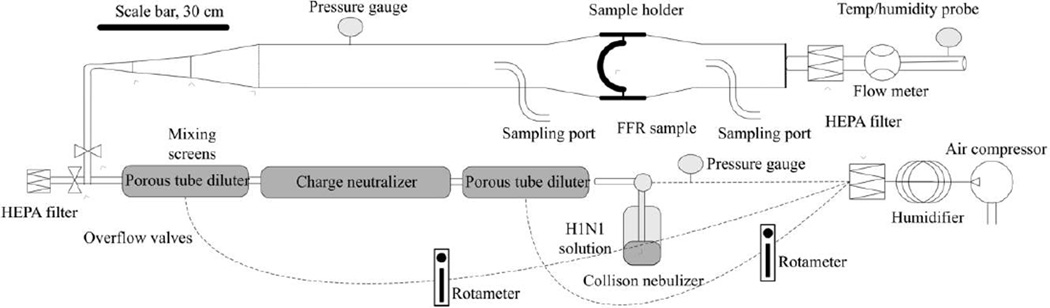
Five models of NIOSH-approved N95 FFRs, of which 2 models contained antimicrobial components (GlaxoSmithKline [GSK] Actiprotect and SafeLife T5000), were used for this study (Table 1). The 3 nonantimicrobial models were chosen for their common use in the healthcare workplace. The 2 antimicrobial models were selected because they were the only 2 such models that were commercially available and NIOSH approved. All models were tested in triplicate under 2 conditions: (1) an aerosol challenge at the NIOSH-specified standard flow rate of 85 liters per minute (LPM) and (2) a morestrenuous aerosol challenge of 170 LPM to evaluate FFR performance under extreme conditions. A laboratory-scale aerosol tunnel (LSAT; Figure 1) was used to challenge the FFRs with viable influenza and inert beads. A complete description of the LSAT has been reported elsewhere.20–22 Prior to each test, the LSAT was flushed with purified air for 30 minutes at a flow rate of 50 LPM. For each independent test (1 FFR at 1 condition), a FFR was glue-sealed into a 6-inchdiameter sample holder as described elsewhere21 and then secured into the LSAT via stainless steel sanitary fittings. Each FFR was first challenged with 0.8-µm polystyrene latex beads (Thermo Scientific). The beads were suspended in sterile water and then placed in a 6-jet Collison nebulizer (BGI), operating at 20 psi to generate the aerosol. Following a 10-minute equilibration period, 3 alternating upstream and downstream samples were collected using the APS. The air flow was then redirected to a high-efficiency particulate air (HEPA) filter, while the Collison nebulizer was replaced with another Collison nebulizer containing 30 mL of H1N1 influenza diluted to a concentration of 1 × 108 TCID50/mL in artificial saliva.
FIGURE 1.
Laboratory-scale aerosol tunnel. FFR, filtering facepiece respirator; HEPA, high-efficiency particulate air.
Following a 10-minute equilibration period, alternating viable samples were collected through the upstream and downstream ports. All-glass impingers (AGI-30; Ace Glass) containing 20 mL of serum-free Eagle’s minimum essential medium (Hyclone Laboratories) supplemented with 1% 100× penicillin-streptomycin and 1% 200 mM l-glutamine (Sigma-Aldrich) were used for collection. To minimize particle loss, the AGI-30s were directly attached to the isokinetic sampling ports on the LSAT. Sampling was initiated by opening the valve on the port and then applying a vacuum source to the AGI-30, which sampled at approximately 12.5 LPM. After 5 minutes, the sampling port was closed, the vacuum was turned off, and the AGI-30 was placed on ice until viable plating was performed. A total of 6 samples (3 upstream and 3 downstream, alternately sampled) were collected for each FFR. Following each run, the FFR was removed and HEPA filters were connected to the sampling ports. The LSAT was subsequently flushed with purified air at 60 ± 10 LPM for 3 hours. A manometer was used to monitor the pressure drop across the filter during each run.
Data Analysis
Upstream and downstream measurements for the 0.8-µm bead study were collected using data from the 0.723–0.925-µm size bins of the APS. The concentration of viable virus (log TCID50 per milliliter of extract) collected in the upstream and downstream AGI-30s was determined using the Spearman-Kärber formula.23 Equation (1) was used to determine the total amount of virus recovered from each sample (20-mL impinger volume). For samples with no detectable downstream viable data, half the detection limit (2.5 TCID50 infectious dose units) of the viable assay was used to calculate the reduction.24 The VFE of the FFRs was determined using equation (2), and the PFE was determined using equation (3). A 2-tailed paired t test was used to compare the inert (0.8-µm bead) and viable (H1N1 influenza) filtration data for each N95 FFR model. The average PFE and VFE values for the 2 flow rates were compared using a 2-tailed unpaired t test. A 1-way analysis of variance (ANOVA) test with a Bonferroni posttest was used to compare data obtained from the antimicrobial and nonantimicrobial FFR models.
Equation (1) is as follows:
| (1) |
where L is viable H1N1 expressed in units of log10 TCID50 per milliliter and V is sample volume. If no viable viruses are present (L = −∞), then LS will be half the detection limit. Equation (2) is
| (2) |
where DLS is downstream log10 TCID50, ULS is upstream log10 TCID50, and n is the number of determinations, and equation (3) is
| (3) |
where U is the upstream particle concentration and D is the downstream particle concentration.
RESULTS
The average upstream challenge for all FFR replicates was 1.8 × 103 TCID50per liter of air. Under standard flow (85 LPM) parameters, the mean PFE for all FFR models ranged from 99.72% to 99.999%, and the mean VFE ranged from 98.93% to 99.996% (Table 2). A statistical comparison of the 2 data sets demonstrated that there is a significant difference (P < .05) between inert and viable particle filtration for only the Kimberly-Clark model (P = .02). The SafeLife T5000 provided 1–2 orders of magnitude higher filtration performance, exceeding the NIOSH standard for an N100 FFR. Four of the 6 SafeLife T5000 replicates produced no detectable virus downstream.
TABLE 2.
Average Removal Efficiencies of 0.8-µm Particles at 85 Liters per Minute
| FFR model | Inert, % | H1N1 influenza, % | P |
|---|---|---|---|
| 3M 1860S | 99.85 ± 0.10 | 99.27 ± 0.38 | .08 |
| 3M 1870 | 99.90 ± 0.09 | 99.13 ± 1.36 | .45 |
| Kimberly-Clark PFR95 | 99.72 ± 0.16 | 98.93 ± 0.36 | .02 |
| SafeLife T5000 | 99.999 ± 0.001 | 99.996 ± 0.002a | .09 |
| GlaxoSmithKline Actiprotect | 99.94 ± 0.06 | 99.23 ± 1.00 | .19 |
The data for 1 filtering facepiece respirator (FFR) replicate were below the detection limit.
Under high flow (170 LPM) parameters, the mean PFE for all FFR models ranged from 98.37% to 99.994%, and the mean VFE ranged from 96.29% to 99.995% (Table 3). The SafeLife T5000 again provided 1–2 orders of magnitude higher filtration performance. A statistical comparison of the 2 data sets demonstrated a significant difference between inert and viable particle filtration for only the Kimberly-Clark FFR (P = .02).
TABLE 3.
Average Removal Efficiencies of 0.8-µm Particles at 170 Liters per Minute
| FFR model | Inert, % | H1N1 influenza, % | P |
|---|---|---|---|
| 3M 1860S | 99.37 ± 0.39 | 98.56 ± 0.87 | .13 |
| 3M 1870 | 99.96 ± 0.03 | 99.59 ± 0.27 | .14 |
| Kimberly-Clark PFR95 | 98.37 ± 0.32 | 96.29 ± 0.56 | .02 |
| SafeLife T5000 | 99.994 ± 0.009 | 99.995 ± 0.002a | .90 |
| GlaxoSmithKline Actiprotect | 99.23 ± 0.15 | 96.29 ± 2.49 | .09 |
The data for all 3 filtering facepiece respirator (FFR) replicates were below the detection limit.
A comparison of performances at 85 and 170 LPM was conducted. The Kimberly-Clark model demonstrated statistically significant different filtration efficiencies for both inert and viable aerosol challenges (P = .003 and .002, respectively). The GSK Actiprotect model was found to demonstrate a significant difference only for the inert particles (P = .0006). A 1-way ANOVA test demonstrated a statistically significant difference between the nonantimicrobial FFR models and both the Safelife T5000 and GSK Actiprotect for VFE at the 170-LPM condition (P = .0001 and .05, respectively). A significant difference was also observed for PFE (P = .0002 and .0003, respectively). No significant difference was found between the nonantimicrobial and antimicrobial FFRs at the 85-LPM condition.
DISCUSSION
Previous experimental studies, supported by filtration theory, demonstrate that PFE increases with particle size above the MPPS. While it is possible in a laboratory setting to artificially generate an influenza aerosol near the MPPS of most FFRs, particles in this size range (approximately 0.1 µm) are relatively unstable and are unlikely to exist in practice. In actual workplace settings, influenza expelled from humans via respiratory sections is typically much larger (approximately 0.8 µm) than the bare virus. We acknowledge the existence of divergent reports pertaining to the assessment of particles/droplets derived from human respiratory secretions,25–28 but we maintain that use of a 0.8-µm particle is justified on the basis of the literature.20
Each N95 FFR model tested as part of this study yielded equivalent VFE and PFE values that exceeded 95% (Tables 2 and 3). As NIOSH certification is based on removal of 0.3-µm particles, these higher removals are to be expected for the larger particles studied here. Although determined to be statistically significant, the differences between PFE and VFE at 85 LPM for the Kimberly-Clark model (less than 2.6%) are not considered to be meaningful because the 95% NIOSH benchmark was met and actual protection is driven more by differences in fit (leakage) than filtration performance. Thus, the statistical analysis in this case is not instructive and indicates only that the low variability among replicate measurements obtained by the particle sizer allows discrimination of the slightly higher filtration efficiencies of inert particles from the generally greater variability associated with capturing and assaying viable biological particles.
A possible bias introduced in this study is that the methods of analysis for inert and viable challenges are different, which may influence the comparison of the VFE and PFE. The PFE is determined using the APS and accounts only for particles whose aerodynamic particle size ranges from 0.723 to 0.925 µm. In contrast, the VFE accounts for all particles in the PSD. Another bias may be present in the sampling procedure because AGI-30 impingers collect larger particles more efficiently,29 as do FFRs. The particles most likely to penetrate the FFR fall into a smaller size range, in which capture efficiency by the impinger is lower. Another factor that must be considered is the distribution of viable particles within the overall PSD, which is not known and may introduce another bias that cannot be accounted for. Our data are consistent with values reported by Borkow et al,18 who demonstrated more than 95% reduction of VFE in an aerosol (approximately 3.0-µm CMD) containing viable influenza, although they sampled by means of impaction rather than impingers and performed their testing at a lower flow rate, 28 LPM. Zuo et al17 also provided data showing that viable influenza can be removed from the airstream but provided particle-count data derived only from a viable challenge of much smaller particles (CMD of less than 0.1 µm), which behave much differently.20
The effect of flow rate on N95 FFR performance was assessed by incorporating 2 flow conditions into the experimental design. According to 42 CFR 84 subpart K, section 84.181, the 85-LPM flow rate is the condition specified by NIOSH for evaluating the performance of FFRs. This flow rate was selected to represent a worker’s inhalation at a high work rate. However, peak inhalation flow during breathing may be greater than 85 LPM for brief periods of time30 and exacerbated further as work intensity is increased. For these reasons, we also tested at 170 LPM to provide an extreme challenge to the filter. The overall filtration numbers were slightly lower in the higher flow rate (Tables 2 and 3), as would be expected for particles smaller than 1 µm. Critical inspection of the data shows that the actual difference in filtration performance between the 85- and 170-LPM conditions for the particle size studied is negligible (1%–2%). Although statistically significant, these differences are merely an indicator of low variability in the data sets and not a physically meaningful distinction.
Although the antimicrobial FFR models (SafeLife T5000 and GSK Actiprotect) demonstrated considerably higher filtration efficiencies than the nonantimicrobial models, they did not provide a significantly greater reduction in viable penetration compared with inert particles, and we attribute the increased filtration efficiency to physical means rather than antimicrobial properties. These results are in line with what was observed by Borkow et al,18 who found no improvement in VFE for FFRs impregnated with copper oxide. The SafeLife T5000’s filtration performance actually exceeds the rating for a N100, observed for both the inert and the viable H1N1 particles. For the GSK FFR, the lack of reduction in VFE due to the antimicrobial was expected, as the manufacturer claims only that the antimicrobial is a surface decontaminant. It is of interest to note that the GSK FFR had the highest variability for VFE (σ = ±2.5%) among all FFRs tested (Tables 2 and 3). The reason for this is unclear; it is possible that the citric acid present on the FFR interferes with the viable assay, but as the VFE is lower than the PFE, it might suggest that citrate is protective, acting to shield the virus downstream of the FFR. Additional research is necessary to isolate the mechanism causing the variability.
The significance of these findings to healthcare workers is that the data provide a basis to estimate the level of protection that a healthcare worker can expect from a respirator during exposure to infectious aerosols. Inhalation exposures received by a respirator wearer come from a combination of leakage around the face seal, direct penetration through the filter, and leakage through other apertures (eg, holes in filters from staples used to secure FFR straps). Numerous workplace studies have shown that a properly fitted NIOSH-certified N95 FFR will reduce toxic inhalation exposures by a factor of 10 or more.31,32 Controlled leak studies conducted using manikin headforms have shown that leak size is the dominant factor affecting respirator inward leakage.33 In the workplace, an OSHA-mandated fit test is required to ensure that the respirator is capable of fitting the healthcare worker (ie, seals tightly to the face to minimize leakage in the face seal area). Because the FFR was sealed (ie, a perfect fit) in our experiments, capture efficiencies for viable H1N1 influenza exceeding 98.9% at the lowest flow rate represent a best-case scenario in terms of fit. However, when some inward leakage during routine respirator wear is factored in, these data, combined with the workplace studies cited above, suggest that an N95 FFR is capable of reducing inhalational exposure to H1N1 influenza or other infectious aerosols by a factor of 10 or greater if properly fitted and used as expected, similar to the attenuation of other workplace aerosols.
In conclusion, this study empirically demonstrates that a NIOSH-approved N95 FFR captures viable H1N1 influenza aerosols with an efficiency equal to or greater than its N95 rating, suggesting that a properly fitted FFR reduces inhalation exposure to airborne influenza virus. Only 5 FFR models were tested as part of this study, but the findings have broad applicability to all properly fitted NIOSH-approved N95 FFRs. This study also demonstrates that the N95 FFR models tested remove particles from the airstream, indiscriminate of viability. Particles that contain H1N1 influenza are equally affected by filtration mechanisms as inert particles of the same size. Although the antimicrobial FFRs demonstrated significantly higher VFE, they also showed significantly higher PFE; thus, their enhanced performance must be attributed to physical means rather than antimicrobial activity.
ACKNOWLEDGMENTS
Financial support. This research was funded by the Biomedical Advanced Research and Development Authority, Office of the Assistant Secretary for Preparedness and Response, US Department of Health and Human Services, through an interagency agreement with the Air Force Research Laboratory (AFRL). This work was also partly funded by the National Institute for Occupational Safety and Health through an interagency agreement with the AFRL. Representatives of both funding agencies were involved in the development of the experimental design, data interpretation, and manuscript preparation.
Footnotes
Potential conflicts of interest. All authors report no conflicts of interest relevant to this article. All authors submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and the conflicts that the editors consider relevant to this article are disclosed here.
The findings and conclusions of this article are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health or the Biomedical Advanced Research and Development Authority, Office of the Assistant Secretary for Preparedness and Response, US Department of Health and Human Services.
REFERENCES
- 1.Tellier R. Aerosol transmission of influenza A virus: a review of new studies. J R Soc Interface. 2009;6:783–790. doi: 10.1098/rsif.2009.0302.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Masaki I, Watanabe T, Masato H, et al. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortment H5 HA/H1N1 virus in ferrets. Nature. 2012;486(7403):420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones RM, Adida E. Influenza infection risk and predominate exposure route: uncertainty analysis. Risk Anal. 2011;31(10):1622–1631. doi: 10.1111/j.1539-6924.2011.01600.x. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine. Preventing Transmission of Pandemic Influenza and Other Viral Respiratory Diseases: Personal Protective Equipment for Healthcare Personnel, Update 2010. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 5.Tellier R. Review of aerosol transmission of influenza A virus. Emerg Infect Dis. 2006;12:1657–1662. doi: 10.3201/eid1211.060426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bridges CB, Kuehnert MJ, Hall CB. Transmission of influenza: implications for control in health care settings. Clin Infect Dis. 2003;37(8):1094–1101. doi: 10.1086/378292. [DOI] [PubMed] [Google Scholar]
- 7.Siegel JD, Rhinehart E, Jackson M, Chiarello L. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings. Am J Infect Control. 2007;25:S65–S164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pandemic influenza preparedness and response guidance for healthcare workers and healthcare employers. [Accessed December 10, 2011];Occupational Safety and Health Administration (OSHA) website. Publication no. OSHA 3328-05. http://www.osha.gov/Publications/3328-05-2007-English.html. Published 2007.
- 9.Birkner JS, Colton CE. Respiratory protective equipment. In: Rose V, Cohrssen B, editors. Patty’s Industrial Hygiene. 6th ed. New York: Wiley; 2010. pp. 1169–1233. [Google Scholar]
- 10.Shaffer RE, Rengasamy S. Respiratory protection against airborne nanoparticles: a review. J Nanopart Res. 2009;11:1661–1672. [Google Scholar]
- 11.Hinds WC. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles. 2nd ed. New York: Wiley; 1999. [Google Scholar]
- 12.Balazy A, Toivola M, Adhikari A, et al. Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am J Infect Control. 2006;34(2):51–57. doi: 10.1016/j.ajic.2005.08.018. [DOI] [PubMed] [Google Scholar]
- 13.Heimbuch BK, Wander JD, Wu CY, Wallace WH, Kinney K, Lumley AE. Defense Technical Information Center. Tyndall Air Force Base, FL: AFRL-ML-TY-TP-2006-4527, Air Force Research Laboratory; 2006. Bioaerosol challenges to antimicrobial surface treatments: enhanced efficacy against MS2 coli phage of air filter media coated with polystyrene-4-methyltrimethylammonium triiodide. Accession no. ADA444909. [Google Scholar]
- 14.Heimbuch BK, Wu CY, Wander JD. Defense Technical Information Center. Tyndall Air Force Base, FL: AFRL-RX-TY-TP-2009-4567, Air Force Research Laboratory; 2009. Viral penetration of high efficiency particulate air (HEPA) filters. Accession no. ADA505315. [Google Scholar]
- 15.Gardner PD, Richardson AW, Eshbaugh JP, Hofacre KC. Defense Technical Information Center. Aberdeen Proving Ground, MD: ECBC-CR-085, Edgewood Chemical and Biological Center, US Army Research Development and Engineering Command; 2006. Respirator filter efficiency testing against particulate and biological aerosols under moderate to high flow rates. Accession no. ADA457318. [Google Scholar]
- 16.Eninger RM, Adhikari A, Reponen T, Grinshpun SA. Differentiating between physical and viable penetrations when challenging respirator filters with bioaerosols. Clean—Soil AirWater. 2008;36(7):615–621. [Google Scholar]
- 17.Zuo Z, Kuehn TH, Pui DYH. Performance evaluation of filtering facepiece respirators using virus aerosols. Am J Infect Control. 2013;41(1):80–82. doi: 10.1016/j.ajic.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 18.Borkow G, Zhoi SS, Page T, Gabbay J. A novel anti-influenza copper oxide containing respiratory face mask. PLoS ONE. 2010;5(6):e11295. doi: 10.1371/journal.pone.0011295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. [Accessed December 14, 2011];WHO Manual on Animal Influenza Diagnosis and Surveillance. http://www.who.int/csr/resources/publications/influenza/whocdscsrncs20025rev.pdf. Published 2002.
- 20.American Society for Testing and Materials (ASTM) Standard Test Method for Effectiveness of Decontamination of Air-Permeable Materials Challenged with Biological Aerosols Containing Human Pathogenic Viruses. West Conshohocken, PA: ASTM International; 2010. Standard E2720-10. [Google Scholar]
- 21.Heimbuch BK, Wu CY, Wander JD, et al. A pandemic influenza preparedness study: use of energetic methods to decontaminate filtering facepiece respirators contaminated with H1N1 aerosols and droplets. Am J Infect Control. 2010;38(1):3–8. doi: 10.1016/j.ajic.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Foarde K, Heimbuch BK, Maxwell A, VanOsdell D. Test Operating Procedure under the Army Test and Evaluation Command. Aberdeen Proving Ground, MD: Edgewood Chemical and Biological Center; 2009. Method for evaluating air purification technologies for collective protection using viable microbial aerosols. (forthcoming). [Google Scholar]
- 23.Finney DJ. Statistical Methods in Biological Assays. 2nd ed. New York: Hafner; 1964. [Google Scholar]
- 24.Singh A, Nocerino J. Robust estimation of mean and variance using environmental data sets with below detection limit observations. Chemometr Intell Lab Syst. 2002;60:69–86. [Google Scholar]
- 25.Duguid JP. The size and duration of air-carriage of respiratory droplets and droplet-nuclei. J Hyg. 1946;4:471–480. doi: 10.1017/s0022172400019288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang S, Lee GWM, Chen CM, Wu CC, Yu KP. The size and concentration of droplets generated by coughing in human subjects. J Aerosol Med. 2007;20(4):484–494. doi: 10.1089/jam.2007.0610. [DOI] [PubMed] [Google Scholar]
- 27.Chao CYH, Wan MP, Morawska L, et al. Characterization of expiration air jets and droplets size distributions immediately at the mouth opening. Aerosol Sci. 2009;40:122–133. doi: 10.1016/j.jaerosci.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morawska L, Johnson GR, Ristovski Z, et al. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. Aerosol Sci. 2009;40:256–269. [Google Scholar]
- 29.Lin X, Willeke K, Ulevicius V, Grinshpun SA. Effect of sampling time on the collection efficiency of all-glass impingers. AIHA J. 1997;58(7):480–487. [Google Scholar]
- 30.Caretti DM, Gardner PD, Coyne KM. Defense Technical Information Center. Aberdeen Proving Ground, MD: ECBC-TR-316, Edgewood Chemical Biological Center, US Army Research, Development, and Engineering Command; 2004. Workplace breathing rates: defining anticipated values and ranges for respirator certification testing. Accession no. ADA465595. [Google Scholar]
- 31.Janssen LL, Nelson TJ, Cuta KT. Workplace protection factors for an N95 filtering facepiece respirator. J Occup Environ Hyg. 2007;4(9):698–707. doi: 10.1080/15459620701517764. [DOI] [PubMed] [Google Scholar]
- 32.Cho KJ, Reponen T, McKay R, et al. Comparison of workplace protection factors for different biological contaminants. J Occup Environ Hyg. 2011;8(7):417–425. doi: 10.1080/15459624.2011.585094. [DOI] [PubMed] [Google Scholar]
- 33.Rengasamy S, Eimer BC. Total inward leakage of nanoparticles through filtering facepiece respirators. Ann Occup Hyg. 2011;55(3):253–263. doi: 10.1093/annhyg/meq096. [DOI] [PubMed] [Google Scholar]