Abstract
Background:
Reoperation of femoral neck fractures in elderly patients is frequent. Our aim was to determine predictors of reoperations following primary internal fixation with 3 cannulated screws.
Materials and Methods:
A follow-up study included all patients aged 65+ years old patients consecutively admitted to an orthopedic ward with femoral neck fracture in the period from January 1, 2007, to December 31, 2010, and fixed with cannulated screws. We retrospectively obtained all available data from patient databases related to potential predictors of reoperations: gender, age, dwelling, dementia, body mass index, vitamin D, albumin, prednisolone treatment, walking aid, performance of activities of daily living, low-energy trauma, initial displacement, and surgery quality. Outcome was reoperation due to fixation failure/prominent screws, nonunion, or avascular necrosis of femoral head within 2 years after surgery. By multivariate Cox proportional hazards regression, including mortality as a competing risk, we estimated crude and adjusted hazards ratios (HRs) with 95% confidence intervals (CIs) for reoperation.
Results:
Two years after surgery, 29% of 322 elderly patients underwent reoperation. Reoperation was associated with primary fracture displacement (HRadjusted 1.61; 95% CI: 1.01-2.55; P = .04) compared to undisplacement. A poor quality of primary reduction was associated with a higher risk of reoperations than a good quality (HRadjusted 1.95; 95% CI: 1.02-3.72; P = .04). Elderly individuals in own homes and sheltered housings had a higher risk of reoperation (HRadjusted 2.67; 95% CI 1.35-5.31; P = .005) compared to nursing home residents.
Conclusion:
Our findings support the evidence of a higher incidence of reoperation in displaced femoral neck fractures compared to the nondisplaced and is associated with poor quality of fracture reduction. Reoperations are most frequent in younger and more independent patients living at home.
Keywords: femoral neck fracture, reoperation, elderly individuals, cannulated screws
Introduction
Hip fractures are common in the elderly individuals and associated with increased morbidity and mortality. In Denmark, in 2013, the hip fracture rate was 6.86 per 1000 inhabitants in the population aged 65+ years.1 Femoral neck fractures account for 55% of the hip fractures including both nondisplaced and displaced fractures.1 The Danish national guidelines on treatment of hip fractures recommend internal fixation in nondisplaced fractures, whereas arthroplasty is recommended in displaced fractures.2–6 However, internal screw fixation is in some cases considered the treatment of choice in frail elderly individuals due to shorter operation time, less bleeding, and fewer blood transfusions compared to prosthetic replacement.7,8 Furthermore, use of cement in hip hemiarthroplasty of fractured femoral neck is associated with increased perioperative death or severe harm.9
A major disadvantage of internal fixation is the high number of reoperations caused by fixation failure, nonunion fracture, and avascular necrosis of the femoral head.10 Within 2 years after primary surgery, the incidence of reoperations has been reported to be between 20% and 36% after internal fixation versus 6% and 18% after hemiarthroplasty.3,6 A varus collapse of the femoral neck after fixation of the fracture is correlated with shortening of the femoral neck and results in impaired quality of life (QoL).11 After 2 years, patients with nondisplaced fractures report a better functional status and QoL.12
Previous studies have investigated single components in the healing process of the femoral neck fracture in the elderly individuals: Healing takes longer as bone mineral density declines with age.13–15 Prevalence of osteoporosis thus increases with age, and consequently the incidence of low-energy fractures is more frequent in elderly individuals. Moreover, risk of secondary displacement is enhanced due to frail trabecular and cortical bone.13,16 Female gender, malnutrition (low albumin), vitamin D deficiency, and prednisolone treatment are associated with reduced bone mineral density.17,18 Bone quality and healing potential combined with the fracture pattern and inadequate fixation techniques are the most important issues for hardware failure.3 Despite the growing amount of research in this field, there is no clinical consensus on the characteristics in the elderly patients with hip fractures at risk of reoperation. The purpose of this study was to identify factors that predict reoperation in elderly patients with screw fixed femoral neck fractures and to identify the type of elderly patients with the highest risk of reoperation.
Materials and Methods
Population, Design, and Ethics
The study was conducted as a case–cohort study, and the source population was all patients aged 65 years and older admitted to our hospital with a femoral neck fracture between January 1, 2007, and December 31, 2010. All included were treated operatively with 6.5 mm cannulated screw fixation from Smith & Nephew, Inc (Memphis, Tennessee). Patients with cancer in the hip and patients who left the country were excluded. The study was approved by the Danish Data Protection Agency, and no approval was needed from the Central Denmark Region Committee on Biomedical and Research Ethics.
Data Collection
Data were obtained from the electronic patient records, national databases, and a local research database in the Department of Geriatrics at Aarhus University Hospital in Denmark.
Baseline data were collected on gender, age, type of dwelling (own home/sheltered housing/nursing home), dementia diagnosis, body mass index (BMI), vitamin D level measures < 1 year before the fracture until <1 month after (normal: ≥ 50 nmol/L/deficiency: 25 to 49 nmol/L/osteomalacia: <25 nmol/L19), albumin level at admission (normal: ≥ 34 g/L/low: < 34 g/L), treatment with prednisolone <1 year before the fracture until <1 month after, use of prefracture walking aids (none/sticks/frame/wheelchair), performance of activities of daily living (ADLs) between 2nd and 30th postoperative day measured by the Modified Barthel Index (self-sufficiency/moderate dependent/ substantial or complete dependent),20 low-energy trauma, and fracture type according to Garden classification (I-II = nondisplaced/ III-IV = displaced).21
Good reduction was considered when Garden angle on the anteroposterior (AP) view was 160° to 175°, the posterior or anterior angulation on the lateral view was ≤10°, and a maximum fracture displacement of 2 mm. Fair reduction was defined when Garden angle was 160° to 175°, the posterior or anterior angulation on the lateral view was maximum 20°, and if the fracture displacement was maximum 5 mm. Poor reduction was defined as Garden angle outside interval of 160° to 175° or more than 20° angulation in the lateral view or more than 5-mm fracture displacement.22
Cases were all patients who underwent reoperation within 3 months and 2 years due to (1) fixation failure/prominent screws, (2) nonunion, or (3) avascular necrosis of the femoral head. Nationwide data were collected for all patient hospitalizations according to reoperation during 2 years follow-up. Reoperation due to infection was not included in the assessment of patient outcome. All patients who died within the 2 years of follow-up were registered.
Postsurgery Care and Follow-Up
The patients were allowed to perform weight bearing as tolerated. Mobilization was initiated the day after surgery by a physiotherapist. Patients were discharged from the orthopedic surgery department 1 to 2 days after surgery either to their own home with follow-up by a physiotherapist or to rehabilitation in the geriatric ward. Special attention was paid to impaired gait, persistent pain, and wound infection. A routine X-ray examination after 3 postoperative months, or if it was needed, was performed in the orthopedic outpatient clinic.
Statistical Analysis
Baseline characteristics were categorized and presented with percentages. Reoperation within 2 years after hip fracture surgery was the dichotomous outcome variable. Time-to-event analyses were applied in all baseline variables. Multivariate Cox proportional hazards regression analysis was used to estimate crude and adjusted hazards ratios (HRs) with 95% confidence intervals (CIs). According to well-known factors related to bone quality, healing, inadequate fixation, and fracture pattern, we adjusted for gender, age, quality of fracture reduction, Garden type (fracture stability), prednisone treatment, and proxy measure of osteoporosis: low-energy fracture. Mortality was considered as a competing risk factor in the Cox regression analysis in which patients were censored at the date of death during the 2-years follow-up. Subsequently, the regression model was checked for proportionality by log–log plots. Missing data were not replaced by multiple imputations. If data were missing on the single patient, this patient was excluded from the analysis. The analyses were performed with Stata software version 13.1. A P value of 5% or less was considered statistically significant.
Results
During a 4-year period, 325 elderly individuals with femoral neck fractures underwent surgical repair with cannulated screws of whom 3 patients were excluded, 2 patients were reoperated due to infection and 1 patient due to cancer in the hip. Mean age of included patients was 82 years (± 8.3), and the population was a majority of females, frequently with low-energy trauma, and 30% were admitted from nursing homes. More than half of the elderly individuals were dependent on walking aids before the hip fracture. About half of the fractures were displaced, and 12% of the initial surgical repair repositions with cannulated screws were performed inadequately (Table 1).
Table 1.
Baseline Characteristics.a
| Baseline | N = 322 | |
|---|---|---|
| n | (%) | |
| Females | 229 | (71) |
| Age, y | ||
| 65-74 | 66 | (21) |
| 75-84 | 114 | (35) |
| ≥85 | 142 | (44) |
| Dwelling | ||
| Own home | 187 | (59) |
| Sheltered housing | 37 | (11) |
| Nursing home | 98 | (30) |
| Dementia diagnosis | 55 | (17) |
| Body Mass Index | ||
| Underweight (<20) | 48 | (15) |
| Normal weight (20-24) | 140 | (43) |
| Overweight (25-29) | 74 | (23) |
| Obesity (≥30) | 15 | (5) |
| Missing data | 45 | (14) |
| Vitamin D level, nmol/L (<1 year prefracture, <1 month postfracture) | ||
| Normal (≥50) | 115 | (36) |
| Deficiency (25-49) | 59 | (18) |
| Osteomalacia (<25) | 41 | (13) |
| Missing data | 107 | (33) |
| Albumin, g/L | ||
| Low (<34) | 33 | (10) |
| Normal | 287 | (89) |
| Missing data | 2 | (1) |
| Prednisone treatment | ||
| (<2 years prefracture < 1-month postfracture) | 32 | (10) |
| Walking aid prefracture | ||
| None | 130 | (40) |
| Stick(s) | 48 | (15) |
| Frame (standard/rollator) | 109 | (34) |
| No walking ability | 5 | (2) |
| Missing data | 30 | (9) |
| ADL performance (within 2-30 days postfracture) | ||
| Independent | 45 | (14) |
| Moderate dependent | 75 | (23) |
| Substantial dependent | 65 | (20) |
| Missing data | 137 | (43) |
| Low-energy trauma | 266 | (85) |
| Fracture classification | ||
| Undisplaced (Garden I-II) | 167 | (52) |
| Displaced (Garden III-IV) | 155 | (48) |
| Quality of reposition | ||
| Good | 211 | (66) |
| Fair | 65 | (20) |
| Poor | 38 | (12) |
| Missing data | 8 | (2) |
Abbreviation: ADL, activities of daily living.
aAll patients aged 65+ years with femoral neck fracture treated with 3 cannulated screws in the years of 2007 to 2010.
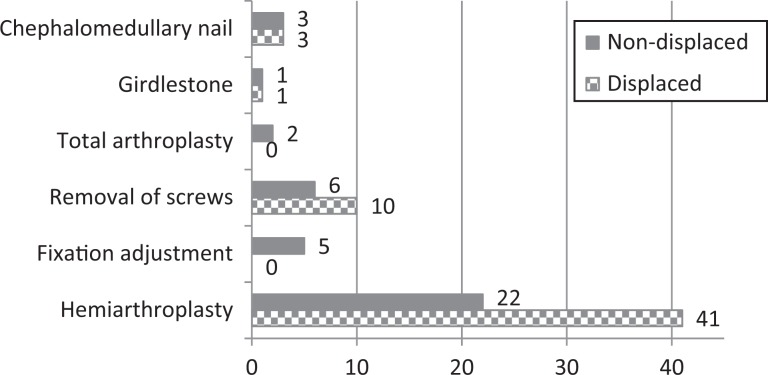
Median day for time to reoperation was 144 (interquartile range: 56-259). Within 3 months after surgery, 12% of the elderly individuals were reoperated due to failed internal fixation. Within 2 years after surgery, 29% of the elderly individuals underwent resurgery due to failed internal fixation/prominent screws (n = 62, 19%), nonunion (n = 13, 4%), and avascular necrosis (n = 19, 6%). In patients with nondisplaced fractures, 24% were reoperated, and in patients with displaced fractures, 35% were reoperated (P = .03). All the reoperations were conducted at our hospital. Overview of reoperations is illustrated in Figure 1. The crude regression analysis showed that reoperations were associated with age between 65 and 74 years, living in own home or sheltered housing, independent concerning ADL, nondementia, primary displacement, and poor quality of surgical reposition. After adjustments, reoperation was no longer associated with nondementia or ADL independency (Table 2). The elderly individuals from own homes and sheltered housings had an almost 3-fold risk of secondary displacement compared to nursing home residents (HR adjusted 2.67, 95% CI 1.34-5.31; P = .005; Figure 2). Furthermore, underweight seems to be associated with a lower risk of reoperation compared to elderly individuals with a BMI ≥ 19 (HRadjusted 0.33, 95% CI 0.11-0.95; P = .04). Trends toward lower risk of reoperation were seen in males, patients with dementia, and elderly individuals with no walking ability and substantial ADL dependency.
Figure 1.
Reoperation treatment divided into initial displaced and nondisplaced femoral neck fractures (n = 94).
Table 2.
Cox Regression Analysis.a
| Reoperation for secondary displacement (N = 322) | |||||||
|---|---|---|---|---|---|---|---|
| Proportion | Crude hazard ratio | 95% CI | P value | Adjusted hazard ratiob | 95% CI | P value | |
| Gender | |||||||
| Male | 25/94 | 1.00 | reference | 1.00 | reference | ||
| Female | 69/228 | 1.13 | 0.69-1.84 | .63 | 1.32 | 0.79-2.19 | .29 |
| Age, y | |||||||
| 65-74 | 28/66 | 1.00 | reference | 1.00 | reference | ||
| 75-84 | 41/114 | 0.85 | 0.52-1.40 | .53 | 0.90 | 0.53-1.51 | .69 |
| ≥85 | 25/142 | 0.56 | 0.32-0.98 | .04 | 0.47 | 0.27-0.85 | .01 |
| Dwelling | |||||||
| Own home | 66/187 | 1.00 | reference | 1.00 | reference | ||
| Sheltered housing | 18/37 | 1.86 | 1.08-3.21 | .02 | 2.05 | 1.11-3.77 | .02 |
| Nursing home | 10/98 | 0.38 | 0.19-0.74 | .005 | 0.45 | 0.22-0.91 | .03 |
| Dementia diagnoses | |||||||
| No | 88/267 | 1.00 | reference | 1.00 | reference | ||
| Yes | 6/55 | 0.39 | 0.17-0.91 | .03 | 0.47 | 0.20-1.09 | .08 |
| Body mass index | |||||||
| Underweight (<19) | 5/48 | 0.42 | 0.16-1.06 | .06 | 0.33 | 0.11-0.97 | .04 |
| Normal weight (19-24) | 47/140 | 1.00 | reference | 1.00 | reference | ||
| Overweight (25-29) | 26/74 | 1.10 | 0.67-1.80 | .69 | 1.06 | 0.63-1.77 | .83 |
| Obesity (≥30) | 4/15 | 0.70 | 0.22-2.27 | .55 | 0.70 | 0.17-2.91 | .62 |
| Vitamin-D level, nmol/L | |||||||
| Normal (≥ 50) | 38/115 | 1.00 | reference | 1.00 | reference | ||
| Deficiency (25-49) | 22/59 | 1.11 | 0.64-1.91 | .70 | 1.11 | 0.63-1.96 | .71 |
| Osteomalacia (<25) | 11/41 | 0.78 | 0.37-1.64 | .53 | 0.82 | 0.38-1.74 | .61 |
| Albumin, g/L | |||||||
| Normal | 87/287 | 1.00 | reference | 1.00 | reference | ||
| Low (<34) | 5/33 | 0.67 | 0.24-1.83 | .43 | 0.57 | 0.18-1.87 | .36 |
| Prednisone treatment | |||||||
| No | 80/287 | 1.00 | reference | 1.00 | reference | ||
| Yes | 13/32 | 1.79 | 0.92-3.46 | .08 | 1.50 | 0.73-3.03 | .26 |
| Walking aid prefracture | |||||||
| None | 47/130 | 1.00 | reference | 1.00 | reference | ||
| Sticks | 14/48 | 0.90 | 0.48-1.67 | .75 | 1.01 | 0.53-1.93 | .97 |
| Frame (standard/rollator) | 26/109 | 0.65 | 0.39-1.08 | .10 | 0.66 | 0.37-1.17 | .16 |
| No walking ability | 0/5 | - | - | - | - | - | - |
| ADL performance | |||||||
| Independent | 23/45 | 1.00 | reference | 1.00 | reference | ||
| Moderately dependent | 25/75 | 0.65 | 0.36-1.18 | .16 | 0.74 | 0.40-1.37 | .34 |
| Substantially dependent | 11/65 | 0.38 | 0.17-0.83 | .01 | 0.49 | 0.21-1.17 | .11 |
| Low-energy fracture | |||||||
| No | 15/47 | 1.00 | reference | 1.00 | reference | ||
| Yes | 79/266 | 1.09 | 0.62-1.93 | .76 | 1.16 | 0.63-2.13 | .63 |
| Fracture classification | |||||||
| Nondisplaced | 40/167 | 1.00 | reference | 1.00 | reference | ||
| Displaced | 54/155 | 1.88 | 1.22-2.89 | .004 | 1.61 | 1.01-2.55 | .04 |
| Quality of reposition | |||||||
| Good | 57/211 | 1.00 | reference | 1.00 | reference | ||
| Fair | 20/65 | 1.49 | 0.88-2.51 | .13 | 1.45 | 0.85-2.47 | .17 |
| Poor | 16/38 | 1.89 | 1.04-3.42 | .04 | 1.95 | 1.02-3.72 | .04 |
Note. Boldface values are statistically significant.
Abbreviations: ADL, activities of daily living; CI, confidence interval.
aFactors Associated with the Risk of Reoperation Due to Secondary Displacement Within 2 Years after hip fracture.
bAdjusted for gender, age, prednisone treatment, low-energy fracture, Garden type, and quality of reposition.
Figure 2.
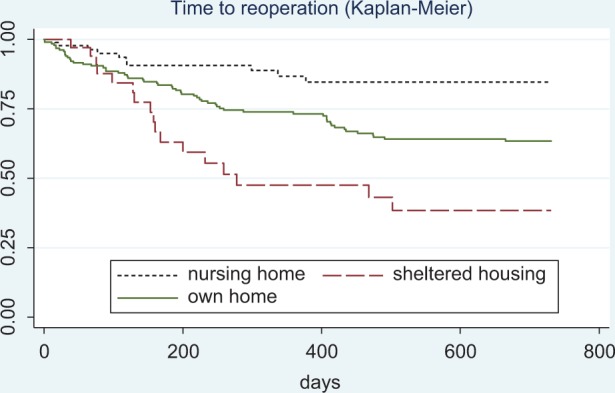
Kaplan-Meier plot. Time to reoperation within 2 years after femoral neck fracture in 65+ aged elderly patients treated with cannulated screws and admitted from own homes, sheltered housings, or nursing homes.
Discussion
We have attempted to identify related nonhealing factors that increase the risk of reoperation within 2 years in elderly patients with femoral neck fractures treated with cannulated screws. The elderly individuals with displaced fractures had the highest risk of reoperation. Our findings are consistent with Jordan et al reporting that initial fracture displacement is the most important factor related to risk of reoperation.23 Hui et al found that internal fixation may not be the best treatment for femoral neck fractures, whereas hemiarthroplasty for displaced fractures in elderly individuals yielded a better result in terms of lower rates of reoperation compared to internal fixation in patients with nondisplaced fractures.24 Even in elderly patients with severely impaired cognitive function, hemiarthroplasty seemed to be the best choice.25 Although guidelines recommend internal fixation only in the nondisplaced fractures, half of the femoral neck fractures in our study were treated with cannulated screws, despite displacement. However, the surgeons may have chosen this technique due to the frailty of the patient population, since it is well known that longer duration of surgery combined with the arthroplasty procedure increases the risk of complications and mortality in the elderly individuals.7,8 Our reoperation rates were within the ranges reported in the literature.10,26,27
We found that reoperations were mostly performed in the youngest group of the elderly individuals and possibly in the cognitively and physically well-functioning elderly individuals. Residents from own homes and sheltered housing facilities are not as old, frail, and functionally impaired as the nursing home residents and may perform activities with higher loads and strains. The younger and more mobile patients have higher demands to good functional results, and their QoL depends on being pain free; thus, they are more often referred to a reoperation. Nursing home residents might not have the same need for independence, lack the ability to express it, or postsurgical follow-up is inadequate in the weakest patients. The findings that nursing home residents are at highest risk of dying but inversely at lowest risk of reoperation were consistent with the results of a study by Hoelsbrekken et al in Norwegian patients with femoral neck fracture.27
In the nondisplaced fractures, no significant association was found between the risk of reoperation and quality of the fracture repair reduction most likely due to a high degree of inherent stability. In the displaced fractures, however, we found a higher risk of reoperation in patients with poor fracture reduction, and this is consistent with earlier studies.28 When a satisfactory surgical reduction cannot be attained, conversion to arthroplasty should be considered. Total hip arthroplasty is recommended for the displaced hip fractures primarily in cognitively well-functioning patients aged 70+ years and hemiarthroplasty in elderly individuals with dementia.2–6 The bone quality in elderly patients plays an extremely important role in the outcome of internal fixation. Preventing bone loss by weight bearing is essential for healing of the osteoporotic bone postoperatively. Bed rest is critical to bone loss, since serum calcium increases during bed rest and tends to increase less by exercise.29 The low-energy trauma would indicate significant loss of density and potential risk of fixation failure. Furthermore, the physical and mental state of elderly patients is important to the treatment algorithm of femoral neck fractures as is fracture type and bone density due to the ability to control the injured limb.
Strengths and Limitations
The study population was complete for the chosen time period, and all the follow-up outcomes were obtained. We had the possibility to analyze data presuming that our results may generate new hypotheses. However, our study had several limitations. The retrospective design with search for true information in patient records and databases was in some cases sparse or missing and may have affected the results. Surgical delay is not taken into account and may have confounded the result, due to higher risk of nonunion for patients treated more than 48 hours after injury.27 We did not take other potential predictors into consideration such as comorbidity, anemia, risk of fall, and surgeon’s skills and experience.
Conclusion
In elderly patients with femoral neck fracture treated with cannulated screws, 1 of every 3 patients is expected to undergo a reoperation within 2 years. Younger age, displaced femoral neck fracture, higher BMI, and poor quality of fracture repair were associated with reoperation. Primary prosthetic replacement should be recommended over internal fixation in elderly individuals with displaced femoral neck fractures in the youngest and most ADL-independent elderly individuals. Impact of outlined predictors on complications needs to be examined in future prospective studies.
Acknowledgments
We would like to thank the Department of Assistive Devices and the National Indicator Project.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. “Danish Hip Fracture Register”. Danish annual report (December 1, 2012-November 30, 2013). Web site https://www.sundhed.dk/content/cms/62/4662_hofte_lprrapport2013_06april2014_2_offt.pdf. Accessed April 6, 2014. Published April 6, 2014. Updated April 6, 2014.
- 2. Sygeplejeråd Dansk, Fysioterapeuter Danske, Selskab Dansk Ortopædisk. Referenceprogram for patienter med hoftefraktur. Website http://www.ortopaedi.dk/fileadmin/Guidelines/Referenceprogrammer/Referenceprogram_for_patienter_med_hoftebrud2008.pdf . Accessed Oktober/16, 2008. Published October 16, 2008. Updated October 16, 2008.
- 3. Rogmark C, Johnell O. Primary arthroplasty is better than internal fixation of displaced femoral neck fractures: a meta-analysis of 14 randomized studies with 2,289 patients. Acta Orthop. 2006;77(3):359–367. [DOI] [PubMed] [Google Scholar]
- 4. Parker MJ, Pryor G, Gurusamy K. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures: a long-term follow-up of a randomised trial. Injury. 2010;41(4):370–373. [DOI] [PubMed] [Google Scholar]
- 5. Parker MJ, Gurusamy K. Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adults. Cochrane Database Syst Rev. 2006;(4):CD001708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76(1):15–25. [DOI] [PubMed] [Google Scholar]
- 7. Parker MJ, Pryor GA. Internal fixation or arthroplasty for displaced cervical hip fractures in the elderly: a randomised controlled trial of 208 patients. Acta Orthop Scand. 2000;71(5):440–446. [DOI] [PubMed] [Google Scholar]
- 8. van Dortmont LM, Douw CM, van Breukelen AM, et al. Cannulated screws versus hemiarthroplasty for displaced intracapsular femoral neck fractures in demented patients. Ann Chir Gynaecol. 2000;89(2):132–137. [PubMed] [Google Scholar]
- 9. Rutter PD, Panesar SS, Darzi A, Donaldson LJ. What is the risk of death or severe harm due to bone cement implantation syndrome among patients undergoing hip hemiarthroplasty for fractured neck of femur? A patient safety surveillance study. BMJ Open. 2014;4(6):e004853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Murphy DK, Randell T, Brennan KL, Probe RA, Brennan ML. Treatment and displacement affect the reoperation rate for femoral neck fracture trauma. Clin Orthop Relat Res. 2013;471(8):2691–2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zlowodzki M, Brink O, Switzer J, et al. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: a multi-centre cohort study. J Bone Joint Surg Br. 2008;90(11):1487–1494. [DOI] [PubMed] [Google Scholar]
- 12. Tidermark J. Quality of life and femoral neck fractures. Acta Orthop Scand Suppl. 2003;74(309):1–42. [PubMed] [Google Scholar]
- 13. Lauritzen JB. The importance of osteoporosis in the treatment of fractures and orthopedic-surgical possibilities. Ugeskr Laeger. 2001;163(40):5496–5502. [PubMed] [Google Scholar]
- 14. Woltman K, den Hoed PT. Osteoporosis in patients with a low-energy fracture: 3 years of screening in an osteoporosis outpatient clinic. J Trauma. 2010;69(1):169–173. [DOI] [PubMed] [Google Scholar]
- 15. Ortiz-Alonso FJ, Vidan-Astiz M, Alonso-Armesto M, et al. The pattern of recovery of ambulation after hip fracture differs with age in elderly patients. J Gerontol A Biol Sci Med Sci. 2012;67(6):690–697. [DOI] [PubMed] [Google Scholar]
- 16. Barrios C, Brostrom LA, Stark A, Walheim G. Healing complications after internal fixation of trochanteric hip fractures: the prognostic value of osteoporosis. J Orthop Trauma. 1993;7(5):438–442. [DOI] [PubMed] [Google Scholar]
- 17. Espaulella J, Guyer H, Diaz-Escriu F, Mellado-Navas JA, Castells M, Pladevall M. Nutritional supplementation of elderly hip fracture patients. a randomized, double-blind, placebo-controlled trial. Age Ageing. 2000;29(5):425–431. [DOI] [PubMed] [Google Scholar]
- 18. Porter KH, Johnson MA. Dietary protein supplementation and recovery from femoral fracture. Nutr Rev. 1998;56(11):337–340. [DOI] [PubMed] [Google Scholar]
- 19. Sundhedsstyrelsen. Anbefalinger om D-vitamin. Web site http://sundhedsstyrelsen.dk/da/sundhed/ernaering/d-vitamin?sc_site=website. Accessed March 13, 2009. Published March 13, 2009. Updated February 28, 2013.
- 20. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42(8):703–709. [DOI] [PubMed] [Google Scholar]
- 21. Garden RS. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br. 1961;43B(4):647–663. [Google Scholar]
- 22. Lindequist S, Törnkvist H. Quality of reduction and cortical screw support in femoral neck fractures. J Orthop Trauma. 1995:9(3):215–221 [DOI] [PubMed] [Google Scholar]
- 23. Jordan RW, Smith NA, Dickenson E, Parsons H, Griffin X. Risk factors associated with the early failure of cannulated hip screws. Acta Orthop Belg. 2014;80(1):34–38. [PubMed] [Google Scholar]
- 24. Hui ACW, Anderson GH, Choudhry R, Boyle J, Gregg PJ. Internal fixation or hemiarthroplasty for undisplaced fractures of the femoral neck in octogenarians. J Bone Jt Surg Ser B. 1994;76(6):891–894. [PubMed] [Google Scholar]
- 25. Hedbeck CJ, Inngul C, Blomfeldt R, Ponzer S, Tornkvist H, Enocson A. Internal fixation versus cemented hemiarthroplasty for displaced femoral neck fractures in patients with severe cognitive dysfunction: a randomized controlled trial. J Orthop Trauma. 2013;27(12):690–695. [DOI] [PubMed] [Google Scholar]
- 26. Elmerson S, Sjostedt A, Zetterberg C. Fixation of femoral neck fracture. A randomized 2-year follow-up study of hook pins and sliding screw plate in 222 patients. Acta Orthop Scand. 1995;66(6):507–510. [DOI] [PubMed] [Google Scholar]
- 27. Holmberg S, Kalen R, Thorngren K. Treatment and outcome of femoral neck fractures: an analysis of 2418 patients admitted from their own homes. Clin Orthop Relat Res. 1987;(218):42–52. [PubMed] [Google Scholar]
- 28. Hoelsbrekken SE, Opsahl JH, Stiris M, Paulsrud O, Stromsoe K. Failed internal fixation of femoral neck fractures. Tidsskr Nor Laegeforen. 2012;132(11):1343–1347. [DOI] [PubMed] [Google Scholar]
- 29. Bray TJ, Smith-Hoefer E, Hooper A, Timmerman L. The displaced femoral neck fracture. internal fixation versus bipolar endoprosthesis. results of a prospective, randomized comparison. Clin Orthop Relat Res. 1988(230):127–140. [PubMed] [Google Scholar]