Abstract
Background:
Increases in intracranial pressure (ICP) require a rapid recognition to allow for adequate treatments. The aim of this study was to determine whether transocular Doppler and optic nerve sheath diameter (ONSD) monitoring could reliably identify increases in ICP.
Materials and Methods:
This is a cross-sectional case-control study, which was carried out on 2013. Subjects were chosen from patients who admitted to the neurology and neurosurgery departments and the intensive care unit of Alzahra Hospital (Isfahan, Iran). To measure the ICP, the authors used ultrasound to measure the diameter of the optic nerve sheath and transocular Doppler (TOD) to measure blood flew velocity in ophthalmic artery (OA) and ophthalmic vein (OV) in both groups.
Results:
The mean of ONSD was 4.8 mm (SD 0.77) in patients with raised ICP and 3.2 mm (SD 0.3) in healthy volunteers which was significant (P < 0.001). The mean (SD) of TOD parameters were also significantly more in OA and OV of patients with raised ICP.
Conclusion:
Ultrasound methods has been proposed as an alternative safe technique for invasive ICP measuring methods.
Keywords: Intracranial pressure, optic nerve sheath diameter, transocular Doppler, ultrasound
INTRODUCTION
Raised intracranial pressure (ICP) is a common life-threatening condition that can occur in multiple neurological or non-neurological settings and requires rapid diagnosis and therapeutic intervention.[1] Clinical signs of raised ICP are not specific and often difficult to interpret, though direct measurement of ICP using an intraventricular catheter has been known to be a gold standard method for evaluating ICP; but it is a highly invasive technique that may not be feasible in many clinical settings due to the severe complications associated with its use, such as hemorrhage, infection and malfunction; absence of available neurosurgical expertise; and contraindications (coagulopathy, thrombocythemia).[2,3,4] Several noninvasive techniques for the evaluation of ICP have been developed and include Fundoscopy and Papilledema, computed tomography (CT) scan, Magnetic resonance imaging (MRI), tympanic membrane displacement (TMD), and transcranial doppler sonography (TCD).[5] However, the accuracy of these methods in predicting ICP values appears to be limited.[5,6,7,8,9]
Recently, clinical studies have suggested that ultrasonographic measurements of the Optic Nerve Sheath Diameter (ONSD) correlate with signs of raised ICP.[10,11] The optic nerve is part of the central nervous system, and therefore surrounded by the dural sheath. Between the sheath and the white matter is a small (0.1–0.2 mm) subarachnoid space, which communicates with the subarachnoid space surrounding the brain. In the cases of increased ICP, the sheath expands and changes in the diameter of the nerve sheath can be visualized using transocular ultrasound.[5,12,13] Abnormal ONSD is usually present when ICP raises above 20 mmHg.[14] Three millimeters behind the ocular globe, the optic nerve is only surrounded by fat and the dural sheath is distensible within its fatty environment, particularly in case of raised pressure in the cerebrospinal fluid.[15] In vitro studies suggest that the retrobulbar optic nerve sheath, may undergo sonographically detectable distension seconds after the development of intracranial hypertension.[15,16] The technique is safe, cheap and efficient.[17] Previous clinical studies have confirmed the accuracy of ONSD measurement at detecting raised ICP in several clinical situations: Traumatic brain injury, hydrocephalus, and intracranial hemorrhage.[10,18,19,20] Two recent meta-analyses suggest that ONSD may be a reliable noninvasive surrogate marker of raised ICP.[11,21] But a recent review article concluded that this technique is not accurate enough to be used instead of invasive ICP measuring methods. They suggested that It can potentially be used as a screening method for detecting raised ICP when invasive ICP monitoring capabilities are not available.[5]
In the other hand, hemodynamic measurements can bean accurate and reliable noninvasive method to measure ICP. This technique applies color Doppler imaging to measure the blood flow velocity indifferent intracranial vessels such as middle cerebral artery (MCA); and intracranial part of the internal carotid artery and jugular vein.[5,22,23,24,25] But these technique cannot be used on 10–15% of the patients due to the ultrasound not being able to penetrate the skull (the so-called bone window).[26] However, the arteries that perfuse and the vein that drains the orbit are exposed to the ambient ICP while coursing through the cerebrospinal fluid or optic nerve.[22,27] So transocular color Doppler imaging can be applied to measure the blood flow velocity in vessels such as ophthalmic artery (OA) and ophthalmic vein (OV). The OA is being used as a natural pair of scales, in which the intracranial segment of the OA is compressed by ICP and the extracranial segment of the OA is compressed by extracranial pressure (Pe) applied to the orbit. The blood flow parameters in both OA segments are approximately the same in the scales balance case when Pe = ICP.[28]
The aim of this study was to investigate a possible relationship between, ONSD ortransocular Doppler (TOD) ultrasonography parameters, and ICP changes in patients with raised ICP and healthy population.
MATERIALS AND METHODS
Study design and participants
This is a cross-sectional case-control study, which was carried out on 2013. The study followed the Declaration of Helsinki on Biomedical Research Involving Human Subjects and was approved by the Ethics Committee from the Isfahan University of Medical Sciences (N = 392067). All participants provided written informed consent.
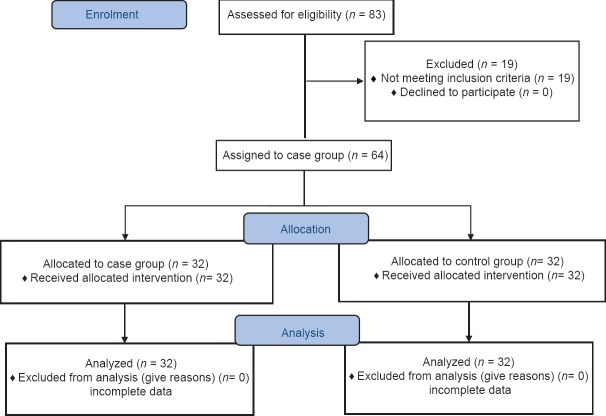
Subjects were chosen from patients who admitted to the neurology and neurosurgery departments and the intensive care unit of Alzahra Hospital (Isfahan, Iran). All subjects met the following inclusion criteria: (1) ≥18 years aged; (2) presence of clinical symptoms and signs of raised ICP, including nausea, vomiting, and symptoms of brain herniation such as secondary midbrain syndrome and papilledema on ophthalmoscopy; and confirmed by lumbar puncture (LP) by a neurologist;[29,30] (3) written or oral informed consent of patient or family. Subjects also met none of the following exclusion criteria: (1) history of glaucoma; (2) known disease of the optic nerve (optic neuritis, meningioma, and gliomas); (3) known orbital injury or prior ocular surgery. A total of 83 individuals screened which 32 met all inclusion and no exclusion criteria for case group and 32 subjects were chosen as control group [Figure 1]. The control group included age- and sex-matched healthy volunteers.
Figure 1.
Study design flow chart
Procedures and variables assessment
To measure the ICP, the authors used a transocular 7.5-MHz linear ultrasound probe to measure the diameter of the optic nerve sheath three mm behind the globe in both groups.[15]
We also used TOD to measure blood flew velocity in OA and OV in both groups. TOD parameters included peak systolic velocities (PSV), mead systolic velocity (MD), plasticity index (PI) [peak systolic-end diastolic velocities/mean flow velocity], and resistance index (RI).[5]
Statistical analysis
Data were analyzed by SPSS version 20.0 (SPSS Inc, Chicago, Illinois, USA). A P < 0.05 was considered significant. Continuous variables were expressed as mean ± SD. ANOVA and Pierson correlation were used for analysis.
RESULTS
The mean age of participants was 58.8 years, range from 41 to 78. The demographic features of the sample are reported in Table 1.
Table 1.
Demographic data of the 64 participants
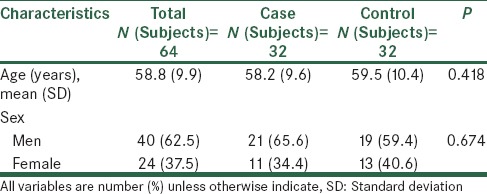
There were no statistically significant differences on demographic data between two groups.
We assessed ONSD in both eyes in each group. The ONSD range was 3.2to 6.3 mm with a mean of 4.8(SD 0.77) in patients with raised ICP and 2.6 to 4.1 mm with a mean of 3.2(SD 0.3) in healthy volunteers. The difference between groups was significant (P < 0.001).
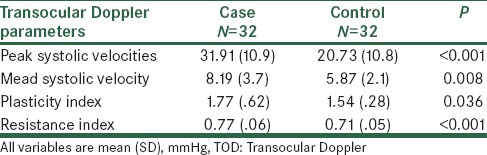
TOD ultrasound was used in OA and OV, in both eyes in each group. TOD parameters included PSV, MD, PI, and RI.
In OA, mean (SD) of PS, MD, PI and RI were significantly more inpatients with raised ICP. TOD parameters in OA are reported in Table 2.
Table 2.
Comparison of TOD parametersbetween two groups in ophthalmic artery
In OV mean velocity was 6.7 (SD 3.27) mm Hg in patients with raised ICP and 4.7 (SD 1.51) mm Hg in healthy volunteers. The difference between groups was significant (P = 0.005).
DISCUSSION
ICP monitoring techniques are multiple and diverse. Nevertheless, before choosing the technique to apply in critical care, several factors need to be considered; the precision of measurements made, the cost of the device as well as the possible complications and mechanical problems associated with the individual techniques. In this study we compared patients with raised ICP, and healthy volunteers for ONSD and TOD parameters in ultrasound.
The use of ONSD measurement for the detection of raised ICP has generated considerable interest, and several studies suggesting a good correlation with the gold standard of invasive ICP monitoring.[10,11,18,19,20] Our study showed that average of ONSD in patients with raised ICP is more than healthy volunteers significantly. The average ONSD was 4.8 mm in the patients with raised ICP.
A position three mm behind the globe was chosen because the ultrasound contrast is greatest, the results are more reproducible, and anatomically the anterior nerve is most distensible.[15,31]
This is consistent with Qayyum et al., Cammarata et al., and Amini et al., which concluded that ocular ultrasound may be considered as a good alternative for invasive methods to identify increased ICP.[10,18,19]
Against this Beare et al. showed that raised ICP is less commonly detected by ONSD measurement than LP in children with cerebral malaria.[32] And Strumwasser et al. concluded that ONSD measurement for elevated ICP is not reliable due to poor accuracy and correlation.[33]
The average ONSD in the patients in our study (4.8 mm) was consistent with previous studies which showed that the cut off value of 4.8 mm or more for ONSD is of sufficient sensitivity 96% (95% CI 91-99%) and specificity 94% (92–96%) for predicting elevated ICP.[34]
In our study, all of TOD parameters (PS, MD, PI, and RI) were significantly more in case group. This result shows that TOD ultrasound can measure ICP as a noninvasive method.
In previous studies, Gura et al. concluded that Independent of the type of intracranial pathology, there is a strong correlation between PI intranscranial Doppler ultrasonography (TCD) and invasive ICP measurements.[35] Also Ragauskas et al. showed that Doppler ultrasound of OA is precise and accurate compared with gold standard CSF pressure measured via lumbar puncture.[28]
In against with this, Brandi et al. showed that PI-calculated ICP is too uncertain,[25] and Zweifel et al. concluded that the value of TCD-PI to assess ICP is very limited. However, extreme values of PI can still potentially be used in support of a decision for invasive ICP monitoring.[36]
CONCLUSION
In conclusion, as ICP monitoring is invasive and has disadvantages of infection, hemorrhage, malfunction, obstruction or malposition, thus, this ultrasound methods has been proposed as an alternative safe technique because of advantages of being rapid, non-invasive, having no radiation exposure and being accessible at the bedside without moving critically ill patients. It can therefore be easily repeated to re-evaluate a patient. But this methods also requires basic ultrasonography skills, training, and experience.
ACKNOWLEDGMENT
We would like to express thanks for staffs of radiology ward of Alzahra Hospital (Isfahan, Iran).
Footnotes
Source of Support: This study is funded by Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Tayal VS, Neulander M, Norton HJ, Foster T, Saunders T, Blaivas M. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med. 2007;49:508–14. doi: 10.1016/j.annemergmed.2006.06.040. [DOI] [PubMed] [Google Scholar]
- 2.Czosnyka M, Pickard JD. Monitoring and interpretation of intracranial pressure. J Neurol Neurosurg Psychiatry. 2004;75:813–21. doi: 10.1136/jnnp.2003.033126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsung JW, Blaivas M, Cooper A, Levick NR. A rapid noninvasive method of detecting elevated intracranial pressure using bedside ocular ultrasound: Application to 3 cases of head trauma in the pediatric emergency department. Pediatr Emerg Care. 2005;21:94–8. doi: 10.1097/01.pec.0000159052.64930.64. [DOI] [PubMed] [Google Scholar]
- 4.Rickert K, Sinson G. Intracranial pressure monitoring. Oper Tech Gen Surg. 2003;5:170–5. [Google Scholar]
- 5.Raboel PH, Bartek J, Jr, Andresen M, Bellander BM, Romner B. Intracranial pressure monitoring: Invasive versus non-invasive methods- A review. Crit Care Res Pract 2012. 2012 doi: 10.1155/2012/950393. 950393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winkler F, Kastenbauer S, Yousry TA, Maerz U, Pfister HW. Discrepancies between brain CT imaging and severely raised intracranial pressure proven by ventriculostomy in adults with pneumococcal meningitis. J Neurol. 2002;249:1292–7. doi: 10.1007/s00415-002-0844-8. [DOI] [PubMed] [Google Scholar]
- 7.Hiler M, Czosnyka M, Hutchinson P, Balestreri M, Smielewski P, Matta B, et al. Predictive value of initial computerized tomography scan, intracranial pressure, and state of autoregulation in patients with traumatic brain injury. J Neurosurg. 2006;104:731–7. doi: 10.3171/jns.2006.104.5.731. [DOI] [PubMed] [Google Scholar]
- 8.Hassler W, Steinmetz H, Gawlowski J. Transcranial Doppler ultrasonography in raised intracranial pressure and in intracranial circulatory arrest. J Neurosurg. 1988;68:745–51. [PubMed] [Google Scholar]
- 9.Schmidt B, Czosnyka M, Raabe A, Yahya H, Schwarze JJ, Sackerer D, et al. Adaptive noninvasive assessment of intracranial pressure and cerebral autoregulation. Stroke. 2003;34:84–9. doi: 10.1161/01.str.0000047849.01376.ae. [DOI] [PubMed] [Google Scholar]
- 10.Qayyum H, Ramlakhan S. Can ocular ultrasound predict intracranial hypertension? A pilot diagnostic accuracy evaluation in a UK emergency department. Eur J Emerg Med. 2013;20:91–7. doi: 10.1097/MEJ.0b013e32835105c8. [DOI] [PubMed] [Google Scholar]
- 11.Moretti R, Pizzi B. Ultrasonography of the optic nerve in neurocritically ill patients. Acta Anaesthe siol Scand. 2011;55:644–52. doi: 10.1111/j.1399-6576.2011.02432.x. [DOI] [PubMed] [Google Scholar]
- 12.Karakitsos D, Soldatos T, Gouliamos A, Armaganidis A, Poularas J, Kalogeromitros A, et al. Transorbital sonographic monitoring of optic nerve diameter in patients with severe brain injury. Transplant Proc. 2006;38:3700–6. doi: 10.1016/j.transproceed.2006.10.185. [DOI] [PubMed] [Google Scholar]
- 13.Girisgin AS, Kalkan E, Kocak S, Cander B, Gul M, Semiz M. The role of optic nerve ultrasonography in the diagnosis of elevated intracranial pressure. Emerg Med J. 2007;24:251–4. doi: 10.1136/emj.2006.040931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bäuerle J, Lochner P, Kaps M, Nedelmann M. Intra- and interobsever reliability of sonographic assessment of the optic nerve sheath diameter in healthy adults. J Neuroimaging. 2010;22:42–5. doi: 10.1111/j.1552-6569.2010.00546.x. [DOI] [PubMed] [Google Scholar]
- 15.Dubost C, Le Gouez A, Jouffroy V, Roger-Christoph S, Benhamou D, Mercier FJ, et al. Optic nerves heath diameter used as ultrasonographic assessment of the incidence of raised intracranial pressure in preeclampsia: A pilot study. Anesthesiology. 2012;116:1066–71. doi: 10.1097/ALN.0b013e318246ea1a. [DOI] [PubMed] [Google Scholar]
- 16.Helmke K, Hansen HC. Fundamentals of transorbital so no graphic evaluation of optic nerve sheath expansion under intracranial hypertension. I. Experimental study. Pediatr Radiol. 1996;26:701–5. doi: 10.1007/BF01383383. [DOI] [PubMed] [Google Scholar]
- 17.Kimberly HH, Shah S, Marill K, Noble V. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad Emerg Med. 2008;15:201–4. doi: 10.1111/j.1553-2712.2007.00031.x. [DOI] [PubMed] [Google Scholar]
- 18.Cammarata G, Ristagno G, Cammarata A, Mannanici G, Denaro C, Gullo A. Ocular ultrasound to detect intracranial hypertension in trauma patients. J Trauma. 2011;71:779–81. doi: 10.1097/TA.0b013e3182220673. [DOI] [PubMed] [Google Scholar]
- 19.Amini A, Kariman H, ArhamiDolatabadi A, Hatamabadi HR, Derakhshanfar H, Mansouri B, et al. Use of the sonographic diameter of optic nerve sheath to estimate intracranial pressure. Am J Emerg Med. 2013;31:236–9. doi: 10.1016/j.ajem.2012.06.025. [DOI] [PubMed] [Google Scholar]
- 20.Rosenberg JB, Shiloh AL, Savel RH, Eisen LA. Non-invasive methods of estimating intracranial pressure. Neurocrit Care. 2011;15:599–608. doi: 10.1007/s12028-011-9545-4. [DOI] [PubMed] [Google Scholar]
- 21.Dubourg J, Javouhey E, Geeraerts T, Messerer M, Kassai B. Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: A systematic review and meta-analysis. Intensive Care Med. 2011;37:1059–68. doi: 10.1007/s00134-011-2224-2. [DOI] [PubMed] [Google Scholar]
- 22.Querfurth HW, Arms SW, Lichy CM, Irwin WT, Steiner T. Prediction of intracranial pressure from noninvasive transocular venous and arterial hemodynamic measurements: A pilot study. Neurocrit Care. 2004;1:183–94. doi: 10.1385/NCC:1:2:183. [DOI] [PubMed] [Google Scholar]
- 23.Voulgaris SG, Partheni M, Kaliora H, Haftouras N, Pessach IS, Polyzoidis KS. Early cerebral monitoring using the transcranial Doppler pulsatility index in patients with severe brain trauma. Med Sci Monit. 2005;11:CR49–52. [PubMed] [Google Scholar]
- 24.Sidi A, Messinger G, Mahla ME. Transcranial Doppler monitoring compared with invasive monitoring of intracranial pressure during acute intracranial hypertension. J Clin Monit Comput. 1999;15:185–95. doi: 10.1023/a:1009993232534. [DOI] [PubMed] [Google Scholar]
- 25.Brandi G, Béchir M, Sailer S, Haberthür C, Stocker R, Stover JF. Transcranial color-coded duplex sonography allows to assess cerebral perfusion pressure noninvasively following severe traumatic brain injury. Acta Neurochir (Wien) 2010;152:965–72. doi: 10.1007/s00701-010-0643-4. [DOI] [PubMed] [Google Scholar]
- 26.Tsivgoulis G, Alexandrov AV, Sloan MA. Advances in transcranial Doppler ultrasonography. Curr Neurol Neurosci Rep. 2009;9:46–54. doi: 10.1007/s11910-009-0008-7. [DOI] [PubMed] [Google Scholar]
- 27.Firsching R, Schütze M, Motschmann M, Behrens-Baumann W. Venous opthalmodynamometry: A noninvasive method for assessment of intracranial pressure. J Neurosurg. 2000;93:33–6. doi: 10.3171/jns.2000.93.1.0033. [DOI] [PubMed] [Google Scholar]
- 28.Ragauskas A, Matijosaitis V, Zakelis R, Petrikonis K, Rastenyte D, Piper I, et al. Clinical assessment of noninvasive intracranial pressure absolute value measurement method. Neurology. 2012;78:1684–91. doi: 10.1212/WNL.0b013e3182574f50. [DOI] [PubMed] [Google Scholar]
- 29.Malayeri AA, Bavarian S, Mehdizadeh M. Sonographicevaluation of optic nerve diameter in children with raised intracranial pressure. J Ultrasound Med. 2005;24:143–7. doi: 10.7863/jum.2005.24.2.143. [DOI] [PubMed] [Google Scholar]
- 30.Kapadia FN, Jha AN. Simultaneous lumbar and intraventricular manometry to evaluate the role and safety of lumbar puncture in raised intracranial pressure following subarachnoid haemorrhage. Br J Neurosurg. 1996;10:585–7. doi: 10.1080/02688699646907. [DOI] [PubMed] [Google Scholar]
- 31.Soldatos T, Chatzimichail K, Papathanasiou M, Gouliamos A. Optic nerve sonography: A new window for the non-invasive evaluation of intracranial pressure in brain injury. Emerg Med J. 2009;26:630–4. doi: 10.1136/emj.2008.058453. [DOI] [PubMed] [Google Scholar]
- 32.Beare NA, Glover SJ, Lewallen S, Taylor TE, Harding SP, Molyneux ME. Prevalence of raised intracranial pressure in cerebral malaria detected by optic nerve sheath ultrasound. Am J Trop Med Hyg. 2012;87:985–8. doi: 10.4269/ajtmh.2012.11-0459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Strumwasser A, Kwan RO, Yeung L, Miraflor E, Ereso A, Castro-Moure F, et al. Sonographic optic nerve sheath diameter as an estimate of intracranial pressure in adult trauma. J Surg Res. 2011;170:265–71. doi: 10.1016/j.jss.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 34.Rajajee V, Vanaman M, Fletcher JJ, Jacobs TL. Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocrit Care. 2011;15:506–15. doi: 10.1007/s12028-011-9606-8. [DOI] [PubMed] [Google Scholar]
- 35.Gura M, Silav G, Isik N, Elmaci I. Noninvasive estimation of cerebral perfusion pressure with transcranial Doppler ultrasonography in traumatic brain injury. Turk Neurosurg. 2012;22:411–5. doi: 10.5137/1019-5149.JTN.4201-11.1. [DOI] [PubMed] [Google Scholar]
- 36.Zweifel C, Czosnyka M, Carrera E, de Riva N, Pickard JD, Smielewski P. Reliability of the blood flow velocity pulsatility index for assessment of intracranial and cerebral perfusion pressures in head-injured patients. Neurosurgery. 2012;71:853–61. doi: 10.1227/NEU.0b013e3182675b42. [DOI] [PubMed] [Google Scholar]