Abstract
Introduction:
Osteoarthritis (OA) is the most common age-related joint disease affecting >80% people beyond 55 years of age. It is a leading cause of elderly visit to outpatient departments and accounts for almost half of all nonsteroidal anti-inflammatory drug prescriptions. The burden and impact of knee OA in Indian population and extent of public health services usage by people with OA are not known.
Methods:
We performed a prospective blinded multicenter screening and therapeutic study from June 2013 to June 2014 at 3 centers to screen patients >55 years with knee OA to assess quality of life, functional disability, and limitation of functions and to compare the effectiveness of hip and leg strengthening exercise programs in these patients. Functional disability was assessed by Western Ontario and McMaster’s Universities OA index (WOMAC), Friedman, and Wyman Scores; locomotor function was assessed by walking status, Visual Analog Scale (VAS), and 30-second timed chair stand tests; and quality of life was assessed by Short Form-36 (SF-36).
Results:
Of 2854 patients screened, 2054 (72%) patients had OA (male:female-1.9:1) with mean age of 63 years and standard deviation of 8. Of 2054 patients, 226 patients were randomly selected for therapeutic study. In remaining 1828 patients, baseline 10-meter walk test (10MWT) was 0.3 m/s, mean SF-36 Physical Component Score (PCS) was 31.3, and Mental Component Score (MCS) was 34.2. At 3 months, 79% patients were comfortable with significant VAS, WOMAC, Friedman-Wyman Scores, 10MWT, and timed chair test improvements in patients who performed lifestyle modifications and exercises (P = .04). Short Form-36 improved, mean PCS was 43.6, and MCS was 54.2. At 3 months, 274 (15%) patients were unsatisfied among whom 26% and 74% were treated with arthroscopic procedures and arthroplasty, respectively. Isolated hip and leg strengthening exercise programs similarly improved knee pain, function, and quality of life.
Conclusion:
Motivation and counseling with hip and leg strengthening exercises should be incorporated with pharmacotherapy in each OA prescription. Physical fitness and weight reduction should be promoted as first-line management of OA.
Keywords: osteoarthritis, disability, knee, WOMAC, screening, India
Introduction
Osteoarthritis (OA) is the most common age-related joint disease affecting more than 80% of people older than the age1 of 55 and one of the leading causes of elderly visits to hospital outpatient departments. Osteoarthritis is one of the major reasons for family physician visits and accounts for almost half of all nonsteroidal anti-inflammatory drug (NSAID) prescriptions.2 Arthritis of the knee and hip in particular can compromise activities such as walking, climbing stairs, and self-care.3 Osteoarthritis especially of the hip and knee not only affects the quality of life of the individual physically but also emotionally and socially.
India has a high share of population beyond 55 years of age, and as the population ages, the economic impact of OA is expected to increase proportionately.4 By 2050, India’s 60 and older population is expected to encompass 323 million people, a number greater than the total US population in 2012.1,4 Despite the prevalence and burden of OA in India, there is little published data on epidemiology and long-term treatment outcomes from the subcontinent. There is little information about the use of health services by people with OA, making it difficult for policy makers and health care administrators to make decisions about resources allocation.
Osteoarthritis is one of the leading causes for absence of the elderly individuals from workplaces, social gatherings, and festivities. Often, these patients neglect and remain unsatisfied due to ignorance, delayed presentation, long duration of therapy, financial constraints, rampant quack practices,3 ineffective motivation, and counseling with ineffective exercise regimens. One of the challenges of managing OA is the prevailing perception among people that OA is a general aging procedure and that little can be done to slow down the progress of joint damage or improve joint function.5–7
India lacks community-based health centers, health programs, and access to occupational therapists and a healthy environment for the elderly patients to exercise and remain fit. The burden and impact of knee OA in the Indian population, policies, and the use of public health services by the people with OA are not known. Thus, we initiated this multicenter screening and therapeutic study at 3 centers in Bhubaneswar, India, to assess the knee OA burden in our population; to assess the quality of life, health status and functional disability, walking ability, limitation of functions in people living with knee OA; and to compare the effectiveness of hip and leg strengthening exercise programs in these patients.
Materials and Methods
This is a prospective blinded multicenter screening and therapeutic study from June 2013 to June 2014 at 3 centers in Bhubaneswar, Odisha, India. The purpose of this study was to screen the patients with knee OA in our population to assess the quality of life, health status and functional disability, knee pain, walking ability, and limitation of functions of people living with OA and to compare the effectiveness of hip and leg strengthening exercise programs in patients with knee OA.
Inclusion criteria: male/female, age >55 years, atraumatic knee pain, and foot and ankle pain.
Exclusion criteria: patients refusing treatment or consent.
Main Outcome Measures
Functional disability was assessed with Western Ontario and McMaster’s Universities OA index (WOMAC) and Friedmann and Wyman Classification of Functional Outcome.
Locomotor function was assessed using a walking pain (VAS) score and walking status grading, 10-meter walk test (10MWT), and the 30-second timed chair stand tests. General health, lower limb strength, range of movement, and compliance with exercise were also measured.
Social disability and quality of life was assessed by Short Form-36 Questionnaire (SF-36), Walking status grading, and 10MWT. All the tests were performed, and data were obtained at baseline, 1 month, 2 months, and 3 months through face-to-face interaction and, where appropriate, examination of hospital medical records.
Intervention: screening, physical therapy, pharmacotherapy.
Methodology
Screening Protocol
Patients beyond 55 years of age, complaining of knee or foot and ankle pain without history of trauma at the 3 centers, were included in the study for the screening procedure; the preliminary data of all these patients were entered in the data charts at the 3 centers and later were entered into the registry at the parent institution. The patients were subjected to history, clinical examination, standing X-rays of bilateral knee in anteroposterior and lateral views, and routine blood investigations such as blood sugar, serum uric acid, differential and complete blood counts, and synovial fluid examination in cases with knee effusion. Once knee OA was confirmed clinically and radiologically (see Table 1),8 the disease was graded, and the patient details were recorded for the data calculations and therapeutic procedures. All the patients were prescribed physiotherapy and pharmacotherapy for OA which included hip and leg strengthening exercises, water exercises, diet, and lifestyle modification (avoid squatting and cross leg sitting, usage of western toiletries, avoid sitting on knee, avoid walking for long distances, and shoe modification) with anti-OA medications for cartilage development (S-adenosyl methionine 400 mg twice daily) and pain relief (acetaminophen 325 mg–tramadol hydrochloride 37.5 mg twice daily). Patients with severe OA received intra-articular steroidal preparations and/or viscosupplementation, repeated 2 to 3 times over 3 months under strict aseptic precautions as required.
Table 1.
Radiographic Classification of Degenerative Joint Disease.a,b
| Grade | Description |
|---|---|
| Knees | |
| 0 | Normal |
| 1 | Doubtful narrowing of joint space and possible osteophytic lipping |
| 2 | Definite osteophytes and possible narrowing of joint space |
| 3 | Moderate multiple osteophytes, definite narrowing of joint space, some sclerosis, and possible deformity of bone ends |
| 4 | Large osteophytes, marked narrowing of joint space, severe sclerosis, and definite deformity of bone ends. Subchondral cysts may be present. |
| Hips | |
| 0 | Normal |
| 1 | Possible narrowing of joint space medially and possible osteophytes around the femoral head |
| 2 | Definite narrowing of joint space inferiorly, definite osteophytes, and slight sclerosis |
| 3 | Marked narrowing of joint space, slight osteophytes, some sclerosis and cyst formation, and deformity of femoral head and acetabulum |
| 4 | Gross loss of joint space with sclerosis and cysts, marked deformity of femoral head and acetabulum, and large osteophytes |
aAdapted from the Council for International Organization of Medical Sciences, 1963.
bAdapted from Rheumatic Diseases: Diagnosis and Management. Turek’s Orthopaedics: Principles and Their Application.8
Therapeutic Study Protocol
From the screened population, 226 patients with knee OA in age-group 55 to 70 were selected who gave consent were included in the therapeutic study group where they were randomly divided into 2 groups with male–female ratio of 1:1 (n = 113 each) by a person unaware of the therapeutic procedures and interventions. These patients received only mild analgesics to facilitate initial pain relief. Group 1 (113 patients) with KOA was assigned a 12-week hip strengthening exercise program and group 2 (113 patients) was assigned a 12-week leg strengthening exercise program. Both exercise programs consisted of a range of motion, strengthening, and flexibility exercises that were completed 3 to 5 days a week. The first 3 weeks of exercise were supervised, and the remaining 9 weeks consisted of at-home exercise aimed to improve muscle strength, endurance, and improving balance. Compliance was managed by telephonic conversations and home visits if required. The results were tabulated at 3-month follow-up.
Results
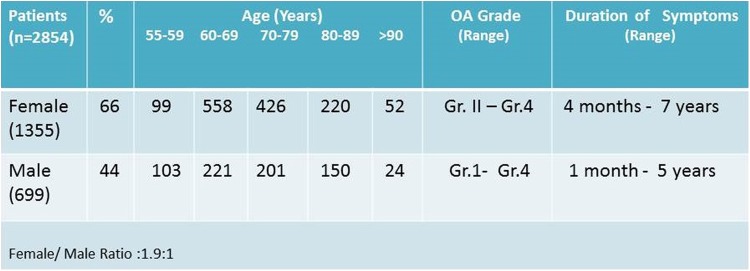
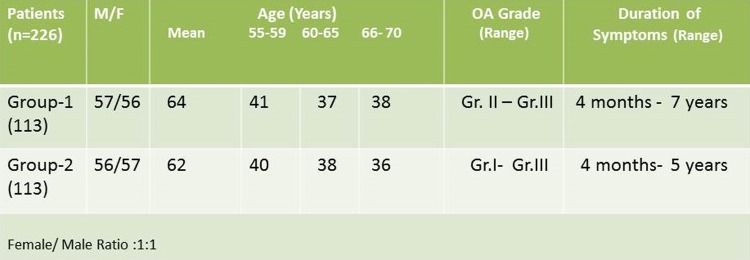
In our study, we screened 2854 patients beyond 55 years of age with atraumatic knee pain. Patient’s characteristics are represented in Figure 1. In all, 1355 (66%) were females and 699 (44%) were male patients with a female to male ratio of 1.9:1 with a wide range of age distribution from 55 to 92 years with a mean of 63 years, SD 8, and range 55 to 92 years. One thousand five hundred and seventy six(76.7%) patients were married, 478 (23.3%) patients were widowed, and 60% patients were working at the time presentation to hospital. Men were affected more in the 55 to 59 age-groups. We observed 2054 (72%) patients to have knee OA ranging from grade 1 to 4 based on the radiological classification (see Table 1),8 which was a significant finding (P = .02; see Figure 2).
Figure 1.
Patient characteristics of 2854 people—screening population.
Figure 2.
Pattern and grading of osteoarthritis (OA) in 2854 people.
Of the 2054 patients with OA, 226 patients (M:F = 1.1) in age-group 55 to 70 were selected and comprised the study population for the therapeutic study. Thus, in remaining 1828 patients, baseline WOMAC, Friedman-Wyman disability scores, and walking ability with the 30-second timed chair test data (mean and range) were performed and represented in Table 2. The mean 10MWT results for self-selected velocity was 0.3 m/s and fast velocity was 0.4 m/s. The patients had moderately low quality of life both physically and mentally, the baseline mean SF-36 PCS was 31.3, and MCS was 34.2.
Table 2.
Baseline: WOMAC, VAS, Friedman-Wyman Disability Scores, Walking Ability, and 30-Second Timed Chair Test Results.
| Patients With OA (n = 1828) | WOMAC (%) | VAS | Friedman-Wyman Score (%) | Walking Ability (%) | 30-Second Timed Chair Test (Range) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | Good | Fair | Poor | IV | III | II | I | ||
| Female (n = 1242) | 49 | 35-61 | 5 | 3-8 | - | 64 | 36 | 61 | 26 | 8 | 5 | 4-10 |
| Male (n = 586) | 44 | 29-60 | 4 | 2-7 | - | 70 | 30 | 65 | 25 | 6 | 4 | 5-14 |
Abbreviations: OA, Osteoarthritis; VAS, Visual Analog Scale; WOMAC, Western Ontario and McMaster’s Universities OA index.
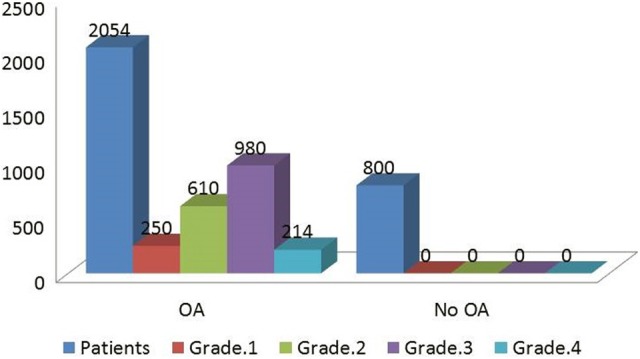
At 3 months, in 1828 patients, 1444 (79%) patients were comfortable with lifestyle modification and physiotherapy with medications and were performing daily routine activities. Among the 1444 patients, 505 (36%) and 361 (25%) patients required intra-articular steroidal preparations and viscosupplementation, respectively, which were repeated 2 to 3 times over 3 months (see Figure 3). The WOMAC and Friedman-Wyman disability scores, walking ability with the 30-second timed chair test, and 10MWT (mean and range) improved significantly (P = .04) over 3 months (see Table 3). At 3 months, mean 10MWT results for self-selected velocity was 0.5 m/s and fast velocity was 0.8 m/s, the quality of life (SF-36 values) improved, and the patients felt better physically and mentally. The mean PCS was 43.6 and MCS was 54.2.
Figure 3.
Treatment modality at 3 months in 1828 patients.
Table 3.
At 3 Months: WOMAC, VAS, Friedman-Wyman Disability Scores, Walking Ability, and 30-Second Timed Chair Test Results.
| Patients With OA (n = 1828) | WOMAC (%) | VAS Mean Range | Friedman-Wyman Score (%) | Walking Ability (%) | 30-Second Timed Chair Test, Range | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | Good | Fair | Poor | IV | III | II | I | ||
| Female (n = 1242) | 36 | 26-49 | 3 | 0-4 | 16 | 72 | 12 | 75 | 45 | 7 | 1 | 7-14 |
| Male (n = 586) | 31 | 21-43 | 2 | 0-4 | 22 | 70 | 8 | 82 | 15 | 2 | 1 | 7-16 |
Abbreviations: OA, Osteoarthritis; VAS, Visual Analog Scale; WOMAC, Western Ontario and McMaster’s Universities OA index.
At 3 months, among 1828 patients, 110 (6%) patients did not perform the exercises or lifestyle modification as advised seeking excuses such as lack of time, household work pressure, lack of motivation, embarrassment, and laziness. Only 31 (28%) patients were comfortable with medications alone, and the remaining 79 (72%) reported to the outdoor with similar or more complaints. There were significant differences in terms of VAS, WOMAC scores, Friedman-Wyman scores, 10MWT, timed chair test, and analgesic requirement in patients who did and who did not perform lifestyle modifications and exercises at 3-month follow-up (P = .02).
At 3-month follow-up, of 1828 patients, 274 (15%) patients were unsatisfied with the physical and medical therapy, and these patients had mostly grade 3 and 4 OA, who were then counseled for surgical procedures. Sixty-eight (26%) were treated with arthroscopic joint lavage and debridement with intra-articular steroidal preparation, and 206 (74%) patients required surfacing or total knee arthroplasty. These patients were mostly grade 3 and 4 knee OA. Patients in the surgical group had significant improvement in VAS, WOMAC, and timed chair test when compared to the physiotherapy/pharmacotherapy group (P = .03). Pre and postoperative VAS, WOMAC, Friedman-Wyman scores, walking ability, and 30-second timed chair test (mean and range) are represented in Table 4.
Table 4.
Pre and Postoperative: WOMAC, VAS, Friedman-Wyman Disability Scores, Walking Ability, and 30-Second Timed Chair Test Results.
| Surgical Population (n = 274) | WOMAC (%) | VAS | Friedman-Wyman Score (%) | Walking Ability (%) | 30-Second Timed Chair Test, Range | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | Good | Fair | Poor | IV | III | II | I | ||
| Preoperative | 46 | 41-61 | 5 | 3-8 | 0 | 44 | 56 | 28 | 52 | 8 | 12 | 4-10 |
| Postoperativea | 28 | 22-32 | 2 | 0-4 | 20 | 75 | 5 | 65 | 29 | 4 | 2 | 8-13 |
Abbreviation: VAS, Visual Analog Scale; WOMAC, Western Ontario and McMaster’s Universities osteoarthritis index.
aArtroplasty (n = 206 cases) and arthroscopy (n = 68 cases), P = .03.
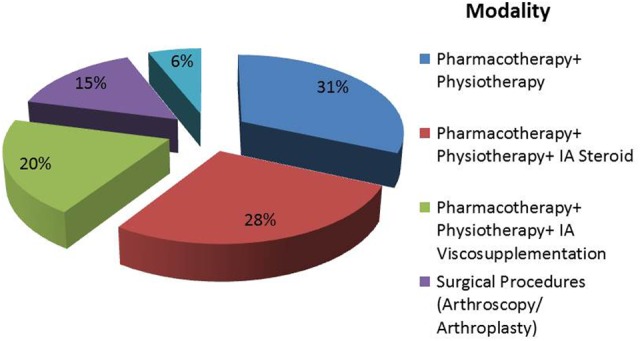
In the therapeutic exercise group, of 226 patients, 113 were females and 113 were male patients with a female–male ratio of 1:1, mean age 63 years, SD 8, and range 55 to 70 years to compare the effectiveness of hip and knee exercises for knee OA. Patient characteristics for groups 1 and 2 are represented in Figure 4.
Figure 4.
Patient characteristics of 226 people—therapeutic population.
For groups 1 and 2, pre- and posttherapeutic VAS, WOMAC, Friedman-Wyman scores, and 30-second timed chair test (mean and range) are represented in Table 5. Both the groups had similar significant improvement (P = .02) when compared to their pretherapeutic status.
Table 5.
Pre- and Posttherapeutic: WOMAC, VAS, Friedman-Wyman Disability Scores, Walking Ability, and 30-Second Timed Chair Test Results.
| Therapeutic Population (n = 226) | WOMAC (%) | VAS | Friedman-Wyman Score (%) | 30-Second Timed Chair Test, Range | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | Good | Fair | Poor | |||
| Pretherapeutic | 47 | 29-61 | 5 | 2-8 | 10 | 67 | 23 | 4-12 | |
| Posttherapeutic (n = 226) | Group 1 (hip ex), n = 113 | 30 | 26-38 | 2 | 0-4 | 22 | 73 | 5 | 8-15 |
| Group 2 (leg ex), n = 113 | 31 | 24-36 | 2 | 0-4 | 24 | 71 | 5 | 9-15 | |
Abbreviations: VAS, Visual Analog Scale; WOMAC, Western Ontario and McMaster’s Universities osteoarthritis index; ex, exercise.
Discussion
Osteoarthritis, the most common joint disease, is age related, affecting more than 80% of people older than the age of 55.8 It is more common in women, especially after menopause. Osteoarthritis of the knees is common, and risk is strongly linked to body mass index.8 Symptoms include pain with walking, standing up from a chair, climbing or descending stairs, and stiffness after periods of rest. Patients will typically report pain that is increased with activity and relieved by rest, although rest pain occurs in advanced disease. “Gelling”—stiffness that occurs after any period of rest—is also common. Morning stiffness, when present, rarely lasts more than 30 minutes. The heterogeneity of OA arises from the many factors that can contribute to cartilage damage.
British Columbia Osteoarthritis (BCOA) Survey’ 2008 found mean age of participants to be 67.3 years, SD 11.1, and more than 30% continued to work at the time of presentation, whereas we found it to be 63 years, SD 8, and more than 60% continued to work, this could be attributed to the financial stress, large family size, low Gross Domestic Product (GDP), and per capita income in our country due to which most elderly patients cannot afford a relaxing retirement time. In Canada in 2004 to 2005, there were 8734 joint replacement surgeries, and the number increased to more than 10 000 in 2006 to 2007. By 2020, this figure is estimated to rise to 20 000 with an annual cost of US$230 million.2
India has a high share of population beyond 55 years of age, and as the population ages, the economic impact of OA is expected to increase proportionately.1,2,4 The United Nations (UN) Population Division projects that India’s population aged 50 and older will reach 34% by 2050 (UN 2011). Between 2010 and 2050, the share 65 and older is expected to increase from 5% to 14%, while the share in the oldest age-group (80 and older) will triple from 1% to 3%. Life expectancy at birth in India climbed from 37 years in 1950 to 65 years in 2011, reflecting declines in infant mortality and survival at older ages in response to public health improvements.1,4
The pathogenesis of OA involves an imbalance between normal cartilage degenerative and repair mechanisms, which results in net loss of cartilage, hypertrophy of bone, and generation of osteophytes, which are the single most common feature of OA.8 Osteoarthritis has a predilection for finger joints, knees, hips, shoulders, and the spine. Occurrence in an atypical joint, such as an elbow, can usually be traced to prior trauma, a congenital joint abnormality, underlying systemic disease, or a chronic crystalline arthropathy. The characteristic radiographic features of OA are osteophytes, asymmetric joint space narrowing, subchondral bone sclerosis, and subchondral cysts beneath eburnated or sclerotic surfaces. The severity of OA can be scored based on these 4 common features. Arthritis of the knee and hip in particular can compromise activities such as walking, climbing stairs, and self-care.9,10
The natural history of OA may be one of slow, chronic progression, or of stable periods with intermittent worsening. With new or increased pain, there is a natural tendency to reduce activity. As activity decreases over time so does muscle bulk and strength, which may lead to decreased joint stability, worsening of joint degeneration, and further decline in functional status which can have major systemic consequences, affecting cardiovascular health, emotional health, and sense of well-being. Breaking this cycle may require a team approach targeted toward educating the patient and family, evaluating and sometimes altering the patient’s lifestyle, offering assistive devices, and prescribing both physical and pharmacotherapy.
Treatments for OA consist of education, exercise, weight management, medication, and surgery.11–13 Patient education is vital, especially in early disease where intervention is most likely to be effective. Obesity is one of the most important risk factors for the development of severe OA of the knee.14 Among people with OA who are overweight, even a moderate weight loss of 5% can significantly improve physical disability,15 hence these patients should be counseled to maintain weight loss and increasing or at least maintaining muscle strength which alters course of disease and improve their level of safety and functioning. Periodic rest of affected joints is appropriate, especially in acute disease exacerbations, but excessive rest or reduction in activity may begin the cycle of atrophy, weakness, and further functional decline, which may actually worsen pain over time.
Exercise, weight management, and medications are the first-line treatment for OA. Regular exercise is beneficial for people with OA and16 is required to strengthen muscles, reduce pain, and improve the functional status of patients with mild to moderate OA. Although exercise improves OA pain, people in pain may avoid exercise and, therefore, may not adhere to the exercise regime;17 thus, health professionals should tailor the type and intensity of exercise according to the individual needs and abilities of the patient and should provide guidance. Also, integrating physical activities and exercise into one’s personal lifestyle helps adherence.18 For patients with moderately severe OA pain, a twice-daily set of supine 10-second isometric quadriceps contractions can improve strength, reduce pain, and reduce the risk of falling. In general, low impact exercise, such as walking, is preferred to high impact exercise, such as running or jogging. Exercise in water helps to unload the weight-bearing joints, can be especially beneficial when weight-bearing pain in the knees, back, or hips limits land exercise. Exercises performed in a group under supervision have better functional results and compliance as compared to exercises performed in home-based exercise programs. India lacks community-based fitness centers, groups, or activities for geriatric population with OA.
Although the American College of Rheumatology’s (ACR) recommends that, at minimum, people with arthritis should accumulate 30 minutes of moderate-intensity physical activity (eg, brisk walking), 3 days a week or the equivalent 90 minutes per week.19 In our study, only 20% people met the ACR recommendation on physical activity. Physical therapists can instruct patients on the proper use of canes and walkers, to decrease weight-bearing stress on knees and hips, reduce the risk of injurious falls, and reduce the fear of falling that by itself can greatly limit patient mobility. Therapists can also instruct patients on the proper use of transcutaneous electrical nerve stimulation units to reduce pain in specific areas. Insoles, braces, and orthopedic shoes can benefit OA of the knees, ankles, and feet. Biomechanical studies show that knee braces and lateral wedged shoe inserts can sometimes reduce pain of medial knee joint OA by shifting weight to the less affected lateral compartment. Medial patellar taping may reduce the lateral compartment pain of patellofemoral syndrome. Paraffin baths are particularly soothing for the pain of erosive OA.
Pharmacotherapy for OA constitutes topical (rubefacient) therapies, intra-articular therapies, oral analgesic therapies, and dietary supplements. Topical capsaicin can selectively reduce pain sensation in that region by depleting substance P from type C unmyelinated pain neurons. Intra-articular corticosteroid injections are particularly helpful when there is inflammation and joint effusion. Intra-articular injection of hyaluronic acid derivatives is beneficial for mild to moderate OA of the knee, particularly for patients who cannot take analgesics or who are not candidates for joint replacement. Oral analgesics are mainstay in the management of OA pain and include acetaminophen, NSAIDs, selective (COX-2) inhibitors, nonacetylated salicylates, synthetic opioid agonists, and narcotics. Almost all oral analgesics have some potential for hepatic toxicity. Dietary supplements, such as glucosamine sulfate, are now widely used. Studies suggest that it may slow cartilage breakdown or at least a modest benefit of reduced pain or reduce need for other oral analgesics.
Surgical intervention is considered for intractable and rest pain or deformity. It includes arthroplasty (unicompartmental and total knee replacement), osteotomy, and joint preserving surgical procedures for severe OA, joint fusion as a salvage procedure when joint replacement had failed,14 and arthroscopic procedures (joint lavage and debridement, microfractures, and cartilage transplant procedures) for early and moderate OA.
One of the challenges of managing OA is the prevailing perception among people that OA is a general part of the aging procedure and that little can be done to slow down the progress of joint damage or to improve joint function.5–7 India lacks community-based health centers, health programs, and access to occupational therapists and a healthy environment for the elderly patients to remain fit and exercise.
For effective management of people with OA and reduction of OA burden from the community, to improve the quality of life in patients with OA and the quality of OA care in the community, work to improve the awareness about the myths and facts of OA and the use of inexpensive an effective approaches, such as improving physical fitness and weight reduction by an integrated approach as the first-line management should be promoted through paper, electronic media, and demonstrations with support from non-governmental organization’s dealing with geriatric concerns and the government.
Conclusion
Isolated hip and leg strengthening exercise programs seem to similarly improve knee pain, function, and quality of life in patients with knee OA. Patients who performed exercises with diet and lifestyle modifications showed significant improvements in balance, locomotor function, and routine activity with decrease in pain, analgesic requirement, improved WOMAC, Friedman-Wyman scores, 10MWT, and timed chair test results at 3-month follow-up. Patients also demonstrated smaller but significant improvements in balance, strength, and SF-36 results.
Optimal exercise programs for knee OA should have one aim and focus on improving aerobic capacity, quadriceps muscle strength, or lower extremity performance. For best results, the program should be supervised. Thus with a good motivation and counselling, both hip and leg strengthening exercises should be incorporated into their exercise prescription of patients with knee OA along with the pharmacotherapy.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Population Reference Bureau. India’s Aging Population. Today’s Research on Aging. Program and Policy Implications. No. 25; 2012:1–6. [Google Scholar]
- 2. Li L. British Columbia Osteoarthritis survey on 6000 patients British Columbia Ministry of Health The Arthritis Society, BC: & Yukon Division, Arthritis Research Centre of Canada; January 2008. [Google Scholar]
- 3. Dash SK, Panigrahi R, Palo N, Priyadarshi A, Biswal MR. Fragility Hip Fractures in Elderly Patients in Bhubaneswar, India (2012-2014). A Prospective Multicenter Study of 1031 Elderly Patients. Geriatric Orthopaedic Surgery & Rehabilitation. December 18, 2014; doi: 10.1177/2151458514555570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Situation Analysis of the Elderly in India. New Delhi, India: Central Statistics Office Ministry of Statistics & Programme Implementation, Government of India; 2011. [Google Scholar]
- 5. Hudak PL, Clark JP, Hawker GA, et al. “You’re Perfect for the Procedure! Why Don’t You Want It?” Elderly Arthritis Patients’ Unwillingness to Consider Total Joint Arthroplasty Surgery: a qualitative study. Med Decis Making. 2002;22(3):272–278. [DOI] [PubMed] [Google Scholar]
- 6. Gignac MA, Davis AM, Hawker G, et al. “What do you expect? You’re just getting older”: a comparison of perceived osteoarthritis-related and aging-related health experiences in middle- and older-age adults. Arthritis Rheum. 2006;55(6):905–912. [DOI] [PubMed] [Google Scholar]
- 7. Appelt CJ, Burant CJ, Siminoff LA, Kwoh CK, Ibrahim SA. Arthritis-specific health beliefs related to aging among older male patients with knee and/or hip osteoarthritis. J Gerontol A Biol Sci Med Sci. 2007;62(2):184–190. [DOI] [PubMed] [Google Scholar]
- 8. Weinstein SL, Buckwalter JA. Rheumatic diseases: diagnosis and management In: Weinstein SL, Buckwalter JA, eds. Turek’s Orthopaedics: Principles and Their Application, 6th Edition Philadelphia, PA: Lippincott Williams & Wilkins; 2005:154–162. [Google Scholar]
- 9. Corti MC, Rigon C. Epidemiology of osteoarthritis: prevalence, risk factors and functional impact. Aging Clin Exp Res. 2003;15(5):359–363. [DOI] [PubMed] [Google Scholar]
- 10. Fines P, Flanagan W, Kopec JA, et al. Projecting number of osteoarthritis patients from 2001 to 2021 in Canada using microsimulation. Int Soc Qual. 2007;49(suppl A):Abstract #1598. [Google Scholar]
- 11. Hochberg MC, Altman RD, Brandt KD, et al. Guidelines for the medical management of osteoarthritis. Part I. Osteoarthritis of the hip. American College of Rheumatology. Arthritis Rheum. 1995;38(11):1535–1540. [DOI] [PubMed] [Google Scholar]
- 12. Hochberg MC, Altman RD, Brandt KD, et al. Guidelines for the medical management of osteoarthritis. Part II. Osteoarthritis of the knee. American College of Rheumatology. Arthritis Rheum. 1995;38(11):1541–1546. [DOI] [PubMed] [Google Scholar]
- 13. Ottawa panel evidence-based clinical practice guidelines for therapeutic exercises and manual therapy in the management of osteoarthritis. Phys Ther. 2005;85(9):907–971. [PubMed] [Google Scholar]
- 14. Bliddal H, Christensen R. The management of osteoarthritis in the obese patient: practical considerations and guidelines for therapy. Obes Rev. 2006;7(4):323–331. [DOI] [PubMed] [Google Scholar]
- 15. Christensen R, Bartels EM, Astrup A, Bliddal H. Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: a systematic review and meta-analysis. Ann Rheum Dis. 2007;66(4):433–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Westby MD, Li L. Physical therapy an exercise for arthritis: Do they work? Geriatr Aging. 2006;9(9):624–630. [Google Scholar]
- 17. van Gool CH, Penninx BJ, Kempen GI, et al. Effects of exercise adherence on physical function among overweight older adults with knee osteoarthritis. Arthritis Rheum. 2005;53(1):24–32. [DOI] [PubMed] [Google Scholar]
- 18. Westby MD, Li L. Physical therapy an exercise for arthritis: do they work? Geriatr Aging. 2006;9(9):624–630. [Google Scholar]
- 19. Minor M, Stenstrom CH, Klepper SE, Hurley M, Ettinger WH. Work group recommendations: 2002 exercise and physical activity conference, St. Louis, Missouri. Arthritis Rheum. 2003;49(3):453–454. [DOI] [PubMed] [Google Scholar]