Abstract
International experts met to discuss recent advances and to revise the 2004 recommendations for assessing and reporting precursor lesions to invasive carcinomas of the pancreas, including pancreatic intraepithelial neoplasia (PanIN), intraductal papillary mucinous neoplasm (IPMN), mucinous cystic neoplasm, and other lesions. Consensus recommendations include the following: 1) To improve concordance and to align with practical consequences, a two-tiered system (low vs. high-grade) is proposed for all precursor lesions, with the provision that the current PanIN-2 and neoplasms with intermediate-grade dysplasia now be categorized as low-grade. Thus, “high-grade dysplasia” is to be reserved for only the uppermost end of the spectrum (“carcinoma in situ” type lesions). 2) Current data indicate that PanIN of any grade at a margin of a resected pancreas with invasive carcinoma does not have prognostic implications; the clinical significance of dysplasia at a margin in a resected pancreas with IPMN lacking invasive carcinoma remains to be determined. 3) Intraductal lesions 0.5–1 cm can be either large PanINs or small IPMNs. The term “incipient IPMN” should be reserved for lesions in this size with intestinal- or oncocytic-papillae or GNAS mutations. 4) Measurement of the distance between an IPMN and invasive carcinoma and sampling of intervening tissue are recommended to assess concomitant versus associated status. Conceptually, concomitant invasive carcinoma (in contrast with the “associated” group) ought to be genetically distinct from an IPMN elsewhere in the gland. 5) “Intraductal spread of invasive carcinoma” (aka, “colonization”) is recommended to describe lesions of invasive carcinoma invading back into and extending along the duct system, which may morphologically mimic high-grade PanIN or even IPMN. 6) “Simple mucinous cyst” is recommended to describe cysts > 1 cm having gastric-type flat mucinous lining at most minimal atypia without ovarian-type stroma to distinguish them from IPMN. 7) Human lesions resembling the acinar-to-ductal metaplasia and atypical flat lesions of genetically engineered mouse models exist and may reflect an alternate pathway of carcinogenesis; however, their biological significance requires further study. These revised recommendations are expected to improve our management and understanding of precursor lesions in the pancreas.
Keywords: Pancreatic intraepithelial neoplasia (PanIN), intraductal papillary mucinous neoplasm (IPMN), mucinous cystic neoplasm (MCN), precursor, adenocarcinoma, atypical flat lesions (AFL)
INTRODUCTION
International consensus meetings held in 1999, 2000, and 2003 formed the basis for the current definition and classification of the two major precursor lesions to invasive pancreatic carcinoma; pancreatic intraepithelial neoplasia (PanIN) and intraductal papillary mucinous neoplasm (IPMN) 1, 2. PanIN is defined as a microscopic, flat or papillary, noninvasive epithelial neoplasm characterized by varying amounts of mucin and degrees of cytologic and architectural atypia. IPMN is defined as a grossly visible, predominantly papillary or rarely flat, noninvasive mucin-producing epithelial neoplasm arising in the main pancreatic duct or branch ducts 1, 2. All grades of PanINs and IPMNs are regarded to be neoplastic, and these lesions are divided into three tiers based on the degree of dysplasia1, 2. The classification and grading system developed for PanIN, IPMN, and mucinous cystic neoplasm (MCN) has tremendously helped our understanding of these lesions and was subsequently incorporated in the classifications of the Armed Forces Institutes of Pathology/American Registry of Pathology (AFIP/ARP) 3 and of the World Health Organization (WHO) 4. The classification system has also helped researchers interpret genetically engineered mouse models (GEMM) that recapitulate human disease and formed the basis for studies of the genetics and gene expression patterns of these precursor lesions in the human pancreas 5–10.
However, when the original classification was introduced, pancreas surgery was mainly performed at a few large tertiary referral centers, mostly on patients with invasive pancreatic carcinoma. In spite of a rising academic awareness of pancreatic cancer precursor lesions at that time, meticulous pathologic studies in conjunction with molecular analyses were just in their infancy. The classification was therefore based on limited data on the natural history and clinical significance of the lesions, which were almost all studied in the setting of invasive carcinoma, and genetic analyses, while they supported the classification, were incomplete. With improvements in imaging to detect minute pancreatic lesions and increases in the number of centers now performing pancreatic surgery, although the situation that surgeries are performed mainly for PDA at a few large tertiary referral centers is still the case, more surgeries have been performed for indications other than invasive carcinoma. This has enormously added to our knowledge of the whole spectrum of pancreatic neoplasms including PanIN and IPMN 11–19. In addition, our understanding of the genetics of precursors has greatly expanded with the introduction of routine molecular genetic analyses, including next generation sequencing 20–28.
Clinical advances have produced a management dichotomy, especially for IPMNs, such that lesions with low-grade or intermediate-grade dysplasia are mostly regarded as low-risk for progression and therefore amenable to clinical observation, whereas the precursor lesions with high-grade dysplasia (also called “carcinoma in situ” based on geographic practice preferences) are considered to have a significant potential for progression to invasive carcinoma and thus usually are surgically resected 29. Similarly, we also recognize that while PanINs are biologically important for understanding the origins of invasive carcinoma, PanIN-1s and PanIN-2s are common incidental findings and probably not clinically relevant at this time 30.
To assess the impact of these advances and to discuss the possibility of devising a pathologic definition and classification system that more accurately reflects our new knowledge and new clinical needs, an international consensus meeting was organized by Drs. Ralph H. Hruban and David S. Klimstra. The group convened at The Johns Hopkins University School of Medicine from June 17 to 18, 2014, under the auspices of The Sol Goldman Pancreatic Cancer Research Center, and included an international group of experts from various disciplines.
DESIGN
An international consensus meeting as well as pre- and post-meeting analyses were organized and co-chaired by R.H.H. and D.S.K. Participants including pathologists, surgeons, and gastroenterologists from North America (Mexico, USA), Europe (France, Germany, Netherlands, United Kingdom), and Asia (Japan, Korea) were selected based on participation in the 2003 consensus meeting or significant contributions to the field after the 2003 meeting. Before the meeting, an elaborate list of discussion topics was created based on input from all meeting participants. These discussion topics were collated and recirculated for further input from all of the participants in the meeting, and selected meeting participants were tasked to give presentations at the meeting summarizing the current published data and highlighting issues of controversy related to these topics during the meeting.
The discussion was focused on classification, reporting and histologic grading of PanINs, IPMNs, and MCNs, as well as on additional lesions with possible relevance to pancreatic carcinogenesis, such as acinar-ductal metaplasia and atypical flat lesion. After discussion, specific questions and action items were proposed and subjected to voting by the participants. Agreement among >80% of participants was regarded as consensus.
RESULTS
TWO-TIERED VS THREE-TIERED CLASSIFICATION SYSTEM FOR PanINs, IPMNs AND MCNs
Problematic Issues
The three-tiered grading systems for PanINs, IPMNs, and MCNs were originally created to encompass the full spectrum of lesions, and because it was felt that they would allow for detailed clinical and genetic studies of the entire range of lesions observed, which they did. However, the clinical significance of PanIN 1 and 2 lesions has been questioned 13, 31. Moreover, with the growing use of abdominal imaging, more IPMNs are being diagnosed incidentally, and many of these are low- or intermediate-grade and of uncertain clinical significance 31–35. Non-operative follow-up of these cysts has revealed a very low risk of progression to invasive cancer 36. In the meantime, the distinction of these innocuous processes from more clinically-relevant advanced forms of intraepithelial neoplasia has become more than an academic exercise, with major clinical implications in daily clinical management of these patients. Therefore, it is not surprising that the current three-tiered classification scheme is not in line with the 2012 consensus guidelines of the International Association of Pancreatology for the management of IPMNs and MCNs. According to these guidelines, precursor lesions with either low-grade or intermediate-grade dysplasia are mostly regarded as amenable to clinical observation, whereas surgery is recommended for precursor lesions with high-grade dysplasia 29.
As the goal of clinical management is to observe low- and intermediate-grade precursor lesions and to resect high-grade precursor lesions in order to decrease the risk of invasive cancer, a two-tiered classification scheme was felt to be more in line with practical consequences: low-grade and intermediate-grade dysplasia likely has no immediate clinical consequences, whereas high-grade dysplasia usually requires clinical attention.
Revised Classification
A two-tiered classification, low-grade versus high-grade, was recommended to replace the former three-tiered classification for PanIN, IPMN and MCN (Table 1).
Table 1.
Proposed Revised Terminology of PanIN, IPMN and MCN
| Former terminology (based on 2004 Classification2 and 2010 WHO) | Revised terminology (2015) |
|---|---|
| PanIN-1a | Low-grade PanIN |
| PanIN-1b | Low-grade PanIN |
| PanIN-2 | Low-grade PanIN |
| PanIN-3 (carcinoma in-situ) | High-grade PanIN |
| IPMN with low-grade dysplasia | IPMN, low-grade |
| IPMN with intermediate-grade dysplasia | IPMN, low-grade |
| IPMN with high-grade dysplasia (carcinoma in-situ) | IPMN, high-grade |
| IPMN with an associated invasive carcinoma | IPMN with an associated invasive carcinoma/invasive carcinoma with an associated IPMN (the latter may be used if the invasive component is substantial) |
| MCN with low-grade dysplasia | MCN, low-grade |
| MCN with intermediate-grade dysplasia | MCN, low-grade |
| MCN with high-grade dysplasia (carcinoma in-situ) | MCN, high-grade |
| MCN with an associated invasive carcinoma | MCN with an associated invasive carcinoma/invasive carcinoma with an associated MCN (the latter may be used if the invasive component is substantial) |
The former PanIN-2 and intermediate-grade dysplasia IPMN/MCN categories are now to be categorized as low-grade. Accordingly, the term high-grade is to be reserved ONLY for the uppermost end of the spectrum, i.e. most advanced dysplasia. In some geographic regions, high-grade dysplasia is parenthetically referred to as “carcinoma in situ”. As in the former three-tiered classification, this revised two-tiered classification is also based ONLY on the histology, and the lesions are graded on the basis of the highest degree of architectural and cytologic atypia identified anywhere within the lesion (Figures 1–3).
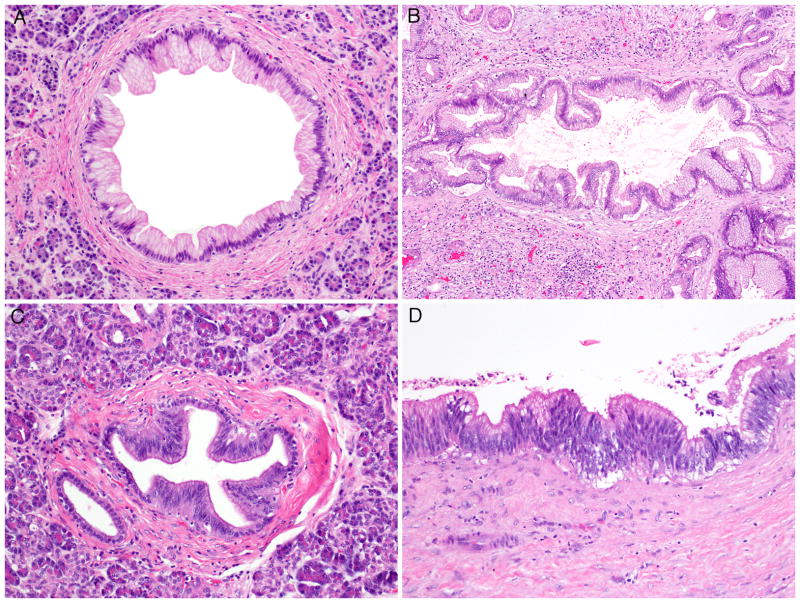
Figure 1.
Low-grade PanINs. A. Low-grade PanIN previously regarded as PanIN-1a in WHO 2010. B. Low-grade PanIN previously regarded as PanIN-1b in WHO 2010. C and D. Low-grade PanIN previously regarded as PanIN-2 in WHO 2010. All panels are hematoxylin and eosin staining. Original magnifications were A–C, 10×; D, 20×.
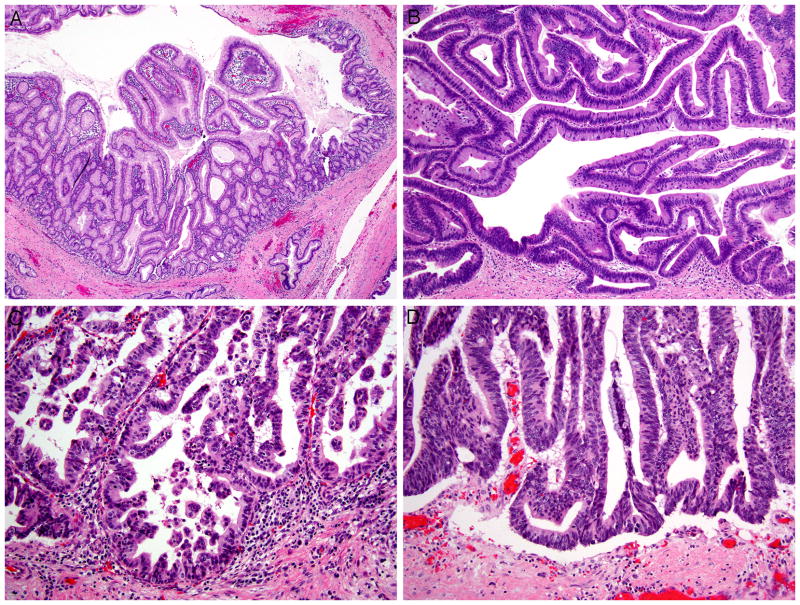
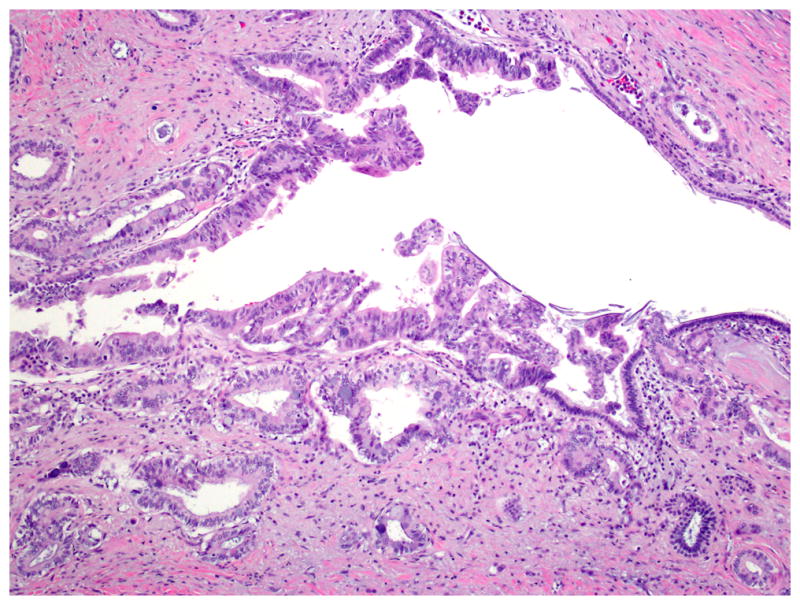
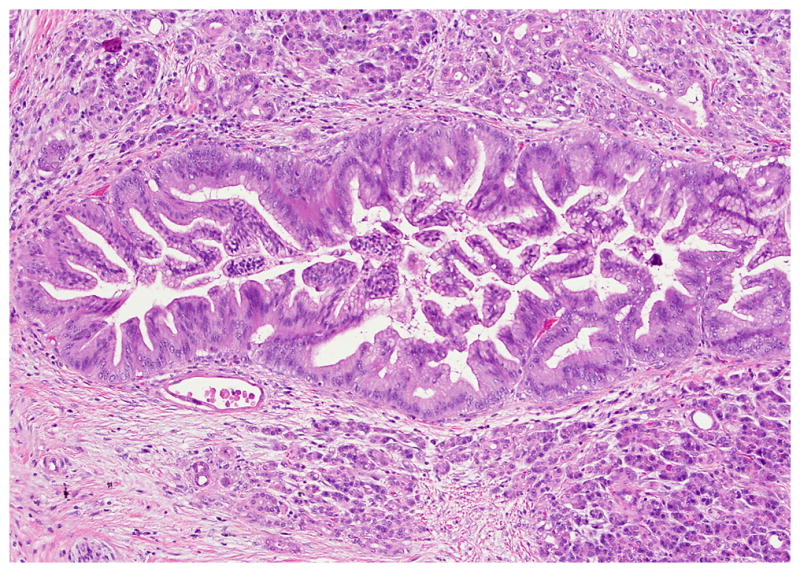
Figure 3.
IPMNs in various grades. A. IPMN, low-grade, previously regarded as IPMN with low-grade dysplasia in WHO 2010. B. IPMN, low-grade, previously regarded as IPMN with intermediate-grade dysplasia in WHO 2010. C and D. IPMN, high-grade, previously regarded as IPMN with high-grade dysplasia in WHO 2010. All panels are hematoxylin and eosin staining. Original magnifications were A, 4×; B–D, 20×.
Reporting of Cases
The recommended terminology is:
-
For PanIN:
Low-grade PanIN
High-grade PanIN (“carcinoma in situ”, according to local usage)
-
For tumor-forming intraepithelial neoplasms (IPMN and MCN)
IPMN/MCN, low-grade
-
IPMN/MCN, high-grade
IPMN (and MCN), high-grade may be further classified with the relevant local usage such as “carcinoma in situ” in parenthesis.
-
For cases that also have an associated invasive carcinoma
-
IPMN/MCN, ___ grade, with an associated invasive carcinoma
Invasive carcinoma with an associated IPMN/MCN may also be used.
-
In reporting IPMN and MCN, it is suggested that the order of reporting starts with the entity name (IPMN or MCN), followed by the grade, and then the morphologic type (gastric, intestinal, pancreatobiliary, or oncocytic) 37, an involved portion of ducts (the main or branch) (if relevant), and size. It is of utmost relevance to determine and document the presence or absence of an associated invasive carcinoma. If there is an associated invasive carcinoma, the pathology report should separately and clearly document the detailed characteristics of the precursor lesion (IPMN or MCN) and the invasive components (type, grade, size, and the stage) 38. Although the recommended terminology is IPMN or MCN with an associated invasive carcinoma, in order to report the biologically more important lesion first, “Invasive carcinoma with an associated IPMN/MCN” may also be used. Following the WHO 2010’s recommendation, the terms “invasive IPMN/MCN”, “malignant IPMN/MCN”, or “mucinous cystadenocarcinoma” (which have been used in the literature to describe a wide variety of neoplasms ranging from precursors with high-grade dysplasia to invasive carcinoma) should be avoided, as they are non-specific and may create confusion and prevent accurate comparison of data from different centers,39–53.
During transition to the revised two-tiered classification and for research purposes, the diagnosis may be further supplemented with the former three-tiered classification for each precursor lesion 1, 2. If the former three-tiered classification is used, it should be reported in parentheses after the main diagnosis. For example, a neoplasm previously reported as “MCN with intermediate-grade dysplasia” would now be reported as MCN, low-grade (intermediate-grade dysplasia in WHO-2010).
Because they are so common and of no proven clinical significance 13, 30, 31, 35, 54–57, it was agreed that low-grade PanIN lesions (PanIN-1 or PanIN-2 in WHO 2010) do not need to be reported in pathology reports, especially in patients with an invasive ductal adenocarcinoma. Given the low rate of progression from low-grade PanIN to invasive carcinoma, the clinical significance of isolated foci of low-grade PanIN is regarded to be negligible 58. If these lesions are to be included in reports, it is advisable to emphasize their clinical inconsequentiality in order to avoid overtreatment 30.
In contrast, if high-grade PanINs (PanIN-3 in WHO 2010) are encountered, these lesions may have clinical significance and should be reported, particularly in the absence of an invasive carcinoma elsewhere in the pancreas. In fact, high-grade PanINs are usually found in pancreata with an invasive carcinoma, and they may in fact serve as a surrogate marker for invasion elsewhere in the organ 31, 59.
ASSESSMENT OF PanIN AND IPMN LESIONS ON RESECTION MARGINS
Current data suggests that the presence of PanIN lesions at a surgical resection margin does not affect the survival of patients who undergo resection for invasive carcinoma; i.e., no significant difference in the median survival time was observed between patients with PanIN of any grade at a resection margin and those without PanIN at the margin 30. In the absence of an established invasive carcinoma, if high-grade PanIN is present at a margin, additional surgery may be justifiable because of the rarity of high-grade PanIN lesions in the absence of an invasive carcinoma 60.
The clinical significance of IPMN at a resection margin in patients without an invasive carcinoma is less clear 61–65. Some have reported that recurrences after surgical resection are associated with the presence of IPMN at a margin, while others have not found such an association 61–65. Other data suggest that the risk for recurrence is more related to the overall grade of dysplasia within the IPMN than with the status of the margin 66. Many studies of recurrence after resection of IPMNs are limited by relatively short follow-up, and emerging data suggest that patients with resected IPMNs are at increased risk of developing a metachronous IPMN or invasive carcinoma after prolonged follow-up 67–69. In addition, IPMNs can be multifocal, and this multifocality can confound the interpretation of recurrences after the surgical resection of an IPMN 70. Regardless of whether disease in the remnant pancreas is caused by recurrence of the patient’s original IPMN or the growth of a separate lesion, careful clinical follow-up after the resection is warranted for patients with an IPMN of any grade dysplasia and any margin status.
Intraoperative frozen sections may be used to evaluate resection marginal status 71. At research centers, frozen sections can also be used to guide the harvesting of tissues for research purposes. The value of frozen sections in evaluating the main lesion in IPMNs is less clear, unless an intraoperative decision would depend on the results of the frozen section diagnosis. Similarly, there are few data to guide the use of frozen sections in evaluating resection margins for IPMNs without an associated invasive carcinoma. Although the evidence is not strong, further resection is recommended if high-grade dysplasia is present at a resection margin at the time of frozen section 72. Due to the low probability of a positive result, evaluation of margin status may be inconsequential for cases with branch duct IPMNs without main duct dilatation. If a margin is submitted for frozen section diagnosis, the grade of dysplasia at the margin may be reported without distinguishing IPMN from PanIN because such distinction can be difficult based purely on histology 2. In this case, a diagnosis of intraductal mucinous epithelium with low- /high-grade dysplasia (PanIN or IPMN) may be rendered.
DIFFERENTIAL DIAGNOSIS OF PRECURSOR LESIONS
Lesions Between PanIN and IPMN
Although PanINs and IPMNs are distinct intraductal neoplasms in their most classic manifestations73, the distinction between PanINs and IPMNs is often a difficult task in daily practice. As discussed in the previous consensus report, PanINs and IPMNs share fundamental common features, i.e., they are composed of mucinous columnar cells with papillary configuration, they exhibit various grades of atypia, and they may involve both smaller and major ducts 2. Size is the major feature used to distinguish these lesions: PanINs usually are < 0.5 cm, while IPMNs usually are ≥ 1.0 cm in diameter 2. Although this classification is clinically useful (as clinical imaging can routinely detect lesions ≥ 1 cm), the classification does leave a “no man’s land” of lesions between 0.5 and 1.0 cm. Such lesions can be large PanINs or small IPMNs.
One feature that can be useful in classifying lesions between 0.5 and 1 cm is the direction of differentiation of the neoplastic cells. The epithelial cells in almost all PanINs have gastric-foveolar differentiation. By contrast, IPMNs can have a variety of different directions of differentiation including gastric, intestinal, pancreatobiliary, and oncocytic 37. Therefore, although small gastric-type IPMNs are difficult to distinguish from large PanINs, lesions with intestinal or oncocytic differentiation are most likely IPMNs. Unfortunately, the majority of intraductal lesions in the size range of 0.5–1.0 cm exhibit gastric differentiation, limiting the utility of this criterion.
GNAS mutations typically occur in IPMNs, mostly of intestinal or gastric subtype 22, 23, 74, whereas they are very rarely encountered in PanIN lesions 75. Therefore, GNAS mutations could be used for the differential diagnosis of small cyst-forming lesions ≤ 1.0 cm, as has been recently shown 75, 76 (Figure 4). At the molecular level, it is clear that IPMNs start as smaller lesions, some of which overlap with PanIN lesions.
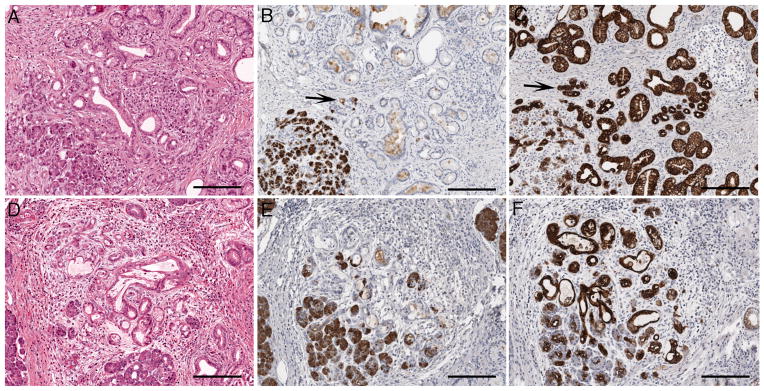
Figure 4.
Incipient IPMN lined with intestinal-type papillae.
Based on these results, it is recognized that there is likely a continuum of progression in gastric-type lesions from some that would be initially classified as a PanIN and later be recognizable as IPMN because of larger size. The term incipient IPMN can be applied to lesions between 0.5 and 1.0 cm in diameter with long finger-like papillae, villous intestinal or oncocytic differentiation, or with a GNAS mutation. Small cystic gastric-type lesions without any features of the incipient IPMN should be documented descriptively (such as intraductal neoplasm, 0.7 cm, lined by low-grade gastric type epithelium; differential diagnosis includes low-grade PanIN and IPMN, low-grade). Finally, because such thin walled cysts may collapse during resection or pathological examination, the suggestion was made that radiographic findings may be integrated to determine the actual size of small cysts. When this is done, some lesions that microscopically fall in the 0.5 to 1 cm range may in fact be larger and reach diagnostic size criteria for an IPMN.
IPMN with Concomitant Invasive Carcinoma
It is now well-established that invasive carcinoma can arise from an IPMN 74. However, invasive carcinoma can also arise independently in a pancreas that also contains an IPMN elsewhere. This has been previously referred to as IPMN with “concomitant” invasive carcinoma to distinguish it from cases in which the relation of the IPMN and the invasive carcinoma is more clearly evident 77, 78. These two situations in which IPMN and invasive carcinoma occur in the same pancreas are conceptually quite distinct: the IPMN is a direct precursor to the carcinoma in IPMN-associated carcinoma, while the IPMN and carcinoma are separate and likely independent in IPMN with a concomitant invasive carcinoma. These two situations may also be clinically distinct. For example, Yamaguchi, et al. found that IPMNs and their associated invasive carcinomas are enriched for main duct IPMNs and colloid carcinomas, whereas IPMNs with concomitant carcinoma are almost always branch duct type, and the invasive carcinomas are rarely colloid carcinomas 78. Interestingly, the reported survival difference between the concomitant invasive carcinomas and invasive carcinomas without IPMN suggest that the presence of IPMN (even separate from the invasive carcinoma) is associated with improved patient outcome 78. Some of this difference is lost after adjusting for tumor stage, suggesting that the survival difference is due to earlier diagnosis of IPMN with a concomitant invasive carcinoma 79. Further clinicopathological and genetic studies are needed to definitively characterize the relationship of IPMNs with concomitant invasive carcinoma and to determine the clinical relevance of this entity.
Although conceptually concomitant invasive carcinoma ought to be genetically distinct from an IPMN elsewhere in the gland (in contrast with the “associated” group), there are no definite criteria to clearly distinguish between the two situations on a morphological basis besides a clear transition between in situ and invasive carcinoma supports a carcinoma associated with IPMN while intervening uninvolved pancreas supports that the carcinoma is concomitant rather than associated. In order to produce evidence to support this distinction, radiologic, gross, and microscopic findings should be incorporated. At the pathologic level, we therefore recommend careful gross measurement of the distance between the IPMN and the invasive carcinoma, as well as extensive or complete histologic sampling of intervening pancreatic tissue to determine the microscopic relationship of the IPMN to the invasive carcinoma. Although currently only performed in the research setting, genetic studies may indicate that concomitant invasive carcinomas are independent from the IPMN in contrast to IPMN-associated carcinomas, which should share most genetic alterations with the IPMN.
Intraductal Spread of Invasive Carcinoma
Invasive ductal adenocarcinoma can invade back into and extend along the duct system, morphologically mimicking intraductal neoplasia such as PanIN or even IPMN (Figure 5). Although few studies address this specific issue, this form of intraductal spread, also known as “cancerization of the ducts,” is common and has been reported in as many as 70% of resections for invasive pancreatic cancer 80. This difficulty has hampered research on PanIN lesions in pancreata with an invasive cancer, as the investigator can never be certain if the lesion being studied is a true precursor lesion or just invasive carcinoma growing along a duct.
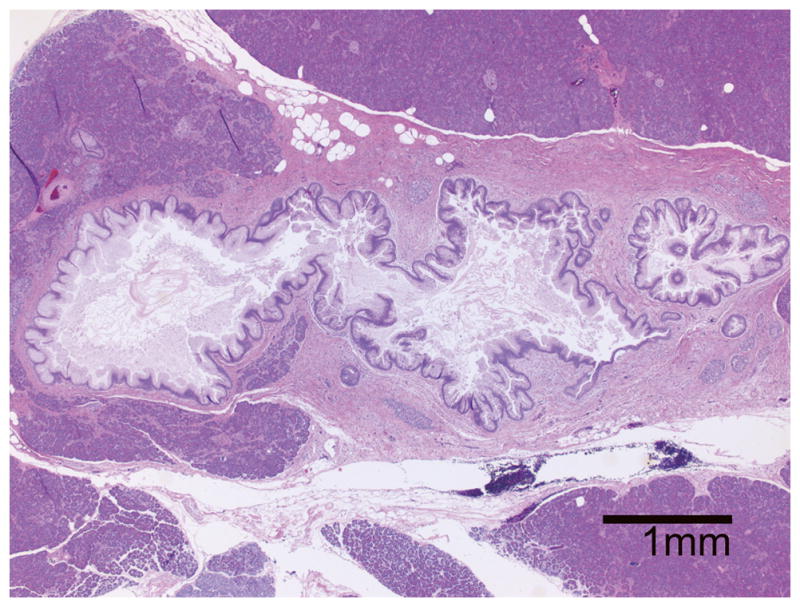
Figure 5.
Intraductal spread of invasive carcinoma. Highly atypical epithelia undistinguishable from invasive carcinoma line a duct. Front-formation between normal cuboidal epithelia and the atypical epithelia can be recognized. Hematoxylin and eosin staining. An original magnification was 10×.
The meeting participants reached the consensus that the term intraductal spread of invasive carcinoma should be used to describe these lesions. This consensus was reached with the understanding that intraductal spread of invasive carcinoma can sometimes be impossible to distinguish definitively from high-grade PanIN, as both consist of cytologically malignant epithelium within a duct. We also recognize the difficulty in dealing with such lesions at resection margins, particularly on frozen section.
Macroscopic Cysts with Flat Mucinous Lining
Cysts with predominantly flat (i.e. non papillary) mucinous lining, usually with gastric phenotype (MUC1 and MUC2 negative, MUC5AC positive) and at most minimal atypia, are sometimes encountered in daily practice (Figure 6). These cysts lack ovarian-type stroma and are >1 cm. These lesions have been addressed with different terms in the literature, depending for instance on the features of the surrounding pancreatic tissue. In the presence of an obstruction of the pancreatic duct, they have been interpreted as retention cysts with partial PanIN1-lining 3. Lesions with no visible obstructive process surrounded by paucicellular fibrous bands have been termed as “mucinous non-neoplastic cysts” 81 or “cystic mucinous duct lesion” (Figure 6) 82. Although their pathogenesis remains elusive, the participants felt that these lesions are benign with no potential for progression and should be clearly distinguished from IPMN and MCN. The term simple mucinous cyst is recommended.
Figure 6.
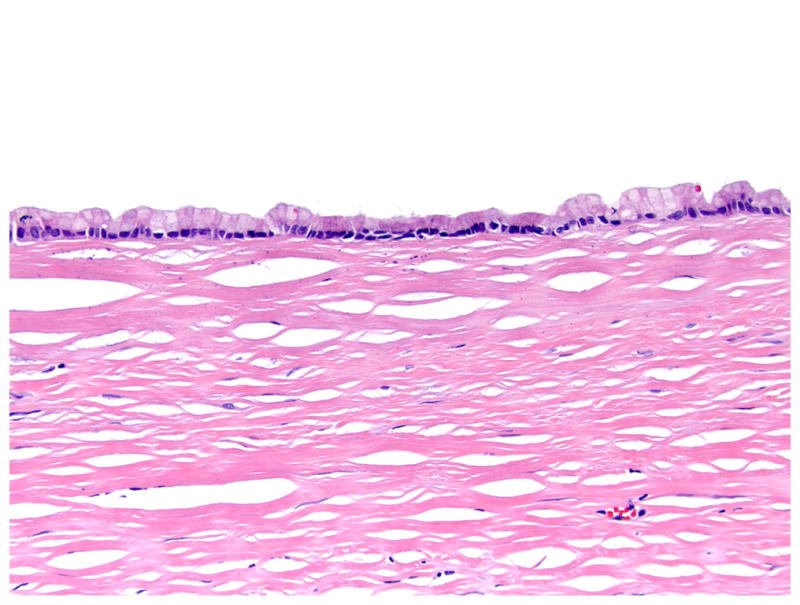
Macroscopic cyst with flat mucinous lining. A cyst with predominantly flat mucinous lining with gastric phenotype is shown. Note no ovarian-like stroma. Hematoxylin and eosin staining. An original magnification was 20×.
ACINAR-DUCTAL METAPLASIA AND ATYPICAL FLAT LESIONS
Acinar-Ductal Metaplasia
A growing body of evidence, mostly coming from recently developed GEMMs but also based on observations in the pancreas of individuals with a history of familial pancreatic cancer, supports the concept of a possible alternative pathway to the development of invasive carcinoma, originating through so-called acinar-ductal metaplasia (ADM). It is suggested that ADM could be related to ductal carcinogenesis along a metaplasia-dysplasia-cancer sequence 83.
ADM lesions are usually associated with fibrosis and inflammation, and the formation of tubular complexes is accompanied by loss of acinar markers and progressive increase of ductal markers (Figure 7) 84–86. The role of ADM as a possible precursor lesion of infiltrating pancreatic cancer has been boosted in the last years by numerous mouse models, which have shown that KRAS-based genetic targeting of acinar cells leads to the development ADM, PanIN, and invasive carcinoma 87–89, while genetically targeting the mature ductal compartment produces little change 90, 91. ADM lesions have been described in humans, but the biological significance of these lesions is unclear 92, 93. ADM is quite common in pancreatic resection specimens for both inflammatory and neoplastic diseases and can harbour KRAS mutations 94, 95. On the other hand, genetic analyses of human PanIN lesions and their associated ADM suggest that the two lesions are not always genetically linked, as in some instances a KRAS gene mutation can be found in a PanIN but not in its associated ADM 4, 94–96.
Figure 7.
Acinar-ductal metaplasia (ADM) and the atypical flat lesion (AFL) in the human pancreas. AC: ADM presents as an intralobular change characterized by progressive replacement of acini by ductular structures, which might display intracytoplasmic mucin, thereby resembling low-grade PanIN. Arrows indicate hybrid ductuli with co-expression of trypsin (B) and CK7 (C). Scale bars: 200μm. D–F: AFL are intralobular ductular proliferations with cytological atypia surrounded by a loose matrix with inflammatory infiltrates. AFL are located in ADM areas and may show focally retained tryspin expression (E), but mostly display a ductal phenotype with strong and diffuse CK7 staining (F). Scale bars: 200μm.
Atypical Flat Lesions
Atypical flat lesions (AFLs) have recently been described. They are mostly non-mucinous, intralobular aggregates of small ducts usually measuring less than 0.5 cm, lined by cuboidal cells with cytologic atypia and surrounded by cellular stroma, often with whorls of spindle cells in a myxomatous matrix (Figure 7) 97. AFLs were first described in genetically engineered mouse models, where they seem related to the process of ADM. However, AFLs are distinguished from ADM by the presence of cytological atypia and their peculiar stromal reaction (Figure 7). Due to their immunophenotypical and molecular resemblance to invasive carcinoma in mouse models, it has been hypothesized that AFLs are also alternative precursor lesions. Morphologically similar lesions have been identified in the pancreata of human patients with an inherited predisposition for pancreatic cancer. In humans, AFLs occur in areas of lobulocentric atrophy and often harbour KRAS mutations 97, 98. Whether AFLs represent alternative precursors to invasive carcinoma or are merely reactive changes or retrograde growth of PanINs in humans remains to be determined. ADM and AFL may be included in histopathological descriptions for research purposes, but they need not be documented in routine clinical pathological reports until their true significance is known.
CONCLUSIVE REMARKS
Recent advances in genetics and molecular biology, as well as more sensitive imaging methods and new surgical techniques, have improved our understanding of the precursor lesions that give rise to invasive carcinoma in the pancreas. There is now overwhelming evidence in the literature for a variety of organs that the clinical management of precursor lesions is best served by two-tiered classification systems. In these systems, the uppermost end of the spectrum (those that represent the most advanced dysplasia) requires careful clinical attention and treatment 99–101, while lower grade lesions lack a significant risk for progression to invasive carcinoma, and as such, do not warrant therapy 102–107. These advances represent the basis for the introduction of two-tiered classification systems for PanIN, IPMN and MCN described here. Furthermore, it has been shown that two-tiered systems improve concordance and uniformity over three-tiered systems 1, 108–113. Even in pure morphology, the two-tiered system is suggested to classify the dysplasia grade of precursor lesions most appropriately114. The applicability of the proposed two-tiered classification system to cytopathology is, however, potentially problematic because cytologic (or any preoperative) diagnosis is not intended to establish the final grade of dysplasia but rather to provide an assessment of the risk of finding high-grade dysplasia or invasive carcinoma in the resected specimen, and it is therefore we conclude that most of the classification issues discussed above are not applicable to pancreatic fine needle aspiration specimens. While our recommendations concerning differential diagnosis of precursor lesions, frozen section diagnostic, terminology and reporting are supported by experimental and clinical data, strong evidence for some of the topics addressed in this manuscript (e.g. definition of incipient IPMN; distinction between carcinoma with concomitant IPMN and carcinoma originating from IPMN; significance of ADM) is still lacking.
Despite these limitations, we believe that a more clinically relevant classification of precursor lesions, together with the use of standardized nomenclature and advances in molecular testing, will help answer most of the open questions outlined in this paper, and in particular those that are prone to have major impact on diagnosis, treatment and prognosis of patients with pancreatic diseases.
Figure 2.
High-grade PanIN previously regarded as PanIN-3 in WHO 2010. This lesion may be termed as carcinoma in situ in some geographical regions. Hematoxylin and eosin staining. An original magnification was 20×.
Acknowledgments
Source of Funding: The meeting at which this classification was established was funded by the Sol Goldman Pancreatic Cancer Research Center supported by National Institutes of Health grant (P50 CA62924).
The authors thank Mrs. Sandra Markowitz for her invaluable assistance and hard work arranging the meeting at Johns Hopkins. The authors also thank to Drs. Michelle Reid, Carlie Sigel, and Edward Stelow for providing their expertise in the potential implications of the revised classification in cytopathology practice.
Footnotes
This study was presented in part at the annual meeting of the United States and Canadian Academy of Pathology in Boston, March 2015.
Conflicts of Interest: The authors declare no conflicts of interest.
References
- 1.Hruban RH, Adsay NV, Albores-Saavedra J, et al. Pancreatic intraepithelial neoplasia: a new nomenclature and classification system for pancreatic duct lesions. Am J Surg Pathol. 2001;25:579–586. doi: 10.1097/00000478-200105000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Hruban RH, Takaori K, Klimstra DS, et al. An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol. 2004;28:977–987. doi: 10.1097/01.pas.0000126675.59108.80. [DOI] [PubMed] [Google Scholar]
- 3.Hruban RH, Pitman MB, Klimstra DS. Tumors of the pancreas. Washington, DC: American Registry of Pathology; 2007. [Google Scholar]
- 4.Adsay NV, Fukushima N, Furukawa T, et al. Intraductal neoplasms of the pancreas. In: Bosman FT, Hruban RH, Carneiro F, et al., editors. WHO Classification of Tumours of the Digestive System. Lyon: IARC; 2010. pp. 304–313. [Google Scholar]
- 5.Hruban RH, Adsay NV, Albores-Saavedra J, et al. Pathology of genetically engineered mouse models of pancreatic exocrine cancer: consensus report and recommendations. Cancer Res. 2006;66:95–106. doi: 10.1158/0008-5472.CAN-05-2168. [DOI] [PubMed] [Google Scholar]
- 6.Wada K. p16 and p53 gene alterations and accumulations in the malignant evolution of intraductal papillary-mucinous tumors of the pancreas. J Hepatobiliary Pancreat Surg. 2002;9:76–85. doi: 10.1007/s005340200007. [DOI] [PubMed] [Google Scholar]
- 7.Fujii H, Inagaki M, Kasai S, et al. Genetic progression and heterogeneity in intraductal papillary-mucinous neoplasms of the pancreas. Am J Pathol. 1997;151:1447–1454. [PMC free article] [PubMed] [Google Scholar]
- 8.Mueller J, Gansauge S, Mattfeldt T. P53 mutation but not p16/MTS1 mutation occurs in intraductal papillary mucinous tumors of the pancreas. Hepatogastroenterology. 2003;50:541–544. [PubMed] [Google Scholar]
- 9.Fukushima N, Sato N, Ueki T, et al. Aberrant methylation of preproenkephalin and p16 genes in pancreatic intraepithelial neoplasia and pancreatic ductal adenocarcinoma. Am J Pathol. 2002;160:1573–1581. doi: 10.1016/S0002-9440(10)61104-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lohr M, Kloppel G, Maisonneuve P, et al. Frequency of K-ras mutations in pancreatic intraductal neoplasias associated with pancreatic ductal adenocarcinoma and chronic pancreatitis: a meta-analysis. Neoplasia. 2005;7:17–23. doi: 10.1593/neo.04445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seki M, Ninomiya E, Hayashi K, et al. Widespread and multifocal carcinomas in situ (CISs) through almost the entire pancreas: report of a case with preoperative cytological diagnosis. Langenbecks Arch Surg. 2010;395:589–592. doi: 10.1007/s00423-009-0579-4. [DOI] [PubMed] [Google Scholar]
- 12.Kawada N, Uehara H, Takada R, et al. Microinvasion of high-grade pancreatic intraepithelial neoplasia. Case Rep Gastroenterol. 2013;7:30–36. doi: 10.1159/000346693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Konstantinidis IT, Vinuela EF, Tang LH, et al. Incidentally discovered pancreatic intraepithelial neoplasia: what is its clinical significance? Ann Surg Oncol. 2013;20:3643–3647. doi: 10.1245/s10434-013-3042-2. [DOI] [PubMed] [Google Scholar]
- 14.Lami G, Biagini MR, Galli A. Endoscopic ultrasonography for surveillance of individuals at high risk for pancreatic cancer. World J Gastrointest Endosc. 2014;6:272–285. doi: 10.4253/wjge.v6.i7.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.LeBlanc JK, Chen JH, Al-Haddad M, et al. Can endoscopic ultrasound predict pancreatic intraepithelial neoplasia lesions in chronic pancreatitis?: a retrospective study of pathologic correlation. Pancreas. 2014;43:849–854. doi: 10.1097/MPA.0000000000000142. [DOI] [PubMed] [Google Scholar]
- 16.Ito H, Kawaguchi Y, Kawashima Y, et al. A case of pancreatic intraepithelial neoplasia that was difficult to diagnose preoperatively. Case Rep Oncol. 2015;8:30–36. doi: 10.1159/000371842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matsuda Y, Ishiwata T, Izumiyama-Shimomura N, et al. Gradual telomere shortening and increasing chromosomal instability among PanIN grades and normal ductal epithelia with and without cancer in the pancreas. PLoS One. 2015;10:e0117575. doi: 10.1371/journal.pone.0117575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rebours V, Gaujoux S, d'Assignies G, et al. Obesity and fatty pancreatic infiltration are risk factors for pancreatic precancerous lesions (PanIN) Clin Cancer Res. 2015 doi: 10.1158/1078-0432.CCR-14-2385. in press. [DOI] [PubMed] [Google Scholar]
- 19.Bartsch DK, Dietzel K, Bargello M, et al. Multiple small “imaging” branch-duct type intraductal papillary mucinous neoplasms (IPMNs) in familial pancreatic cancer: indicator for concomitant high grade pancreatic intraepithelial neoplasia? Fam Cancer. 2013;12:89–96. doi: 10.1007/s10689-012-9582-y. [DOI] [PubMed] [Google Scholar]
- 20.Fritz S, Fernandez-del Castillo C, Mino-Kenudson M, et al. Global genomic analysis of intraductal papillary mucinous neoplasms of the pancreas reveals significant molecular differences compared to ductal adenocarcinoma. Ann Surg. 2009;249:440–447. doi: 10.1097/SLA.0b013e31819a6e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones S, Zhang X, Parsons DW, et al. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science. 2008;321:1801–1806. doi: 10.1126/science.1164368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu J, Jiao Y, Dal Molin M, et al. Whole-exome sequencing of neoplastic cysts of the pancreas reveals recurrent mutations in components of ubiquitin-dependent pathways. Proc Natl Acad Sci U S A. 2011;108:21188–21193. doi: 10.1073/pnas.1118046108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Furukawa T, Kuboki Y, Tanji E, et al. Whole-exome sequencing uncovers frequent GNAS mutations in intraductal papillary mucinous neoplasms of the pancreas. Sci Rep. 2011;1:161. doi: 10.1038/srep00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yachida S, Vakiani E, White CM, et al. Small cell and large cell neuroendocrine carcinomas of the pancreas are genetically similar and distinct from well-differentiated pancreatic neuroendocrine tumors. Am J Surg Pathol. 2012;36:173–184. doi: 10.1097/PAS.0b013e3182417d36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jiao Y, Yonescu R, Offerhaus GJ, et al. Whole-exome sequencing of pancreatic neoplasms with acinar differentiation. J Pathol. 2014;232:428–435. doi: 10.1002/path.4310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park M, Kim M, Hwang D, et al. Characterization of gene expression and activated signaling pathways in solid-pseudopapillary neoplasm of pancreas. Mod Pathol. 2014;27:580–593. doi: 10.1038/modpathol.2013.154. [DOI] [PubMed] [Google Scholar]
- 27.Furlan D, Sahnane N, Bernasconi B, et al. APC alterations are frequently involved in the pathogenesis of acinar cell carcinoma of the pancreas, mainly through gene loss and promoter hypermethylation. Virchows Arch. 2014;464:553–564. doi: 10.1007/s00428-014-1562-1. [DOI] [PubMed] [Google Scholar]
- 28.Garcia-Carracedo D, Chen ZM, Qiu W, et al. PIK3CA mutations in mucinous cystic neoplasms of the pancreas. Pancreas. 2014;43:245–249. doi: 10.1097/MPA.0000000000000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tanaka M, Fernandez-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183–197. doi: 10.1016/j.pan.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Matthaei H, Hong SM, Mayo SC, et al. Presence of pancreatic intraepithelial neoplasia in the pancreatic transection margin does not influence outcome in patients with R0 resected pancreatic cancer. Ann Surg Oncol. 2011;18:3493–3499. doi: 10.1245/s10434-011-1745-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andea A, Sarkar F, Adsay VN. Clinicopathological correlates of pancreatic intraepithelial neoplasia: a comparative analysis of 82 cases with and 152 cases without pancreatic ductal adenocarcinoma. Mod Pathol. 2003;16:996–1006. doi: 10.1097/01.MP.0000087422.24733.62. [DOI] [PubMed] [Google Scholar]
- 32.Winter JM, Cameron JL, Lillemoe KD, et al. Periampullary and pancreatic incidentaloma: a single institution's experience with an increasingly common diagnosis. Ann Surg. 2006;243:673–680. doi: 10.1097/01.sla.0000216763.27673.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laffan TA, Horton KM, Klein AP, et al. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol. 2008;191:802–807. doi: 10.2214/AJR.07.3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kent TS, Jr, CM, Callery MP. Intraductal papillary mucinous neoplasm and the pancreatic incidentaloma. World J Gastrointest Surg. 2010;2:319–323. doi: 10.4240/wjgs.v2.i10.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abraham SC, Wilentz RE, Yeo CJ, et al. Pancreaticoduodenectomy (Whipple resections) in patients without malignancy: are they all 'chronic pancreatitis'? Am J Surg Pathol. 2003;27:110–120. doi: 10.1097/00000478-200301000-00012. [DOI] [PubMed] [Google Scholar]
- 36.Allen PJ, D'Angelica M, Gonen M, et al. A selective approach to the resection of cystic lesions of the pancreas: results from 539 consecutive patients. Ann Surg. 2006;244:572–582. doi: 10.1097/01.sla.0000237652.84466.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Furukawa T, Kloppel G, Volkan Adsay N, et al. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch. 2005;447:794–799. doi: 10.1007/s00428-005-0039-7. [DOI] [PubMed] [Google Scholar]
- 38.Adsay V, Mino-Kenudson M, Furukawa T, et al. Pathologic Evaluation and Reporting of Intraductal Papillary Mucinous Neoplasms of the Pancreas and Other Tumoral Intraepithelial Neoplasms of Pancreatobiliary Tract: Recommendations of Verona Consensus Meeting. Ann Surg. doi: 10.1097/SLA.0000000000001173. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ammori JB, Do RK, Brennan MF, et al. Uncinate duct dilation in intraductal papillary mucinous neoplasms of the pancreas: a radiographic finding with potentially increased malignant potential. J Gastrointest Surg. 2014;18:911–916. doi: 10.1007/s11605-014-2449-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shimizu Y, Yamaue H, Maguchi H, et al. Predictors of malignancy in intraductal papillary mucinous neoplasm of the pancreas: analysis of 310 pancreatic resection patients at multiple high-volume centers. Pancreas. 2013;42:883–888. doi: 10.1097/MPA.0b013e31827a7b84. [DOI] [PubMed] [Google Scholar]
- 41.Ohno E, Itoh A, Kawashima H, et al. Malignant transformation of branch duct-type intraductal papillary mucinous neoplasms of the pancreas based on contrast-enhanced endoscopic ultrasonography morphological changes: focus on malignant transformation of intraductal papillary mucinous neoplasm itself. Pancreas. 2012;41:855–862. doi: 10.1097/MPA.0b013e3182480c44. [DOI] [PubMed] [Google Scholar]
- 42.Hwang DW, Jang JY, Lim CS, et al. Determination of malignant and invasive predictors in branch duct type intraductal papillary mucinous neoplasms of the pancreas: a suggested scoring formula. J Korean Med Sci. 2011;26:740–746. doi: 10.3346/jkms.2011.26.6.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tomimaru Y, Takeda Y, Tatsumi M, et al. Utility of 2-[18F] fluoro-2-deoxy-D-glucose positron emission tomography in differential diagnosis of benign and malignant intraductal papillary-mucinous neoplasm of the pancreas. Oncol Rep. 2010;24:613–620. doi: 10.3892/or_00000899. [DOI] [PubMed] [Google Scholar]
- 44.Mimura T, Masuda A, Matsumoto I, et al. Predictors of malignant intraductal papillary mucinous neoplasm of the pancreas. J Clin Gastroenterol. 2010;44:e224–229. doi: 10.1097/MCG.0b013e3181d8fb91. [DOI] [PubMed] [Google Scholar]
- 45.Shimamoto T, Tani M, Kawai M, et al. MUC1 is a useful molecular marker for malignant intraductal papillary mucinous neoplasms in pancreatic juice obtained from endoscopic retrograde pancreatography. Pancreas. 2010;39:879–883. doi: 10.1097/MPA.0b013e3181d6ba04. [DOI] [PubMed] [Google Scholar]
- 46.Bausch D, Mino-Kenudson M, Fernandez-Del Castillo C, et al. Plectin-1 is a biomarker of malignant pancreatic intraductal papillary mucinous neoplasms. J Gastrointest Surg. 2009;13:1948–1954. doi: 10.1007/s11605-009-1001-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Le H, Ziogas A, Rhee JM, et al. A population-based, descriptive analysis of malignant intraductal papillary mucinous neoplasms of the pancreas. Cancer Epidemiol Biomarkers Prev. 2008;17:2737–2741. doi: 10.1158/1055-9965.EPI-08-0417. [DOI] [PubMed] [Google Scholar]
- 48.Cone MM, Rea JD, Diggs BS, et al. Predicting malignant intraductal papillary mucinous neoplasm: a single-center review. Am J Surg. 2011;201:575–579. doi: 10.1016/j.amjsurg.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 49.Fritz S, Hackert T, Hinz U, et al. Role of serum carbohydrate antigen 19–9 and carcinoembryonic antigen in distinguishing between benign and invasive intraductal papillary mucinous neoplasm of the pancreas. Br J Surg. 2011;98:104–110. doi: 10.1002/bjs.7280. [DOI] [PubMed] [Google Scholar]
- 50.Simons JP, Ng SC, Shah SA, et al. Malignant intraductal papillary mucinous neoplasm: are we doing the right thing? J Surg Res. 2011;167:251–257. doi: 10.1016/j.jss.2009.05.035. [DOI] [PubMed] [Google Scholar]
- 51.Lee CJ, Scheiman J, Anderson MA, et al. Risk of malignancy in resected cystic tumors of the pancreas < or =3 cm in size: is it safe to observe asymptomatic patients? A multi-institutional report. J Gastrointest Surg. 2008;12:234–242. doi: 10.1007/s11605-007-0381-y. [DOI] [PubMed] [Google Scholar]
- 52.Kawamoto S, Horton KM, Lawler LP, et al. Intraductal papillary mucinous neoplasm of the pancreas: can benign lesions be differentiated from malignant lesions with multidetector CT? Radiographics. 2005;25:1451–1468. doi: 10.1148/rg.256055036. [DOI] [PubMed] [Google Scholar]
- 53.Manfredi R, Graziani R, Motton M, et al. Main pancreatic duct intraductal papillary mucinous neoplasms: accuracy of MR imaging in differentiation between benign and malignant tumors compared with histopathologic analysis. Radiology. 2009;253:106–115. doi: 10.1148/radiol.2531080604. [DOI] [PubMed] [Google Scholar]
- 54.Klöppel G, Bommer G, Ruckert K, et al. Intraductal proliferation in the pancreas and its relationship to human and experimental carcinogenesis. Virchows Arch A Pathol Anat Histol. 1980;387:221–233. doi: 10.1007/BF00430702. [DOI] [PubMed] [Google Scholar]
- 55.Pour PM, Sayed S, Sayed G. Hyperplastic, preneoplastic and neoplastic lesions found in 83 human pancreases. Am J Clin Pathol. 1982;77:137–152. doi: 10.1093/ajcp/77.2.137. [DOI] [PubMed] [Google Scholar]
- 56.Detlefsen S, Sipos B, Feyerabend B, et al. Pancreatic fibrosis associated with age and ductal papillary hyperplasia. Virchows Arch. 2005;447:800–805. doi: 10.1007/s00428-005-0032-1. [DOI] [PubMed] [Google Scholar]
- 57.Ito R, Kondo F, Yamaguchi T, et al. Pancreatic intraepithelial neoplasms in the normal appearing pancreas: on their precise relationship with age. Hepatogastroenterology. 2008;55:1103–1106. [PubMed] [Google Scholar]
- 58.Hruban RH, Klimstra DS. Adenocarcinoma of the pancreas. Semin Diagn Pathol. 2014;31:443–451. doi: 10.1053/j.semdp.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brat DJ, Lillemoe KD, Yeo CJ, et al. Progression of pancreatic intraductal neoplasias to infiltrating adenocarcinoma of the pancreas. Am J Surg Pathol. 1998;22:163–169. doi: 10.1097/00000478-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 60.McCarthy DM, Brat DJ, Wilentz RE, et al. Pancreatic intraepithelial neoplasia and infiltrating adenocarcinoma: analysis of progression and recurrence by DPC4 immunohistochemical labeling. Hum Pathol. 2001;32:638–642. doi: 10.1053/hupa.2001.24991. [DOI] [PubMed] [Google Scholar]
- 61.Fujii T, Kato K, Kodera Y, et al. Prognostic impact of pancreatic margin status in the intraductal papillary mucinous neoplasms of the pancreas. Surgery. 2010;148:285–290. doi: 10.1016/j.surg.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 62.Nakagohri T, Kinoshita T, Konishi M, et al. Surgical outcome of intraductal papillary mucinous neoplasms of the pancreas. Ann Surg Oncol. 2007;14:3174–3180. doi: 10.1245/s10434-007-9546-x. [DOI] [PubMed] [Google Scholar]
- 63.Raut CP, Cleary KR, Staerkel GA, et al. Intraductal papillary mucinous neoplasms of the pancreas: effect of invasion and pancreatic margin status on recurrence and survival. Ann Surg Oncol. 2006;13:582–594. doi: 10.1245/ASO.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 64.Leng KM, Wang ZD, Zhao JB, et al. Impact of pancreatic margin status and lymph node metastases on recurrence after resection for invasive and noninvasive intraductal papillary mucinous neoplasms of the pancreas: a meta-analysis. Dig Surg. 2012;29:213–225. doi: 10.1159/000339334. [DOI] [PubMed] [Google Scholar]
- 65.Frankel TL, LaFemina J, Bamboat ZM, et al. Dysplasia at the surgical margin is associated with recurrence after resection of non-invasive intraductal papillary mucinous neoplasms. HPB (Oxford) 2013;15:814–821. doi: 10.1111/hpb.12137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.White R, D'Angelica M, Katabi N, et al. Fate of the remnant pancreas after resection of noninvasive intraductal papillary mucinous neoplasm. J Am Coll Surg. 2007;204:987–993. doi: 10.1016/j.jamcollsurg.2006.12.040. discussion 993–985. [DOI] [PubMed] [Google Scholar]
- 67.Kang MJ, Jang JY, Lee KB, et al. Long-term prospective cohort study of patients undergoing pancreatectomy for intraductal papillary mucinous neoplasm of the pancreas: implications for postoperative surveillance. Ann Surg. 2014;260:356–363. doi: 10.1097/SLA.0000000000000470. [DOI] [PubMed] [Google Scholar]
- 68.Dejean NM, Dumitra S, Barkun JS. Recurrence of non-invasive intraductal papillary municious neoplasm seven years following total pancreatectomy. Int J Surg Case Rep. 2013;4:789–791. doi: 10.1016/j.ijscr.2013.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tanno S, Nakano Y, Sugiyama Y, et al. Incidence of synchronous and metachronous pancreatic carcinoma in 168 patients with branch duct intraductal papillary mucinous neoplasm. Pancreatology. 2010;10:173–178. doi: 10.1159/000231982. [DOI] [PubMed] [Google Scholar]
- 70.Eguchi H, Ishikawa O, Ohigashi H, et al. Role of intraoperative cytology combined with histology in detecting continuous and skip type intraductal cancer existence for intraductal papillary mucinous carcinoma of the pancreas. Cancer. 2006;107:2567–2575. doi: 10.1002/cncr.22301. [DOI] [PubMed] [Google Scholar]
- 71.Cioc AM, Ellison EC, Proca DM, et al. Frozen section diagnosis of pancreatic lesions. Arch Pathol Lab Med. 2002;126:1169–1173. doi: 10.5858/2002-126-1169-FSDOPL. [DOI] [PubMed] [Google Scholar]
- 72.Gigot JF, Deprez P, Sempoux C, et al. Surgical management of intraductal papillary mucinous tumors of the pancreas: the role of routine frozen section of the surgical margin, intraoperative endoscopic staged biopsies of the Wirsung duct, and pancreaticogastric anastomosis. Arch Surg. 2001;136:1256–1262. doi: 10.1001/archsurg.136.11.1256. [DOI] [PubMed] [Google Scholar]
- 73.Nakanuma Y, Curado M-P, Franceschi S, et al. Intrahepatic cholangiocarcinoma. In: Bosman FT, Hruban RH, Carneiro F, et al., editors. WHO Classification of Tumours of the Digestive System. Lyon: IARC; 2010. pp. 217–224. [Google Scholar]
- 74.Wu J, Matthaei H, Maitra A, et al. Recurrent GNAS mutations define an unexpected pathway for pancreatic cyst development. Sci Transl Med. 2011;3:92ra66. doi: 10.1126/scitranslmed.3002543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kanda M, Matthaei H, Wu J, et al. Presence of somatic mutations in most early-stage pancreatic intraepithelial neoplasia. Gastroenterology. 2012;142:730–733. e739. doi: 10.1053/j.gastro.2011.12.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Matthaei H, Wu J, Dal Molin M, et al. GNAS sequencing identifies IPMN-specific mutations in a subgroup of diminutive pancreatic cysts referred to as “incipient IPMNs”. Am J Surg Pathol. 2014;38:360–363. doi: 10.1097/PAS.0000000000000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yamaguchi K, Ohuchida J, Ohtsuka T, et al. Intraductal papillary-mucinous tumor of the pancreas concomitant with ductal carcinoma of the pancreas. Pancreatology. 2002;2:484–490. doi: 10.1159/000064716. [DOI] [PubMed] [Google Scholar]
- 78.Yamaguchi K, Kanemitsu S, Hatori T, et al. Pancreatic ductal adenocarcinoma derived from IPMN and pancreatic ductal adenocarcinoma concomitant with IPMN. Pancreas. 2011;40:571–580. doi: 10.1097/MPA.0b013e318215010c. [DOI] [PubMed] [Google Scholar]
- 79.Ideno N, Ohtsuka T, Kono H, et al. Intraductal papillary mucinous neoplasms of the pancreas with distinct pancreatic ductal adenocarcinomas are frequently of gastric subtype. Ann Surg. 2013;258:141–151. doi: 10.1097/SLA.0b013e31828cd008. [DOI] [PubMed] [Google Scholar]
- 80.Yamasaki S, Suda K, Nobukawa B, et al. Intraductal spread of pancreatic cancer. Clinicopathologic study of 54 pancreatectomized patients. Pancreatology. 2002;2:407–412. doi: 10.1159/000065089. [DOI] [PubMed] [Google Scholar]
- 81.Kosmahl M, Egawa N, Schroder S, et al. Mucinous nonneoplastic cyst of the pancreas: a novel nonneoplastic cystic change? Mod Pathol. 2002;15:154–158. doi: 10.1038/modpathol.3880507. [DOI] [PubMed] [Google Scholar]
- 82.Krasinskas A, Oakley GJ, Bagci P, et al. Cystic mucinous duct lesion of the pancreas: A clinicopathologic analysis of 40 examples of a diagnostically challenging and terminologically controversial entity. Mod Pathol. 2012;25:445A. [Google Scholar]
- 83.Murtaugh LC, Leach SD. A case of mistaken identity? Nonductal origins of pancreatic “ductal” cancers. Cancer Cell. 2007;11:211–213. doi: 10.1016/j.ccr.2007.02.020. [DOI] [PubMed] [Google Scholar]
- 84.Willemer S, Adler G. Histochemical and ultrastructural characteristics of tubular complexes in human acute pancreatitis. Dig Dis Sci. 1989;34:46–55. doi: 10.1007/BF01536153. [DOI] [PubMed] [Google Scholar]
- 85.Bockman DE, Guo J, Buchler P, et al. Origin and development of the precursor lesions in experimental pancreatic cancer in rats. Lab Invest. 2003;83:853–859. doi: 10.1097/01.lab.0000074918.31303.5a. [DOI] [PubMed] [Google Scholar]
- 86.Shi G, DiRenzo D, Qu C, et al. Maintenance of acinar cell organization is critical to preventing Kras-induced acinar-ductal metaplasia. Oncogene. 2013;32:1950–1958. doi: 10.1038/onc.2012.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.De La OJ, Emerson LL, Goodman JL, et al. Notch and Kras reprogram pancreatic acinar cells to ductal intraepithelial neoplasia. Proc Natl Acad Sci U S A. 2008;105:18907–18912. doi: 10.1073/pnas.0810111105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Guerra C, Schuhmacher AJ, Canamero M, et al. Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell. 2007;11:291–302. doi: 10.1016/j.ccr.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 89.Habbe N, Shi G, Meguid RA, et al. Spontaneous induction of murine pancreatic intraepithelial neoplasia (mPanIN) by acinar cell targeting of oncogenic Kras in adult mice. Proc Natl Acad Sci U S A. 2008;105:18913–18918. doi: 10.1073/pnas.0810097105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ray KC, Bell KM, Yan J, et al. Epithelial tissues have varying degrees of susceptibility to Kras(G12D)-initiated tumorigenesis in a mouse model. PLoS One. 2011;6:e16786. doi: 10.1371/journal.pone.0016786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kopp JL, von Figura G, Mayes E, et al. Identification of Sox9-dependent acinar-to-ductal reprogramming as the principal mechanism for initiation of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;22:737–750. doi: 10.1016/j.ccr.2012.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bockman DE, Boydston WR, Anderson MC. Origin of tubular complexes in human chronic pancreatitis. Am J Surg. 1982;144:243–249. doi: 10.1016/0002-9610(82)90518-9. [DOI] [PubMed] [Google Scholar]
- 93.Parsa I, Longnecker DS, Scarpelli DG, et al. Ductal metaplasia of human exocrine pancreas and its association with carcinoma. Cancer Res. 1985;45:1285–1290. [PubMed] [Google Scholar]
- 94.Esposito I, Seiler C, Bergmann F, et al. Hypothetical progression model of pancreatic cancer with origin in the centroacinar-acinar compartment. Pancreas. 2007;35:212–217. doi: 10.1097/mpa.0b013e31805d0190. [DOI] [PubMed] [Google Scholar]
- 95.Shi C, Hong SM, Lim P, et al. KRAS2 mutations in human pancreatic acinar-ductal metaplastic lesions are limited to those with PanIN: implications for the human pancreatic cancer cell of origin. Mol Cancer Res. 2009;7:230–236. doi: 10.1158/1541-7786.MCR-08-0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Brune K, Abe T, Canto M, et al. Multifocal neoplastic precursor lesions associated with lobular atrophy of the pancreas in patients having a strong family history of pancreatic cancer. Am J Surg Pathol. 2006;30:1067–1076. [PMC free article] [PubMed] [Google Scholar]
- 97.Aichler M, Seiler C, Tost M, et al. Origin of pancreatic ductal adenocarcinoma from atypical flat lesions: a comparative study in transgenic mice and human tissues. J Pathol. 2012;226:723–734. doi: 10.1002/path.3017. [DOI] [PubMed] [Google Scholar]
- 98.Konukiewitz B, Schlitter AM, Berchtold S, et al. Characterization of putative precursor lesions of familial pancreatic cancer. Pancreatology. 2013;13:S14. [Google Scholar]
- 99.Akita H, Takeda Y, Hoshino H, et al. Mural nodule in branch duct-type intraductal papillary mucinous neoplasms of the pancreas is a marker of malignant transformation and indication for surgery. Am J Surg. 2011;202:214–219. doi: 10.1016/j.amjsurg.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 100.Salvia R, Fernandez-del Castillo C, Bassi C, et al. Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg. 2004;239:678–685. doi: 10.1097/01.sla.0000124386.54496.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sugiyama M, Izumisato Y, Abe N, et al. Predictive factors for malignancy in intraductal papillary-mucinous tumours of the pancreas. Br J Surg. 2003;90:1244–1249. doi: 10.1002/bjs.4265. [DOI] [PubMed] [Google Scholar]
- 102.Terris B, Ponsot P, Paye F, et al. Intraductal papillary mucinous tumors of the pancreas confined to secondary ducts show less aggressive pathologic features as compared with those involving the main pancreatic duct. Am J Surg Pathol. 2000;24:1372–1377. doi: 10.1097/00000478-200010000-00006. [DOI] [PubMed] [Google Scholar]
- 103.Irie H, Yoshimitsu K, Aibe H, et al. Natural history of pancreatic intraductal papillary mucinous tumor of branch duct type: follow-up study by magnetic resonance cholangiopancreatography. J Comput Assist Tomogr. 2004;28:117–122. doi: 10.1097/00004728-200401000-00020. [DOI] [PubMed] [Google Scholar]
- 104.Sadakari Y, Ienaga J, Kobayashi K, et al. Cyst size indicates malignant transformation in branch duct intraductal papillary mucinous neoplasm of the pancreas without mural nodules. Pancreas. 2010;39:232–236. doi: 10.1097/MPA.0b013e3181bab60e. [DOI] [PubMed] [Google Scholar]
- 105.Maguchi H, Tanno S, Mizuno N, et al. Natural history of branch duct intraductal papillary mucinous neoplasms of the pancreas: a multicenter study in Japan. Pancreas. 2011;40:364–370. doi: 10.1097/MPA.0b013e31820a5975. [DOI] [PubMed] [Google Scholar]
- 106.Salvia R, Crippa S, Falconi M, et al. Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate? Gut. 2007;56:1086–1090. doi: 10.1136/gut.2006.100628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tanno S, Nakano Y, Nishikawa T, et al. Natural history of branch duct intraductal papillary-mucinous neoplasms of the pancreas without mural nodules: long-term follow-up results. Gut. 2008;57:339–343. doi: 10.1136/gut.2007.129684. [DOI] [PubMed] [Google Scholar]
- 108.Reid BJ, Haggitt RC, Rubin CE, et al. Observer variation in the diagnosis of dysplasia in Barrett's esophagus. Hum Pathol. 1988;19:166–178. doi: 10.1016/s0046-8177(88)80344-7. [DOI] [PubMed] [Google Scholar]
- 109.Fenger C, Bak M, Kronborg O, et al. Observer reproducibility in grading dysplasia in colorectal adenomas: comparison between two different grading systems. J Clin Pathol. 1990;43:320–324. doi: 10.1136/jcp.43.4.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jensen P, Krogsgaard MR, Christiansen J, et al. Observer variability in the assessment of type and dysplasia of colorectal adenomas, analyzed using kappa statistics. Dis Colon Rectum. 1995;38:195–198. doi: 10.1007/BF02052450. [DOI] [PubMed] [Google Scholar]
- 111.Epstein JI, Grignon DJ, Humphrey PA, et al. Interobserver reproducibility in the diagnosis of prostatic intraepithelial neoplasia. Am J Surg Pathol. 1995;19:873–886. doi: 10.1097/00000478-199508000-00002. [DOI] [PubMed] [Google Scholar]
- 112.Waxman AG, Chelmow D, Darragh TM, et al. Revised terminology for cervical histopathology and its implications for management of high-grade squamous intraepithelial lesions of the cervix. Obstet Gynecol. 2012;120:1465–1471. doi: 10.1097/aog.0b013e31827001d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Darragh TM, Colgan TJ, Thomas Cox J, et al. The Lower Anogenital Squamous Terminology Standardization project for HPV-associated lesions: background and consensus recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. Int J Gynecol Pathol. 2013;32:76–115. doi: 10.1097/PGP.0b013e31826916c7. [DOI] [PubMed] [Google Scholar]
- 114.Furukawa T, Chiba R, Kobari M, et al. Varying grades of epithelial atypia in the pancreatic ducts of humans. Classification based on morphometry and multivariate analysis and correlated with positive reactions of carcinoembryonic antigen. Arch Pathol Lab Med. 1994;118:227–234. [PubMed] [Google Scholar]