Summary
The course of cystic fibrosis (CF) progression in children is affected by parent adherence to treatment plans. The Theory of Reasoned Action (TRA) posits that intentions are the best behavioral predictors and that intentions reasonably follow from beliefs (“determinants”). Determinants are affected by multiple “background factors,” including spirituality. This study’s purpose was to understand whether two parental adherence determinants (attitude towards treatment and self-efficacy) were associated with spirituality (religious coping and sanctification of the body). We hypothesized that parents’ attitudes toward treatment adherence are associated with these spiritual constructs. A convenience sample of parents of children with CF aged 3–12 years (n = 28) participated by completing surveys of adherence and spirituality during a regular outpatient clinic visit. Type and degree of religious coping was examined using principal component analysis. Adherence measures were compared based on religious coping styles and sanctification of the body using unpaired t-tests. Collaborative religious coping was associated with higher self-efficacy for completing airway clearance (M = 1070.8; SD = 35.8; P = 0.012), for completing aerosolized medication administration (M = 1077.1; SD = 37.4; P = 0.018), and for attitude towards treatment utility (M = 38.8; SD = 2.36; P = 0.038). Parents who attributed sacred qualities to their child’s body (e.g., “blessed” or “miraculous”) had higher mean scores for self-efficacy (airway clearance, M = 1058.6; SD = 37.7; P = 0.023; aerosols M = 1070.8; SD = 41.6; P = 0.020). Parents for whom God was manifested in their child’s body (e.g., “My child’s body is created in God’s image”) had higher mean scores for self-efficacy for airway clearance (M = 1056.4; SD = 59.0; P = 0.039), aerosolized medications (M = 1068.8; SD = 42.6; P = 0.033) and treatment utility (M = 38.8; SD = 2.4; P = 0.025). Spiritual constructs show promising significance and are currently undervalued in chronic disease management.
Keywords: Theory of Reasoned Action, treatment utility, self-efficacy, religious coping, sanctification of the body
INTRODUCTION
Poor adherence to recommended medical treatments exacerbates the course of cystic fibrosis (CF) and is associated with shortened life span due to decreased lung functioning, poorer health-related quality of life, more frequent hospitalizations and emergency department use, as well as increased costs to families and patients.1–3 Adherence among children and adolescents with CF has been shown to be as low as 40–47% for some airway clearance techniques and 36% for nebulized therapies.4–6 Adherence to airway clearance and nebulized therapies is critical because lung function is a robust predictor of mortality and survival in CF and are deemed important enough to have practice guidelines.7–10
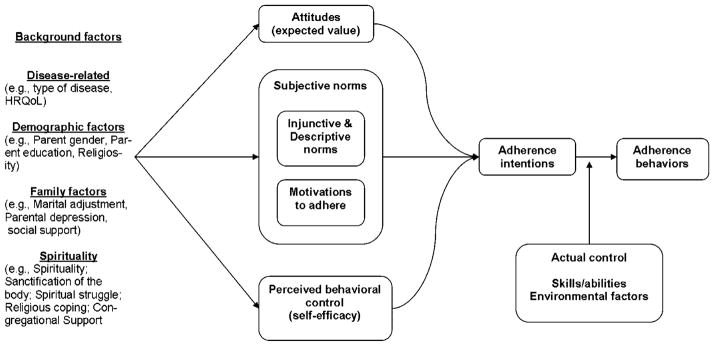
In order to improve adherence, it is first necessary to understand the drivers of adherence behaviors for parents of chronically ill children. The Theory of Reasoned Action (TRA; Fig. 1) is a frequently used conceptual model for understanding adherence behavior and has been applied across a variety of populations, including attention deficit hyperactivity disorder, hypertension, and diabetes.2,3,11 Briefly, the TRA posits that the best predictor of whether someone will perform a behavior is their intentions. One’s intentions follow in a reasonable and consistent manner from their beliefs about that behavior. Their beliefs are composed three dimensions: their attitudes about the behavior’s value; their perceptions about whether important other people in their lives think the behavior should be done—and whether they themselves do the behavior; and, finally, beliefs about their competence and capability of carrying out the behavior (self-efficacy). Collectively, these three beliefs are referred to as the “determinants” of intentions. Self-efficacy has been shown to be a necessary but not sufficient criteria for dietary adherence among mothers of children with CF (Anthony), and a predictor of self-management behaviors12 and effective monitoring of respiratory problems.13 Self-efficacy was inversely related to maternal depression.14 Two mechanisms of action have been proposed: a direct effect on behavior, and an inverse effect on stress responses.15
Fig. 1.
Theory of Reasoned Action (TRA).
Adherence determinants are formed by “background factors,” including demographics, disease severity, mood, and spirituality. Spirituality and religion are related, but different concepts. Both are defined as the “feelings, thoughts, experiences, and behaviors that arise from a search for the sacred.”16 Religion is distinguished from spirituality by its inherent organizational nature—that the “means and methods (e.g., rituals or prescribed behaviors) of the search receive validation and support from within an identifiable group of people.”17 Spirituality is thought of as more personal and internal, whereas religiosity is generally understood to be observable aspects of religion—often organizationally related. Just as race is considered a “marker variable” of sociological processes (e.g., discrimination, educational attainment), so religion, here, is considered a marker variable of spiritual process. The two are not necessarily interchangeable, and it is the spiritual factors that are thought to be related to adherence (via attitudes, norms, and self-efficacy) rather than religious affiliation or congregational attendance.
Spirituality is a background factor that has been largely overlooked in the study of adherence in general, as well as in CF. This is surprising given the importance of spirituality and religion to a significant proportion of the American population. According to 2008 Gallup data, 93% of respondents believe in God or a universal spirit.18 Spirituality/religion may play varied roles in different racial/ethnic groups. They have particular salience among African-Americans,19 who are much more likely to say that religion is very important in their lives (85%) compared to their Caucasian counterparts (56%).20 Prayer was the most frequently used form of non-medical treatment in a study of adults with CF, demonstrating its relevance in this primarily Caucasian population.21 Further, research suggests that spirituality and religion are important constructs for understanding health behaviors among older adolescents and adults with CF and other chronic diseases, as well as parental adaptation to the diagnosis of CF.22–27
Adherence is associated with spirituality in adult patients. HIV-positive (HIV+), predominately African-American adults participating in a qualitative study of barriers and facilitators of adherence stated that prayer and spirituality facilitated adherence.22 Kemppainen et al.26 found an association between an HIV+ patient’s attribution of their disease (chance, luck, or God’s will) and adherence. Attribution of one’s health being in God’s control was negatively associated with adherence to antiretroviral therapy among HIV+ adults.28 Parsons et al.23 found that in an HIV+ population of adults, religious beliefs were both positively and negatively correlated with adherence. There were no racial/ethnic differences between how African-American or Caucasian participants used religious coping to construct the meaning that HIV was a punishment from God.23,29 A study of adults with heart failure demonstrated that situations perceived as challenges to one’s moral-ethical-spiritual self were positively associated with increased adherence to treatment regimens.24 Adherence has been shown to be affected by a patient’s trust in their physician, which is mediated by religious variables, among others.30
Interventions with a spiritual basis have demonstrated positive outcomes among adults with chronic diseases and in a general population of young adults. A spiritually based intervention for HIV adults combining Buddhist religious practices and cognitive behavior therapy demonstrated increased treatment motivations and adherence.31 A randomized clinical trial of women with breast cancer reported increased spiritual well-being and improved quality of life among women who received an intervention that included different views of healing, forgiveness, and guided imagery32—all of which have spiritual roots. Texts of an on-line support group consisting of women with breast cancer showed that increased use of religious language—words, such as pray, worship, faith, holy—was associated with lower negative emotion, self-efficacy, and functional well-being, after controlling for level of religiosity.33 An 8-session spiritual intervention rooted in theistic concepts common to the five major world monotheistic traditions (Judaism, Christianity, Islam, Zoroastrianism, and Sikkhism) demonstrated increases in both positive religious coping and spiritual well-being among female sexual abuse survivors).34 Although these studies provide convincing evidence that adherence and spirituality are associated in adult patients, their interplay for parents of chronically ill children has not been studied.
The relationship between parenting and religion is generally associated with positive parental and marital functioning in healthy samples.35 However, when parental assumptions about life are violated, as in the diagnosis of their child with a genetic, life-shortening disease, personal and interpersonal emotional, religious, and spiritual struggles may occur.35 Hexem et al.36 described both positive and negative experiences of religion and spirituality among parents of pediatric palliative care patients, and noted that it plays an important role in most of the parents in their study. Tarakeshwar and Pargament’s37 study of mothers of children with autism described negative maternal emotions and spiritual struggles (abandonment by God and by the church). These struggles were predictive of increased anxiety and depression. Parents of children with sickle cell disease used both positive forms of religious coping (seeking comfort/intimacy with the Divine and constructing meaning by reframing the event) and negative forms of religious coping (reframing event as God’s Punishment or an act of the devil).38 Parents of children diagnosed with CF have previously been shown to use religious coping in three ways: to gain control/problem-solve; to seek comfort/intimacy; and to construct meaning of their experience.39 Religious coping by parents has also been documented in a qualitative study of prayers written in an open-format notebook in a pediatric hospital chapel, primarily expressing parental coping by seeking comfort/intimacy with God.40 Other studies have also shown that parents use religious coping with their child’s chronic illness to reframe their child’s disease or their role35,41,42 and use religious rituals to cope.35
In this study, we operationalized spirituality using two spiritual constructs: sanctification of the body and Religious coping. Sanctification of the body means imbuing the body with sacred significance and has been related to healthy behaviors in other populations.43 Religious coping is defined as “the search for significance, in ways related to the sacred, during times of stress.”44 These two constructs were selected because of previous associations with health and the possibility that they mediate the effect of religious beliefs on health.45 Many religious traditions understand the body to have a sacred significance.43,46 Mahoney et al.43 described the spiritual construct of “sanctification” in which an object or role is given sacred significance. Sanctification of the body is consists of two distinct but related dimensions. One of these, manifestation of God in the body, taps religious constructs (e.g., “My child’s body is created in God’s image.”). The other, sacred qualities of the body, taps spiritual constructs not necessarily associated with a monotheistic deity (e.g., agreement with the extent to which one sees their child’s body as “blessed” or “miraculous”).43 Mahoney et al.43 reported a relationship between pro-healthy behavior and sanctification of the body in older adolescent/young adult college students. In that study, higher levels of body sanctification were associated with higher levels of pro-healthy behavior (e.g., strenuous exercise and body satisfaction) and with lower levels of alcohol and illegal drug use, and unhealthy eating. In another study of sanctification, this time of sexual relationships among college students, increased sanctification was related to sexual behavior, lending further support to the role of sanctification in the pursuit of positive goals.47 Grossoehme et al.48 found evidence that parents of children with CF do sanctify their children’s bodies. In this study of 92 parents of children with CF, mean levels for manifestation of God in the body subscale were 5.47 (SD = 1.45; on a 7-point Likert-style scale) and 5.97 (SD = 1.37) for the Sacred Qualities of the Body subscale. These means were similar in magnitude and direction to those published elsewhere,43 except that scores on the Sacred Qualities of the Body subscale were higher among parents of children with CF, suggesting that they saw their child’s body as something very special. This led to formulating the hypothesis that parental sanctification of their child’s body would be related to their attitudes about the value of adherence to their child’s daily recommended home treatments. Together, these studies suggested that sanctification of their child’s body might be a mediator of their pro-healthy behaviors on behalf of their child. We hypothesized that higher levels of sanctification of their child’s body would be related to injunctive norms—parent’s perceptions of how they are expected to care for their child’s body.
Religious coping is another potential construct affecting adherence determinants. We focused on religious coping styles whose goal was to gain control of a stressor.44 These are: Collaborative (seeking control through a partnership with God in problem-solving); Deferral (passive waiting for God to control the situation); Active Surrender (relinquishing one’s will to God’s will to solve the problem); Pleading (seeking control by God through asking for divine intervention); and Self-directed (problem-solving directly through individual initiative rather than help through God). Religious coping has numerous associations, both positive and negative, with health.31,40 Self-directed religious coping mediated the relationship between religious beliefs and general alcohol use among college undergraduates.49 Self-directed religious coping was also negatively correlated with African-American men’s intentions to be screened for prostate cancer.50 Poorer psychosocial outcomes were associated with both self-directed and pleading styles among those recovering from mental health conditions; on the other hand, collaborative religious coping was associated with increased involvement in recovery-enhancing activities and empowerment in a sample of adults with serious mental illness.51 Pleading religious coping (asking for divine intervention), associated with depression and negative affect, may be elicited in situations where limited control is perceived.44,52 Pleading is also related to stress-related psychological growth and general health outcomes, suggesting that it serves as a means of experiencing some mastery of a situation through one’s relationship with God.44,52 These studies suggest that religious coping for control may be associated with determinants of parental adherence.
Spirituality is a multi-dimensional construct that has been under-explored in relationship to adherence issues, particularly so in the case of adherence by parents when a child has a chronic illness. While the literature cited above shows a relationship between spiritual constructs in adult samples in the case of their own chronic illness, understanding parental spirituality’s contribution to determinants of health-related behaviors is unexplored. Improving understanding of parental spirituality affords an opportunity to help individuals with beliefs to draw on them in ways that could lead to improved adherence to recommended treatments. This is significant because it has the potential to open a new avenue for developing and delivering strategies to optimize adherence.
Using the TRA as a conceptual framework, the specific aim of this study was to determine the relationship between two determinants of parental adherence (attitudes toward treatment utility and self-efficacy) and spiritual constructs. We hypothesized a positive association between these two determinants of adherence (attitudes toward treatment utility and self-efficacy) and the parental spiritual constructs of religious coping and sanctification of the body.
MATERIALS AND METHODS
Participants
Participants were recruited from an accredited CF center serving patients from a multi-state area. The study was approved by the Institutional Review Board, and informed consent was obtained. Inclusion criteria were being a parent of a child ages 3- to 12-year old, diagnosed with CF for a minimum of 1 year; the exclusion criterion was the inability to read English sufficiently to understand the questionnaires. The lower age limit of this convenience sample was chosen to ensure variation in responses concerning adherence; it was felt that parents of children under age 3 years were likely to be sufficiently new to the disease that they would be highly adherent. The upper age limit was selected because parents generally bear approximately 80% of the responsibility for treatment in children under 12 years.53 Eligible parents were mailed a letter introducing the study which contained a postcard for them to return to “opt out” of receiving a follow-up phone call from project staff. Parents who were interested in participating were seen by study staff at their regularly scheduled clinic appointment to obtain informed consent and complete study measures. Questionnaires were completed immediately following their clinic visit as part of a larger study on provider–parent interactions and adherence. Participants received $20 following completion of the study measures.
Measures: Determinants of Adherence
Self-Efficacy to Adhere to the Prescribed Treatment Plan
Perceived self-efficacy is what a person feels capable of accomplishing. Self-efficacy was measured using Bandura’s Social Cognitive Theory and model for constructing a domain-specific efficacy measure that is responsive to situational demands and characteristics.54 This measure assesses efficacy to adhere to two domains of the CF regimen—airway clearance and aerosolized medications—across varying levels of task demands that represent various challenges to successful performance. The measure asks respondents to “Please rate how certain you are that you can make sure that your child does his or her specified treatment (e.g., airway clearance) the number of times recommended by your doctor each day.” Participants rate their confidence on a 100-point scale ranging in 10-U intervals from 0 (cannot do), through intermediate degrees of confidence, 50 (moderately can do), to complete confidence, 100 (highly certain can do). Each scale consists of 10 conditions, such as “on a normal weekday,” “when my child is sick,” and “when our family is stressed.” Mean efficacy scores were calculated for each airway clearance and aerosolized medication treatment. These and all scales used may be found in Additional Supporting Information.
Attitude Towards Treatment (Perceived Utility)
The perceived utility of the treatment plan was measured with the Perceived Utility Subscale from the Adherence Determination Questionnaire. An example of the items includes, “The benefits of my child’s treatment plan outweigh any difficulty I might have following it.” This 8-item parent survey has demonstrated good internal consistency and concurrent validity.55 It uses a 5-point Likert-style scale (1 = strongly disagree, 5 = strongly agree) to assess attitudes about the usefulness of current treatment plans.
Measures: Background Factors
Religious Coping Styles
Religious coping styles for control/problem-solving were measured using five items from the Brief R-COPE scale.29 This 5-item subscale has been used in numerous studies and has good psychometric properties. Respondents answer how often they use each of the religious coping styles (not whether the coping style “worked”) using a 4-point Likert style scale ranging from 0 (did not use) to 3 (used a great deal).
Sanctification of the Body
Sanctification of the body was measured using a shortened version of the Sanctification of the Body scale.43,48 This shortened, 7-item questionnaire has previously been used in parents of children with CF and demonstrated good reliability and validity. Inter-item reliability was high with alphas of 0.95 for the manifestation of God in the body subscale and 0.85 for the Sacred Qualities of the body subscale. Principal components analysis showed the presence of the same two subscales as the complete measure.48 The manifestation of God in the body subscale taps religious perspectives with items like, “My child’s body is created in God’s image.” Agreement with items is rated on a 7-item Likert-style response scale (7 = strongly agree). The Sacred Qualities of the body subscale taps spiritual perspectives with items like, “My child’s body is miraculous.” Agreement with items was rated on a 7-item Likert-style response scale (1 = doesn’t apply to 7 = applies strongly).
Analysis
The data were analyzed using PASW Statistics 18.0 and SAS 9.2. Likert-style responses from the R-COPE scale were dichotomized, assigning responses of 0 and 1 (used “not at all” or “somewhat”) to 0 and assigning responses of 2 and 3 (used “quite a bit” and “a great deal”) to 3. Individuals who did not use religious coping were excluded from further analysis, resulting in N = 24 individuals. To examine relationships among religious coping styles, and to determine if certain religious coping styles were used in combination with others, principal components were determined for participant responses to the five religious coping items using the polychoric correlation matrix, which is adjusted for ordinal data.56 Loadings were interpreted after VARIMAX rotation. Importance of each component was based on the magnitude of the corresponding eigenvalue. Participants were also dichotomized based on being above or below the median score for each of the two sanctification of the body subscales (sacred qualities of the body and for manifestation of God in the body). Group comparisons were made using unpaired t-tests assuming unequal variances for the mean scores of the response variables (self-efficacy and treatment attitude).
RESULTS
Demographic and Clinical Data
The median age of the parents (n = 28) was 39 years (range: 23–56 years), and the median age of the children (n = 28) was 7.7 years (range: 3.5–12.7 years). The median parental income level of the sample was $50,000–$74,999 per year (range: $5000–$100,000 or higher). Fifty-five percent of parents had education less than a Bachelor’s degree; 36% had a Bachelor’s or graduate degree. Mean length of time since diagnosis for the sample was 6.5 years (SD = 3.01 years). The median FEV1% predicted was 103% (range: 58–123% predicted; n = 14). Using this measure of lung function, the children represented a moderately broad distribution of lung disease. The median number of CF exacerbations in the previous 12 months was 1 (range: 0–4). The median child BMI percentile was 70 (range: 21–98%ile).
Sanctification of the Body
The high mean sanctification of the body subscale scores (response range: 1–7) indicate that parents in this sample do indeed sanctify their child’s body (sacred qualities of the body: M = 6.1, SD = 1.2; manifestation of God in the body: M = 5.9, SD = 1.4). These means are similar to those presented by Grossoehme et al.48 from parents of children with CF (sacred qualities: M = 5.97, SD = 1.37; manifestation of God: M = 5.47, SD = 1.45). Mean sanctification scores from Mahoney et al., 43 although lower, fall within the SD range of our results (sacred qualities: M = 4.0, SD = 1.43; manifestation of God: M = 4.64, SD = 1.68).
Religious Coping
Styles of religious coping for control had moderate mean scores (corresponding to using such styles “somewhat” and “quite a bit” of the time). Mean scores (SD) for the whole sample (N = 28) were: Collaborative (M = 1.6; SD = 1.1); Pleading (M = 1.7; SD = 1.3); Self-directed (M = 0.96; SD = 1.1); Active Surrender (M = 2.0; SD = 1.0); and Deferring (M = 0.46; SD = 0.92). Dichotomization of the scores (as previously described) allowed calculation of the means (and SD) only for those persons who used religious coping (N = 24). The mean scores (SD) for this subsample were: Collaborative (M = 1.8; SD = 1.1); Pleading (M = 1.8; SD = 1.3); Self-directed (M = 1.0; SD = 1.2); Active Surrender (M = 2.2; SD = 0.96); and Deferring (M = 0.54; SD = 0.98). However, descriptive frequencies showed that most participants endorsed more than one style of religious coping. Principal components were then calculated; two principal components emerged from the data with eigenvalues larger than one. Collaborative and Active Surrender loaded heavily on the first component (correlations 0.92 and 0.91, respectively), while the second component was consists of Deferring, Self-Directed, and Pleading styles. The resulting principal components scores were used (excluding data which showed no religious coping) to form two religious coping groups. These two components were treated as groups in the unpaired t-tests described below.
Determinants of Adherence
Attitudes Towards Treatment Utility
The mean attitude towards treatment utility value was near the upper end of the scale (M = 36.8; SD = 4.6), indicating that parents in this sample perceived their child’s treatment as useful. Parents who used Collaborative or Active Surrender religious coping (only) or the combination of these two styles had mean scores on attitude towards treatment utility scale that were significantly higher from parents who used any other type of religious coping style or combination of styles (Table 1). Parents who saw a manifestation of God in their child’s body had significantly higher mean scores on the treatment utility scale (Table 1) based on unpaired t-tests assuming unequal variances. There was a trend towards significance in the difference of mean scores on the treatment utility scale for parents who saw sacred qualities in their child’s body based on the same type of t-test.
TABLE 1.
Mean Scores of Adherence Determinants by Parental Religious and Spiritual Constructs
| Religious construct | Population subset | Treatment attitude | Self-efficacy (airway clearance) | Self-efficacy (aerosolized medications) |
|---|---|---|---|---|
|
| ||||
| M ± SD (n) | M ± SD (n) | M ± SD (n) | ||
| Sanctification of the body | ||||
| Sacred qualities of the body | High-sanctifiers | 38.8 ± 2.3 (12) P = 0.038* | 1058.6 ± 54.9 (15) P = 0.023* | 1073.0 ± 39.4 (15) P = 0.020* |
| Low-sanctifiers | 34.2 ± 6.6 (9) | 858.9 ± 213.6 (9) | 922.2 ± 153.0 (9) | |
| Manifestation of God in the body | High-sanctifiers | 38.7 ± 2.6 (12) P = 0.047* | 1057.4 ± 60.4 (12) P = 0.033* | 1068.8 ± 42.6 (12) P = 0.043* |
| Low-sanctifiers | 34.7 ± 5.5 (12) | 910.0 ± 204.7 (12) | 965.0 ± 154.3 (12) | |
| Religious coping | Collaborative | 38.8 ± 2.3 (12) P = 0.038* | 1070.89 ± 35.8 (12) P = 0.012* | 1077.1 ± 37.4 (12) P = 0.018* |
| Other | 34.6 ± 5.9 (12) | 896.7 ± 199.0 (12) | 956.7 ± 148.9 (12) | |
P-values are based on unpaired t-tests.
Self-Efficacy
The mean self-efficacy scores for airway clearance and aerosolized medication administration were relatively high (airway clearance: M = 994.4, SD = 156.1; aerosolized medications: M = 1023.2, SD = 115.5). Parents who used Collaborative or Active Surrender religious coping (only) or the combination of these two styles had mean scores for self-efficacy in completing their child’s airway clearance and for completing administration of their child’s aerosolized medications that were significantly higher than did parents who used any other religious coping style or combination of styles (Table 1). Mean scores for self-efficacy for airway clearance, for aerosolized medication administration, and for attitude towards treatment utility were significantly higher for parents who imbued their child’s body with either or both of the sanctification of the body subscales: sacred qualities of the body or manifestation of God in the body (Table 1).
DISCUSSION
The TRA provides a useful model for understanding the many factors that contribute to adherence. This study is the first to link determinants of parental adherence (self-efficacy and attitude towards treatment utility) to their child’s daily recommended CF home treatments and the “background factor,” spirituality. This expands the potential importance of Fishbein and Ajzen’s “background factors,” which ultimately affect adherence behaviors. Although usually held tacitly, it is important to understand the pro-healthy aspects of background factors, including spiritual background factors. As we have shown, spiritual background factors directly related to adherence determinants.
The data show that parents who imbue their child’s body with sacred significance have significantly higher mean scores on their self-efficacy to accomplish their child’s airway clearance and administration of aerosolized medications. Studies of the relationship between health and religion and spirituality have unfortunately relied on single-item measures of religiosity.57–59 Religion and spirituality are both multi-dimensional constructs. Further, single-item measures cannot explain how religion or spirituality exert any influence on health or health-related behaviors and thus have limited value. Mahoney et al.60 has argued that “distal” measures of religiosity (affiliation, frequency of worship) are less important than “proximal” measures, such as beliefs like sanctification of the body (or religious coping styles). Early studies of the proximal construct “sanctification of the body” indicated that persons were most likely to act in ways that conserved aspects of their lives which they considered to be sacred. The present study is the first presentation that this parental belief is related to pro-healthy actions undertaken on their child’s behalf. Since the daily recommended CF treatments in this study (airway clearance and aerosolized medications) are aimed at slowing disease progression, factors which support adherence to those treatments and conserve health are vital and should be well-understood.
These data also show that parents who use Collaborative and or Active Surrender styles of religious coping have significantly higher mean scores on their self-efficacy to accomplish two types of recommended daily treatments of children with CF. In addition, parents who use Collaborative and or Active Surrender styles of religious coping, and those who imbue their child’s body with sacred significance, have higher mean scores on a measure of attitudes towards treatment utility than do parents who cope by other styles of religious coping or those who do not sanctify their child’s body. Our data on these coping styles suggest that parents who view their completion of their child’s recommended home medical care in collaboration with an Ultimate Other (and who sanctify their child’s body) feel greater confidence in their ability to perform these tasks. The impact of religion may be expressed through styles of religious coping in which parents view themselves in partnership with the Divine and so feel empowered with respect to caring for their child’s health. Religious attributions for a child’s health needs (e.g., a form of religious coping) have been associated with mental health outcomes in a study of parents of children with Down’s syndrome.61 Similar findings associating Collaborative and Active Surrender religious coping with positive health outcomes have been previously described.62
This study has limitations. First, it is cross-sectional in design. The sample is small and is drawn from a single CF Center. In order to reduce participant burden, only two determinants of adherence were included in this study. Other aspects of adherence (namely, subjective/injunctive norms) remain to be studied. Second, parental self-efficacy is one determinant of adherence, and does not a substitute for adherence.
Nonetheless, important conclusions can still be drawn. This is the first report of relationships between the determinants of adherence to a child’s recommended treatment regimen and parental spiritual constructs. Previous adherence studies have only examined spiritual and or religious variables with adult patients. Despite the sample size, it was possible to demonstrate that spiritual variables are associated with two of the determinants of adherence following the TRA model. Given the published levels of adherence to airway clearance and aerosolized therapies, it is important to identify and understand those factors which lead to the determinants of adherence, including spiritual factors. Understanding the relationship between parental religious coping styles and parental sanctification of the child’s body opens up a new and potentially important avenue by which to address adherence for the many parents for whom religious or spiritual beliefs are important. It also suggests a broader role for an existing member of many healthcare delivery teams—board certified clinical chaplains—who may be important adjuncts to help address adherence issues with parents. Future research should include regression analyses to examine the contribution of religious variables to self-efficacy and other factors affecting it, as well as the effect of spiritual variables on the other determinants of adherence. This would also permit study of whether those effects are direct, mediated, or moderated by adherence determinants.
Supplementary Material
Acknowledgments
Funding source: Division of Pulmonary Medicine at Cincinnati Children’s Hospital Medical Center.
No author has a conflict of interest; the first draft was prepared by Dr. Grossoehme and no author received any honorarium, grant or other form of payment for the preparation of this manuscript.
Footnotes
Conflict of interest: None.
The information contained in this paper was presented at the North American Cystic Fibrosis Conference, Baltimore, Maryland, on October 21, 2010.
Additional Supporting Information may be found in the online version of this article.
References
- 1.Modi AC, Quittner AL. Utilizing computerized phone diary procedures to assess health behaviors in family and social contexts. Child Health Care. 2006;35:29–45. [Google Scholar]
- 2.Zivin K, Kales HC. Adherence to depression treatment in older adults: a narrative review. Drugs Aging. 2008;25:559–571. doi: 10.2165/00002512-200825070-00003. [DOI] [PubMed] [Google Scholar]
- 3.Scoular D. An evaluation of medication adherence in children with attention-deficit/hyperactivity disorder using the Theory of Reasoned Action and planned behavior. Vancouver, BC, Canada: University of British Columbia; 2006. [Google Scholar]
- 4.Modi AC, Quittner AL. Barriers to treatment adherence for children with cystic fibrosis and asthma: what gets in the way? J Pediatr Psychol. 2006;31:846–858. doi: 10.1093/jpepsy/jsj096. [DOI] [PubMed] [Google Scholar]
- 5.Modi AC, Lim CS, Yu N, Geller D, Wagner MH, Quittner AL. A multi-method assessment of treatment adherence for children with cystic fibrosis. J Cyst Fibros. 2006;5:177–185. doi: 10.1016/j.jcf.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Daniels T, Goodacre L, Sutton C, Pollard K, Conway S, Peckham D. Accurate assessment of adherence: self and clinician report versus electronic monitoring of nebulizers. Chest. 2011;140:425–435. doi: 10.1378/chest.09-3074. [DOI] [PubMed] [Google Scholar]
- 7.Kerem E, Reisman J, Corey M, Canny G, Levison H. Prediction of mortality in patients with cystic fibrosis. NEJM. 1992;326:1187–1191. doi: 10.1056/NEJM199204303261804. [DOI] [PubMed] [Google Scholar]
- 8.Flume PA, O’Sullivan BP, Robinson KA, Goss CH, Mogayzel PJ, Jr, Willey-Courand DB, Bujan J, Finder J, Lester M, Quittell L, Rosenblatt R, Vender RL, Hazle L, Sabadosa K, Marshall B Cystic Fibrosis Foundation PTC. Cystic fibrosis pulmonary guidelines: chronic medications for maintenance of lung health. Am J Respir Crit Care Med. 2007;176:957–969. doi: 10.1164/rccm.200705-664OC. [DOI] [PubMed] [Google Scholar]
- 9.Flume PA, Robinson KA, O’Sullivan BP, Finder JD, Vender RL, Willey-Courand DB, White TB, Marshall BC Committee CPGfPT. Cystic fibrosis pulmonary guidelines: airway clearance therapies. Respir Care. 2009;54:522–537. [PubMed] [Google Scholar]
- 10.Liou TG, Adler FR, FitzSimmons SC, Cahill B, Hibbs J, Marshall B. Predictive 5-year survivorship model of cystic fibrosis. Am J Epidemiol. 2001;153:345–352. doi: 10.1093/aje/153.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Syrjala AM, Niskanen MC, Knuuttila ML. The Theory of Reasoned Action in describing tooth brushing, dental caries and diabetes adherence among diabetic patients. J Clin Periodontol. 2002;29:427–432. doi: 10.1034/j.1600-051x.2002.290507.x. [DOI] [PubMed] [Google Scholar]
- 12.Bartholomew LK, Parcel GS, Swank PR, Czyzewski DI. Measuring self-efficacy expecatations for the self-managment of cystic fibrosis. Chest. 1993;103:1524–1530. doi: 10.1378/chest.103.5.1524. [DOI] [PubMed] [Google Scholar]
- 13.Parcel GS, Swank PR, Mariotto MJ, Bartholomew LK, Czyewski DI, Sockrider MM, Seilheimer DK. Self-managment of cystic fibrosis: a structural model for educational and behavioural variables. Soc Sci Med. 1994;38:1307–1315. doi: 10.1016/0277-9536(94)90194-5. [DOI] [PubMed] [Google Scholar]
- 14.Bartlett SJ, Krishnan JA, Riekert KA, Butz AM, Malveaux FJ, Rand CS. Maternal depressive symptoms and adherence to therapy in inner-city children with asthma. Pediatrics. 2004;113:229–237. doi: 10.1542/peds.113.2.229. [DOI] [PubMed] [Google Scholar]
- 15.Rapoff MA. Adherence to pediatric medical regimens. New York, NY: Kluwer Academic/Plenum Publishers; 1999. [Google Scholar]
- 16.Hill PC, Pargament KI, Hood RW, McCullough ME, Swyers JP, Larson DB, Zinnbauer BJ. Conceptualizing religion and spirituality: points of comonality, points of departure. J Theory Soc Behav. 2000;30:51–77. [Google Scholar]
- 17.Hill PC, Pargament KI, Hood RW, McCullough ME, Swyers JP, Larson DB, Zinnbauer BJ. Conceptualizing religion and spirituality: points of commonality, points of departure. J Theory Soc Behav. 2000;30:51–77. [Google Scholar]
- 18.Gallup I. [Access date June 23, 2008];Religion. 2008 http://wwwgallupcom/poll/1690/Religionaspx.
- 19.Newlin K, Knafl K, Melkus GD. African-American spirituality: a conceptual analysis. ANS Adv Nurs Sci. 2002;25:57–70. doi: 10.1097/00012272-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Newport F. Religion most important to blacks, women, and older Americans. Vol. 2011. Gallup, Inc; 2006. [Access date 27 July 2011]. http://www.gallup.com/poll/25585/Religion-Most-Important-Blacks-Women-Older-Americans.aspx. [Google Scholar]
- 21.Stern RC, Canda ER, Doershuk CF. Use of non-medical treatments by cystic fibrosis patients. J Adolesc Health. 1992;13:612–615. doi: 10.1016/1054-139x(92)90376-m. [DOI] [PubMed] [Google Scholar]
- 22.Konkle-Parker DJ, Erlen JA, Dubbert PM. Barriers and facilitators to medication adherence in a southern minority population with HIV disease. J Assoc Nurses AIDS Care. 2008;19:98–104. doi: 10.1016/j.jana.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parsons SK, Cruise PL, Davenport WM, Jones V. Religious beliefs, practices and treatment adherence among individuals with HIV in the southern United States. AIDS Patient Care STDS. 2006;20:97–111. doi: 10.1089/apc.2006.20.97. [DOI] [PubMed] [Google Scholar]
- 24.Thomas CM. The influence of self-concept on adherence to recommended health regimens in adults with heart failure. J Cardiovasc Nurs. 2007;22:405–416. doi: 10.1097/01.JCN.0000287037.85067.3d. [DOI] [PubMed] [Google Scholar]
- 25.Benjamins MR. Religious influences on trust in physicians and the health care system. Int J Psychiatry Med. 2006;36:69–83. doi: 10.2190/EKJ2-BCCT-8LT4-K01W. [DOI] [PubMed] [Google Scholar]
- 26.Kemppainen J, Kim-Godwin YS, Reynolds NR, Spencer VS. Beliefs about HIV disease and medication adherence in persons living with HIV/AIDS in rural southeastern North Carolina. J Assoc Nurses AIDS Care. 2008;19:127–136. doi: 10.1016/j.jana.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Goldbeck L. Parental coping with the diagnosis of childhood cancer: gender effects, dissimilarity within couples and quality of life. Psychooncology. 2001;10:325–335. doi: 10.1002/pon.530. [DOI] [PubMed] [Google Scholar]
- 28.Finocchario-Kessler S, Catley D, Berkley-Patton J, Gerkovich M, Williams K, Banderas J, Goggin K. Baseline predictors of ninety percent or higher antiretroviral therapy adherence in a diverse urban sample: the role of patient autonomy and fatalistic religious beliefs. AIDS Patient Care STDS. 2011;25:103–111. doi: 10.1089/apc.2010.0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: development and initial validation of the RCOPE. J Clin Psychol. 2000;56:519–543. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 30.Benjamins MR. Religious influences on trust in physicians in the health care system. Int J Psychiatry Med. 2006;36:69–83. doi: 10.2190/EKJ2-BCCT-8LT4-K01W. [DOI] [PubMed] [Google Scholar]
- 31.Margolin A, Schuman-Olivier Z, Beitel M, Arnold RM, Fulwiler CE, Avants SK. A preliminary study of spiritual self-schema (3-S(+)) therapy for reducing impulsivity in HIV-positive drug users. J Clin Psychol. 2007;63:979–999. doi: 10.1002/jclp.20407. [DOI] [PubMed] [Google Scholar]
- 32.Targ EF, Levine EG. The efficacy of a mind-body-spirit group for women with breast cancer: a randomized controlled trial. Gen Hosp Psychiatry. 2002;24:238–248. doi: 10.1016/s0163-8343(02)00191-3. [DOI] [PubMed] [Google Scholar]
- 33.Shaw B, Han JY, Kim E, Gustafson D, Hawkins R, Cleary J, McTavish F, Pingree S, Eliason P, Lumpkins C. Effects of prayer and religious expression within computer support groups on women with breast cancer. Psychooncology. 2007;16:676–687. doi: 10.1002/pon.1129. [DOI] [PubMed] [Google Scholar]
- 34.Murray-Swank NA, Pargament KI. God, where are you? Evaluating a spiritually-integrated intervention for sexual abuse. Mental Health Relig Cult. 2005;8:191–203. [Google Scholar]
- 35.Mahoney A, Tarakeshwar N. Religion’s role in marriage and parenting in daily life and during family crises. In: Paloutzian RF, Park CL, editors. Handbook of the psychology of religion and spirituality. New York, NY: Guilford Press; 2005. pp. 177–195. [Google Scholar]
- 36.Hexem KR, Mollen CJ, Carroll K, Lanctot DA, Feudtner C. How parents of children receiving pediatric palliative care use religion, spirituality, or life philosophy in tough times. J Palliat Med. 2011;14:39–44. doi: 10.1089/jpm.2010.0256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tarakeshwar N, Pargament KI. Religious coping in families with autism. Focus Autism Other Dev Delays. 2001;16:247–260. [Google Scholar]
- 38.Grossoehme DH, Cotton S, Pallerla H, Tsevat J. Religious/spiritual coping by parents of adolescents with sickle cell disease: a pilot study. Paper presented at the meeting, Spirituality, Health and Human Flourishing: Meaning? Measurement? Implications?; Durham, NC. 2008. [Google Scholar]
- 39.Grossoehme DH, Ragsdale JR, Wooldridge JL, Cotton S, Seid M. Parents’ use of religion in the first year following their child’s diagnosis with cystic fibrosis. Pediatr Pulmonol. 2009;44(S32):427. doi: 10.1080/08854726.2010.480833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grossoehme DH, Jacobson CJ, Cotton S, Ragsdale JR, VanDyke R, Seid M. Written prayers and religious coping in a paediatric hospital setting. Mental Health Relig Cult. 2011;14:423–432. [Google Scholar]
- 41.Marshall ES, Olsen SF, Mandleco BL, Dyches TT, Allred KW, Sansom N. “This is a spiritual experience”: perspectives of Latter-Day Saint famlies living with a child with disabilities. Qual Health Res. 2003;13:57–76. doi: 10.1177/1049732302239411. [DOI] [PubMed] [Google Scholar]
- 42.Grossoehme DH, Ragsdale JR, Wooldridge JL, Cotton S, Seid M. ‘We can handle this’: parents’ use of religion in the first year following their child’s diagnosis with cystic fibrosis. J Health Care Chaplain. 2010;16:95–108. doi: 10.1080/08854726.2010.480833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mahoney A, Carels RA, Pargament KI, Wachholtz A, Leeper LE, Kaplar M, Frutchey R. The sanctification of the body and behavioral health patterns of college students. Int J Psychol Relig. 2005;15:221–238. [Google Scholar]
- 44.Pargament KI. Psychology of religious coping. New York: Guildford Press; 1997. [Google Scholar]
- 45.Park CL. Religiousness/spirituality and health: a meaning systems perspective. J Behav Med. 2007;30:319–328. doi: 10.1007/s10865-007-9111-x. [DOI] [PubMed] [Google Scholar]
- 46.Mahoney A, Pargament KI, Murray-Swank A, Murray-Swank NA. Religion and the sanctifiction of family relationships. Rev Relig Res. 2003;40:220–236. [Google Scholar]
- 47.Murray-Swank NA, Pargament KI, Mahoney A. At the crossroads of sexuality and spirituality: the sanctification of sex by college students. Int J Psychol Relig. 2005;15:199–219. [Google Scholar]
- 48.Grossoehme DH, VanDyke R, Seid M. Spirituality’s role in chronic disease self-management: sanctifiction of the body in families dealing with cystic fibrosis. J Health Care Chaplain. 2009;15:1–10. doi: 10.1080/08854720903163312. [DOI] [PubMed] [Google Scholar]
- 49.Hernandez G, Salerno JM, Bottoms BL. Attachment to God, spiritual coping and alcohol use. Int J Psychol Relig. 2010;20:97–108. [Google Scholar]
- 50.Abernethy AD, Houston TR, Bjorck JP, Gorsuch RL, Arnold HL. Religiousness and prostate cancer screening in African American men. J Psychosoc Oncol. 2009;27:316–331. doi: 10.1080/07347330902979036. [DOI] [PubMed] [Google Scholar]
- 51.Yangarber-Hicks N. Religious coping styles and recovery from serious mental illness. J Psychol Theol. 2004;32:305–317. [Google Scholar]
- 52.Belavich T, Pargament KI. The role of attachment in predicting religious coping with a loved one in surgery. J Adult Dev. 2002;9:13–29. [Google Scholar]
- 53.Drotar D, Ievers C. Age differences in parent and child responsibilities for management of cystic fibrosis and insulin-dependent diabetes mellitus. J Dev Behav Pediatr. 1994;15:265–272. [PubMed] [Google Scholar]
- 54.Bandura A. Guide for creating self-efficacy scales. In: Pajares F, Urdan T, editors. Self-efficacy beliefs of adolescents. Greenwich, CT: Information Age Publishing, Inc; 2006. p. 367. [Google Scholar]
- 55.DiMatteo MR, Hays RD, Gritz ER, Bastani R, Crane L, Elashoff R, Ganz P, Heber D, McCarthy W, Marcus A. Patient adherence to cancer control regimens: scale development and initial validation. Psychol Assess. 1993;5:102–112. [Google Scholar]
- 56.Olsson U. Maximum likelihood estimation of the polychoric correlation coefficient. Psychometrika. 1979;44:443–460. [Google Scholar]
- 57.Fetzer/National Institute on Aging WG. Mulitdimensional measurement of religiousness/spirituality for use in health research: a report of the Fetzer/National Insitute on Aging Working Group. Kalamazoo, MI: Fetzer Institute; 1999. [Google Scholar]
- 58.Idler EL, Idler EL, Musick MA, Ellison CG, George LK, Krause N, Ory MG, Pargament KI, Powell LH, Underwood LG, Williams DR. Measuring multiple dimensions of religion and spirituality for health research: conceptual background and findings from the 1998 General Social Survey. Res Aging. 2003;25:327–365. [Google Scholar]
- 59.Idler EL, Idler EL, Musick MA, Ellison CG, George LK, Krause N, Ory MG, Pargament KI, Powell LH, Underwood LG, Williams DR. Erratum. Res Aging. 2004;26:284. [Google Scholar]
- 60.Mahoney A, Pargament KI, Jewell T, Swank AB, Scott E, Emery E, Rye M. Marriage and the spiritual realm: the role of proximal and distal religious constructs in marital functioning. J Fam Psychol. 1999;13:321–338. [Google Scholar]
- 61.Mickelson KD, Wrobe M, Helgeson VS. “Why my child?”: parental attributions for children’s special needs. J Appl Soc Psychol. 1999;29:1263–1292. [Google Scholar]
- 62.Pargament KI. The psychology of religious coping. New York: Guilford Press; 1997. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.