Abstract
Depression and severe psychological distress are frequently comorbid with diabetes and are associated with reduced adherence to medication and healthy lifestyle regimens, poorer glycemic control, and increased complications. The mixed success of existing treatments for depression in diabetes patients suggests a need for supplementary approaches to this common problem. This article reviews recent evidence for the benefits of self-compassion in chronically ill patients, suggesting its utility as a clinical tool for improving self-care, depression, and glycemic control in diabetes. Possible physical and psychological pathways by which self-compassion may promote better outcomes in diabetes patients are considered, with particular attention given to reductions in negative self-judgment and improved motivation to undertake self-care.
Diabetes can be described as a tidal wave about to crash on health systems around the world, with global prevalence of the disease estimated at 9% among adults (1). Living with diabetes is challenging, demanding a relentless effort to achieve glycemic control through strict behavioral self-regulation and adherence to medical regimens. Making self-management more complex, serious psychological difficulties are frequently present among diabetes patients, accompanied by increased suffering and compromised quality of life (2). Building on evidence linking positive aspects of psychological adjustment to improved coping in physically ill populations, this article describes how research into self-compassion may offer a supplementary framework for the improved management of diabetes, providing some protection against depression and its downstream effects.
Depression in Diabetes: The Status Quo
The prevalence of depression in diabetes is well documented, with a raft of research over the past two decades focusing on links between the two conditions. People with diabetes are between 1.4 and 3 times more likely to develop depression compared to the general population (3), with depression affecting 15–20% of diabetes patients overall (4). When subclinical depression is included, prevalence estimates are greater, with at least two-thirds of a large sample of type 2 diabetes patients experiencing depressive symptoms (5).
Comorbid depression in diabetes patients is associated with poorer metabolic control, an outcome that predicts hyperglycemia and an increased risk of diabetes-related complications and mortality (6). These complications are, in turn, thought to be at least partly mediated by depression’s association with poor adherence to medication and lifestyle recommendations, both of which predict reduced quality of life and increased health care costs (7).
If anything, these figures likely underestimate both the prevalence of affective disturbances in diabetes and the associated costs of disease management, suggesting that the problem of depression may be far larger than is currently accepted. Commensurately, the negative effects of these conditions on crucial self-care regimens—and the resulting consequences in terms of increased disability, health care utilization, and mortality—also may be far more widespread.
Current Treatment Approaches
Given the scale of the problem of depression in diabetes, evidence to support the effectiveness of current antidepressant therapies is surprisingly sparse, and overall outcomes are still unclear. A recent systematic review and meta-analysis (8), including 14 randomized, controlled trials (RCTs) evaluating psychotherapy, pharmacotherapy, and collaborative care in 1,724 diabetes patients with comorbid depression, showed moderate effects for treatment overall. It should be noted, however, that four of the five RCTs (n = 310) involving a psychotherapeutic intervention such as cognitive behavioral therapy (CBT) also included other supportive treatment such as diabetes education alongside the psychotherapy, making it difficult to assess the merits of the psychological intervention in isolation. Additionally, most studies were small (10 investigated samples ranging from 13 to 60 participants) and mainly involved type 2 diabetes patients, meaning results may not be generalizable to insulin-dependent type 1 diabetes patients.
Furthermore, although depression in diabetes patients is linked to glycemic indices, it is not yet clear if successfully treating low mood is associated with improved metabolic control. One review (7) found that improvements in depression were linked to improvements in glycemic control and overall perceptions of well-being. Contradicting these findings, however, are results of a meta-analysis (11 studies in adults and 10 studies in children and adolescents) showing that, although both CBT and antidepressant medications were associated with an improvement in blood glucose readings in some studies, overall, there was no significant effect of either of these treatments on glycemic control in adults and only weak evidence of an effect in children and adolescents (9).
Successfully treating depression in diabetes is further complicated by the difficulty of detecting the presence of low mood, with evidence that only a small fraction of depressed patients receive any form of treatment, likely because of an overlap between symptoms of both conditions, such as pain and fatigue (7,10,11). Furthermore, patients with diabetes may find depression difficult to acknowledge because it represents another area for them to be dissatisfied with themselves, perhaps further evidence of personal failure beyond their daily struggle with self-management targets (12), and a focus, therefore, for continued negative self-judgment.
In summary, evidence for the treatment of depression in diabetes patients is limited, with existing studies suggesting modest effects in some groups, at best. Further investigation is essential in light of the devastating downstream effects of depression on glycemic control and overall quality of life. Emerging research into the construct of self-compassion, with its specific focus on reducing self-criticism and treating oneself kindly, suggests its potential utility for this population.
Self-Compassion: Does Kindness Matter?
Self-compassion is defined as the practice of treating oneself with kindness, care, and concern in the face of negative events (13,14). For diabetes patients, “negative events” may include receiving less-than-optimal blood glucose readings together with other self-management failures involving nonadherence to medication, diet, and exercise prescriptions (15). In this context, self-criticism, a common consequence of self-care failure among diabetes patients, can be seen as the opposite of self-compassion (16).
Neff (13) conceptualizes self-compassion as being composed of three components, all of which may be relevant to the experience of living with diabetes and managing its daily demands. First, self-kindness refers to the tendency to be caring and understanding of oneself rather than being harshly critical or judgmental. Second, common humanity recognizes that all humans are imperfect, fail, and make mistakes, framing difficulties and painful experiences in light of the shared human experience. Finally, mindfulness, the third component of self-compassion, involves being aware of the present-moment experience so that one neither ignores nor ruminates on disliked aspects of oneself or one’s behavior (17).
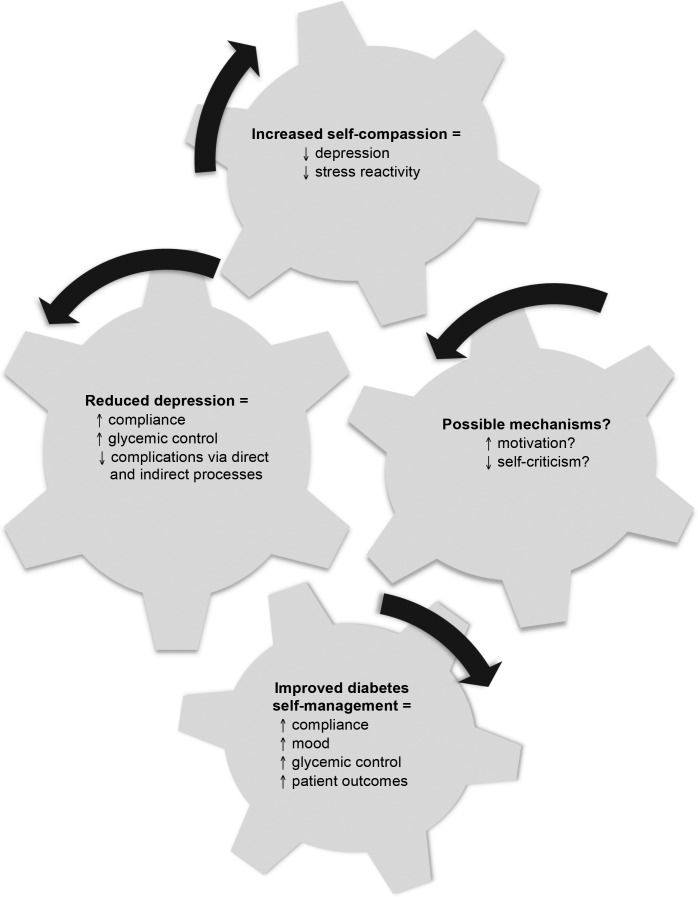
Taken together, developing these capacities may not only enable individuals to reflect concern and compassion toward others, but also may improve their capacity to direct this same concern and compassion toward themselves (13). In doing so, self-compassion may offer not only a gentler way of self-relating, but also one that may have the potential to reduce the depression and psychological suffering often associated with diabetes and its management. In the following section, the direct and indirect pathways by which both self-compassion and depression may relate to diabetes self-management are briefly reviewed, suggesting the utility of self-compassion for improving both mood and overall diabetes outcomes (Figure 1).
FIGURE 1.
Interlocking cogs illustrate the hypothesized processes linking self-compassion to improved outcomes in diabetes patients. Increasing self-compassion may reduce depression, leading to improved outcomes via mechanisms including increased motivation and reduced self-criticism.
Depression and Self-Compassion: Common Pathways?
Although the exact mechanisms by which depression is associated with markers of diabetes remain uncertain, there is evidence to suggest both direct (physiological) and indirect (behavioral) pathways. Interestingly, in terms of the current discussion, emerging evidence suggests that self-compassion may operate through similar processes.
Direct Pathways
Early studies indicate that depression may complicate, or possibly contribute to, the cause of diabetes due to direct, reciprocal effects on endocrine and other physiological processes. These effects include abnormalities of the hypothalamic-pituitary-adrenal axis, changes in sympathetic nervous system functioning as measured by decreased heart rate variability (HRV), and increased release of inflammatory cytokines (11,18,19). Support for a possible biological link between depression and diabetes was demonstrated in a recent meta-analysis (20) involving 24 studies that found patients with depression had significantly higher concentrations of tumor necrosis factor-α and interleukin-6 (IL-6) levels compared to nondepressed subjects. In turn, markers of inflammation such as IL-6 have been proposed to be involved in diabetes disease onset (21).
Interestingly, emerging evidence suggests that self-compassion might be linked to improved mood through similar or related metabolic and autonomic processes, including inflammatory and sympathetic nervous system responses to stress. Cross-sectional reports show that self-compassion is associated with lower blood plasma levels of IL-6 (22), as well as improved autonomic nervous system responding to stress (23), as measured by increased HRV (24). Such data are consistent with the theoretical proposition that self-compassion may calm the threat system, which is associated with defensiveness and autonomic arousal, and activate the self-soothing system (14).
A series of experimental studies suggests that quantifiable physiological and neurological processes underlie the experience of self-compassion. Klimecki et al. (25) used functional magnetic resonance imaging to demonstrate that the specific neuronal networks associated with love and affiliation were activated after the experimental stimulation of compassion. Participants also demonstrated an increase in positive affect; compared with a memory control, participants who reacted with negative affect when witnessing others in distress before compassion training subsequently showed increased positive affective experiences after training. Weng et al. (26) also found that compassion training increased both altruistic behavior and neural responses to suffering, including activation of the inferior parietal cortex and dorsolateral prefrontal cortex.
Taken together, these early fin-dings suggest that activation of attachment and affiliation circuitry through self-compassion may be linked to particular direct processes involving autonomic and metabolic pathways that may be common to both depression and diabetes.
Indirect Pathways
Although depression and self-compassion may be associated with processes directly linked to physical health, a number of cross-sectional and experimental studies in both patient and nonpatient populations suggest that compassion may alter psychological and behavioral processes leading to reductions in depressed affect and better self-regulation.
First, consistent evidence suggests that self-compassion is related to physical and psychological health as a result of reduced negative affect (17,27–29). For example, in a study in patients with obesity and pain problems (30), self-compassion predicted lower negative affect, higher positive affect, more adaptive pain coping, higher pain self-efficacy, and lower pain catastrophizing. Self-compassion also predicted more adaptive reactions to having HIV, including better adjustment and lower levels of stress, anxiety, and shame (31). Such studies suggest that more self-compassionate people may treat themselves more kindly, recognize that their problems are common aspects of human experience, and, as a consequence, be less ruminative and self-judgmental when confronting negative or difficult feelings (32,33).
On the other hand, the opposites of self-compassion, including self-criticism, self-hate, self-judgment, and negative perfectionism, have been linked to greater psychological distress, including depression (16). One recent study in chronically ill patients found that self-criticism predicted depression, illness-related stress, and diminished quality of life (34). Other nonpatient (college student) data likewise suggest a key role for self-criticism; self-reported physical symptoms increased as self-judgment increased and self-kindness decreased (35). Self-judgment may be particularly important to investigate in relation to diabetes patients given the daily demands of managing the illness and the difficulty in achieving “ideal” metabolic control, which seems a likely trigger for self-criticism (15).
A second indirect pathway by which self-compassion may improve physical health among diabetes patients is as a consequence of greater self-care (36). Evidence for this possibility can be seen in research, indicating that people reporting greater self-compassion may take greater responsibility for their problems and be less overwhelmed by difficulties, suggesting that they are more likely to take care of themselves when ill or injured (37). For diabetes patients, it may be that “taking care of oneself” includes seeking medical treatment, maintaining regular physical activity, maintaining appropriate dietary behavior, having regular foot checks, and self-monitoring blood glucose. This suggestion is consistent with data from a study with type 2 diabetes patients showing that depression predicted a decline in the self-care routines that protect against poor glucose control and the development of complications (12).
Provocatively, Egede and Osborn (12) suggest that the link between depression and poor self-care is mediated by a decline in the motivation to maintain self-care. A series of experimental studies in nonpatient groups (38) adds weight to this suggestion, showing that self-compassion leads to increased self-improvement motivations, possibly because it provides a nonjudgmental context in which to appraise one’s strengths and weaknesses and to strive to improve without the threat of unhelpful self-criticism. In the context of diabetes, enhancing self-compassion thus may enable patients to address evidence of less-than-ideal control without paralyzing self-criticism and help them reappraise and adjust their goals in support of good control.
The idea that self-compassionate individuals may be more motivated to take care of their health out of a desire to maximize well-being is also consistent with studies of several health behaviors that are directly related to outcomes among patients with diabetes. For example, interventions to maintain diet (39) and exercise (40) and to quit smoking (41) have demonstrated the positive influence of self-compassion on affect and behavior. Kelly et al. (41) found that smokers who were highly self-critical were helped to achieve their goals with an intervention that stimulated warmth and understanding while they attempted to quit. These authors suggest that for highly self-critical people in particular, self-compassion might inhibit a reflex toward rumination and self-judgment when faced with setbacks, helping them tolerate the distress they experience while trying to quit and enabling self-regulation via the soothing system rather than the threat system (14). A further intervention study (39) found that a self-compassion induction helped reduce negative self-evaluation, distress, and subsequent food consumption among highly restrictive eaters compared to dieters in a control condition. Participants in the self-compassion condition were able to hold eating goals in mind without ruminating or allowing negative evaluation to interfere with their eating goals. Alterations in self-management when confronting failures may be highly relevant to diabetes patients, who are generally required to monitor food intake as part of controlling blood glucose and can be assumed to experience setbacks as part of daily life. Finally, another study (40) found that self-compassion predicted superior exercise-related outcomes among women. Specifically, self-compassion was related to greater intrinsic motivation (behaviors initiated and regulated through choice as an expression of oneself) and lower external motivation (behaviors pressured by environmental forces) (42). In sum, these initial studies are encouraging in that they illuminate the potential utility of self-compassion–based interventions in improving some of the health behaviors that routinely challenge diabetes patients.
Finally, a theoretical model (43) suggests a third indirect pathway by which self-compassion may be linked to improved health as a consequence of broad improvements in motivational management and self-regulation (44). Successful self-regulation involves selecting goals, engaging in behaviors that support achievement of those goals, monitoring goal progress, and adjusting those goals when sufficient progress is not being made—all of which are highly relevant to diabetes self-care. It seems likely that more self-compassionate people may therefore attend to their own self-care out of a desire to treat themselves kindly and well by engaging in behaviors that support their ultimate good. They may, for example, set more specific, achievable, and appropriate goals related to diet, exercise, and blood glucose targets; prioritize attendance to these goals perhaps through regular medical appointments; adhere to regular medication and testing regimens; disengage from diet and exercise goals that are not working; and establish new behavioral targets associated with better control. Evidence of this can be seen in a study (37) with a large sample of participants (n = 241) with a range of serious medical conditions that found that self-compassionate people were more likely to take action with regard to their medical problems, including promptly visiting health care professionals when needed. Further analyses suggest that the benefits of self-compassion on outcomes results from the combined influence of benevolent self-talk, a motivation to treat oneself kindly, and a tendency to be proactive with regard to one’s health.
Self-Compassion and Hypothesized Effects in Diabetes Self-Management
Although research to date on self-compassion has not specifically examined its possible utility in diabetes patients, several considerations suggest that findings linking self-compassion to improved psychological and physical health, through both direct and indirect processes, could be of particular relevance to this group. First, the daily struggle of diabetes patients to maintain adequate control is frequently characterized by negative feelings of stress, anxiety, guilt, and shame (15), particularly when patients are continually reminded that their long-term health is dependent on their ability to self-manage. Second, maintaining good control involves ongoing adherence to a relentless daily self-management regimen to maintain optimal health and reduce the risk of long-term complications. Self-compassion may support adherence by reducing distressing and demotivating cognitive and emotional responses to medical problems such as self-blame, nonacceptance, and anger (43,45). Negative emotions often accompany a diagnosis of a chronic, incurable illness such as diabetes (15), and these emotions in themselves may be linked to self-regulatory failure (31). Third, self-compassion may be linked to improved adherence through increased conscientiousness (32). It may be that the emotional stability provided by self-compassion helps engender more responsible behavior, even though taking care of one’s health by maintaining a good diet and exercising frequently might initially involve a certain amount of displeasure.
Overall, the relationships between diabetes, psychological distress, depression, and self-care are complex, and the pathways by which they are related are not yet fully understood. What is clear, however, is that depression and distress play an important role in increasing the suffering and complications associated with managing this chronic condition (10,18) and that current approaches are having mixed success. Given the links between self-compassion and improved psychological and physical health, self-compassion–based interventions may be a supplementary approach with the potential to reduce suffering and its negative effects on physical health outcomes among diabetes patients.
Summary
Depression often complicates the original diagnosis of diabetes, leading to worse outcomes. Nascent research suggests that intervening to increase self-compassion, a construct that appears to tap into brain structures adapted for self-soothing and calming, may have quantifiable physiological, psychological, and behavioral effects that may help diabetes patients cope better with their condition and enjoy improved quality of life. In particular, the bulk of research to date suggests that processes involving a reduction in negative self-evaluation and improved motivations for self-care may underpin the beneficial effects of self-compassion on physical and psychological health. Thus, the utility of self-compassion as an intervention to reduce self-criticism, improve mood, and increase motivation to maintain self-care among diabetes patients may be worthy of substantial further investigation.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.World Health Organization Fact Sheet N 312—Diabetes. Available from http://www.who.int/mediacentre/factsheets/fs312/en. Accessed 14 August 2015
- 2.Snoek F, Skinner T. Psychological counseling in problematic diabetes: does it help? Diabet Med 2002;19:265–273 [DOI] [PubMed] [Google Scholar]
- 3.Andreoulakis E, Hyphantis T, Kandylis D, Iacovides A. Depression in diabetes mellitus: a comprehensive review. Hippokratia 2012;16:205–214 [PMC free article] [PubMed] [Google Scholar]
- 4.Ali S, Stone M, Peters J, Davies M, Khunti K. The prevalence of co-morbid depression in adults with type 2 diabetes: a systematic review and meta-analysis. Diabetic Med 2006;23:1165–1173 [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez J, Safren S, Gagliero E, et al. Depression, self-care, and medication adherence in type 2 diabetes. Diabetes Care 2007;30:2222–2227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pouwer F, Nefs G, Nouwen A. Adverse effects of depression on glycemic control and health outcomes in people with diabetes: a review. Endocrin Metab Clin North Am 2013;42:529–544 [DOI] [PubMed] [Google Scholar]
- 7.Lustman P, Clouse R. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes 2005;19:113–122 [DOI] [PubMed] [Google Scholar]
- 8.Van der Felt-Cornelis C, Nuyen J, Stoop C, et al. Effect of interventions for major depressive disorder and significant depressive symptoms in patients with diabetes mellitus: a systemic review and meta-analysis. Gen Hosp Psych 2010;32:380–395 [DOI] [PubMed] [Google Scholar]
- 9.Winkley K, Landau S, Eisler I, Ismail L. Psychological interventions to improve glycaemic control in patients with type 1 diabetes: systematic review and meta-analysis of randomized controlled trials. BMJ 2006;333:65–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hawamdeh S, Almakhzoomy I, Hayajneh Y. Screening and correlates of depression and HbA1c in United Arab Emirates (UAE) women with diabetes. Perspect Psychiatr Care 2013;49:262–268 [DOI] [PubMed] [Google Scholar]
- 11.Katon W. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci 2011;13:7–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Egede L, Osborn C. Role of motivation in the relationship between depression, self-care, and glycemic control in adults with type 2 diabetes. Diabetes Educ 2010;36:276–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neff K. The development and validation of a scale to measure self-compassion. Self Identity 2003;2:223–250 [Google Scholar]
- 14.Gilbert P. Introducing compassion focused therapy. Adv Psychiatr Treat 2009;15:199–208 [Google Scholar]
- 15.Barnard K, Lloyd C (Eds.). Psychology and Diabetes Care. London, U.K., Springer-Verlag, 2012 [Google Scholar]
- 16.Neff K. Self-compassion, self-esteem, and well-being. Soc Personal Psychol Compass 2011;5:1–12 [Google Scholar]
- 17.Neff K, Dahm K. Self-compassion: what it is, what it does, and how it relates to mindfulness. In Mindfulness and Self-Regulation. Robinson M, Meier B, Ostafin B, Eds. New York, Springer; In press [Google Scholar]
- 18.Golden S. A review of the evidence for a neuroendocrine link between stress, depression and diabetes mellitus. Curr Diabetes Rev 2007;3:252–259 [DOI] [PubMed] [Google Scholar]
- 19.Donath M, Shoelson S. Type 2 diabetes as an inflammatory disease. Nat Immunol 2011;11:98–104 [DOI] [PubMed] [Google Scholar]
- 20.Pizzi C, Manzoli L, Mancini S, Bedetti G, Fonatana F, Costa G. Autonomic nervous system, inflammation and preclinical atherosclerosis in depressed subjects with coronary risk factors. Atherosclerosis 2010;21:292–298 [DOI] [PubMed] [Google Scholar]
- 21.Kristiansen O, Mandrup-Pousen T. Interleukin-6 and diabetes: the good, the bad, or the indifferent. Diabetes 2005;54(Suppl. 2):S114–S124 [DOI] [PubMed] [Google Scholar]
- 22.Breines J, Thoma M, Gianferante D, Hanlin L, Chen X, Rohleder N. Self-compassion as a predictor of interleukin-6 response to acute psychosocial stress. Brain Behav Immun 2014;37:109–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rockliff H, Gilbert P, McEwan K, Lightman S, Glover D. A pilot exploration of heart rate variability and salivary cortisol responses to compassion-focused imagery. Clin Neuropsychiatry 2008;5:132–139 [Google Scholar]
- 24.Thayer J, Hansen A, Saus-Rose E, Johnsen B. Heart rate variability, prefrontal neural function, and cognitive performance: the neurovisceral integration perspective on self-regulation, adaption and health. Ann Behav Med 2009;37:141–153 [DOI] [PubMed] [Google Scholar]
- 25.Klimecki O, Leiberg S, Lamm C, Singer T. Functional neural plasticity and associated changes in positive affect after compassion training. Cereb Cortex 2013;23:1552–1561 [DOI] [PubMed] [Google Scholar]
- 26.Weng H, Fox A, Shackman A, et al. Compassion training alters altruism and neural responses to suffering. Psychol Sci 2013;1171–1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Macbeth A, Gumley A. Exploring compassion: a meta analysis of the association between compassion and psychopathology. Clin Psychol Rev 2013;32:545–552 [DOI] [PubMed] [Google Scholar]
- 28.Neff K, Germer C. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psych 2013;69:28–44 [DOI] [PubMed] [Google Scholar]
- 29.Neff K, Kirkpatrick K, Rude S. Self-compassion and adaptive psychological functioning. J Res Pers 2007;41:139–154 [Google Scholar]
- 30.Wren A, Somers T, Wright M, Goetz M, Leary M, Fras A. Self-compassion in patients with persistent musculoskeletal pain: relationship of self-compassion to adjustment to persistent pain. J Pain Symptom Manage 2012;43:759–770 [DOI] [PubMed] [Google Scholar]
- 31.Brion J, Leary M, Drabkin A. Self-compassion and reactions to serious illness: the case of HIV. J Health Psychol 2013;14:218–229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Neff K, Rude S, Kirkpatrick K. An examination of self-compassion in relation to positive psychological functioning and personality traits. J Res Pers 2006;41:908–916 [Google Scholar]
- 33.Gilbert P. Evolution and depression: issues and implications. Psychol Med 2006;36:287–297 [DOI] [PubMed] [Google Scholar]
- 34.Pinto-Gouveia J, Duarte C, Matos M, Fráguas S. The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic and in cancer patients. Clinical Psychol Psychother 2014;21:311–323 [DOI] [PubMed] [Google Scholar]
- 35.Hall C, Row K, Wuensch K, Godley K. The role of self-compassion in physical and psychological well-being. J Psychol 2013;147:311–323 [DOI] [PubMed] [Google Scholar]
- 36.Penninx B, Guralnik J, Ferrucci L, Simonsick E, Deeg D, Wallace R. Depressive symptoms and physical decline in community-dwelling older persons. JAMA 1988;279:1720–1726 [DOI] [PubMed] [Google Scholar]
- 37.Terry M, Leary M, Mehta S, Henderson K. Self-compassionate reactions to health threats. Person Soc Psychol Bull 2013;39:911–926 [DOI] [PubMed] [Google Scholar]
- 38.Breines J, Chen S. Self-compassion increases self-improvement motivation. Person Soc Psychol Bull 2012;38:1133–1143 [DOI] [PubMed] [Google Scholar]
- 39.Adams C, Leary M. Promoting self-compassionate attitudes toward eating among restrictive and guilty eaters. J Soc Clin Psychol 2007;26:1120–1144 [Google Scholar]
- 40.Magnus C, Kowalski K, McHugh T. The role of self-compassion in women’s self-determined motives to exercise and exercise-related outcomes. Self Identity 2010;9:3363–3382 [Google Scholar]
- 41.Kelly A, Zuroff D, Foa C, Gilbert P. Who benefits from training in self compassionate self-regulation? A study of smoking reduction. J Soc Clin Psychol 2010;29:727–755 [Google Scholar]
- 42.Ryan R, Deci E. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68–78 [DOI] [PubMed] [Google Scholar]
- 43.Terry M, Leary M. Self-compassion, self-regulation, and health. Self Identity 2011;10:352–362 [Google Scholar]
- 44.Baumeister R, Heatherton T. Self-regulation failure: an overview. Psychol Inq 1996;7:1–15 [Google Scholar]
- 45.Terry M, Leary M, Mehta S. Self-compassion as a buffer against homesickness, depression, and dissatisfaction in the transition to college. Self Identity 2013;12:278–290 [Google Scholar]