Abstract
Background
Renal coloboma syndrome (RCS) is characterized by renal anomalies and optic nerve colobomas. PAX2 mutations contribute to RCS. However, approximately half of the patients with RCS have no mutation in PAX2 gene.
Methods
To investigate the incidence and effects of mutations of PAX2 and 25 candidate genes, patient genes were screened using next-generation sequence analysis, and candidate mutations were confirmed using Sanger sequencing. The correlation between mutations and clinical manifestation was evaluated.
Result
Thirty patients, including 26 patients (two families of five and two, 19 sporadic cases) with RCS, and 4 optic nerve coloboma only control cases were evaluated in the present study. Six PAX2 mutations in 21 probands [28%; two in family cohorts (n = 5 and n = 2) and in 4 out of 19 patients with sporadic disease] including four novel mutations were confirmed using Sanger sequencing. Moreover, four other sequence variants (CHD7, SALL4, KIF26B, and SIX4) were also confirmed, including a potentially pathogenic novel KIF26B mutation. Kidney function and proteinuria were more severe in patients with PAX2 mutations than in those without the mutation. Moreover, the coloboma score was significantly higher in patients with PAX2 gene mutations. Three out of five patients with PAX2 mutations had focal segmental glomerulosclerosis (FSGS) diagnosed from kidney biopsies.
Conclusion
The results of this study identify several new mutations of PAX2, and sequence variants in four additional genes, including a novel potentially pathogenic mutation in KIF26B, which may play a role in the pathogenesis of RCS.
Introduction
Renal coloboma syndrome (RCS; papillorenal syndrome) is characterized by kidney hypoplasia or dysplasia and abnormality of the optic nerve. Abnormal kidney structure and function vary among patients. For example, some abnormalities are clinically silent but others include kidney insufficiency and end-stage renal disease. Further, patients with RCS exhibit ocular abnormalities. Developmental abnormalities of the optic nerve (ranging from mild optic disc dysplasia to optic nerve aplasia), retina, choroid, and iris are included in coloboma [1]. Abnormal eye structure and function, such as serious retinal detachment and thin hypoplastic peripheral retinas, also vary among patients [2]. Although the diagnosis of RCS is based on the morphological examination of the kidney, ophthalmologic findings, and family history, the variations of clinical manifestations make timely diagnosis difficult.
PAX2 mutations represent one of the main genetic abnormalities of RCS [3, 4]. PAX2 encodes a transcription factor that mediates development and plays key roles in different stages of the development of the kidneys, eyes, ears, and genital tract [5]. Studies of animals with PAX2 mutations show congenital loss of nephron number [2, 4–6].Approximately 170 cases with PAX2 gene abnormalities have been reported in cases with RCS worldwide [7]. However, around 50% cases of RCS have no abnormality in PAX2 gene[8].
PAX2 is a key transcriptional factor that functions in the regulation of a diverse range of genes involved in kidney and eye development. A previous study using RNA-seq analysis following PAX2 siRNA knockdown identified 3135 transcripts differentially regulated by PAX2 [9]. PAX2-mediated gene expression is reportedly regulated by many transcriptional and intra-cellular signaling factors including Wnt ligands, bone morphogenic proteins, fibroblast growth factor, sonic hedgehog, RET/glial cell-derived neurotrophic factor, notch signaling pathways [9], PAX2-binding proteins such as Hox11 and Eya1 [10], and epigenetic modulation of target genes regulated by PTIP and the mixed-lineage leukemia (MLL) complex [11, 12]. Moreover, kidney and eye development is regulated by a complex network of genes, including GDF11, GDNF, FOXC1, SIX1, SALL1, PAX8, and WT1) [13]. Among them, we selected 25 candidate genes. Therefore, we speculated mutations in our candidate genes, in addition to PAX2 mutations, contribute to RCS pathogenesis.
In the present study, we hypothesized that PAX2 and 25 candidate genes contribute to the pathogenesis of RCS. Here we report the evaluation of 26 patients, including two family cohorts (n = 5 and n = 2) and 19 patients with sporadic disease for mutations in PAX2 and 25 candidate genes. We have detected four novel PAX2 mutations in 11 patients, and a potentially pathogenic KIF26B mutation in one patient. Our results suggest that these mutations may contribute to the pathogenesis of RCS.
Methods
Patients
Thirty patients, including two family cohorts (n = 5 and n = 2), 19 patients with sporadic RCS, and 4 coloboma only control cases were evaluated in the present study. Although the diagnosis of RCS is established according to clinical studies of the kidneys and eyes, there are no formal diagnostic criteria for RCS [14]. In the present study, we enrolled patients with kidney dysfunction, renal morphological abnormalities, or both. Optic nerve coloboma (dysplasia of the optic nerve) was defined as a clearly demarcated bowl-shaped excavation of the optic disc, which is typically decentered and deep. Slit-lamp examination, intraocular pressure measurement, fundus examination, and photography as well as measurement of visual acuity were performed. In addition to these clinical findings on the kidney and eyes, similar other syndromes were excluded by clinical evaluation. Patients with CHARGE syndrome (coloboma, heart malformations, atresia choanae, retardation of growth and development, genital anomalies, and ear and hearing abnormalities) were excluded according to the absence of the typical CHARGE syndrome findings of craniofacial abnormalities or cognitive difficulties. Patients with COACH syndrome (cerebral vermis hypoplasia, oligophrenia, ataxia, optic nerve coloboma, hepatic fibrosis) and Joubert syndrome were excluded according to the absence of the typical COACH and Joubert syndrome findings of developmental disability, cerebellar hypoplasia, cerebellar dysfunction, and hepatic dysfunction. We analyzed the sequences of PAX2 and 25 other genes in 26 patients clinically diagnosed with RCS, and 4 optic nerve coloboma only patients as disease-negative controls.
Ethics statement
The Ethics Committee of the Kanazawa University Graduate School of Medicine approved the study (Approval No. 169). All analyses in this study conformed to the ethical guidelines of the 1975 Declaration of Helsinki in its respective latest version. All individuals were >18 years of age. Written informed consent was obtained from all participants.
Nucleotide sequence analysis
Screening of DNA sequences was conducted using an Ion Torrent PGM sequencer equipped with the Ion 318 chip. We obtained sequences covering >90% of all genes, and the mean coverage was 97.7% (Table 1). Genomic positions of the mutations were determined using human genome build 19 and the University of California, Santa Cruz genome annotation database http://genome.ucsc.edu. The CLC Genomics Workbench was used to further process the sequence alignments and genotyping data. Variants were filtered using data from dbSNP 142 and the 1000 Genomes Project.
Table 1. DNA screening by next-generation sequencing.
| Name | Target (bp) | Missed (bp) | Covered (%) | |
|---|---|---|---|---|
| 1 | WNT4 | 1111 | 88 | 92.1 |
| 2 | SIX2 | 898 | 13 | 98.6 |
| 3 | SIX1 | 877 | 0 | 100.0 |
| 4 | SALL4 | 3206 | 0 | 100.0 |
| 5 | SALL1 | 7266 | 87 | 98.8 |
| 6 | NOTCH2 | 7987 | 139 | 98.3 |
| 7 | FOXC1 | 1673 | 163 | 90.3 |
| 8 | PAX8 | 1595 | 0 | 100.0 |
| 9 | HNF1B | 1971 | 0 | 100.0 |
| 10 | EYA1 | 2125 | 0 | 100.0 |
| 11 | HOX11 | 1041 | 14 | 98.7 |
| 12 | RET | 3756 | 8 | 99.8 |
| 13 | PAX2 | 1602 | 0 | 100.0 |
| 14 | KIF26B | 6492 | 238 | 96.3 |
| 15 | HESR1 | 1077 | 0 | 100.0 |
| 16 | BMP7 | 1373 | 0 | 100.0 |
| 17 | BMP4 | 1249 | 0 | 100.0 |
| 18 | WT1 | 1780 | 76 | 95.7 |
| 19 | WNT9A | 1142 | 106 | 90.7 |
| 20 | CHD7 | 9401 | 28 | 99.7 |
| 21 | WNT9B | 1118 | 81 | 92.8 |
| 22 | LHX1 | 1276 | 84 | 93.4 |
| 23 | GDNF | 1076 | 6 | 99.4 |
| 24 | NOTCH1 | 8042 | 106 | 98.7 |
| 25 | JAG1 | 3943 | 10 | 99.8 |
| 26 | SIX4 | 2379 | 65 | 97.3 |
| Mean | 2902.1 | 50.5 | 97.7 |
Gene mutations were screened using next-generation sequence analysis.
All genes were covered more than 90%, and the mean coverage was 97.7%.
PAX2 gene mutations were evaluated according to our published method[15]. Twelve primer sets for each PAX2 exon were synthesized according to sequence information with some modifications [16]. Amplified DNA fragments were purified and sequenced using a dye terminator cycle sequencing kit (DYEnamic ET Terminator; GE Healthcare Bio-Sciences Corp., Piscataway, NJ) and an automated DNA sequencer (ABI PRISM 310 DNA Sequencer; Applied Biosystems, Foster City, CA). Candidate mutations of the 25 other genes were determined using Sanger sequencing with same primers used for the Ion Torrent PGM sequencer at TaKaRa Dragon Genomics Center. Mutation Taster (http://www.mutationtaster.org) was used to predict potential contributions of individual mutations to disease. Moreover, allele frequencies were evaluated using the ExAc database (http://exac.broadinstitute.org).
Kidney biopsy specimens
Kidney biopsies were obtained from eight patients. For pathological diagnosis, a portion of each kidney specimen was fixed with 10% phosphate-buffered formalin (pH 7.4), embedded in paraffin, cut into 4-μm thick sections, and stained with hematoxylin and eosin, periodic acid-Schiff’s reagent, periodic acid silver methenamine, and Mallory-Azan solutions.
Scoring of optic disc coloboma
An experienced ophthalmologist (T. H.) reviewed photographs of the fundus of both eyes of each patient to determine the presence of an optic disc coloboma and other abnormalities of the fundus. The optic disc coloboma was scored according to a 5-point scale of 0 (normal) to 4 (severe) [8] as follows: 0 = normal; 1 = optic disc dysplasia, with an unusual pattern of retinal vessels and cilioretinal arteries; 2 = optic disc pit associated with vascular abnormalities and a cilioretinal artery; 3 = large coloboma involving the entire surface of the optic disc; 4 = large coloboma of the optic disc and adjacent retina or morning-glory anomaly (with radial emergence of the retinal vessels).
Statistical analysis
SPSS 19.0 and the StatView program were used for statistical analysis. Data are expressed as the mean ± standard error (mean ± SEM). Statistical analyses were performed using the Mann–Whitney U test; p < 0.05 indicated a statistically significant difference.
Results
Detection of mutations in patients with RCS
Screening the sequences of PAX2 and 25 other genes identified 760 SNPs and 9 small indels. Among them, 162 SNPs and 9 small indels were missense mutations. Moreover, 116 SNPs were deleted by filtering using the dbSNP137 and the 1000 Genomes Project database. Of these, 46 non-synonymous SNPs and 9 indels shared by the affected individuals were retained in the analysis (Table 1).
Among candidate gene abnormalities, six PAX2 mutations in 21 probands (28%; two in family cohorts [n = 5 and n = 2] and in 4 out of 19 patients with sporadic disease), including four novel mutations, were confirmed using Sanger sequencing (Table 1). Case 1–5 (a family) had the novel mutationc.119-120delGC (ClinVar accession number; SCV000255937). The novel heterozygous mutation ex2 c.187G>A (ClinVar accession number; SCV000255938) was detected in exon 2 of Patient 9, which generates the missense mutation G63S (Fig 1). Patients 10 and 11 had the novel PAX2 mutations ex2, c.57-58insGTGAACC (ClinVar accession number; SCV000255939) and ex3, c.224-225insAC (ClinVar accession number; SCV000255940), respectively.
Fig 1. Mutations of PAX2.
The paired domain of PAX family proteins (DNA binding domain) is well conserved among PAX family members (A). Panel B shows a partial amino acid sequence of the paired domain of PAX family proteins and PAX2 from different species. Yellow bars indicate sequences with 100% identity with human PAX1–9 and four different species. Red and blue bars indicate mutations identified in the present study and previous studies, respectively. Five mutation of PAX2 were detected in exon 2. Three out of five mutations were insertion or deletion mutation in exon 2 with frameshifts. These frameshifts created new stop codons and thus generate nonsense mutations. Two other mutations were single nucleotide mutations (ex2 c.187G>A, G63S and ex2 c.212G>C, R71T). These two mutations are shown in panels C. The 3D-structure of the paired domain is shown in panel Ci. The 3D-structure highlighted by the square in panel Ci is magnified in panel Cii. Changes in structure and electric polarity by G63S and R71T mutations are shown in panels Ciii to vi. Wild-type amino acids involved in DNA binding, glycine and arginine are shown in red. These two non-polar amino acid residues were mutated to the polar amino acid residues, serine and threonine, respectively. Blue and red highlighted amino acids in panels Cv and vi are hydrophobic and hydrophilic, respectively.
Mutations of CHD7, SALL4, KIF26B, and SIX4 were confirmed using Sanger sequencing (S1 Fig). The SALL4 variant (ex3 c.541G>A) was detected in Patient 8, and Patient 12 had multiple variants in CHD7 (ex1 c.1565G>T), KIF26B (ex12 c.55146-5167dell ACCTCGCCCCCCAGCTCCGGGG) (ClinVar accession number; SCV000255941), and SIX4 (ex1 c.1778A>T). Mutations were not detected in the other fourteen RCS cases without PAX2 mutations and in four patients with only optic nerve coloboma.
PAX2 DNA recognition site and mutations in PAX2 exon 2
The paired domain of PAX family proteins binds DNA and is well conserved among PAX proteins of humans (Fig 1A). The yellow bars in Fig 1B indicate 100% conservation of the amino acid sequences of PAX1 to 9 of humans and PAX2 of other species. Blue bars indicate known mutations, and the red bars indicate mutations in this study. Six mutation of PAX2 were detected in this study, and five of them were in exon 2. Three out of five mutations in exon 2 were insertion or deletion mutation with frameshifts. These frameshifts created new stop codons and thus generate nonsense mutations. Two other mutations were single nucleotide mutations (ex2 c.187G>A, G63S and ex2 c.212G>C, R71T) (Fig 1B). These mutations are located within the three-dimensional structure of the paired domain of PAX shown in Fig 1C. Blue and red indicate previously reported mutations and those discovered here, respectively. Red contact DNA and original amino acids are glycine and arginine (Fig 1C, S1 Movie and S2 Movie). These two non-polar amino acid residues (hydrophobic) were mutated to the polar (hydrophilic) amino acid residues serine and threonine, respectively. Mutation Taster was used to predict the pathogenicity of mutations. Almost all the identified mutations in our cases were found to have the potential to cause disease (Table 2).
Table 2. Gene mutation in renal coloboma syndrome.
| Data of Mutation Taster | Data of ExAC | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Gene | Exon | Chromosome and position (hg 19) | DNA sequence change | AA changes | Score | Summary of Mutation Taster | dbSNP | Allele Frequency | |||||
| 1 | PAX2 | 2 | chr10;102509578 102509579delGC | c.119-120delGC | cDNA. 669-670delGC | R40Hfs*13 | N/A | Prediction disease causing | Amino acid sequence changed | Frameshift | Protein features (might be) affected | Splice site changes | Not reported | - |
| 2 | PAX2 | 2 | chr10;102509578 102509579delGC | c.119-120delGC | cDNA. 669-670delGC | R40Hfs*13 | N/A | Prediction disease causing | Amino acid sequence changed | Frameshift | Protein features (might be) affected | Splice site changes | Not reported | - |
| 3 | PAX2 | 2 | chr10;102509578 102509579delGC | c.119-120delGC | cDNA. 669-670delGC | R40Hfs*13 | N/A | Prediction disease causing | Amino acid sequence changed | Frameshift | Protein features (might be) affected | Splice site changes | Not reported | - |
| 4 | PAX2 | 2 | chr10;102509578 102509579delGC | c.119-120delGC | cDNA. 669-670delGC | R40Hfs*13 | N/A | Prediction disease causing | Amino acid sequence changed | Frameshift | Protein features (might be) affected | Splice site changes | Not reported | - |
| 5 | PAX2 | 2 | chr10;102509578 102509579delGC | c.119-120delGC | cDNA. 669-670delGC | R40Hfs*13 | N/A | Prediction disease causing | Amino acid sequence changed | Frameshift | Protein features (might be) affected | Splice site changes | Not reported | - |
| 6 | PAX2 | 2 | chr10;102509671G>C | c.212G>C | cDNA. 762G>C | R71T | 71 | Prediction disease causing | Amino acid sequence changed | Known disease mutatio (pathogenic) | Protein features (might be) affected | Splice site changes | rs104894170 | No data |
| 7 | PAX2 | 2 | chr10;102509671G>C | c.212G>C | cDNA. 762G>C | R71T | 71 | Prediction disease causing | Amino acid sequence changed | Known disease mutatio (pathogenic) | Protein features (might be) affected | Splice site changes | rs104894170 | No data |
| 8 | PAX2 | 9 | chr10;102584439C>A | c.1023C>A | cDNA. 1573C>A | Y341* | 6 | Prediction disease causing | Amino acid sequence changed | Protein features (might be) affected | Splice site changes | rs78122364 | 3.30E-05 | |
| 8 | SALL4 | 3 | chr20;50408481C>T | c.541G>A | cDNA. 653G>A | V181M | 21 | Prediction disease causing | Amino acid sequence changed | Heterozygous in TGP or ExAC | Protein features (might be) affected | Splice site changes | rs139382539 | 0.0004284 |
| 9 | PAX2 | 2 | chr10;102509646G>A | c.187G>A | cDNA. 737G>A | G63S | 56 | Prediction disease causing | Amino acid sequence changed | Protein features (might be) affected | Splice site changes | Not reported | - | |
| 10 | PAX2 | 2 | chr10;102509516 102509517insGTGAACC | c.57-58insGTGAACC | cDNA.607-608insGTGAACC | Q22Rfs*34 | N/A | Prediction disease causing | Amino acid sequence changed | Frameshift | Protein features (might be) affected | Not reported | - | |
| 11 | PAX2 | 3 | chr10:102510462-102510463insAC | c.224-225insAC | cDNA.774-775insAC | G76Pfs*8 | N/A | Prediction disease causing | Amino acid sequence changed | Frameshift | Protein features (might be) affected | Splice site changes | Not reported | - |
| 12 | KIF26B | 12 | chr1:245851431-245851452delACCTCGCCCCCCAGCTCCGGGG | c.5146-5167delACCTCGCCCCCCAGCTCCGGGG | cDNA.5586-5607delACCTCGCCCCCCAGCTCCGGGG | T1716Pfs*13 | N/A | N/A | Not reported | - | ||||
| 12 | CHD7 | 1 | chr8;61655556G>T | c. 1565 G>T | cDNA. 2044G>T | G522V | 109 | Prediction disease causing | Amino acid sequence changed | Heterozygous in TGP or ExAC | Protein features (might be) affected | Splice site changes | rs142962579 | 0.002318 |
| 12 | SIX4 | 1 | chr14;61180693T>A | c.1778A>T | cDNA. 1828A>T | N593I | 149 | Prediction polymorphism | Amino acid sequence changed | Heterozygous in TGP or ExAC | Protein features (might be) affected | Splice site changes | rs77115877 | 0.002656 |
Mutation Taster (http://www.mutationtaster.org) was used to predict potential contributions of individual mutations to disease. Allele frequencies were evaluated using the ExAc database (http://exac.broadinstitute.org). N/A; not appropriate. The score of Mutation Taster is taken from the Grantham Matrix for amino acid substitutions and reflects the physicochemical difference between the original and the mutated amino acid. It ranges from 0.0 to 215 but does not provide a value for amino acid insertions/deletions. A higher Grantham score is indicative of a greater difference in chemical properties between two amino acids and can indicate a stronger effect on protein structure and function.
Clinical manifestation of RCS with or without PAX2 mutations
Among twenty-six patients clinically diagnosed with RCS, six probands (28%) had PAX2 mutations (Table 2). PAX2 mutations were undetectable in the other fifteen patients (57.7%) who were clinically diagnosed with RCS. Although 54.5% of patients with PAX2 mutations received hemodialysis, only 13.3% of those without PAX2 mutations received dialysis or received a kidney transplant (Table 3). Estimated GFR was lower in patients with PAX2 mutations (Fig 2A). Proteinuria was more severe in patients with PAX2 mutations (Fig 2B).
Table 3. Clinical manifestation of renal coloboma syndrome with/without PAX2 mutation.
| Case | Age | Gender | Coloboma | Kidney | |||||
|---|---|---|---|---|---|---|---|---|---|
| Rt | Lt | total | Gross morphology | Pathology | Function | ||||
| With PAX2 mutation | 1 | 44 | F | 1 | 3 | 4 | Normal | ND | HD |
| With PAX2 mutation | 2 | 18 | M | 1 | 1 | 2 | Malrotation | Glomerulomegaly | Cr 1.23 |
| With PAX2 mutation | 3 | 61 | F | 1 | 1 | 2 | Hypoplasia/atrophy | ND | HD |
| With PAX2 mutation | 4 | 59 | F | 3 | 4 | 7 | Malrotation | ND | Cr 1.08 |
| With PAX2 mutation | 5 | 61 | F | 1 | 2 | 3 | Hypoplasia/atrophy | ND | HD |
| With PAX2 mutation | 6 | 34 | F | 3 | 3 | 6 | Malrotation | TIN | HD |
| With PAX2 mutation | 7 | 61 | F | 3 | 2 | 5 | Hypoplasia/atrophy | ND | HD |
| With PAX2 mutation | 8 | 28 | F | 1 | 3 | 4 | ML, lt. double ureters | FSGS | Cr 1.47 |
| With PAX2 mutation | 9 | 37 | F | 3 | 1 | 4 | Hypoplasia/atrophy | Mes PGN | Cr 2.20 |
| With PAX2 mutation | 10 | 14 | M | 3 | 3 | 6 | Normal | FSGS | Cr 1.41 |
| With PAX2 mutation | 11 | 38 | M | 4 | 4 | 8 | Hypoplasia/atrophy | FSGS | HD |
| Without PAX2 mutation | 12 | 31 | F | 1 | 1 | 2 | Rt. hypoplasia/atrophy | ND | Transplantation |
| Without PAX2 mutation | 13 | 65 | M | 0 | 1 | 1 | Malrotation | IgA nephropaty | Cr 1.27 |
| Without PAX2 mutation | 14 | 76 | F | 3 | 3 | 6 | Malrotation | Glomerulomegaly | Cr 0.50 |
| Without PAX2 mutation | 15 | 27 | M | 1 | 1 | 2 | Malrotation | Glomerulomegaly | Cr 1.80 |
| Without PAX2 mutation | 16 | 11 | F | 1 | 1 | 2 | Malrotation | ND | Cr 0.50 |
| Without PAX2 mutation | 17 | 44 | F | 1 | 0 | 1 | Malrotation | ND | Cr 0.60 |
| Without PAX2 mutation | 18 | 51 | F | 0 | 1 | 1 | Hypoplasia/atrophy | ND | Cr 1.07 |
| Without PAX2 mutation | 19 | 65 | M | 1 | 0 | 1 | Hypoplasia/atrophy | ND | Cr 1.97 |
| Without PAX2 mutation | 20 | 43 | F | 1 | 0 | 1 | Hypoplasia/atrophy | ND | Cr 4.31 |
| Without PAX2 mutation | 21 | 37 | M | 1 | 0 | 1 | Hypoplasia/atrophy | MCNS | Cr 2.26 |
| Without PAX2 mutation | 22 | 60 | F | 0 | 1 | 1 | Malrotation | ND | Cr 0.69 |
| Without PAX2 mutation | 23 | 66 | M | 1 | 0 | 1 | Rt. hypoplasia/atrophy | ND | Cr 1.57 |
| Without PAX2 mutation | 24 | 52 | F | 1 | 0 | 1 | Rt. hypoplasia/atrophy | ND | CAPD |
| Without PAX2 mutation | 25 | 47 | M | 1 | 1 | 2 | Malrotation | ND | Cr 1.17 |
| Without PAX2 mutation | 26 | 63 | M | 1 | 1 | 2 | Rt. hypoplasia/atrophy | ND | Cr 0.83 |
| Coloboma only | 27 | 29 | F | 1 | 1 | 2 | Normal | ND | Cr 0.70 |
| Coloboma only | 28 | 30 | F | 1 | 0 | 1 | Normal | ND | Cr 0.60 |
| Coloboma only | 29 | 73 | F | 1 | 1 | 2 | Normal | ND | Cr 0.60 |
| Coloboma only | 30 | 65 | F | 1 | 0 | 1 | Normal | ND | Cr 0.51 |
Optic nerve coloboma of each eye was scored 0 to 4 (Score 0, normal optic disc to score 4, severe c olobomma). Kidney abnormality of gross morphology, pathology, and function are summarized. ND; not done, FSGS; focal segmental glomerulosclerosis, Mes PGN; mesangial proliferative glomerulonephritis, MCNS; minimal change nephrotic syndrome.
Fig 2. Clinical manifestation of kidney in patients with PAX2 mutations.
PAX2 mutations substantially contribute to the renal manifestations of RCS. In patients without dialysis or kidney transplantation, estimated GFR were lower in patients with PAX2 mutations (A), and proteinuria was more severe in patients with PAX2 mutations (B). Histology of a renal biopsy specimen from Patient 8 is shown in panel C.A representative segmental sclerosing lesion is observed at a glomerulus by PAS (i, ii) and PAM (iii) staining. Original magnifications; panel I, ×100; planes ii and iii, ×400. Panel iv shows a representative image from transmission electron microscopy at an original magnification of ×3,000. Foot process effacement is observed without evidence of immune deposits. Scale bars represent 100 μm in light microscopy images and 5 μm in electron microscopy images. Values represent the mean ± SEM. *, p < 0.05 vs. “Coloboma only”. “RCS with PAX2 mutations” indicates clinically diagnosed renal-coloboma syndrome cases with PAX2 gene mutations (n = 5), “RCS without PAX2 mutations” indicates clinically diagnosed renal-coloboma syndrome cases without PAX2 gene mutations (n = 13), and “Coloboma only” indicates cases with optic nerve coloboma and no kidney abnormality (a disease control; n = 4).
Kidney biopsies were acquired from nine of twenty-six clinically diagnosed patients with RCS. Five patients had PAX2 mutations, and PAX2 mutations were undetectable in four patients. Three of five patients with PAX2 mutations had FSGS (Table 3, Fig 2C), and the other two had glomerulomegaly or non-IgA mesangial proliferative glomerulonephritis. However, the four patients without PAX2 mutations did not have FSGS, two had glomerulomegaly, and one each had IgA nephropathy or minimal change nephrotic syndrome.
Thirteen and six patients had bilateral or monolateral typical ocular coloboma, respectively. The coloboma scores were significantly higher in patients with PAX2 mutations (Table 3, Fig 3). However, the degree of kidney dysfunction and coloboma varied, even among patients with the same PAX2 mutation.
Fig 3. Optic nerve coloboma was severe in patients with PAX2 mutations.
Representative images of coloboma scores 0–4 are shown in panel A. Score 0, normal optic disc; Score 1, optic disc dysplasia with an unusual pattern of the retinal vessels and cilioretinal arteries; Score 2, optic disc pit associated with vascular abnormalities and a cilioretinal artery; Score 3, large coloboma involving the entire surface of the optic disc; Score 4, large coloboma of the optic disc and adjacent retina, or morning glory anomaly (with radial emergence of the retinal vessels). The mean coloboma scores of each group are shown in panel B. The coloboma scores (total, right and left eye) were significantly higher in patients with PAX2 mutations. Values represent the mean ± SEM. *, p < 0.05 vs. coloboma scores of patients without PAX2 mutations. “RCS with PAX2 mutations” indicates clinically diagnosed renal-coloboma syndrome cases with PAX2 gene mutations (n = 11), “RCS without PAX2 mutations” indicates clinically diagnosed renal-coloboma syndrome cases without PAX2 gene mutations (n = 15), and “Coloboma only” indicates cases with optic nerve coloboma and no kidney abnormality (a disease control; n = 4).
Patients 8 and 12 had variants in other genes. Patient 8 had SALL4 variant. Patient 12 with severe kidney dysfunction had three variants (KIF26B, CHD7, and SIX4) and subsequently received a kidney transplant (Tables 2 and 3).
Familial cases with PAX2 mutations
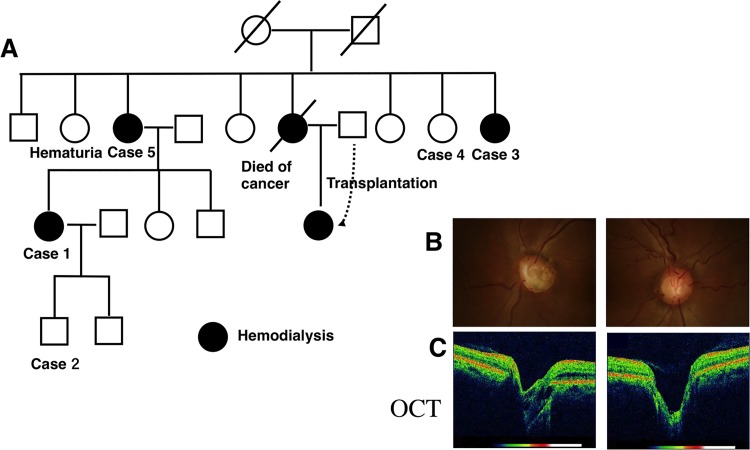
Patients 1–5 represented one family cohort with the same novel PAX2 mutation ex2 c. 119-120delGC (Table 2, Fig 4). Patients 1, 3, and 5 received hemodialysis. Although Patient 4 was the sister of Patients 3 and 5, who all had the same PAX2 mutation, her kidney dysfunction was mild (Cr 1.24 mg/dl). Patient 1 had a visual disability with some visual field defects. She and her son (Patient 2, 18 years of age) had bilateral optic nerve coloboma, and they each had the same PAX2 mutation. The left eye of Patient 1 was the most severely affected (coloboma scores: Patient 1, right eye score = 1, left eye score = 3; Patient 2, right eye score = 1, left eye score = 2 (Fig 4).
Fig 4. Pedigree of the family with RCS with PAX2 mutations.
Pedigree of the family with RCS showing classical autosomal dominant inheritance across three generations. ☐, males; ❍, females; ●, female patients receiving hemodialysis. A diagonal line through a symbol means a patient is deceased.Ocular fundal images of Patient 1 (B, C) indicate that she had ocular coloboma (coloboma scores: right eye = 1, left eye = 3). Cross-sectional images of the optic disc acquired using optical coherence tomography (OCT) show deep excavation in both eyes (C).
The second family cohort included Patient 6 and her mother, Patient 7. They had a heterozygous PAX2 mutation c.212G>C in exon 2 that creates the missense mutation R71T. Patient 6 previously reported as a case of acro-renal-ocular syndrome [17]. These patients received hemodialysis and had very severe ocular coloboma (coloboma scores: Patient 6, right eye score = 3, left eye score = 3; Patient 7, right eye score = 3, left eye score = 2).
Discussion
In the present study, we screened the nucleotide sequences of PAX2 and those of 25 other genes and identified PAX2 mutations, including four mutations that are novel, in 6 out of 21 probands who were clinically diagnosed with RCS (28%). Moreover, we detected four sequence variants in other genes, including a novel KIF26B mutation.PAX2 mutations manifest as clinical abnormalities of the kidneys and eyes, and mutations in other genes may exert the same effects. The most significant findings of the present study are as follows: 1. Mutations in genes other than PAX2 may contribute to the pathogenesis of RCS; 2. We present an analysis of a series of kidney biopsies of patients with RCS; and 3. Factors other than PAX2 mutations may contribute to the progression of kidney and eye abnormalities in patients with RCS.
Of the 21 probands with RCS characterized here, 6 (28%) had PAX2 mutations, and two further patients had sequence variants in other genes, including one patient with a novel KIF26B mutation. Approximately 50% cases of RCS have no PAX2 mutations[14]; however, no other mutations are reported. We detected four non-PAX2 sequence variants in our cases of RCS. Among them, we detected KIF26B mutation that have not been reported, to our knowledge, in patients with RCS. The allele frequency of CHD7, SIX4, and SALL4 sequence variants were 0.04–0.2% and may therefore represent polymorphisms. Therefore, these sequence variants would not be considered to be pathogenic[18, 19]. In contrast, KIF26B, which encodes a member of the kinesin family of motor proteins, exerts a major effect on development [20]. Thus, KIF26B-deficient mice exhibit neonatal lethality with impaired kidney development towing to the loss of cortical nephrogenic zone mesenchyme and the failure of ureteric buds to invade and branch into the mesenchyme. To the best of our knowledge, the present study is the first to detect a KIF26B mutation in humans with kidney dysfunction. The novel KIF26B sequence variant, which was a 22bp deletion affecting exon 12 of KIF26B, and was predicted to cause a frameshift mutation prior to the termination of the coding region of KIF26B in exon 15, would be damaging to the protein. Because patient 12 with the KIF26B variant did not have a PAX2 mutation, this mutation is potentially the causative mutation in this patient. Our patient with the KIF26B mutation developed kidney dysfunction and eventually received a kidney transplant. Further studies of renal coloboma syndrome that analyze exosome or whole genome sequences are required to detect gene mutation in this syndrome and mutation in other genes of patients with RCS.
Our analysis of kidney biopsies from nine of 26 patients with RCS reveal that five harborPAX2 mutations. Three of five patients with PAX2 mutations, but not those without, exhibited FSGS. Previous analyses of the biopsies of patients indicate that re-expression of PAX2 by podocytes is an early marker of FSGS [21]. Moreover, proliferating parietal epithelial cells that express PAX2 and cytokeratin may contribute to FSGS [22]. Moreover, a PAX2 mutation contributes to adult-onset FSGS, and 4% of patients with FSGS harbor the PAX2 mutation [23]. Here we show that 60% of patients with PAX2 mutations had FSGS, indicating that although the mechanisms of FSGS progression are not defined, PAX2 may play a critical role in disease progression.
We report here two families with PAX2 mutations (Case1 to 5 and Case6, 7) in this manuscript. Each member of one family (Case1 to 5) had one PAX2 mutation (c.119-120delGC), and each member of another family (Case6 and 7) had the other PAX2 mutation (c.212G>C). Although each family member had the same PAX2 mutation, the extent of kidney dysfunction differed significantly among them. Vesicoureteral reflux (VUR) is an important factor when considering determinants of renal dysfunction of patients with RCS [24]. PAX2 mutations contribute to the kidney and urinary tract development, and participate in VUR. Minor VUR can cause renal failure and kidney scarring over time. In addition to various pathological glomerular changes, the severity of VUR may explain the differences in kidney dysfunction between subjects with the same PAX2 mutation.
Ocular involvement is present in patients with PAX2 mutations [25, 26], and bilateral optic nerve coloboma is typically associated with RCS. Optic nerve or disc dysplasia, microphthalmia, morning glory anomaly, optic nerve cysts, scleral staphyloma, myopia, nystagmus, and cataracts were observed as well [27, 28]. Our data reveal that optic nerve coloboma was more severe in patients with PAX2 mutations. However, the degree of optic nerve coloboma varied between patients or between each eye of an individual, although patients had the same PAX2 mutation. Moreover, a recent study reveals that even identical twins with PAX2 mutations show different eye and kidney abnormalities [29]. Consistent with the present data, others suggest that point mutations within the coding region of PAX2 may not represent the only cause of RCS [14].These findings indicate that other factors may exert additive effects on the progression of kidney and eye dysfunctions.
This study had some limitations. Parental studies are necessary to understand the contribution of genetic mutations to clinical phenotypes. However, the approved protocol of the present study did not include parents without the clinical manifestations of RCS. Therefore, we aim to include parental studies in our future studies. Secondly, family bias may have been present in this study. As RCS is very rare, we included as many cases as possible. Therefore, two families (of 5 and 2 cases, respectively) were included in this study. As there were significant differences in clinical ocular and renal manifestations between individual family members with identical gene mutations [23, 30, 31], family bias may have affected the analysis conducted in the present study. Moreover, the patient numbers in this study are very small, and that even just a small phenotypic bias can sway the analysis one way or the other. Therefore conclusions from this study can only be very tentative. Additional familial cases are required to adequately reduce this potential source of bias.
Our data indicate that PAX2 mutation is a key abnormality in RCS and may make a major contribution to the pathogenesis of kidney and eye abnormalities. However, other factors and gene mutations may play a role, and further human and animal studies will be required to define the mechanism of pathogenesis of RCS.
Supporting Information
To detect mutations associated with renal coloboma syndrome (RCS), 26 patients with RCS and 4 patients with optic nerve coloboma only were screened using next-generation sequence analysis. Detected candidate mutations were confirmed using Sanger sequencing. Mutation c.5146-5167delACCTCGCCCCCCAGCTCCGGGG in KIF26B was detected in exon 12. Similarly, mutation c.1565 G>T in CHD7 was detected in exon 1, mutation c.569 T>A in SIX4 was detected in exon 1, and mutation c.2814 C>T in SALL4 was detected in exon 3.
(PPT)
3D-structure images are shown in Fig 1 Ci-iv and Cv-vi, respectively. The 3D-structure of the paired domain is shown in S1 Movie. Changes in structure by G63S and R71T mutations are shown. Wild-type amino acids involved in DNA binding, glycine and arginine, are shown in red. These two non-polar amino acid residues were mutated to the polar amino acid residues, serine and threonine, respectively.
(MOV)
3D-structure images are shown in Fig 1 Ci-iv and Cv-vi, respectively. The 3D-structure of the paired domain is shown in S2 Movie. Changes in electric polarity by G63S and R71T mutations are shown. Amino acids highlighted in blue and red are hydrophobic and hydrophilic, respectively.
(MOV)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported in part by Grants-in-Aids from the Ministry of Education, Culture, Sports, Science, and Technology of the Japanese Government (#22590883, #26293126, #15K15328). There was no additional external funding received for this study.
References
- 1. Cunliffe HE, McNoe LA, Ward TA, Devriendt K, Brunner HG, Eccles MR. The prevalence of PAX2 mutations in patients with isolated colobomas or colobomas associated with urogenital anomalies. J Med Genet. 1998;35(10):806–12. Epub 1998/10/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Torban E, Eccles MR, Favor J, Goodyer PR. PAX2 suppresses apoptosis in renal collecting duct cells. Am J Pathol. 2000;157(3):833–42. Epub 2000/09/12. doi: S0002-9440(10)64597-X [pii] 10.1016/S0002-9440(10)64597-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sanyanusin P, McNoe LA, Sullivan MJ, Weaver RG, Eccles MR. Mutation of PAX2 in two siblings with renal-coloboma syndrome. Hum Mol Genet. 1995;4(11):2183–4. Epub 1995/11/01. . [DOI] [PubMed] [Google Scholar]
- 4. Porteous S, Torban E, Cho NP, Cunliffe H, Chua L, McNoe L, et al. Primary renal hypoplasia in humans and mice with PAX2 mutations: evidence of increased apoptosis in fetal kidneys of Pax2(1Neu) +/- mutant mice. Hum Mol Genet. 2000;9(1):1–11. Epub 1999/12/10. doi: ddd014 [pii]. . [DOI] [PubMed] [Google Scholar]
- 5. Dziarmaga A, Quinlan J, Goodyer P. Renal hypoplasia: lessons from Pax2. Pediatr Nephrol. 2006;21(1):26–31. Epub 2005/11/08. 10.1007/s00467-005-2039-x . [DOI] [PubMed] [Google Scholar]
- 6. Clark P, Dziarmaga A, Eccles M, Goodyer P. Rescue of defective branching nephrogenesis in renal-coloboma syndrome by the caspase inhibitor, Z-VAD-fmk. Journal of the American Society of Nephrology: JASN. 2004;15(2):299–305. Epub 2004/01/30. . [DOI] [PubMed] [Google Scholar]
- 7. Bower M, Salomon R, Allanson J, Antignac C, Benedicenti F, Benetti E, et al. Update of PAX2 mutations in renal coloboma syndrome and establishment of a locus-specific database. Hum Mutat. 2012;33(3):457–66. Epub 2012/01/04. 10.1002/humu.22020 . [DOI] [PubMed] [Google Scholar]
- 8. Dureau P, Attie-Bitach T, Salomon R, Bettembourg O, Amiel J, Uteza Y, et al. Renal coloboma syndrome. Ophthalmology. 2001;108(10):1912–6. Epub 2001/10/03. doi: S0161-6420(01)00722-9 [pii]. . [DOI] [PubMed] [Google Scholar]
- 9. Reidy KJ, Rosenblum ND. Cell and molecular biology of kidney development. Semin Nephrol. 2009;29(4):321–37. 10.1016/j.semnephrol.2009.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gong KQ, Yallowitz AR, Sun H, Dressler GR, Wellik DM. A Hox-Eya-Pax complex regulates early kidney developmental gene expression. Mol Cell Biol. 2007;27(21):7661–8. 10.1128/MCB.00465-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abraham S, Paknikar R, Bhumbra S, Luan D, Garg R, Dressler GR, et al. The Groucho-associated phosphatase PPM1B displaces Pax transactivation domain interacting protein (PTIP) to switch the transcription factor Pax2 from a transcriptional activator to a repressor. J Biol Chem. 2015;290(11):7185–94. 10.1074/jbc.M114.607424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Patel SR, Ranghini E, Dressler GR. Mechanisms of gene activation and repression by Pax proteins in the developing kidney. Pediatr Nephrol. 2014;29(4):589–95. 10.1007/s00467-013-2603-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brodbeck S, Englert C. Genetic determination of nephrogenesis: the Pax/Eya/Six gene network. Pediatr Nephrol. 2004;19(3):249–55. 10.1007/s00467-003-1374-z . [DOI] [PubMed] [Google Scholar]
- 14. Schimmenti LA. Renal coloboma syndrome. European journal of human genetics: EJHG. 2011;19(12):1207–12. 10.1038/ejhg.2011.102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Higashide T, Wada T, Sakurai M, Yokoyama H, Sugiyama K. Macular abnormalities and optic disk anomaly associated with a new PAX2 missense mutation. Am J Ophthalmol. 2005;139(1):203–5. Epub 2005/01/18. doi: S0002-9394(04)00870-0 [pii] 10.1016/j.ajo.2004.07.021 . [DOI] [PubMed] [Google Scholar]
- 16. Schimmenti LA, Cunliffe HE, McNoe LA, Ward TA, French MC, Shim HH, et al. Further delineation of renal-coloboma syndrome in patients with extreme variability of phenotype and identical PAX2 mutations. Am J Hum Genet. 1997;60(4):869–78. Epub 1997/04/01. [PMC free article] [PubMed] [Google Scholar]
- 17. Naito T, Kida H, Yokoyama H, Abe T, Takeda S, Uno D, et al. Nature of renal involvement in the acro-renal-ocular syndrome. Nephron. 1989;51(1):115–8. Epub 1989/01/01. . [DOI] [PubMed] [Google Scholar]
- 18. Grifone R, Demignon J, Houbron C, Souil E, Niro C, Seller MJ, et al. Six1 and Six4 homeoproteins are required for Pax3 and Mrf expression during myogenesis in the mouse embryo. Development. 2005;132(9):2235–49. 10.1242/dev.01773 . [DOI] [PubMed] [Google Scholar]
- 19. Ozaki H, Nakamura K, Funahashi J, Ikeda K, Yamada G, Tokano H, et al. Six1 controls patterning of the mouse otic vesicle. Development. 2004;131(3):551–62. 10.1242/dev.00943 . [DOI] [PubMed] [Google Scholar]
- 20. Uchiyama Y, Sakaguchi M, Terabayashi T, Inenaga T, Inoue S, Kobayashi C, et al. Kif26b, a kinesin family gene, regulates adhesion of the embryonic kidney mesenchyme. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(20):9240–5. 10.1073/pnas.0913748107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ohtaka A, Ootaka T, Sato H, Soma J, Sato T, Saito T, et al. Significance of early phenotypic change of glomerular podocytes detected by Pax2 in primary focal segmental glomerulosclerosis. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2002;39(3):475–85. 10.1053/ajkd.2002.31391 . [DOI] [PubMed] [Google Scholar]
- 22. Hill GS, Karoui KE, Karras A, Mandet C, Duong Van Huyen JP, Nochy D, et al. Focal segmental glomerulosclerosis plays a major role in the progression of IgA nephropathy. I. Immunohistochemical studies. Kidney international. 2011;79(6):635–42. 10.1038/ki.2010.466 . [DOI] [PubMed] [Google Scholar]
- 23. Barua M, Stellacci E, Stella L, Weins A, Genovese G, Muto V, et al. Mutations in PAX2 associate with adult-onset FSGS. Journal of the American Society of Nephrology: JASN. 2014;25(9):1942–53. 10.1681/ASN.2013070686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Eccles MR, Bailey RR, Abbott GD, Sullivan MJ. Unravelling the genetics of vesicoureteric reflux: a common familial disorder. Hum Mol Genet. 1996;5 Spec No:1425–9. Epub 1996/01/01. . [DOI] [PubMed] [Google Scholar]
- 25. Amiel J, Audollent S, Joly D, Dureau P, Salomon R, Tellier AL, et al. PAX2 mutations in renal-coloboma syndrome: mutational hotspot and germline mosaicism. European journal of human genetics: EJHG. 2000;8(11):820–6. Epub 2000/11/28. 10.1038/sj.ejhg.5200539 . [DOI] [PubMed] [Google Scholar]
- 26. Eccles MR, Schimmenti LA. Renal-coloboma syndrome: a multi-system developmental disorder caused by PAX2 mutations. Clin Genet. 1999;56(1):1–9. Epub 1999/08/31. . [DOI] [PubMed] [Google Scholar]
- 27. Schimmenti LA, Manligas GS, Sieving PA. Optic nerve dysplasia and renal insufficiency in a family with a novel PAX2 mutation, Arg115X: further ophthalmologic delineation of the renal-coloboma syndrome. Ophthalmic Genet. 2003;24(4):191–202. Epub 2003/10/21. . [DOI] [PubMed] [Google Scholar]
- 28. Cheong HI, Cho HY, Kim JH, Yu YS, Ha IS, Choi Y. A clinico-genetic study of renal coloboma syndrome in children. Pediatr Nephrol. 2007;22(9):1283–9. Epub 2007/06/02. 10.1007/s00467-007-0525-z . [DOI] [PubMed] [Google Scholar]
- 29. Iatropoulos P, Daina E, Mele C, Maranta R, Remuzzi G, Noris M. Discordant phenotype in monozygotic twins with renal coloboma syndrome and a PAX2 mutation. Pediatr Nephrol. 2012;27(10):1989–93. Epub 2012/06/05. 10.1007/s00467-012-2205-x . [DOI] [PubMed] [Google Scholar]
- 30. Taranta A, Palma A, De Luca V, Romanzo A, Massella L, Emma F, et al. Renal-coloboma syndrome: a single nucleotide deletion in the PAX2 gene at Exon 8 is associated with a highly variable phenotype. Clin Nephrol. 2007;67(1):1–4. . [DOI] [PubMed] [Google Scholar]
- 31. Ford B, Rupps R, Lirenman D, Van Allen MI, Farquharson D, Lyons C, et al. Renal-coloboma syndrome: prenatal detection and clinical spectrum in a large family. Am J Med Genet. 2001;99(2):137–41. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
To detect mutations associated with renal coloboma syndrome (RCS), 26 patients with RCS and 4 patients with optic nerve coloboma only were screened using next-generation sequence analysis. Detected candidate mutations were confirmed using Sanger sequencing. Mutation c.5146-5167delACCTCGCCCCCCAGCTCCGGGG in KIF26B was detected in exon 12. Similarly, mutation c.1565 G>T in CHD7 was detected in exon 1, mutation c.569 T>A in SIX4 was detected in exon 1, and mutation c.2814 C>T in SALL4 was detected in exon 3.
(PPT)
3D-structure images are shown in Fig 1 Ci-iv and Cv-vi, respectively. The 3D-structure of the paired domain is shown in S1 Movie. Changes in structure by G63S and R71T mutations are shown. Wild-type amino acids involved in DNA binding, glycine and arginine, are shown in red. These two non-polar amino acid residues were mutated to the polar amino acid residues, serine and threonine, respectively.
(MOV)
3D-structure images are shown in Fig 1 Ci-iv and Cv-vi, respectively. The 3D-structure of the paired domain is shown in S2 Movie. Changes in electric polarity by G63S and R71T mutations are shown. Amino acids highlighted in blue and red are hydrophobic and hydrophilic, respectively.
(MOV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.