Introduction
In 1769, Giovanni Battista Morgagni, an Italian anatomist described an anterior retrosternal diaphragmatic defect that occurs between the xiphoid process of the sternum and the costochondral attachments of the diaphragm. It results from failure of muscle tissues to spread over the area during embryologic development and constitutes less than 2% of reported diaphragmatic defects.1 Since the space is covered by pericardium on the left, abdominal contents more commonly herniate through the defect on the right side.2 We describe one such rare case of Morgagni hernia occurring on the left side in a 28 year old male patient who was initially managed as a case of pulmonary tuberculosis.
Case report
A 28 year old male patient, non-smoker with no known co-morbidities, presented with history of progressively worsening breathlessness after physical exertion, associated with a dry, unproductive cough for approximately two years. The onset of both symptoms was insidious and they used to subside after taking rest. There was no history of weight loss, fever, night sweats, chest pain or aggravation of symptoms after meals. There was no past history of abdominal/thoracic trauma. The patient had earlier been evaluated at a private hospital where he was diagnosed as a case of pulmonary tuberculosis and was taking anti tubercular treatment (ATT) for one year, without any relief of symptoms and hence he reported to us.
On general examination he had a weight of 55 Kilograms and there was no pallor, icterus, cyanosis, pedal edema or peripheral lymphadenopathy. Vital parameters were within normal limits. Examination of chest revealed reduced air entry in the left infra-scapular region. There were, however no adventitious sounds. The rest of physical and systemic examination was unremarkable. Radiograph of the chest showed bowel loops in the left lower lung field with mediastinal shift to the right. (Fig. 1). Contrast enhanced Computed Tomography (CECT) scan of thorax and upper abdomen was suggestive of a diaphragmatic hernia (Morgagni type) on the left side, with the defect measuring 8.3 × 2.5 cm present in left hemi-diaphragm antero-medially, and herniation of bowel along with its mesentery and fat in the left hemithorax (Fig. 2, Fig. 3). Endoscopy showed gastro-esophageal (GE) junction at 41 cm with no features suggestive of esophagitis or presence of a paraesophageal hernia. Other routine hematological and biochemical investigations were normal. Serology for HIV and tuberculosis was non-reactive. UItrasonography of abdomen was normal. Pulmonary function tests showed mild reduction in FEV1 and FVC. The patient was started on incentive spirometry and chest physiotherapy and taken up for surgery under GA after placement of a double lumen endo-tracheal tube. Access to the thorax was gained via a standard left posterolateral thoracotomy. The left lung was collapsed, with single lung ventilation, to facilitate surgery. A large Morgagni hernia with an intact sac was found (Fig.4). The sac was dissected out and opened. It contained omentum and portions of large bowel and stomach (Fig.5). These were carefully separated out and returned back into the abdomen. The redundant portion of the sac was excised and the defect was closed with interrupted sutures using 2/0 polypropylene. The repair was then reinforced by placing a 15 × 15 cm polypropylene mesh over it (Fig.6). The lung was re-expanded and chest closed after placing an intercostal tube drain. The patient had an uneventful post operative recovery and was discharged from hospital on the fifth post operative day. He is presently asymptomatic, after 18 months of follow up, the chest radiograph shows satisfactory post operative appearance (Fig.7).
Fig. 1.

Radiograph of the chest showing bowel loops in the left lower lung field with mediastinal shift to the right. The left hemidiaphragmatic outline is indistinct.
Fig. 2.

CT topogram of the thorax demonstrating a soft tissue mass in the left hemithorax in para-cardiac region with bowel loops.
Fig. 3.

Contrast enhanced coronal reformatted image of the thorax and upper abdomen demonstrating the hernia.
Fig. 4.
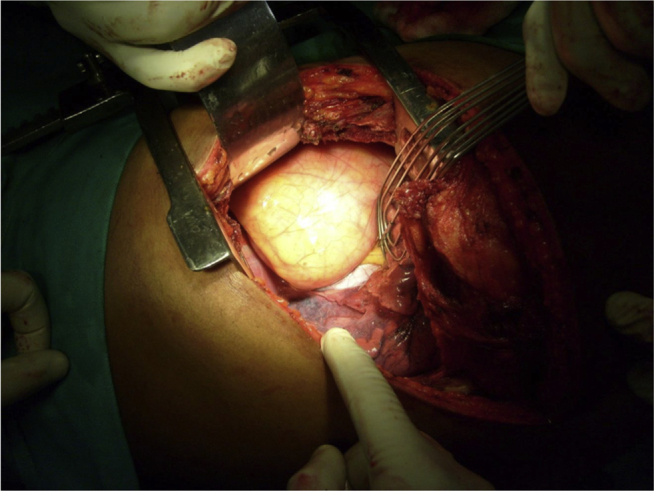
Intra-operative appearance of the hernia sac.
Fig. 5.

Hernia sac opened and contents displayed.
Fig. 6.

Completed repair.
Fig. 7.

Chest radiograph 18 months after surgery.
Discussion
A hernia of Morgagni is a rare entity and usually occurs on the right side. Although it is congenital, it is most often discovered in adults, with men presenting earlier in life than women.3 Pulmonary symptoms are the commonest presenting feature followed by abdominal discomfort3, 4, 5 but often it is an incidental finding discovered on a chest radiograph done for some other condition.2 A high incidence of associated anomalies, commonly congenital heart disease and Down syndrome has also been reported.4 Its occurrence on the left side, as was seen in our patient, is extremely uncommon.5
The presence of this condition can usually be suspected on a plain chest radiograph and subsequently confirmed by other imaging modalities such as upper gastro-intestinal contrast series, CT and MRI. In our patient, the radiographic findings were erroneously interpreted as pulmonary tuberculosis and the patient was administered ATT for one year before the underlying condition was correctly diagnosed. A CT scan is very useful to image the defect and to evaluate the extent of abdominal visceral herniation.1
The treatment of a Morgagni hernia is surgical and is advisable at initial diagnosis, even in the absence of symptoms.2 The two main surgical approaches that have been described are trans-abdominal (open or laparoscopic) and trans-thoracic (open or thoracoscopic). Thoracotomy is the most widely used surgical approach; however, laparoscopic repair has gained popularity since its first report in 1992.3 A trans-thoracic repair allows better and safer control during thoracic dissection6 and is especially appropriate when the contents of the hernia are fixed in position at or above the level of the carina. Reduction of these structures can be difficult using the abdominal approach because of dense adhesions and hence a trans-thoracic approach is preferable.2 It facilitates easy dissection of the adhesions between the sac and surrounding structures and safe reduction of the contents of the sac back into the peritoneal cavity. The defect in the diaphragm can then be carefully evaluated and repaired. It is for these reasons that the authors chose to perform the surgery through the trans-thoracic approach.
There are multiple ways of dealing with the defect. Small defects that are surrounded by a rim of muscle may be repaired primarily with heavy non-absorbable interrupted mattress sutures. A defect with an incomplete muscular rim is repaired by attaching the free edge of the muscle to the costal margin. Defects that are too large to close primarily should be closed with a non-absorbable mesh interposed between the muscular rim and the chest wall.2 In our case we initially closed the defect primarily with interrupted horizontal mattress sutures of 2/0 polypropylene and thereafter buttressed the suture line with a polypropylene mesh.
Laparoscopic repair of Morgagni hernias has been described, especially in the pediatric age group, and it offers the advantages of minimally invasive surgery to the patient.4, 7 When compared to the open repair, the laparoscopic-assisted approach is associated with a shorter operative time, an earlier commencement of feeds, less requirement for post operative analgesia, a shorter hospital stay, and better cosmetic appearance.4 It however, needs to be performed properly using a prosthetic patch and a recent study has reported that there is a high rate of recurrence after laparoscopic Morgagni hernia repair without patch.8 A transxiphoid hand-assisted video-thoracoscopic approach has also been described.6 These minimally invasive approaches are yet to become popular and a comparative analysis of diaphragmatic hernia repair outcomes using the nationwide inpatient sample database demonstrated that most diaphragmatic hernia repairs are performed through open abdominal and thoracic approaches.9 A combined transthoracic and transabdominal approach may sometimes be required in a very large hernia.10
In summary, a Morgagni hernia occurring on the left side is rare and requires a high index of suspicion for diagnosis. Surgical repair at an early date is the treatment of choice. Laparoscopic repair is gaining popularity and is especially useful in the pediatric age group.
Conflicts of interest
All authors have none to declare.
References
- 1.Nasr A., Fecteau A. Foramen of Morgagni hernia: presentation and treatment. Thorac Surg Clin. 2009;19(4):463–468. doi: 10.1016/j.thorsurg.2009.08.010. [review] [DOI] [PubMed] [Google Scholar]
- 2.Maish M.S. The diaphragm. Surg Clin N Am. 2010;90:955–968. doi: 10.1016/j.suc.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Horton J.D., Hofmann L.J., Hetz S.P. Presentation and management of Morgagni hernias in adults: a review of 298 cases. Surg Endosc. 2008;22:1413–1420. doi: 10.1007/s00464-008-9754-x. [DOI] [PubMed] [Google Scholar]
- 4.Al-Salem A.H., Zamakhshary M., Al Mohaidly M., Al-Qahtani A., Abdulla M.R., Naga M.I. Congenital Morgagni's hernia: a national multicenter study. J Pediatr Surg. 2014;49:503–507. doi: 10.1016/j.jpedsurg.2013.08.029. [DOI] [PubMed] [Google Scholar]
- 5.Sirmali M., Turut H., Gezer S. Clinical and radiologic evaluation of foramen of Morgagni hernias and the transthoracic approach. World J Surg. 2005;29:1520–1524. doi: 10.1007/s00268-005-0055-4. [DOI] [PubMed] [Google Scholar]
- 6.Ambrogi V., Forcella D., Gatti A., Vanni G., Mineo T.C. Transthoracic repair of Morgagni's hernia: a 20-year experience from open to video-assisted approach. Surg Endosc. 2007;21:587–591. doi: 10.1007/s00464-006-9017-7. [DOI] [PubMed] [Google Scholar]
- 7.Laituri C.A., Garey C.L., Ostlie D.J., Holcomb G.W., St Peter S.D. Morgagni hernia repair in children: comparison of laparoscopic and open results. J Laparoendosc Adv Surg Tech A. 2011;21:89–91. doi: 10.1089/lap.2010.0174. [DOI] [PubMed] [Google Scholar]
- 8.Garriboli M., Bishay M., Kiely E.M. Recurrence rate of Morgagni diaphragmatic hernia following laparoscopic repair. Pediatr Surg Int. 2013;29:185–189. doi: 10.1007/s00383-012-3199-y. [DOI] [PubMed] [Google Scholar]
- 9.Paul S., Nasar A., Port J.L. Comparative analysis of diaphragmatic hernia repair outcomes using the nationwide inpatient sample database. Arch Surg. 2012;147:607–612. doi: 10.1001/archsurg.2012.127. [DOI] [PubMed] [Google Scholar]
- 10.Marinceu D., Loubani M., O'Grady H. Late presentation of a large Morgagni hernia in an adult. BMJ Case Rep. 2014 Jan 15:2014. doi: 10.1136/bcr-2013-202440. pii: bcr2013202440. [DOI] [PMC free article] [PubMed] [Google Scholar]


